Abstract
Minimal residual disease (MRD) enables reliable assessment of risk in acute lymphoblastic leukemia (ALL). However, little is known on association between MRD status and germline genetic variation. We examined 159 Caucasian (Slavic) patients with pediatric ALL, treated according to ALL-IC-BFM 2002/2009 protocols, in search for association between 23 germline polymorphisms and MRD status at day 15, day 33 and week 12, with adjustment for MRD-associated clinical covariates. Three variants were significantly associated with MRD: rs1544410 in VDR (MRD-day15); rs1051266 in RFC (MRD-day33, MRD-week12), independently and in an additive effect with rs10519613 in IL15 (MRD-day33). The risk alleles for MRD-positivity were: A allele of VDR (OR = 2.37, 95%CI = 1.07–5.21, P = 0.03, MRD-day15); A of RFC (OR = 1.93, 95%CI = 1.05–3.52, P = 0.03, MRD-day33 and MRD-week12, P < 0.01); A of IL15 (OR = 2.30, 95%CI = 1.02–5.18, P = 0.04, MRD-day33). The risk for MRD-day33-positive status was higher in patients with risk alleles in both RFC and IL15 loci than in patients with risk alleles in one locus or no risk alleles: 2 vs. 1 (OR = 3.94, 95% CI = 1.28–12.11, P = 0.024), 2 vs. 0 (OR = 6.75, 95% CI = 1.61–28.39, P = 0.012). Germline variation in genes related to pharmacokinetics/pharmacodynamics of anti-leukemic drugs and to anti-tumor immunity of the host is associated with MRD status and might help improve risk assessment in ALL.
Similar content being viewed by others
Introduction
Acute lymphoblastic leukemia (ALL), the most common pediatric cancer accounting for approximately 30% of all childhood neoplasms, is also one of the most successfully treated malignancies in children1. With current treatment protocols, based on the multi-agent chemotherapy, approximately 85% of patients reach a long-term remission2. These relatively high cure rates have been reached through the continuous advancement of therapeutic regimens, introduction of more efficient chemotherapeutic drugs, and treatment diversification in the risk-stratified patient groups.
Quantitative assessment of the level of residual leukemic cells (minimal residual disease, MRD) in patients undergoing treatment for ALL is an important indicator of the efficiency of a therapy. Several clinical studies carried out in the late 1990s demonstrated that monitoring MRD during the first three months of treatment holds the most prognostic value for risk assessment in pediatric ALL; generally, the presence of residual leukemic cells at the specified time points is associated with inferior survival3,4,5. Thus, monitoring MRD allows classification of patients into risk groups, and consequently adjustment of the intensity of the therapy. Incorporation of molecular or flow cytometry-based monitoring of MRD into treatment protocols significantly improved the outcome of pediatric ALL patients6,7. Despite the discovery of novel promising prognostic factors, such as CRLF2 expression or IKZF1 deletions/mutations, monitoring MRD remains the most reliable indicator of the treatment efficacy in ALL8,9.
The reduction of a tumor load (which corresponds to the decreasing level of MRD) in ALL patients undergoing therapy depends both on tumor-related factors (characteristics of the leukemic cells) and on constitutive host-related factors, such as germline polymorphisms in genes involved in transport, metabolism and detoxification of chemotherapeutic agents. The vast majority of pharmacogenetics studies in ALL, searching for association of polymorphic variants with the response to the treatment, have been based on the outcome assessed through survival estimates such as EFS (event free survival) or OS (overall survival)10,11,12,13,14. MRD status, being assessed during the realization of a therapeutic protocol, provides a direct insight into the treatment efficacy. The use of MRD status as an indicator of the treatment response enables rapid assessment of the prognostic potential of genetic polymorphisms in association studies, with no need for a long-term follow-up that is necessary when such studies are based on survival analysis15.
However, very few papers have been published so far on the relation of genetic variation to MRD as a measure of the therapy outcome in ALL16,17,18. In the scarce published studies, MRD levels have been estimated at slightly different time points of the therapeutic regimen. In addition, most of these studies have been performed in groups of patients of diverse ethnic composition and/or treated with various protocols. Since all these factors are crucial for pharmacogenetics association studies, the results of these analyses are not fully comparable.
