Abstract
The prognostic value of forkhead box protein P1 (FOXP1) protein expression in tumors remains controversial. Therefore, we conducted a systematic review and meta-analysis, searching the PubMed, Embase and Web of Science databases to identify eligible studies. In total, we analyzed 22 articles that examined 9 tumor types and included 2468 patients. Overall, decreased expression of FOXP1 protein was associated with favorable overall survival (OS) in lymphoma patients (HR = 0.38, 95%CI: 0.30–0.48, p < 0.001). In patients with solid tumors, decreased FOXP1 expression correlated with unfavorable OS (HR = 1.82, 95%CI: 1.18–2.83, p = 0.007). However, when FOXP1 protein expression was nuclear, decreased expression was also associated with favorable OS (HR = 0.53, 95%CI: 0.32–0.86, p = 0.011). Furthermore, decreased FOXP1 expression resulted in the best OS in patients with mucosa-associated lymphoid tissue (MALT) lymphomas (HR = 0.26, 95%CI: 0.11–0.59, p = 0.001), but the worst OS was observed in non-small cell lung cancer (NSCLC) patients (HR = 3.11, 95%CI: 1.87–5.17, p < 0.001). In addition, decreased FOXP1 expression was significantly correlated with an unfavorable relapse-free survival (RFS) in breast cancer patients (HR = 1.93, 95%CI: 1.33–2.80, p = 0.001).
Similar content being viewed by others
Introduction
Forkhead box protein P1 (FOXP1) is a protein encoded by the FOXP1 gene1 that belongs to the forkhead box transcription factor family2. Functioning as a transcriptional repressor, FOXP1 regulates a program of gene repression that is essential for myocardial development3. In addition, FOXP1 is also a crucial regulator in the development of the lung, esophagus, cortical neuron, hair follicle and jaw tissues4,5,6,7,8.
Aside from a critical role in regulating the development of normal human tissues, FOXP1 is also involved in tumorigenesis. In diffuse large B-cell lymphomas (DLBCL), FOXP1 suppresses immune response signatures and promotes tumor cell survival to act as an oncoprotein9,10. However, in other types of tumors, such as neuroblastoma and prostate cancer, FOXP1 can inhibit cell growth and attenuate tumorigenicity to exert a tumor-suppressive effect11,12. Thus, the function of FOXP1 in tumor development and progression is inconsistent.
Similarly, this contradiction is also demonstrated in the prognostic value of FOXP1 protein expression in tumor patients. Decreased FOXP1 protein expression in DLBCL or mucosa-associated lymphoid tissue (MALT) lymphoma patients is associated with favorable survival13,14,15. However, in patients with breast, endometrial or non-small cell lung cancer (NSCLC), the decreased FOXP1 expression is correlated with poor survival16,17,18. Therefore, we carried out this systematic review and meta-analysis to explore the cause of these inconsistent observations and determine the prognostic value of decreased FOXP1 protein in patients with various tumors.
Methods
This systematic review and meta-analysis was conducted according to the PRISMA statement19.
Search strategy
We systematically searched in the online PubMed, Embase and Web of Science databases (updated until May 6, 2016) with the restrictions of English language and article format. The following keywords or their combinations were used in the searches: “FOXP1 OR forkhead box protein 1” AND “survival OR prognosis OR prognostic” AND “cancer OR tumor OR tumour OR neoplasm OR neoplasma OR neoplasia OR carcinoma OR cancers OR tumors OR tumours OR neoplasms OR neoplasmas OR neoplasias OR carcinomas OR leukemia OR leukemias OR leukaemia OR leukaemias OR lymphoma OR lymphomas”. Additional studies were identified by referring to relevant articles to avoid omissions due to electronic searching.
