Abstract
Cyr61 (CCN1) is the product of a growth factor–inducible immediate early gene and is involved in cell adhesion, survival, proliferation and differentiation. Cyr61 is overexpressed in human tumors and is involved in the development of tumors. However, the role that Cyr61 plays in acute lymphoblastic leukemia (ALL) cells remains undetermined. The aim of this study was to identify the role of Cyr61 in regulating ALL cell survival. Here, we found that the level of Cyr61 was increased in the plasma and bone marrow (BM) from ALL patients compared with samples from normal control patients. Furthermore, we observed that Cyr61 could effectively stimulate Jurkat (T ALL cell lines), Nalm-6 (B ALL cell lines) and primary ALL cell survival. Mechanistically, we showed that Cyr61 stimulated ALL cell survival via the AKT/NF-κB signaling pathways and the consequent up-regulation of Bcl-2. Taken together, our study is the first to reveal that Cyr61 is elevated in ALL and promotes cell survival through the AKT/NF-κB pathway by up-regulating Bcl-2. Our findings suggest that Cyr61 plays an important role in the pathogenesis of ALL.
Similar content being viewed by others
Introduction
Acute lymphoblastic leukemia (ALL) is characterized by the monoclonal and/or oligoclonal proliferation of hematopoietic precursor cells in the bone marrow (BM). Although it has long been recognized that genetic abnormalities are critical for the development of ALL, increasing evidence suggests that BM stromal cell-derived soluble factors contribute to the pathogenesis of ALL1,2,3,4,5.
BM stromal cell-derived soluble factors mainly include extracellular matrix molecules, cytokines and chemokines. BM stromal cell-derived soluble factors and BM stromal cells (mesenchymal stem cells, osteoblasts, fibroblasts, adipocytes) form a highly organized three-dimensional scaffold and provide a permissive environment for leukemogenesis and progression4,5,6. Previous studies have shown that stromal-cell-derived factor 1 (SDF-1), interleukin (IL)-3, IL-7, IL-8, CCL2 and stem cell factor (SCF), alone or in different combinations, were shown to promote the survival and (or) the proliferation of ALL cells, although the degree of stimulation is heterogeneous between patient samples and between growth factors7,8,9,10,11. Levels of basic fibroblast growth factor (bFGF), vascular endothelial factor (VEGF), IL-8 and CCL2 are increased in the BM plasma from ALL patients and these growth factors can enhance angiogenesis and increase the adhesion of ALL cells to BM stromal cells; in some cases, these growth factors may contribute to the development of ALL12,13. Together, these results suggest that BM stromal cell-derived soluble factors play important roles in the pathogenesis of ALL. Thus, studies related to BM stromal cell-derived soluble factors would provide a better understanding of the pathogenesis of ALL and facilitate the design of new treatments.
Cyr61/CCN1 is a secreted extracellular matrix (ECM) protein, which is important for cell proliferation, survival, adhesion, migration and differentiation14. As a secreted protein, Cyr61 binds to integrins and promotes the development of tumors14,15,16. Cyr61 was originally identified as a growth factor-inducible immediate early gene. It is transcriptionally activated within minutes of stimulation by a variety of factors, including growth factors, cytokines, vitamin D3, cortisol and G-protein coupled receptor (GPCR) agonists17,18,19,20. Endothelial and epithelial cells, mesangial cells, mesenchymal cells, smooth muscle cells, cardiomyocytes, osteoblasts, trophoblasts and fibroblast-like synoviocytes have been identified as sources of Cyr6120,21,22,23. Recent studies have shown that stromal cells are the major source of Cyr61 in bone marrow24,25. Notably, Cyr61 is involved in stroma-induced chemo-resistance in acute myeloid leukemia (AML) and the inhibition of Cyr61 could block AML cell growth24,25. However, whether Cyr61 is involved in the pathogenesis of ALL has not yet been explored.
In this study, we explored the level of Cyr61 in ALL patients and investigated the possible role of Cyr61 in ALL cell survival. We found that Cyr61 is increased in the plasma and the BM from ALL patients. Furthermore, we observed that Cyr61 could effectively promote ALL cell survival through the AKT/NF-κB pathway by up-regulating Bcl-2 and that this effect was abrogated using neutralizing antibodies against human Cyr61. To our knowledge, this study is the first to reveal that the level of Cyr61 is increased in ALL patients and that Cyr61 plays a critical role in ALL cell survival. Our findings suggest that Cyr61 plays an important role in the development of ALL.
Results
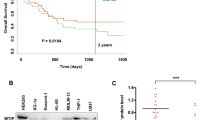
The level of Cyr61 is increased in the plasma and bone marrow (BM) from ALL patients
Numerous studies have demonstrated that Cyr61 is an important ECM protein that plays a key role in the pathogenesis of tumors26,27,28,29,30,31; recent studies have shown that Cyr61 is involved in stroma-induced chemo-resistance in acute myeloid leukemia (AML)24 and that inhibiting Cyr61 could block AML cell growth24,25. To explore the role of Cyr61 in the pathogenesis of ALL, we examined Cyr61 concentrations in the plasma and BM from newly diagnosed without any treatment ALL patients (see Supplementary Table S1 and Supplementary Table S2). The results showed that the levels of Cyr61 were increased in the plasma and BM from ALL patients compared with the plasma and BM derived from healthy controls (Fig. 1a, p < 0.0001, **p < 0.01, Student’s t-test; Fig. 1b, p = 0.0012, **p < 0.01, Student’s t-test) and the levels of Cyr61 were not different in the plasma and BM from T-lymphoblastic leukemia (T-ALL) and B-lymphoblastic leukemia (B-ALL) patients (Data not shown). We analyzed the role of Cyr61 in the diagnosis of leukemia and found that the level of Cyr61 in the plasma was significantly related to the number of white blood cells (WBCs) and the level of Cyr61 in the BM was significantly related to the percentage of blasts (Fig. 1c,d). Taken together, these data showed that the level of Cyr61 is increased in ALL patient samples, suggesting that Cyr61 could play a key role in the pathogenesis of ALL.
