Abstract
To clarify the physiological and pathophysiological roles of intestinal urate excretion via ABCG2 in humans, we genotyped ABCG2 dysfunctional common variants, Q126X (rs72552713) and Q141K (rs2231142), in end-stage renal disease (hemodialysis) and acute gastroenteritis patients, respectively. ABCG2 dysfunction markedly increased serum uric acid (SUA) levels in 106 hemodialysis patients (P = 1.1 × 10−4), which demonstrated the physiological role of ABCG2 for intestinal urate excretion because their urate excretion almost depends on intestinal excretion via ABCG2. Also, ABCG2 dysfunction significantly elevated SUA in 67 acute gastroenteritis patients (P = 6.3 × 10−3) regardless of the degree of dehydration, which demonstrated the pathophysiological role of ABCG2 in acute gastroenteritis. These findings for the first time show ABCG2-mediated intestinal urate excretion in humans, and indicates the physiological and pathophysiological importance of intestinal epithelium as an excretion pathway besides an absorption pathway. Furthermore, increased SUA could be a useful marker not only for dehydration but also epithelial impairment of intestine.
Similar content being viewed by others
Introduction
Hyperuricemia is a common disease which induces gout, and can lead to renal disorder, hypertension, cardiovascular or cerebrovascular diseases1. ATP-binding cassette transporter, subfamily G, member 2 (ABCG2/BCRP) is a high-capacity urate transporter2 and expresses in both intestine3 and kidney4. We and others previously demonstrated that ABCG2 dysfunction by its common variants causes gout2,5,6 and hyperuricemia2,7 by decreasing urate excretion. However, the evaluation of intestinal urate excretion in humans is very difficult due to urate degradation by intestinal bacterial flora. Thus, our previous study8 has revealed the importance of ABCG2 for intestinal urate excretion using Abcg2-knockout mice, but not in humans. In this study, to clarify the physiological role of intestinal urate excretion via ABCG2 in humans, we performed genotyping of ABCG2 dysfunctional variants in end-stage renal disease (hemodialysis) patients whose serum uric acid (SUA) levels are extremely elevated9,10 and urate excretion almost depends on intestinal excretion via ABCG2 because of their almost complete absence of renal urate excretion. Furthermore, to investigate the pathophysiological role of intestinal urate excretion via ABCG2 in intestinal diseases, we also performed genotyping of ABCG2 dysfunctional variants in acute gastroenteritis patients whose ABCG2 function of intestinal urate excretion should be seriously impaired due to damage to the intestinal epithelium.
Results
Genotyping of ABCG2
Genotyping results of the two ABCG2 dysfunctional variants, Q126X (rs72552713) and Q141K (rs2231142), for 106 hemodialysis patients, 106 sex- and body mass index (BMI)-matched health examination participants and 67 acute gastroenteritis patients, were shown in Table 1. The call rates for both variants were 100%, and they were in Hardy-Weinberg equilibrium (P > 0.05). Haplotype frequency of Q126X and Q141K was estimated as shown in Supplementary Table 1. This result indicates that there is no simultaneous presence of the minor allele of Q126X (“T” allele) and Q141K (“A” allele) in one haplotype, which is consistent with our previous study2. Therefore, we presumed the diplotypes of all samples as shown in Table 1. In this study, all of the participants were divided into three groups (full function, 3/4 function and ≤1/2 function) based on estimated ABCG2 function for the following analyses.
Analysis of hemodialysis patients
The estimated ABCG2 function of 106 hemodialysis patients and the mean SUA for each group were shown in Table 2. The less activity the ABCG2 function showed the higher the SUA (7.1 mg/dl for full function, 7.9 mg/dl for 3/4 function and 8.4 mg/dl for ≤1/2 function), and multiple regression analysis revealed that ABCG2 dysfunction significantly elevated SUA (P = 1.1 × 10−4). On the other hand, in 106 sex- and BMI-matched health examination participants, ABCG2 dysfunction tended to elevate SUA (5.3 mg/dl for full function, 5.0 mg/dl for 3/4 function and 6.0 mg/dl for ≤1/2 function), although not significantly (P = 0.36, Table 2).