Study selection criteria
Eligible studies in our meta-analysis were selected according to the following criteria: (1) full text original studies published in English that measured the FOXP1 protein expression in patients with tumors without restricting the type of cancer; (2) the protein expression was determined by immunohistochemistry (IHC); (3) results included the determination of a correlation between FOXP1 expression and patient survival; (4) the hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs) were either reported or calculated using other information (e.g., survival curves); and (5) when repeated results were reported by the same authors, we included the most complete report. However, patient survival outcomes in this meta-analysis included overall survival (OS), cancer-specific survival (CSS), relapse-free survival (RFS), progression-free survival (PFS), disease-free survival (DFS) and failure-free survival (FFS, which was defined as in Nyman’s study20 that evaluated survival from the date of diagnosis until relapse or death of any cause). Additionally, unpublished studies, meeting abstracts, comments, letters, case reports, literature reviews and meta-analyses were excluded.
Quality assessment
In correspondence to a critical review checklist that was proposed by Meta-analysis of Observational Studies in Epidemiology (MOOSE) group issued by Dutch Cochrane Centre21 and referencing Zhou’s study22, we used the following quality control criteria: (1) specific definition of study population; (2) specific description of study design; (3) sample size greater than 30; (4) specific definition of survival outcome such as OS, CSS, RFS, PFS, DFS and FFS; (5) specific definition of the cut-off value for decreased FOXP1 protein expression; and (6) sufficient follow-up time.
Data extraction
Two investigators (Jian Xiao and Bixiu He) independently extracted the primary information according to a predefined form, which included the following sub-categories: first author, year of publication, country of study population, tumor type, sample source, test method, location of FOXP1 protein expression, cut-off value, sample size, follow-up time, survival outcome, analysis method and HR estimation. When both multivariate and univariate analyses of the OS results were performed, HRs and their corresponding 95%CIs were extracted preferentially from the multivariate analyses. If HR and its corresponding 95%CI were not directly reported, they were calculated and estimated using the previously reported methods23. All disagreements were discussed until a consensus was reached.
Statistical analysis
We used STATA 12.0 software (Stata Corporation, College Station, TX, USA) to perform all of the statistical analyses. The extracted HRs and their corresponding 95%CIs were comprehensively calculated to obtain pooled HRs and 95%CIs. If the pooled HR > 1 as well as its 95%CI did not overlap with 1, the decreased expression of the FOXP1 protein would be considered as an indicator for the poor survival prognosis in tumor patients. Analysis of the heterogeneity of the combined HRs was carried out using Cochran’s Q test and Higgins’ I-squared statistic. Heterogeneity was defined as I2 > 50% or p < 0.05. If heterogeneity was present, a random-effects model was conducted. If not, the fixed-effects model would be applied. Sensitivity analysis was performed to assess the stability of the results. Furthermore, subgroup analysis and meta-regression were adopted to explore the sources of the heterogeneity. In addition, the publication bias was evaluated by Begg’s and Egger’s tests. However, all of the p values in our results were two-tailed, and p < 0.05 was considered to be statistically significant.
Results
Study selection
The initial database searching identified one hundred and fifty-three potentially relevant records. After the duplicates were removed, fifty-seven records remained. By assessing the full text for eligibility, thirty-five of these studies were excluded because they did not conform to the selection criteria. However, one additional study that also met our selection criteria was obtained from the references of relevant articles. Thus, a total of twenty-two studies were included in this systematic review. Finally, thirty-one datasets were used to perform the meta-analysis (Fig. 1).
Characteristics of the included studies
The characteristics of the 22 included studies are summarized in Tables 1 and 2. In total, 2468 tumor patients from 9 different countries were included in our meta-analysis, and the studies were published from 2004 to 2015. The tumor types contained are as follows: DLBCL13,14,15,20,24,25,26,27,28,29, breast cancer16,30,31, endometrial cancer17, MALT lymphoma14,32,33,34, hepatocellular carcinoma35, NSCLC18, prostate cancer12, colorectal cancer36 and epithelial ovarian cancer37. As for the survival outcomes, 22 eligible studies were divided into 31 datasets: 20 for OS, 4 for PFS, 3 for RFS, 2 for DFS, 1 for CSS and 1 for FFS (Table 1 and Fig. 1). However, the cut-off value for the decreased expression of FOXP1 protein was inconsistent among these eligible studies (Table 2).