The level of Cyr61 is increased in the plasma and bone marrow (BM) from ALL patients.
(a) The levels of Cyr61 in the plasma from newly diagnosed without any treatment ALL patients (n = 34) and the normal plasma from age-matched healthy individuals (n = 66) were detected by ELISA. (b) The levels of Cyr61 in the BM from newly diagnosed without any treatment ALL patients (n = 49) and the normal BM from age-matched healthy transplant donors (n = 11) were detected by ELISA. (c) The relationship of Cyr61 concentrations in the plasma from ALL patients with the number of white blood cells (WBCs) in the peripheral blood was analyzed (n = 33). (d) The relationship of Cyr61 concentrations in the BM from ALL patients with the percent of blasts in the BM was analyzed (n = 49). **P < 0.01.
Cyr61 effectively stimulated ALL cell survival
In earlier studies, Cyr61 promoted cell growth in many human tumors26,27,29,32,33; however, it inhibited the growth of lung cancer cells and liver cancer cell lines34,35,36. To explore whether increased Cyr61 in ALL BM could regulate ALL cell survival, 3 primary T-ALL cells and 3 primary B-ALL cells (see Supplementary Table S3: P1-P6) were cultured in BM supernatants from ALL patients newly diagnosed without any treatment (see Supplementary Table S3: P1-P6) and the results showed that the anti-Cyr61 monoclonal antibody 093G9 could decrease the survival of primary ALL cells cultured in BM supernatants (Fig. 2a, T-ALL p = 0.0349, *p < 0.05, B-ALL p = 0.0151, *p < 0.05, Student’s t-test). Next, 4 primary T-ALL cells and 5 primary B-ALL cells (see Supplementary Table S3: P7-P15) were collected and exposed to recombinant human Cyr61; the results showed that recombinant human Cyr61 could also enhance primary ALL cell survival and the anti-Cyr61 monoclonal antibody 093G9 could block this effect of Cyr61 on primary ALL cells (Fig. 2b, T-ALL p = 0.0035, *p < 0.05, B-ALL p = 0.0098, **p < 0.01, ANOVA with Student-Newman-Keuls tests). These results showed that Cyr61 could stimulate primary ALL cell survival.
Cyr61 effectively stimulated primary ALL cell survival.
(a) 3 primary T-ALL cells and 3 primary B-ALL cells (see Supplementary Table S3: P1-P6) were collected and incubated with BM supernatants (Cyr61 concentration is 185 pg/ml) with or without preincubation with anti-human Cyr61 monoclonal antibody (093G9) (1000 pg/ml) and after incubation for 72 h, cell survival was measured using the CCK8 kit. Murine isotype-matched antibody (con-IgG) was used as a control. (b) Left panel: Primary T-ALL cell survival was stimulated with 100 ng/ml Cyr61, but Cyr61-stimulated ALL cell survival was inhibited by the addition of the anti-human Cyr61 monoclonal antibody (093G9) (500 ng/ml). Right panel: Primary B-ALL cell survival was stimulated with 1000 ng/ml Cyr61, but Cyr61-stimulated ALL cell survival was inhibited by the addition of the anti-human Cyr61 monoclonal antibody (093G9) (5000 ng/ml). Data represent the mean ± SEM of at least 3 independent experiments. *P < 0.05, **P < 0.01.
To explore the mechanism of Cyr61-stimulated ALL cell survival, T ALL cell lines (Jurkat) and B ALL cell lines (Nalm-6) were exposed to Cyr61 in a suspension culture and its effects on survival were examined. As shown in Fig. 3a, the survival of Jurkat and Nalm-6 cells were markedly increased in a dose-dependent manner when exposed to Cyr61. We then treated Jurkat and Nalm-6 cells with the anti-Cyr61 monoclonal antibody 093G9 to block Cyr61 function and the results showed that exposure to 093G9 significantly decreased the effect of Cyr61 on Jurkat and Nalm-6 cell survival (Fig. 3b, Jurkat p = 0.0059, **p < 0.01, Nalm-6 p = 0.0424, *p < 0.05, ANOVA with Student-Newman-Keuls tests). The up-regulation of ALL cell survival by Cyr61 could be due to enhanced cell division and/or reduced cell apoptosis. The CFSE assay showed that Cyr61 had little effect on ALL cell division (see Supplementary Figure S1). Next, we investigated whether Cyr61 could protect ALL cells from apoptosis. Exogenous Cyr61 was added to cultures of starved Jurkat and Nalm-6 cells and the apoptosis of the Jurkat and Nalm-6 cells was assayed using annexin V-FITC and propidium iodide staining. The apoptosis of the Jurkat and Nalm-6 cells induced by serum deprivation was significantly decreased in the presence of exogenous Cyr61 (Fig. 3c, Jurkat p = 0.0208, *p < 0.05, Nalm-6 p = 0.0046, **p < 0.01, Student’s t-test). These results showed that Cyr61 effectively stimulated ALL cell survival by decreasing cell apoptosis.
Cyr61 effectively decreased ALL cell apoptosis.