Analysis of acute gastroenteritis patients
The SUA levels of 67 patients were measured during an acute period of gastroenteritis. Additionally, the SUA levels of 55 patients were measured during the recovery period from gastroenteritis. The mean SUA levels of the acute and recovery period (Table 2) were 8.8 mg/dl and 4.7 mg/dl, respectively, and the paired t-test showed a significant difference between them (P = 2.3 × 10−12). The number of patients, who were divided into three groups by estimated ABCG2 function, and the mean SUA levels at the acute and recovery period of gastroenteritis were shown in Table 2. In the acute period, ABCG2 dysfunction significantly elevated SUA (7.5 mg/dl for full function, 9.6 mg/dl for 3/4 function and 10.6 mg/dl for ≤1/2 function, P = 6.3 × 10−3), and the degree of dehydration also affected SUA (P = 1.6 × 10−3, Supplementary Table 2). However, ABCG2 dysfunction was not associated with the degree of dehydration in the acute period (P = 0.50, Table 3) and the significant association between ABCG2 dysfunction and SUA remained after the adjustment for the degree of dehydration (P = 7.8 × 10−3), indicating that the association between ABCG2 dysfunction and SUA was not due to dehydration. Regarding the recovery period, there was a trend for SUA to increase by ABCG2 dysfunction (4.2 mg/dl for full function, 4.9 mg/dl for 3/4 function and 5.4 mg/dl for ≤1/2 function, Table 2), but it was not significant (P = 0.10).
Discussion
ABCG2, which mediates urate excretion, expresses in both intestine3 and kidney4. About two-thirds of urate is excreted from kidney and about one-third from intestine11,12. This is consistent with our previous study using Abcg2-knockout mice8. However, ABCG2-mediated intestinal urate excretion has not been directly shown by human study. In end-stage renal disease (hemodialysis) patients whose SUA levels are extremely elevated9,10, renal urate excretion is nearly completely absent, and almost all urate excretion must depend on intestinal excretion via ABCG2. Thus, it was supposed that the degree of intestinal ABCG2 dysfunction strongly affects the severity of hyperuricemia in hemodialysis patients (Fig. 1), as was shown by multiple regression analysis in the present study (Table 2). This finding is the first evidence for a physiological role of ABCG2 on intestinal urate excretion in humans.
SUA, serum uric acid. ABCG2 physiologically mediates urate excretion in both intestine and kidney. In end-stage renal disease (renal failure) patients, renal urate excretion would be nearly eliminated with urate excretion depending almost entirely on intestinal excretion. Thus, the degree of intestinal ABCG2 dysfunction strongly affects the severity of hyperuricemia in renal diseases such as end-stage renal disease. On the other hand, in acute gastroenteritis patients, intestinal inflammation seriously impairs the intestinal urate excretion via ABCG2. Therefore, the degree of renal ABCG2 dysfunction markedly affects the severity of hyperuricemia in intestinal diseases such as acute gastroenteritis patients.
Besides the physiological role for intestinal urate excretion via ABCG2 in humans, we for the first time demonstrated that hyperuricemia in acute gastroenteritis patients is caused by decreased urate excretion in addition to dehydration which is generally considered to be a major cause of hyperuricemia in acute gastroenteritis patients13. Pathogens which cause acute gastroenteritis, such as rotaviruses, primarily infect the villus epithelium of the small intestine14,15,16,17. These viruses induce the destruction of infected intestinal epithelial cells, but they also mediate the down-regulation of the expression of absorptive enzymes, transporters and cytokines, which instigate malabsorption of D-xylose, lipid or lactose14,17,18. In acute gastroenteritis patients, intestinal inflammation would also seriously impair the function of intestinal urate excretion of ABCG2, which could be one of the reasons why SUA is markedly increased in acute gastroenteritis patients. Therefore, it is clearly possible that the degree of renal ABCG2 dysfunction affects the severity of hyperuricemia in gastroenteritis patients (Fig. 1), as was first shown by linear regression analysis in acute period gastroenteritis patients in the present study (Table 2).
The evaluation of intestinal urate excretion in humans is very difficult because urate excreted into the intestinal lumen is rapidly metabolized by bacterial flora. Thus, our previous study8 could reveal the importance of ABCG2 for intestinal urate excretion not using human, but rather Abcg2-knockout mice treated with oxonate, an uricase inhibitor. In addition, another study has also reported the decreased intestinal excretion and increased plasma concentration of uric acid in Abcg2-knockout mice19.
Taking into account the results from both hemodialysis and acute gastroenteritis patients in the present study, we for the first time demonstrated that ABCG2 mediates intestinal urate excretion in humans, which suggests the physiological importance of intestinal epithelium as an excretion pathway besides an absorption pathway. In addition, if an end-stage renal disease patient develops acute gastroenteritis, both renal and intestinal urate excretion via ABCG2 will extremely decrease, and thereby greatly elevate SUA.