Meta-analysis of OS
The pooled result from twenty datasets yielded no significant association between decreased FOXP1 protein expression and OS in patients with various tumors (HR = 0.75, 95%CI: 0.48–1.17, p = 0.203) (Table 3 and Fig. 2). A sensitivity analysis was performed by successively omitting each study, and the results revealed the pooled HRs did not vary substantially after excluding any individual study (Fig. 3), which implied that the pooled OS HR was stable. However, in the subgroup analyses based on cancer type (which included DLBCL and MALT lymphoma) and solid tumors (which excluded DLBCL and MALT lymphoma), the pooled results demonstrated that decreased FOXP1 expression had a favorable prognostic value for lymphomas (HR = 0.38, 95%CI: 0.30–0.48, p < 0.001) but an unfavorable prognosis for solid tumors (HR = 1.82, 95%CI: 1.18–2.83, p = 0.007) (Figs 4 and 5). Furthermore, when the FOXP1 protein was expressed in the nucleus, decreased FOXP1 expression indicated a good prognosis for OS (HR = 0.53, 95%CI: 0.32–0.86, p = 0.011) (Table 3).
It is interesting that decreased expression of FOXP1 had different prognostic values for lymphomas and solid tumors. To reveal this contradictory phenomenon, we further conducted subgroup analyses for both of these cancer types. As shown in Table 4 for the subgroup analyses results for lymphomas, decreased FOXP1 expression had the best OS in patients with MALT lymphoma (HR = 0.26, 95%CI: 0.11–0.59, p = 0.001). However, decreased FOXP1 protein expression in patients with solid tumors was associated with a significantly worse OS in most of the subgroup categories, and the worst OS was observed in NSCLC patients (HR = 3.11, 95%CI: 1.87–5.17, p < 0.001) (Table 5).
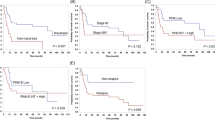
Meta-analysis of CSS/DFS/FFS/PFS/RFS
Both the CSS for prostate cancer and the FFS for DLBCL were derived from only one dataset and neither showed significant associations with the decreased FOXP1 protein expression (HR = 2.51, 95%CI: 0.92–6.83, p = 0.071; HR = 0.71, 95%CI: 0.26–1.94, p = 0.504, respectively). The pooled results from two datasets for the DFS for DLBCL and four datasets for the PFS for DLBCL and colorectal cancer also indicated no statistical significance (HR = 0.43, 95%CI: 0.15–1.25, p = 0.120; HR = 0.57, 95%CI: 0.29–1.13, p = 0.107, respectively). However, in patients with breast cancer, the pooled result of three datasets showed that decreased FOXP1 expression was significantly correlated with an unfavorable RFS (HR = 1.93, 95%CI: 1.33–2.80, p = 0.001) (Fig. 6).
Meta-regression analysis of OS
To investigate the source of heterogeneity among OS datasets (I2 = 84.1%, p < 0.001), we performed meta-regression analyses by choosing variables such as publication year, country, cancer type, sample source, expression location, sample size and analysis method. The results suggested that cancer type (residual I2 = 6.26%, adjusted R2 = 100.00%) and expression location (residual I2 = 80.68%, adjusted R2 = 24.29%) were the major sources of significant heterogeneity among datasets regarding OS (Supplementary Table S1). Consequently, as cancer type can almost completely explain the heterogeneity among OS datasets, the subgroup analyses for it showed that the heterogeneities were much lower (Tables 3, 4, 5).
Publication bias
As the amount of datasets for meta-analysis of CSS/DFS/FFS/PFS/RFS were fewer (each of them were less than five), we only evaluated the publication bias for the OS meta-analysis. However, both Begg’s funnel plot and Egger’s linear regression test were used to evaluate the publication bias. The results indicated that no publication bias in all of the OS datasets for all tumor types (p = 0.347 for Begg’s test and p = 0.275 for Egger’s test). Publication bias also did not exist in the datasets regarding the OS for lymphomas (p = 0.213 for Begg’s test and p = 0.291 for Egger’s test) or solid tumors (p = 0.602 for Begg’s test and p = 0.864 for Egger’s test) (Fig. 7).