(a) Left panel: Jurkat cells were stimulated with exogenous recombinant human Cyr61 (25, 50, 100, 200 ng/ml) and after incubation for 72 h, cell survival was measured using the CCK8 kit. Right panel: Nalm-6 cells were stimulated with exogenous recombinant human Cyr61 (250, 500, 1000, 2000 ng/ml) and after incubation for 72 h, cell survival was measured using the CCK8 kit. (b) Left panel: Jurkat survival induced by Cyr61 was inhibited by the addition of an anti-human Cyr61 monoclonal antibody (093G9) (500 ng/ml). Murine isotype-matched antibody (con-IgG) was used as a control. Right panel: Nalm-6 survival induced by Cyr61 was inhibited by the addition of an anti-human Cyr61 monoclonal antibody (093G9) (5000 ng/ml). Murine isotype-matched antibody (con-IgG) was used as a control. (d) Jurkat and Nalm-6 cells were starved in serum deprivation culture media with or without exogenous recombinant human Cyr61 (100 ng/ml for Jurkat; 1000 ng/ml for Nalm-6) for 48 h, the percentages of apoptotic Jurkat and Nalm-6 (FITC-positive) cells were determined by flow cytometric analysis. Data represent the mean ± SEM of at least 3 independent experiments. *P < 0.05, **P < 0.01.
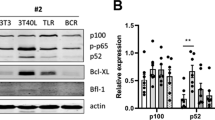
Cyr61 upregulated the Bcl-2 level in ALL cells
Bcl-2 family molecules are important regulators of cell survival and cell death, thus we used real-time PCR to analyze the expression profiles of Bcl-2, Bcl-xL, Bax and Bad in Cyr61-induced ALL cells (Jurkat and Nalm-6). The results showed that in Cyr61-induced Jurkat and Nalm-6 cells, the expression levels of Bcl-2 mRNA were increased significantly (Jurkat p = 0.0185, *p < 0.05, Nalm-6 p = 0.0109, *p < 0.05, Student’s t-test), while the expression levels of Bcl-xL, Bax and Bad did not change (Fig. 4a). Using western blotting, we confirmed that the Bcl-2 protein level was also significantly increased in Cyr61-induced ALL cells (Fig. 4b, Jurkat p = 0.0309, *p < 0.05, Nalm-6 p = 0.0214, *p < 0.05, Student’s t-test). Together, these results suggest that the ALL survival is positively regulated by Cyr61, likely through up-regulating Bcl-2.
Cyr61 upregulated Bcl-2 levels in ALL cells.
(a) Left panel: Bcl-2, Bcl-xL, Bax and Bad mRNA expression in Jurkat cells stimulated by 100 ng/ml Cyr61 for 8 h was detected by real-time PCR. Right panel: Bcl-2, Bcl-xL, Bax and Bad mRNA expression in Nalm-6 cells stimulated by 1000 ng/ml Cyr61 for 8 h was detected by real-time PCR. (b) Left panel: The protein levels of Bcl-2 in Jurkat cells stimulated by 100 ng/ml Cyr61 for 48 h were detected by western blotting. Right panel: The protein level of Bcl-2 in Nalm-6 cells stimulated by 1000 ng/ml Cyr61 for 48 h was detected by western blotting. The band intensity of Bcl-2 was quantified by densitometry and normalized to GAPDH. Data represent the mean ± SEM of at least 3 independent experiments. *P < 0.05, **P < 0.01.
Cyr61-induced ALL cell survival depends on the AKT/NF-κB signaling pathway
To investigate the mechanism of Cyr61-induced ALL cell survival, Jurkat and Nalm-6 cells were further studied. Previous studies have shown that NF-κB, ERK1/2 and PI3K-AKT are activated downstream of Cyr61 and are associated with proliferation in cancer cells15,37,38,39; thus, we probed downstream signaling pathway(s) using known inhibitors of several pathways, including Ly294002 (an inhibitor of the PI3K/AKT pathway), PDTC (an inhibitor of NF-κB activation) and PD98059 (an inhibitor of ERK1/2). The results showed that Cyr61-induced ALL cell (Jurkat and Nalm-6) survival was markedly decreased in the presence of the PI3K/AKT and NF-κB inhibitors. In contrast, the inhibition of ERK1/2 activity had no effect on Cyr61-induced ALL cell survival (Fig. 5a). Further analysis showed that Cyr61 treatment led to a dramatic increase in the phosphorylation of the AKT and NF-κB p65 subunit in Jurkat and Nalm-6 cells (Fig. 5b). Next, we treated cells with the NF-κB inhibitor PDTC to determine whether NF-κB is associated with the Cyr61-mediated regulation of Bcl-2. Our results indicated that treatment with PDTC blocked Cyr61’s up-regulation of Bcl-2 expression in ALL cells (Fig. 5c, Jurkat p = 0.0412, *p < 0.05, Nalm-6 p = 0.0427, *p < 0.05, ANOVA with Student-Newman-Keuls tests). Together, these results suggest that the ALL survival is positively regulated by Cyr61, likely through the AKT/NF-κB pathway by up-regulating Bcl-2.
Signaling pathways involved in Cyr61-induced ALL cell survival.
(a) The effect of the inhibitors of signaling pathways on Cyr61-induced ALL cell survival. Left panel: Jurkat cells were treated with 20 μM LY2940024, 4 μM PDTC or 10 μM SB203580 in combination with Cyr61 (100 ng/ml) (shadow bars) for 72 h and Jurkat cell survival was evaluated using the CCK8 kit. Right panel: Nalm-6 cells were treated with 20 μM LY2940024, 4 μM PDTC or 10 μM SB203580 in combination with Cyr61 (1000 ng/ml) (shadow bars) for 72 h and Nalm-6 survival was evaluated using the CCK8 kit. Control (open bar); Cyr61 (no inhibitors, black bar). (b) The phosphorylation of AKT and NF-κB was detected by western blotting. Lane 1: unstimulated FLS, lane 2: stimulated with Cyr61 (100 ng/ml for Jurkat; 1000 ng/ml for Nalm-6) for 10 min. (c) Left panel: The protein levels of Bcl-2 in Jurkat cells stimulated by 100 ng/ml Cyr61 for 48 h, with or without preincubation with PDTC, were detected by western blotting. Right panel: The protein levels of Bcl-2 in Nalm-6 cells stimulated by 1000 ng/ml Cyr61 for 48 h, with or without preincubation with PDTC, were detected by western blotting. The band intensity of Bcl-2 was quantified by densitometry and normalized to GAPDH. Data represent the mean ± SEM of at least 3 independent experiments. *P < 0.05, **P < 0.01.