Here we present the findings of the search for association between the MRD status and 23 germline variants, 20 localized in genes and 3 in intergenic regions. The study was performed in a group of 159 patients diagnosed with pediatric B-cell precursor ALL (BCP-ALL) and treated according to ALL IC-BFM protocols (2002 or 2009). Importantly, the group of patients was ethnically uniform (all were Caucasian of Slavic origin), and MRD was assessed, by flow cytometry (FC) and/or real-time polymerase chain reaction (RQ-PCR), at three uniformly chosen time points after the beginning of treatment.
Methods
Patients
The study group consisted of 174 patients with pediatric BCP-ALL, diagnosed between June 2006 and August 2012; the median follow-up time was 3 years at the time of analyses. The criteria for inclusion into the study were: availability of a biological material (blood, bone marrow aspirates) for genotyping of polymorphic loci, and availability of MRD data at day 15 (early assessment of the response to the remission induction), day 33 (assessment at the end of the remission induction), and week 12 (assessment before the beginning of the consolidation treatment). It has to be noted that, for the majority of Polish patients admitted to the clinics between 2006 and 2012, assessment of MRD was not obligatory during ALL treatment procedure. Since the availability of MRD data was a key inclusion criterion in our study, the study group did not consist of the consecutive patients.
The patients were treated according to ALL IC-BFM 2002 protocol (146 patients; 83.9%) or according to ALL IC-BFM 2009 protocol (28 patients; 16.1%)19. In the 2002 protocol, classification of patients into the risk group was based solely on clinical and genetic features identified at diagnosis and during the early phase of treatment (remission induction). In the 2009 protocol, these prognostic features were retained, but the flow cytometry (FC)-based assessment of MRD at day 15 was added as an obligatory element of the procedure, and used as one of the criteria in the risk group classification performed after day 33.
With the treatment scheme for the remission induction remaining unchanged until day 33, the data on MRD at day 15 and at day 33 from patients treated according to either of the two protocols could be included in the association analysis. On the other hand, six patients out of the 28 treated according to the 2009 protocol had to be excluded from the analysis of association with the MRD status at week 12. These were patients classified into the high risk group and thus, unlike in the 2002 protocol, receiving augmented protocol IB after day 33 (in Poland the augmented protocol is only administrated to patients in the high risk group).
The study was approved by the Ethics Committee of Poznan University of Medical Sciences (resolution number 1013/09). All experiments were conducted in accordance with the relevant guidelines and regulations, approved by this Committee. All patients or their guardians expressed an informed consent for participation in the study.
MRD assessment
MRD data obtained by standardized quantitative methods was available for 159 of 174 patients (91.4%), and was based on flow cytometry (further referred to as MRDFC) in 136 patients (78.1%) and on real-time PCR detection of Ig/TCR gene rearrangements (further referred to as MRDRQ) in 23 patients (13.2%). For 15 patients (8.6%), the only available MRD data was obtained by a simplified, low-cost method using PCR-based detection of Ig/TCR gene rearrangements and clonality assessment by heteroduplex analysis20; these patients were excluded from the association analyses.
For MRD data obtained by either FC or RQ, a common cut-off level of 10−4 (1 malignant cell/10 000 normal cells) was used to define patients with MRD-positive and MRD-negative status (MRD > = 10−4 and MRD < 10−4, respectively). This cut-off level, often regarded as a sensitivity threshold of the FC method, has been earlier used in other studies on the association of polymorphic variants with MRD measured by FC and/or RQ16,17,18.