In light of these findings, although further studies would be necessary because of the limited sample size in this study, we proposed a physiological model of urate excretion via ABCG2 in humans, and a pathophysiological model of hyperuricemia in intestinal and renal diseases (Fig. 1). Physiologically, ABCG2 mediates urate excretion in both intestine and kidney in humans. Pathophysiologically, in end-stage renal disease patients, the degree of intestinal ABCG2 dysfunction strongly affects the severity of hyperuricemia because urate excretion almost all depends on intestinal excretion via ABCG2. Contrarily, in acute gastroenteritis patients, the function of intestinal urate excretion via ABCG2 is severely impaired. Therefore, the degree of renal ABCG2 dysfunction clearly affects the severity of hyperuricemia. By this proposed model, physicians will recognize that increased SUA levels could be a useful marker not only for dehydration but also for intestinal impairment which induces urate export failure in intestines. Physicians could also consider “the urate excretion failure due to intestinal impairment” as one of the common causes of hyperuricemia which is often complicated in patients with acute gastroenteritis.
In summary, we revealed that two common dysfunctional variants (Q126X and Q141K) of ABCG2 have a significant negative effect on both intestinal and renal urate excretion in humans, and that intestinal and renal ABCG2 dysfunction markedly increases SUA in end-stage renal disease and acute gastroenteritis. These findings for the first time demonstrated the physiological and pathophysiological roles of ABCG2 on intestinal urate excretion in humans.
Methods
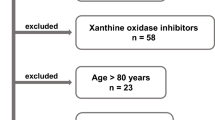
Participants
This study was approved by the institutional ethical committee of the National Defense Medical College, and all procedures were performed in accordance with the Declaration of Helsinki with written informed consent from each subject. When the participant was a minor, written informed consent was obtained from each parent or guardian of that participant. Degree of dehydration in acute gastroenteritis patients was evaluated by physicians (T. Tsunoda and T.S.) according to the criteria recommended by the Center for Disease Control (CDC)20, and classified as “minimal or no dehydration”, “mild to moderate dehydration”, and “severe dehydration”.
In order to clarify the physiological role of intestinal urate excretion via ABCG2, 106 maintenance hemodialysis patients not taking medications for hyperuricemia were assigned from among the outpatients at Ryougoku East Gate Clinic (Tokyo, Japan). Their SUA levels were measured three times just before each maintenance hemodialysis, and the average was used for analyses. In addition, 106 sex- and BMI-matched subjects were selected from health examination participants in the Shizuoka area in the Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study)21,22.
Sixty-seven pediatric patients with acute gastroenteritis were also recruited at the Department of Pediatric Hepatology and Gastroenterology in Saiseikai Yokohamashi Tobu Hospital (Yokohama, Japan). Their SUA levels were measured twice at the acute and recovery period of gastroenteritis.
The details of participants in this study are shown in Supplementary Table 3.
Genetic analysis and estimation of ABCG2 function
Genomic DNA was extracted from whole peripheral blood cells23. Genotyping of ABCG2 dysfunctional variants, Q126X (rs72552713) and Q141K (rs2231142), was performed using the TaqMan method (Life Technologies Corporation, Carlsbad, CA, USA) with a LightCycler 480 (Roche Diagnostics, Mannheim, Germany) as previously described24. Custom TaqMan assay probes were designed as follows: for Q126X, VIC-CCACTAATACTTACTTGTACCAC and FAM-CCACTAATACTTACTTATACCAC; for Q141K, VIC-CTGCTGAGAACTGTAAGTT and FAM-CTGCTGAGAACTTTAAGTT. To confirm their genotypes, DNA sequencing analysis was performed with the following primers: for Q126X, forward 5′-TGTACAATGAAAAGAGAAAGGTGAG-3′ and reverse 5′-CTGCCTTTTCACATAAGTGTC-3′; for Q141K, forward 5′-ATGGAGTTAACTGTCATTTGC-3′ and reverse 5′-CACGTTCATATTATGTAACAAGCC-3′. Direct sequencing was performed with a 3130xl Genetic Analyzer (Life Technologies Corporation)23,24.