Discussion
In this study, we showed that the level of Cyr61 is increased in the plasma and BM from ALL patients. Furthermore, we provide evidence that Cyr61 could effectively promote ALL cell survival. These findings suggested that Cyr61 plays an important role in the development of ALL.
Previous studies have shown that Cyr61 is overexpressed in solid tumors14,15,16. Recent studies have shown that BM stromal cells are the major source of Cyr6124,25. Our study provides evidence that the level of Cyr61 was increased in the plasma and BM from ALL patients. Furthermore, considering that white blood cell (WBC) count in peripheral blood at diagnosis of ALL is considered to be one of independent risk factors and is used for the risk-group stratification40,41,42,43, we evaluated the correlation between the number of WBCs and the level of Cyr61 in peripheral blood from ALL patients. We found that in peripheral blood, the level of Cyr61 was significantly related to the number of WBCs. Importantly, we also found that in the BM from ALL patients, the level of Cyr61 was significantly related to the percentage of blasts, which is important for diagnosing ALL. This finding suggests that the level of Cyr61 is increased in ALL plasma and BM and Cyr61 may play an important role in the pathogenesis of ALL.
It is well known that ALL is characterized by the abnormal proliferation of hematopoietic precursor cells in the BM. Numerous observations support the fact that Cyr61 could promote the survival and (or) proliferation of tumor cells26,27,29,32,33 and a recent study showed that inhibiting Cyr61 could block AML cell growth25. Our study showed that Cyr61 could promote ALL cell survival by reducing apoptosis; however, Cyr61 has little effect on ALL cell division. In this study, we used recombinant human Cyr61 expressed using an E. coli system (PeproTech, Rocky Hill, NJ, USA) for the cell survival assay and the activity of the protein expressed by E. coli was lower than the native protein or that expressed by eukaryotic systems44. In addition, Cyr61’s effectiveness may depend on the bone marrow microenvironment and recombinant human Cyr61 is used in a completely different cell culture condition. Thus, we used higher doses of recombinant human Cyr61 than the amount of endogenous Cyr61 detected in the patients’ bone marrow to test its effect on cell survival in vitro in this study. Moreover, we observed that Jurkat cells (T-ALL cell lines) were more sensitive to Cyr61-induced survival than Nalm-6 cells (B-ALL cell lines), which indicates that different cells have different sensitivities to Cyr61. We speculate that this difference may be caused by the different expression of Bcl-2 in Cyr61-induced jurkat cells and Cyr61-induced Nalm-6 cells. Together, these findings demonstrate for the first time that Cyr61 decreases ALL cell apoptosis and promotes cell survival. The findings reported here are consistent with our previous results in which Cyr61 decreased the apoptosis of fibroblast-like synoviocytes from rheumatoid arthritis patients21. In addition, previous studies have shown that Cyr61 could decrease the apoptosis of tumor cells, resulting in chemotherapy resistance in breast cancer, cervical cancer and acute myeloid leukemia24,45,46. Cyr61 may be one of the causes of drug resistance in ALL. Our previous studies have shown that blocking Cyr61 activity with a specific mAb ameliorated the severity of the disease in rheumatoid arthritis47,48 and psoriasis49. According to the present and previous studies, Cyr61 plays important roles in the survival of ALL cells and blocking the Cyr61 pathway may be used for ALL treatment.
The regulation of cell survival is determined by the balance of anti-apoptotic and pro-apoptotic factors of Bcl-2 family proteins50, thus we evaluated the effect of Cyr61 on the expression of Bcl-2, Bcl-xL, Bax and Bad as a possible mechanism for Cyr61-induced survival. Our findings showed that Cyr61 could up-regulate Bcl-2 levels without affecting Bcl-xL, Bax or Bad. Considering that Bcl-2 acts as an anti-apoptotic factor, our findings suggested that Cyr61 regulates the survival and apoptosis of ALL cells through the Bcl-2 pathway.
It has been shown that AKT/NF-κB and ERK1/2 pathway are activated downstream of Cyr61 and could up-regulate anti-apoptotic Bcl-215,37,38,39,51,52,53,54,55. Thus, to address the signaling pathway of Cyr61-induced ALL cell survival, we evaluated the profile of the AKT/NF-κB and ERK1/2 pathways. As expected, the AKT/NF-κB pathway contributed to Cyr61-induced ALL cell survival. Recent evidences suggest that, in AML, Cyr61 mediated AML cell growth by the ERK1/2 pathway25; however, our findings showed that ERK1/2 did not contribute to Cyr61-induced ALL cell survival. Because early studies have shown that Cyr61 induces NF-κB activation via the PI3K/AKT pathway in breast cancer cells and fibroblast-like synoviocytes56,57,58,59, we suggest that Cyr61-induced ALL cell survival depends on the AKT/NF-κB signaling pathway. Next, we treated ALL cells with the NF-κB inhibitor PDTC and found that treatment with PDTC could block Cyr61’s up-regulation of Bcl-2 expression. Together, these results show that Cyr61-induced ALL cell survival involves the activation of the AKT/NF-κB pathway and the consequent up-regulation of the Bcl-2 pathway. Since BM microenvironment contains lots of growth factors4,5,6 and our study about the signaling pathway of Cyr61-induced ALL cell survival is in vitro study and absent other elements of the BM microenvironment, the signaling pathway of Cyr61-induced ALL cell survival in vivo need further study.