(a) Begg’s funnel plot of publication bias for meta-analysis of OS in all tumor patients included in this study; (b) Begg’s funnel plot of publication bias for meta-analysis of OS in patients with lymphomas; (c) Begg’s funnel plot of publication bias for meta-analysis of OS in patients with solid tumors.
Discussion
FOXP1 plays an important role during pathologic tumor development by potentiating Wnt/β-catenin signaling in DLBCL38. By repressing S1PR2 signaling, FOXP1 also promotes the survival of DLBCL cells10. In addition, FOXP1 negatively regulates androgen receptor signaling in prostate cancer to function as an androgen-responsive transcription factor39. Furthermore, FOXP1 still serves as an oncogene through promoting the cancer stem cell-like characteristics of ovarian cancer cells40. All of these observations indicate that the FOXP1 protein may have a specific prognostic value for tumor patients. However, thus far, no consistent conclusion has been made14,15,16,18.To the best of our knowledge, this is the first meta-analysis examining the prognostic value of decreased FOXP1 protein in various tumors.
Our meta-analysis incorporated 22 eligible studies with 31 datasets. The survival data included OS, PFS, RFS, DFS, CSS and FFS. First, we found no significant association between decreased FOXP1 protein expression and OS in patients with various tumors. When the subgroup analyses were conducted, the pooled results demonstrated that decreased FOXP1 expression was a favorable prognostic factor for lymphomas but an unfavorable factor for solid tumors. However, if the FOXP1 protein expression was located in the nucleus, decreased FOXP1 expression indicated a good OS prognosis. Furthermore, the results showed that decreased FOXP1 expression was correlated with the best OS in patients with MALT lymphoma but associated with the worst OS in NSCLC patients. Additionally, in patients with solid tumors such as breast cancer, decreased FOXP1 expression was also significantly correlated with an unfavorable RFS. It should be noted that no publication bias was found in this meta-analysis.
Several important implications were confirmed by our study. First, decreased FOXP1 protein expression may be a universal favorable prognostic factor for lymphomas. In this meta-analysis, we included the lymphoma type, such as DLBCL13,14,15,20,24,25,26,27,28,29 and MALT lymphoma14,32,33,34, and the results were also confirmed by studies with chronic lymphocytic leukemia41. Thus, we speculate that decreased FOXP1 protein expression may have similar prognostic value for all types of lymphoma that originate from lymphocytes. Second, decreased expression of FOXP1 is an unfavorable factor for solid tumors. As the meta-analysis results were pooled from breast cancer16,30,31, endometrial cancer17, hepatocellular carcinoma35, NSCLC18, prostate cancer12, colorectal cancer36 and epithelial ovarian cancer37, and combined with further evidence from neuroblastoma11, we considered that this finding may be applicable to all solid tumors. Third, FOXP1 protein may function as a tumor promoter in lymphomas and act as a tumor suppressor in solid tumors. However, further research into these mechanisms is needed to verify this inference. Additionally, solid tumor patients with decreased FOXP1 protein expression in tumor tissues may indicate sensitivity to chemotherapy. Studies in vitro found that down-regulated FOXP1 expression can improve the sensitivity to chemotherapy in tumor cells37,40,42. Thus, we speculate that these situations may also occur in patients with solid tumors. However, more in vivo experiments are needed to confirm our speculation.
In this meta-analysis, we wanted to study the prognostic value of decreased FOXP1 protein expression in various tumors. However, we did not comprehensively evaluate the prognostic impact of overexpressed FOXP1 protein in the tumor patients. The major reason for this is that all of the eligible studies included in our study had defined decreased FOXP1 expression (Table 2), whereas relatively few studies15,18,35,36 had reported an association between the overexpression of FOXP1 and survival outcome in tumor patients. Therefore, to highlight the key point of decreased FOXP1 expression, we only focused on the prognostic value of decreased FOXP1 protein expression in our current meta-analysis. However, as more original studies regarding the association between the overexpression of FOXP1 and survival outcomes in tumor patients will be conducted, a systematic study on the prognostic value of overexpressed FOXP1 protein in tumor patients can also be performed in the future.