We previously reported that Q126X is a nonfunctional variant, Q141K is a half-functional variant for urate excretion compared to the wild-type, and that there was no simultaneous presence of the minor alleles of Q126X and Q141K in one haplotype2, which is confirmed in the participants of the present study (Supplementary Table 1). Thus, three haplotypes were defined as *1 (126Q and 141Q), *2 (126Q and 141K) and *3 (126X and 141Q) as previously reported25, and all patients could be divided into the following ABCG2 functional groups: full function (*1/*1), 3/4 function (mild dysfunction, *1/*2), 1/2 function (moderate dysfunction, *1/*3 or *2/*2), and ≤1/4 function (severe dysfunction, *2/*3 or *3/*3)25 as shown in Table 1.
Statistical analysis
For all calculations in the statistical analysis, the software R (version 3.1.1) (http://www.r-project.org/) was used26. Comparison of SUA between the acute and recovery period of gastroenteritis was performed with a paired t-test using a two-tailed P value. Linear regression analysis was performed to test the hypothesis that there was no relation between ABCG2 dysfunction and SUA in the analysis of acute gastroenteritis patients. Multiple regression analysis including ABCG2 function and age in the model was used for the analysis of hemodialysis patients and sex- and BMI-matched health examination participants, because age could not be completely matched in the selection from health examination participants. The association between ABCG2 and dehydration was examined using the Cochran-Armitage trend test. Haplotype estimation was performed with the EM algorithm27 using the package haplo.stats of the software R. We set the significance threshold as α = 0.05.
Additional Information
How to cite this article: Matsuo, H. et al. Hyperuricemia in acute gastroenteritis is caused by decreased urate excretion via ABCG2. Sci. Rep. 6, 31003; doi: 10.1038/srep31003 (2016).
References
Feig, D. I., Kang, D. H. & Johnson, R. J. Uric acid and cardiovascular risk. N. Engl. J. Med. 359, 1811–1821 (2008).
Matsuo, H. et al. Common defects of ABCG2, a high-capacity urate exporter, cause gout: a function-based genetic analysis in a Japanese population. Sci. Transl. Med. 1, 5ra11 (2009).
Maliepaard, M. et al. Subcellular localization and distribution of the breast cancer resistance protein transporter in normal human tissues. Cancer Res. 61, 3458–3464 (2001).
Huls, M. et al. The breast cancer resistance protein transporter ABCG2 is expressed in the human kidney proximal tubule apical membrane. Kidney Int. 73, 220–225 (2008).
Woodward, O. M. et al. Identification of a urate transporter, ABCG2, with a common functional polymorphism causing gout. Proc. Natl. Acad. Sci. USA 106, 10338–10342 (2009).
Matsuo, H. et al. Common dysfunctional variants in ABCG2 are a major cause of early-onset gout. Sci. Rep. 3, 2014 (2013).
Nakayama, A. et al. Common dysfunctional variants of ABCG2 have stronger impact on hyperuricemia progression than typical environmental risk factors. Sci. Rep. 4, 5227 (2014).
Ichida, K. et al. Decreased extra-renal urate excretion is a common cause of hyperuricemia. Nat. Commun. 3, 764 (2012).
Krishnan, E. Chronic kidney disease and the risk of incident gout among middle-aged men: a seven-year prospective observational study. Arthritis Rheum. 65, 3271–3278 (2013).
Prasad Sah, O. S. & Qing, Y. X. Associations between hyperuricemia and chronic kidney disease: a review. Nephrourol Mon 7, e27233 (2015).
Sica, D. A. & Schoolwerth, A. In Brenner and Rector’s The Kidney (ed Brenner, B. M. ) 645–649 (Saunders, 2004).
Sorensen, L. B. Role of the intestinal tract in the elimination of uric acid. Arthritis Rheum. 8, 694–706 (1965).
Adler, R., Robinson, R., Pazdral, P. & Grushkin, C. Hyperuricemia in diarrheal dehydration. Am. J. Dis. Child. 136, 211–213 (1982).
Schreiber, D. S., Blacklow, N. R. & Trier, J. S. The mucosal lesion of the proximal small intestine in acute infectious nonbacterial gastroenteritis. N. Engl. J. Med. 288, 1318–1323 (1973).
Ciarlet, M., Conner, M. E., Finegold, M. J. & Estes, M. K. Group A rotavirus infection and age-dependent diarrheal disease in rats: a new animal model to study the pathophysiology of rotavirus infection. J. Virol. 76, 41–57 (2002).
Ramig, R. F. Pathogenesis of intestinal and systemic rotavirus infection. J. Virol. 78, 10213–10220 (2004).
Greenberg, H. B. & Estes, M. K. Rotaviruses: from pathogenesis to vaccination. Gastroenterol. 136, 1939–1951 (2009).