In this study, we explored the level of Cyr61 in the plasma and BM from ALL patients and investigated the possible role of Cyr61 in the development of ALL. We found that the level of Cyr61 is increased in the BM and plasma from ALL patients. Furthermore, we observed that Cyr61 could effectively stimulate ALL cell survival via the AKT/NF-κB signaling pathways with the consequent up-regulation of the Bcl-2 pathway. Our study indicated for the first time that Cyr61 plays an important role in the development of ALL.
Methods
Patients and specimens
ALL samples were obtained from the Affiliated Union Hospital of Fujian Medical University. The supernatant samples from BM (n = 48) were obtained after centrifugation of the total BM aspirates of consecutive ALL patients. Normal BM samples (n = 11) were obtained from the age-matched healthy transplant donors included as controls. Plasma samples from peripheral blood (n = 34) were collected after the centrifugation of peripheral blood from newly diagnosed without receiving any treatment ALL patients. Normal peripheral blood samples (n = 66) were obtained from the age-matched healthy individuals included as controls. The clinical characteristics of the ALL patients are shown in Supplementary Table S1 and Supplementary Table S2. For the survival studies of primary ALL cells cultured with BM supernatants, BM samples from newly diagnosed without receiving any treatment ALL patients (see Supplementary Table S3: P1-P6) were centrifuged at 500 g for 10 min and supernatants were collected and immediately stored at −80 °C until used. The leukemia cell lines Jurkat and Nalm-6 were kindly provided by Dr. Chen (Shanghai Jiao Tong University School of Medicine, Shanghai, China) and were maintained in RPMI 1640 medium (Hyclone, Logan, UT, USA) supplemented with 10% fetal bovine serum (Gibco, Carlsbad, CA, USA), 100 U/ml penicillin and 100 mg/ml streptomycin at 37 °C and 5% CO2. For the survival study, primary ALL cell samples from patients with ALL at the time of diagnosis were enriched for mononuclear cells by density centrifugation and cryopreserved; 7 patients with T-ALL and 8 patients with B-ALL were included (see Supplementary Table S3). Cells were carefully thawed in warm RPMI 1640 with 10% FBS and were cultured for research at 37 °C and 5% CO2. These studies were performed in accordance with the ethical guidelines under the protocols approved by the Institutional Medical Ethics Review Board of the Affiliated Union Hospital of Fujian Medical University, Fuzhou, China. Informed consent was obtained from all individual participants included in the study.
ELISA
The concentration of Cyr61 in the serum and BM from ALL patients was determined using a sandwich ELISA (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions. Three internal quality control serum samples or BM supernatants were tested in each assay to assess inter-assay precision. The calculated overall inter-assay coefficient of variation was 3.6% to 4.9%.
ALL cell survival and antibody neutralization assays
Approximately 2.5 × 104 cells/well Jurkat, 5 × 104 cells/well Nalm-6 and 5 × 104 cells/well primary ALL cells were plated in 96-well plates with 100 μl RPMI 1640 with 5% FBS and Cyr61 at different concentrations. For the antibody blocking assay, Cyr61 (PeproTech, Rocky Hill, NJ, USA) was preincubated for 1 h with mouse anti-Cyr61 mAb (093G9) [Anti-Cyr61 mAb was kindly provided by Dr. Li (Shanghai Jiao Tong University School of Medicine, Shanghai, China)] before the stimulation of ALL cell survival. An isotype-matched antibody was used as a control. After incubation for 72 h, cell viability was measured by adding 10 μl CCK8 reagent (Promega, Madison, WI, USA) and incubated for 2 h; then, the plates were monitored using a Power Wave XS microplate reader (BIO-TEK) at 450 nm absorbance.
Apoptosis assay
For apoptosis assays, apoptotic Jurkat and Nalm-6 cells were induced by serum deprivation in the presence or absence of Cyr61 (100 ng/ml for Jurkat and 1000 ng/ml for Nalm-6) for 48 h and were detected using an annexin V-fluorescein isothiocyanate (FITC) apoptosis detection kit (BD Biosciences, San Jose, CA, USA) according to the manufacturer’s instructions. The percentages of apoptotic Jurkat and Nalm-6 (FITC-positive) cells were determined by flow cytometric analysis. Flow cytometry was performed using a FACS Calibur cytometer (BD Biosciences, San Jose, CA, USA) and analyzed using Cellquest software (BD Biosciences, San Jose, CA, USA).
Real-time PCR analysis
Total RNA was extracted from specimens using a Tripure isolation reagent (Roche Diagnostics, Indianapolis, IN, USA) according to the manufacturer’s instructions. Total RNA (1 μg) was reverse transcribed into first strand cDNA using the RevertAidTM First Strand cDNA Synthesis Kit (Thermo Scientific, Maryland, USA). Briefly, 1 μl of 50 μM oligo(dT)20 and 1 μl of 10 mM dNTPs mix were added to the RNA and the volume was adjusted to 11 μl using RNase-free water. Messenger RNA (mRNA) was converted to cDNA according to the manufacturer′s instructions. Real-time PCR was performed using SYBR Green Master Mix (Applied Biosystems, Foster City, CA, USA) according to the manufacturer’s instructions. The primers used in this study were as follows: Bcl-2, forward, CTGGTGGGAGCTTGCATCAC; Bcl-2, reverse, ACAGCCTGCAGCTTTGTTTC; Bcl-xl, forward, TCAGGCTGCTTGGG ATAAAGAT; Bcl-xl, reverse, AGAGGCTTCTGGAGGACATTTG; Bax, forward, TGGAGCTGCAGAGGATG ATTG; Bax, reverse, CCAGTTGAAGTTGCCGTCAG A; Bad, forward, TAAGTC GCGAGCCAGGTTTAAC; Bad, reverse, AGACGCGGGCTTTATTAACATTT; GAPDH, forward, CACATGGCCTCCAAGGAGTA; GAPDH, reverse, TGAGGGT CTCTCTCTTCCTCTTGT.