There are some limitations that should be noted in our meta-analysis. The tumor types for both lymphomas and solid tumors included in this meta-analysis are limited, and our results should be cautiously extended to other specific tumor types. We only recruited articles published in English, thus a language bias might exist. Some HRs and their corresponding 95%CIs were extracted from the survival curves. However, these data are less reliable than those directly obtained from survival data. Because of the lack of data, the meta-analysis results regarding the CSS/DFS/FFS/PFS/RFS should be updated when more related studies are completed. Finally, studies regarding various tumors without a consistent cut-off value may be restricted to expand the clinical applicability43,44,45,46. Therefore, a unified cut-off value for the decreased FOXP1 protein is warranted.
In summary, our meta-analysis suggests that decreased expression of the FOXP1 protein is associated with better survival in patients with lymphomas but poorer survival in patients with solid tumors. However, further prospective studies with larger sample sizes are required to validate the prognostic value of decreased FOXP1 expression in various tumors.
Additional Information
How to cite this article: Xiao, J. et al. Prognostic value of decreased FOXP1 protein expression in various tumors: a systematic review and meta-analysis. Sci. Rep. 6, 30437; doi: 10.1038/srep30437 (2016).
References
Shu, W., Yang, H., Zhang, L., Lu, M. M. & Morrisey, E. E. Characterization of a new subfamily of winged-helix/forkhead (Fox) genes that are expressed in the lung and act as transcriptional repressors. J Biol Chem 276, 27488–27497 (2001).
Katoh, M. & Katoh, M. Human FOX gene family (Review). Int J Oncol 25, 1495–1500 (2004).
Jepsen, K., Gleiberman, A. S., Shi, C., Simon, D. I. & Rosenfeld, M. G. Cooperative regulation in development by SMRT and FOXP1. Genes Dev 22, 740–745 (2008).
Li, S. et al. Foxp1/4 control epithelial cell fate during lung development and regeneration through regulation of anterior gradient 2. Development 139, 2500–2509 (2012).
Shu, W. et al. Foxp2 and Foxp1 cooperatively regulate lung and esophagus development. Development 134, 1991–2000 (2007).
Li, X. et al. Foxp1 regulates cortical radial migration and neuronal morphogenesis in developing cerebral cortex. PLoS One 10, e0127671 (2015).
Zhao, J. et al. Foxp1 Regulates the Proliferation of Hair Follicle Stem Cells in Response to Oxidative Stress during Hair Cycling. PLoS One 10, e0131674 (2015).
Cesario, J. M., Almaidhan, A. A. & Jeong, J. Expression of forkhead box transcription factor genes Foxp1 and Foxp2 during jaw development. Gene Expr Patterns (2016).
Brown, P. J. et al. FOXP1 suppresses immune response signatures and MHC class II expression in activated B-cell-like diffuse large B-cell lymphomas. Leukemia 30, 605–616 (2016).
Flori, M. et al. The hematopoietic oncoprotein FOXP1 promotes tumor cell survival in diffuse large B-cell lymphoma by repressing S1PR2 signaling. Blood 127, 1438–1448 (2016).
Ackermann, S. et al. FOXP1 inhibits cell growth and attenuates tumorigenicity of neuroblastoma. BMC Cancer 14, 840 (2014).
Takayama, K. et al. Integrative analysis of FOXP1 function reveals a tumor-suppressive effect in prostate cancer. Mol Endocrinol 28, 2012–2024 (2014).
Yu, B. et al. FOXP1 expression and its clinicopathologic significance in nodal and extranodal diffuse large B-cell lymphoma. Ann Hematol 90, 701–708 (2011).
He, M. et al. Prognostic significance of miR-34a and its target proteins of FOXP1, p53, and BCL2 in gastric MALT lymphoma and DLBCL. Gastric Cancer 17, 431–441 (2014).