Karst, S. M., Zhu, S. & Goodfellow, I. G. The molecular pathology of noroviruses. J. Pathol. 235, 206–216 (2015).
Hosomi, A., Nakanishi, T., Fujita, T. & Tamai, I. Extra-renal elimination of uric acid via intestinal efflux transporter BCRP/ABCG2. PLoS One 7, e30456 (2012).
King, C. K., Glass, R., Bresee, J. S. & Duggan, C. Managing acute gastroenteritis among children: oral rehydration, maintenance, and nutritional therapy. MMWR Recomm. Rep. 52, 1–16 (2003).
Hamajima, N. & J-MICC Study Group. The Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study) to detect gene-environment interactions for cancer. Asian Pac. J. Cancer Prev. 8, 317–323 (2007).
Asai, Y. et al. Baseline data of Shizuoka area in the Japan Multi-Institutional Collaborative Cohort Study (J-MICC Study). Nagoya J. Med. Sci. 71, 137–144 (2009).
Sakiyama, M. et al. Common variant of leucine-rich repeat-containing 16A (LRRC16A) gene is associated with gout susceptibility. Hum. Cell 27, 1–4 (2014).
Sakiyama, M. et al. Ethnic differences in ATP-binding cassette transporter, sub-family G, member 2 (ABCG2/BCRP): Genotype combinations and estimated functions. Drug Metab. Pharmacokinet. 29, 490–492 (2014).
Matsuo, H. et al. ABCG2 dysfunction causes hyperuricemia due to both renal urate underexcretion and renal urate overload. Sci. Rep. 4, 3755 (2014).
R: A language and environment for statistical computing. (R. Foundation for Statistical Computing, Vienna, 2014).
Kitamura, Y. et al. Determination of probability distribution of diplotype configuration (diplotype distribution) for each subject from genotypic data using the EM algorithm. Ann. Hum. Genet. 66, 183–193 (2002).
Acknowledgements
The authors are deeply grateful to all of the individuals who participated in this study. We are also indebted to K. Gotanda, Y. Morimoto, M. Miyazawa, S. Shimizu, T. Chiba, Y. Kawamura, T. Nakamura, H. Nakashima and Y. Sakurai of the National Defense Medical College for their genetic analysis and valuable discussions, and to A. Tokumasu of the Ryougoku East Gate Clinic, and M. Naito and N. Hamajima of the Nagoya University Graduate School of Medicine, for sample collection. This work was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan including the MEXT KAKENHI (Grant numbers 221S0001, 221S0002, 25293145, 26461244, and 15K15227), the Ministry of Health, Labour and Welfare of Japan, the Ministry of Defense of Japan, the Gout Research Foundation of Japan and the Kawano Masanori Memorial Foundation for Promotion of Pediatrics.
Author information
Authors and Affiliations
Contributions
H.M., T. Tsunoda, K.O. and M.S. conceived and designed this study. H.M., T. Tsunoda, K.O., M.S., T.S., K.W., H.O., A.I. and S.F. collected samples and analyzed clinical data. H.M., M.S., A. Nakayama, M.K. and T.H. performed genetic analysis. H.M. and M.S. performed statistical analyses. A. Nakashima, T. Takada, R.H., H.S., K.I., A.I., S.F. and N.S. provided intellectual input and assisted with the preparation of the manuscript. H.M., T. Tsunoda, K.O. and M.S. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
Yes, there is potential competing interest: H.M., T. Takada, K.I. and N.S. have a patent pending based on the work reported in this paper. Other authors have declared that no competing interests exist.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Matsuo, H., Tsunoda, T., Ooyama, K. et al. Hyperuricemia in acute gastroenteritis is caused by decreased urate excretion via ABCG2. Sci Rep 6, 31003 (2016). https://doi.org/10.1038/srep31003
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep31003
This article is cited by
-
Evaluation of ABCG2-mediated extra-renal urate excretion in hemodialysis patients
Scientific Reports (2023)
-
From purines to purinergic signalling: molecular functions and human diseases
Signal Transduction and Targeted Therapy (2021)
-
Multidrug efflux transporter ABCG2: expression and regulation
Cellular and Molecular Life Sciences (2021)
-
Increase of serum uric acid levels associated with APOE ε2 haplotype: a clinico-genetic investigation and in vivo approach
Human Cell (2021)
-
Dysfunctional ABCG2 gene polymorphisms are associated with serum uric acid levels and all-cause mortality in hemodialysis patients
Human Cell (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.