Probing of the signaling pathways involved in Cyr61-induced ALL cell survival
Special inhibitors of the AKT and NF-κB signaling pathways were purchased from Sigma-Aldrich and used to analyze Cyr61-induced ALL cell survival. Briefly, 4 μM pyrrolidine dithiocarbamate (PDTC; an inhibitor of NF-κB activation) or 20 μM Ly294002 (an inhibitor of the PI3K/AKT pathway) was added to the cell culture and Cyr61 was added at the same time. After incubation for 3 days, cell viability was measured by adding 10 μl CCK8 reagent (Promega, Madison, WI, USA) for a 2 h incubation and then the plates were monitored using a Power Wave XS microplate reader (BIO-TEK) at an absorbance of 450 nm.
Western blot analysis
Protein immune blotting was performed as described previously21. In briefly, tissue or cell lysates were separated by SDS–PAGE electrophoresis followed by transferring to PVDF membranes (Millipore Corporation, Bedford, MA, USA) at 100 v for 90 min. The phosphoralation of AKT and NF-κB were analyzed using specific antibodies (Cell Signaling Technology Inc, Beverly, MA, USA). After washing with PBS, the membranes were incubated with HRP-conjugated goat anti-mouse IgG at RT for 1 h followed by washing with PBS. The target proteins were examined with ECL system (Millipore Corporation, Bedford, MA, USA) and visualized with autoradiography film.
Statistical analysis
The results were presented as the mean ± SEM unless indicated otherwise. Statistical analyses were performed using the SPSS software version 13.0 (SPSS Inc., Chi cago, IL, USA). The significance of difference between groups was assessed by the Student’s t test for single comparisons or by the analysis of variance (ANOVA) with the Student-Newman-Keuls tests for multiple comparisons. A value of P < 0.05 was considered as statistical significance.
Additional Information
How to cite this article: Zhu, X. et al. Cyr61 participates in the pathogenesis of acute lymphoblastic leukemia by enhancing cellular survival via the AKT/NF-κB signaling pathway. Sci. Rep. 6, 34018; doi: 10.1038/srep34018 (2016).
References
Shah, N., Oseth, L. & LeBien, T. W. Development of a model for evaluating the interaction between human pre-B acute lymphoblastic leukemic cells and the bone marrow stromal cell microenvironment. Blood 92, 3817–3828 (1998).
Wu, S. et al. Interaction of bone marrow stromal cells with lymphoblasts and effects of predinsolone on cytokine expression. Leuk Res 29, 63–72 (2005).
Purizaca, J., Meza, I. & Pelayo, R. Early lymphoid development and microenvironmental cues in B-cell acute lymphoblastic leukemia. Arch Med Res 43, 89–101 (2012).
Chiarini, F. et al. Advances in understanding the acute lymphoblastic leukemia bone marrow microenvironment: From biology to therapeutic targeting. Biochim Biophys Acta 1863, 449–463 (2016).
Sison, E. A. & Brown, P. The bone marrow microenvironment and leukemia: biology and therapeutic targeting. Expert Rev Hematol 4, 271–283 (2011).
Ayala, F., Dewar, R., Kieran, M. & Kalluri, R. Contribution of bone microenvironment to leukemogenesis and leukemia progression. Leukemia 23, 2233–2241 (2009).
Juarez, J., Baraz, R., Gaundar, S., Bradstock, K. & Bendall, L. Interaction of interleukin-7 and interleukin-3 with the CXCL12-induced proliferation of B-cell progenitor acute lymphoblastic leukemia. Haematologica 92, 450–459 (2007).
de Vasconcellos, J. F. et al. Increased CCL2 and IL-8 in the bone marrow microenvironment in acute lymphoblastic leukemia. Pediatr Blood Cancer 56, 568–577 (2011).
Nishii, K. et al. Survival of human leukaemic B-cell precursors is supported by stromal cells and cytokines: association with the expression of bcl-2 protein. Br J Haematol 105, 701–710 (1999).
Silva, A. et al. IL-7 contributes to the progression of human T-cell acute lymphoblastic leukemias. Cancer Res 71, 4780–4789 (2011).
Mowafi, F. et al. Chemokine CXCL12 enhances proliferation in pre-B-ALL via STAT5 activation. Pediatr Blood Cancer 50, 812–817 (2008).
Aguayo, A. et al. Angiogenesis in acute and chronic leukemias and myelodysplastic syndromes. Blood 96, 2240–2245 (2000).
Veiga, J. P., Costa, L. F., Sallan, S. E., Nadler, L. M. & Cardoso, A. A. Leukemia-stimulated bone marrow endothelium promotes leukemia cell survival. Exp Hematol 34, 610–621 (2006).
Lau, L. F. CCN1/CYR61: the very model of a modern matricellular protein. Cell Mol Life Sci 68, 3149–3163 (2011).
Chen, C. C. & Lau, L. F. Functions and mechanisms of action of CCN matricellular proteins. Int J Biochem Cell Biol 41, 771–783 (2009).