Barrans, S. L., Fenton, J. A., Banham, A., Owen, R. G. & Jack, A. S. Strong expression of FOXP1 identifies a distinct subset of diffuse large B-cell lymphoma (DLBCL) patients with poor outcome. Blood 104, 2933–2935 (2004).
Rayoo, M. et al. Expression of the forkhead box transcription factor FOXP1 is associated with oestrogen receptor alpha, oestrogen receptor beta and improved survival in familial breast cancers. J Clin Pathol 62, 896–902 (2009).
Giatromanolaki, A. et al. Loss of expression and nuclear/cytoplasmic localization of the FOXP1 forkhead transcription factor are common events in early endometrial cancer: relationship with estrogen receptors and HIF-1alpha expression. Mod Pathol 19, 9–16 (2006).
Feng, J. et al. High expression of FoxP1 is associated with improved survival in patients with non-small cell lung cancer. Am J Clin Pathol 138, 230–235 (2012).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6, e1000100 (2009).
Nyman, H. et al. Bcl-2 but not FOXP1, is an adverse risk factor in immunochemotherapy-treated non-germinal center diffuse large B-cell lymphomas. Eur J Haematol 82, 364–372 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 (2000).
Zhou, L. et al. Prognostic Role of C-Reactive Protein In Urological Cancers: A Meta-Analysis. Sci Rep 5, 12733 (2015).
Krieg, A., Riemer, J. C., Telan, L. A., Gabbert, H. E. & Knoefel, W. T. CXCR4–A Prognostic and Clinicopathological Biomarker for Pancreatic Ductal Adenocarcinoma: A Meta-Analysis. PLoS One 10, e0130192 (2015).
Banham, A. H. et al. Expression of the FOXP1 transcription factor is strongly associated with inferior survival in patients with diffuse large B-cell lymphoma. Clin Cancer Res 11, 1065–1072 (2005).
Sagaert, X. et al. Forkhead box protein P1 expression in mucosa-associated lymphoid tissue lymphomas predicts poor prognosis and transformation to diffuse large B-cell lymphoma. J Clin Oncol 24, 2490–2497 (2006).
Hoeller, S., Schneider, A., Haralambieva, E., Dirnhofer, S. & Tzankov, A. FOXP1 protein overexpression is associated with inferior outcome in nodal diffuse large B-cell lymphomas with non-germinal centre phenotype, independent of gains and structural aberrations at 3p14.1. Histopathology 57, 73–80 (2010).
Hu, C. R., Wang, J. H., Wang, R., Sun, Q. & Chen, L. B. Both FOXP1 and p65 expression are adverse risk factors in diffuse large B-cell lymphoma: a retrospective study in China. Acta Histochem 115, 137–143 (2013).
Wong, K. K. et al. Reciprocal expression of the endocytic protein HIP1R and its repressor FOXP1 predicts outcome in R-CHOP-treated diffuse large B-cell lymphoma patients. Leukemia 28, 362–372 (2014).
Tzankov, A. et al. Multiparameter analysis of homogeneously R-CHOP-treated diffuse large B cell lymphomas identifies CD5 and FOXP1 as relevant prognostic biomarkers: report of the prospective SAKK 38/07 study. J Hematol Oncol 8, 70 (2015).
Fox, S. B. et al. Expression of the forkhead transcription factor FOXP1 is associated with estrogen receptor alpha and improved survival in primary human breast carcinomas. Clin Cancer Res 10, 3521–3527 (2004).
Ijichi, N. et al. Association of double-positive FOXA1 and FOXP1 immunoreactivities with favorable prognosis of tamoxifen-treated breast cancer patients. Horm Cancer 3, 147–159 (2012).
Han, S. L. et al. FOXP1 expression predicts polymorphic histology and poor prognosis in gastric mucosa-associated lymphoid tissue lymphomas. Dig Surg 26, 156–162 (2009).
Zhai, L. et al. Expression of PIK3CA and FOXP1 in gastric and intestinal non-Hodgkin’s lymphoma of mucosa-associated lymphoid tissue type. Tumour Biol 32, 913–920 (2011).