Emre, Y. & Imhof, B. A. Matricellular protein CCN1/CYR61: a new player in inflammation and leukocyte trafficking. Semin Immunopathol 36, 253–259 (2014).
Brigstock, D. R. The connective tissue growth factor/cysteine-rich 61/nephroblastoma overexpressed (CCN) family. Endocr Rev 20, 189–206 (1999).
Chen, Y. & Du, X. Y. Functional properties and intracellular signaling of CCN1/Cyr61. J Cell Biochem 100, 1337–1345 (2007).
Kireeva, M. L., Lam, S. C. & Lau, L. F. Adhesion of human umbilical vein endothelial cells to the immediate-early gene product Cyr61 is mediated through integrin alphavbeta3. J Biol Chem 273, 3090–3096 (1998).
Lobel, M. et al. CCN1: a novel inflammation-regulated biphasic immune cell migration modulator. Cell Mol Life Sci 69, 3101–3113 (2012).
Zhang, Q. et al. A critical role of Cyr61 in interleukin-17-dependent proliferation of fibroblast-like synoviocytes in rheumatoid arthritis. Arthritis Rheum 60, 3602–3612 (2009).
Yu, Y. et al. The matrix protein CCN1 (CYR61) promotes proliferation, migration and tube formation of endothelial progenitor cells. Exp Cell Res 314, 3198–3208 (2008).
Hilfiker-Kleiner, D. et al. Regulation of proangiogenic factor CCN1 in cardiac muscle: impact of ischemia, pressure overload and neurohumoral activation. Circulation 109, 2227–2233 (2004).
Long, X., Yu, Y., Perlaky, L., Man, T. K. & Redell, M. S. Stromal CYR61 Confers Resistance to Mitoxantrone via Spleen Tyrosine Kinase Activation in Human Acute Myeloid Leukaemia. Br J Haematol 170, 704–718 (2015).
Niu, C. C. et al. Inhibiting CCN1 blocks AML cell growth by disrupting the MEK/ERK pathway. Cancer Cell Int 14, 74 (2014).
Huang, Y. T. et al. The matricellular protein CYR61 interferes with normal pancreatic islets architecture and promotes pancreatic neuroendocrine tumor progression. Oncotarget 7, 1663–1674 (2016).
Liu, Y. et al. Cyr61/CCN1 overexpression induces epithelial-mesenchymal transition leading to laryngeal tumor invasion and metastasis and poor prognosis. Asian Pac J Cancer Prev 16, 2659–2664 (2015).
Hou, C. H., Lin, F. L., Hou, S. M. & Liu, J. F. Cyr61 promotes epithelial-mesenchymal transition and tumor metastasis of osteosarcoma by Raf-1/MEK/ERK/Elk-1/TWIST-1 signaling pathway. Mol Cancer 13, 236 (2014).
Maity, G. et al. Pancreatic tumor cell secreted CCN1/Cyr61 promotes endothelial cell migration and aberrant neovascularization. Sci Rep 4, 4995 (2014).
Goodwin, C. R. et al. Cyr61 mediates hepatocyte growth factor-dependent tumor cell growth, migration and Akt activation. Cancer Res 70, 2932–2941 (2010).
Nguyen, N., Kuliopulos, A., Graham, R. A. & Covic, L. Tumor-derived Cyr61(CCN1) promotes stromal matrix metalloproteinase-1 production and protease-activated receptor 1-dependent migration of breast cancer cells. Cancer Res 66, 2658–2665 (2006).
Cheng, G., Zhang, H., Zhang, L. & Zhang, J. Cyr61 promotes growth of glioblastoma in vitro and in vivo. Tumour Biol 36, 2869–2873 (2015).
Shi, W. et al. Cyr61 promotes growth of pancreatic carcinoma via nuclear exclusion of p27. Tumour Biol 35, 11147–11151 (2014).
Tong, X. et al. Cyr61 suppresses the growth of non-small-cell lung cancer cells via the beta-catenin-c-myc-p53 pathway. Oncogene 23, 4847–4855 (2004).
Tong, X. et al. Cyr61, a member of CCN family, is a tumor suppressor in non-small cell lung cancer. J Biol Chem 276, 47709–47714 (2001).
Chen, C. C., Kim, K. H. & Lau, L. F. The matricellular protein CCN1 suppresses hepatocarcinogenesis by inhibiting compensatory proliferation. Oncogene 35, 1314–1323 (2016).
Lin, M. T. et al. Cyr61 expression confers resistance to apoptosis in breast cancer MCF-7 cells by a mechanism of NF-kappaB-dependent XIAP up-regulation. J Biol Chem 279, 24015–24023 (2004).
Menendez, J. A. et al. A novel CYR61-triggered ‘CYR61-alphavbeta3 integrin loop’ regulates breast cancer cell survival and chemosensitivity through activation of ERK1/ERK2 MAPK signaling pathway. Oncogene 24, 761–779 (2005).
Kim, K. H., Chen, C. C., Alpini, G. & Lau, L. F. CCN1 induces hepatic ductular reaction through integrin alphavbeta(5)-mediated activation of NF-kappaB. J Clin Invest 125, 1886–1900 (2015).
Gaynon, P. S. et al. Children’s Cancer Group trials in childhood acute lymphoblastic leukemia: 1983-1995. Leukemia 14, 2223–2233 (2000).
Hastings, C. et al. Increased post-induction intensification improves outcome in children and adolescents with a markedly elevated white blood cell count (>/=200 × 10(9)/l) with T cell acute lymphoblastic leukaemia but not B cell disease: a report from the Children’s Oncology Group. Br J Haematol 168, 533–546 (2015).
Vaitkeviciene, G. et al. High white blood cell count at diagnosis of childhood acute lymphoblastic leukaemia: biological background and prognostic impact. Results from the NOPHO ALL-92 and ALL-2000 studies. Eur J Haematol 86, 38–46 (2011).
Donadieu, J. et al. Prognostic study of continuous variables (white blood cell count, peripheral blast cell count, haemoglobin level, platelet count and age) in childhood acute lymphoblastic leukaemia. Analysis Of a population of 1545 children treated by the French Acute Lymphoblastic Leukaemia Group (FRALLE). Br J Cancer 83, 1617–1622 (2000).
Mitra, N., Sinha, S., Ramya, T. N. & Surolia, A. N-linked oligosaccharides as outfitters for glycoprotein folding, form and function. Trends Biochem Sci 31, 156–163 (2006).
Rho, S. B., Woo, J. S., Chun, T. & Park, S. Y. Cysteine-rich 61 (CYR61) inhibits cisplatin-induced apoptosis in ovarian carcinoma cells. Biotechnol Lett 31, 23–28 (2009).
Lai, D., Ho, K. C., Hao, Y. & Yang, X. Taxol resistance in breast cancer cells is mediated by the hippo pathway component TAZ and its downstream transcriptional targets Cyr61 and CTGF. Cancer Res 71, 2728–2738 (2011).
Lin, J. et al. Cyr61 induces IL-6 production by fibroblast-like synoviocytes promoting Th17 differentiation in rheumatoid arthritis. J Immunol 188, 5776–5784 (2012).
Zhu, X. et al. Cyr61 is involved in neutrophil infiltration in joints by inducing IL-8 production by fibroblast-like synoviocytes in rheumatoid arthritis. Arthritis Res Ther 15, R187 (2013).
Sun, Y. et al. CCN1, a Pro-Inflammatory Factor, Aggravates Psoriasis Skin Lesions by Promoting Keratinocyte Activation. J Invest Dermatol 135, 2666–2675 (2015).
Gonzalez-Ramos, R., Defrere, S. & Devoto, L. Nuclear factor-kappaB: a main regulator of inflammation and cell survival in endometriosis pathophysiology. Fertil Steril 98, 520–528 (2012).
Fahy, B. N., Schlieman, M. G., Mortenson, M. M., Virudachalam, S. & Bold, R. J. Targeting BCL-2 overexpression in various human malignancies through NF-kappaB inhibition by the proteasome inhibitor bortezomib. Cancer Chemother Pharmacol 56, 46–54 (2005).
Lee, J. U. et al. Role of Bcl-2 family proteins (Bax, Bcl-2 and Bcl-X) on cellular susceptibility to radiation in pancreatic cancer cells. Eur J Cancer 35, 1374–1380 (1999).
Song, L., Chang, J. & Li, Z. A serine protease extracted from Trichosanthes kirilowii induces apoptosis via the PI3K/AKT-mediated mitochondrial pathway in human colorectal adenocarcinoma cells. Food Funct 7, 843–854 (2016).
Chen, G. et al. Curcumol induces HSC-T6 cell death through suppression of Bcl-2: involvement of PI3K and NF-kappaB pathways. Eur J Pharm Sci 65, 21–28 (2014).
Kim, H. Y. et al. Balsalazide Potentiates Parthenolide-Mediated Inhibition of Nuclear Factor-kappaB Signaling in HCT116 Human Colorectal Cancer Cells. Intest Res 13, 233–241 (2015).
Hayden, M. S. & Ghosh, S. NF-kappaB in immunobiology. Cell Res 21, 223–244 (2011).
Li, Q. & Verma, I. M. NF-kappaB regulation in the immune system. Nat Rev Immunol 2, 725–734 (2002).
Menendez, J. A., Mehmi, I., Griggs, D. W. & Lupu, R. The angiogenic factor CYR61 in breast cancer: molecular pathology and therapeutic perspectives. Endocr Relat Cancer 10, 141–152 (2003).
Zhu, X. et al. Cyr61 participates in the pathogenesis of rheumatoid arthritis by promoting proIL-1beta production by fibroblast-like synoviocytes through an AKT-dependent NF-kappaB signaling pathway. Clin Immunol 157, 187–197 (2015).
Acknowledgements
This work was supported by Natural Science Foundation of Fujian Province (2015J01400, 2016J01569), National Natural Science Foundation of China (81171656) and National Undergraduate Training Program for Innovation and Entrepreneurship (201510392025).
Author information
Authors and Affiliations
Contributions
N.L. and Y.C. conceived the research and took overall supervision in the study. X.Z., Y.S., C.W., C.P., P.L., M.W., P.Z., R.H., C.Z., W.L. and Y.L. performed experiments. X.Z., Y.S., Y.C. and N.L. performed data analysis. X.Z., Y.S., Y.C. and N.L. wrote the manuscript. X.Z., Y.S., Y.C. and N.L. contributed to the discussion of results and to the review of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhu, X., Song, Y., Wu, C. et al. Cyr61 participates in the pathogenesis of acute lymphoblastic leukemia by enhancing cellular survival via the AKT/NF-κB signaling pathway. Sci Rep 6, 34018 (2016). https://doi.org/10.1038/srep34018
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep34018
This article is cited by
-
CCN2 (Cellular Communication Network factor 2) in the bone marrow microenvironment, normal and malignant hematopoiesis
Journal of Cell Communication and Signaling (2021)
-
The CCN axis in cancer development and progression
Journal of Cell Communication and Signaling (2021)
-
Inflammation and tissue homeostasis: the NF-κB system in physiology and malignant progression
Molecular Biology Reports (2020)
-
Global quantitative biology can illuminate ontological connections between diseases
Quantitative Biology (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.