Jiang, W. et al. Expression of FOXP1 in mucosa-associated lymphoid tissue lymphoma suggests a large tumor cell transformation and predicts a poorer prognosis in the positive thyroid patients. Med Oncol 29, 3352–3359 (2012).
Zhang, Y. et al. Prognostic significance of FOXP1 as an oncogene in hepatocellular carcinoma. J Clin Pathol 65, 528–533 (2012).
De Smedt, L. et al. Expression of FOXP1 and Colorectal Cancer Prognosis. Lab Med 46, 299–311 (2015).
Hu, Z. et al. Expression of FOXP1 in epithelial ovarian cancer (EOC) and its correlation with chemotherapy resistance and prognosis. Tumour Biol 36, 7269–7275 (2015).
Walker, M. P. et al. FOXP1 potentiates Wnt/beta-catenin signaling in diffuse large B cell lymphoma. Sci Signal 8 , ra12 (2015).
Takayama, K. et al. FOXP1 is an androgen-responsive transcription factor that negatively regulates androgen receptor signaling in prostate cancer cells. Biochem Biophys Res Commun 374, 388–393 (2008).
Choi, E. J. et al. FOXP1 functions as an oncogene in promoting cancer stem cell-like characteristics in ovarian cancer cells. Oncotarget 7, 3506–3519 (2016).
Mraz, M. et al. miR-150 influences B-cell receptor signaling in chronic lymphocytic leukemia by regulating expression of GAB1 and FOXP1. Blood 124, 84–95 (2014).
van Boxtel, R. et al. FOXP1 acts through a negative feedback loop to suppress FOXO-induced apoptosis. Cell Death Differ 20, 1219–1229 (2013).
Li, J. et al. Prognostic Value of Ezrin in Various Cancers: A Systematic Review and Updated Meta-analysis. Sci Rep 5, 17903 (2015).
Qi, X. W. et al. Wilms’ tumor 1 (WT1) expression and prognosis in solid cancer patients: a systematic review and meta-analysis. Sci Rep 5, 8924 (2015).
Zhang, J. et al. Prognostic value of pretreatment serum lactate dehydrogenase level in patients with solid tumors: a systematic review and meta-analysis. Sci Rep 5, 9800 (2015).
Wu, P. et al. Prognostic role of STAT3 in solid tumors: a systematic review and meta-analysis. Oncotarget (2016).
Acknowledgements
This work was supported by funding from the National Natural Science Foundation of China (Grant No. 81572284) and the important research and development plan of Hunan Provincial Science and Technology Department (Grant No. 2015SK20662)
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: Q.C. and J.X.; Eligible study collection, quality assessment and data extraction: B.H. and J.X.; Statistical analyses: Y.Z., X.C., X.L. and J.X.; Preparation of tables and figures: J.X., M.X. and W.L.; Contributed material/analysis tools: Y.Z., S.H. and S.Y.; Wrote and revised the manuscript: J.X. and Q.C.; All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Xiao, J., He, B., Zou, Y. et al. Prognostic value of decreased FOXP1 protein expression in various tumors: a systematic review and meta-analysis. Sci Rep 6, 30437 (2016). https://doi.org/10.1038/srep30437
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep30437
This article is cited by
-
Identification of FOXP1 as a favorable prognostic biomarker and tumor suppressor in intrahepatic cholangiocarcinoma
BMC Cancer (2024)
-
Immunohistochemistry technique for effect of gold nanoparticles, laser, and photodynamic therapy on FoxP1 level in infected mice with mammary adenocarcinoma
Lasers in Medical Science (2023)
-
Comprehensive Analysis of Prognostic and immune infiltrates for FOXPs Transcription Factors in Human Breast Cancer
Scientific Reports (2022)
-
Prognostic Significance of FOXC1 in Various Cancers: A Systematic Review and Meta-Analysis
Molecular Diagnosis & Therapy (2019)
-
Cytoplasmic FOXP1 expression is correlated with ER and calpain II expression and predicts a poor outcome in breast cancer
Diagnostic Pathology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.