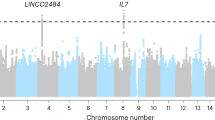
Assessment of MRDFC was performed in full bone marrow aspirates, according to the standard protocols of the EuroFlow Group, using a single or double 8-color combination of standardized monoclonal antibodies and 8-colour Becton Dickinson FACS Canto II flow cytometer21,22. For molecular analyses, mononuclear cells were isolated from the bone marrow using density gradient centrifugation. Real-time PCR analysis of MRD was carried out according to standard EuroMRD-ALL protocols and data interpretation guidelines23, with the use of standardized BIOMED-1 and BIOMED-2 primers24,25 for IGH, IGK-Kde, TCRG, TCRD and TCRB loci (the last with the application of TCRB Gene Clonality Assay-Gel Detection; Invivoscribe). 7900HT Fast Real-Time PCR System (Life Technologies) was used for the quantification of the MRD levels.
Genotyping of polymorphic loci
Selection of 23 polymorphic markers for the association study was based on the combination of two approaches. In a candidate gene approach, the genes were selected based on their involvement in metabolic pathways of drugs used in ALL therapy, as evidenced by Pharmacogenomics Knowledgebase (www.pharmgkb.org) and literature data. The polymorphisms included: GSTM1 and GSTT1 gene deletions, GSTP1 (rs1695), MTHFR (rs1801133), TYMS 28-bp tandem repeats (rs3474033: allele TSER*2, allele TSER*3, and a G > C SNP within the TSER*3 allele; TSER*3G > C), RFC (rs1051266), NR3C1 (rs6198, rs41423247), MDR1 (rs3789243, rs2235046, rs1045642), and VDR (rs2228570, rs1544410). The second approach allowed inclusion of polymorphisms in the genes earlier reported to be associated with the MRD-positive status: CCR5 (rs333 also known as 585del32)16, TPMT (rs1800460, rs1142345)17; other six loci from the genome-wide association study (GWAS)18: IL15 (rs10519613), NALCN (rs7992226), CCDC85C (rs11160533), and three intergenic (rs3862227, rs4888024, rs9871556). The six loci selected from the GWAS study18 were chosen with regard to their P-values for association with MRD, odds ratio (OR) for the MRD-positive status associated with carrying the risk allele, P-values for association with other phenotypes (e.g. methotrexate clearance), and minor allele frequency (MAF) in Caucasians.
Genotyping of polymorphic loci was performed in all 174 patients. DNA was isolated with the use of QIAamp DNA Blood Mini Kit (Qiagen, Germany) from blood/bone marrow samples obtained at the time of hematological remission (in most cases, week 12). High Resolution Melting (HRM) analysis was used for genotyping of 11 loci. Six loci were studied with the use of TaqMan Genotyping Assays (Life Technologies), namely: NALCN, CCDC85C, three intergenic variants selected from GWAS and one polymorphism in NR3C1 (rs41423247). 7900HT Fast Real-Time PCR System was used for both HRM and TaqMan Genotyping assays. Conventional PCR and agarose gel detection was used for genotyping of CCR5 (585del32), GSTM1 and GSTT1 gene deletions, TYMS 28-bp tandem repeats (alleles TSER*2, TSER*3, TSER*3G > C) and RFC, the latter two followed by restriction fragments length polymorphism analysis. For each polymorphic locus, 10% of results were verified by repeating the genotyping analysis or by direct sequencing.
All polymorphic loci were screened for linkage disequilibrium (LD) using SNAP software (SNP Annotation and Proxy Search, Broad Institute) based on Haploview 4.0 and genotype data from International HapMap Project and the 1000 Genomes Project26. Compliance of genotypes distribution with the Hardy-Weinberg equilibrium (not applicable to GSTM1 and GSTT1 gene deletions) was tested using the Court Lab Calculator (http://www.tufts.edu/). PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/) and SIFT (http://sift.jcvi.org/) were used for prediction of functional effects of selected polymorphic variants.
Statistical analyses
MRD results were analyzed as a categorical variable (MRD-positive vs. MRD-negative, with a cut off level 10−4) and as a continuous variable (MRD levels).
Pearson χ2 test or, if expected frequencies were <5, 2-sided Fisher’s exact probability test (2 × 2 tables) and Freeman-Halton extension of 2-sided Fisher’s exact probability test (2 × 3 tables), with 2-sided Z-test for difference in proportions as a post hoc test were used to estimate the significance of: 1/differences in genotypes distribution between patients with MRD-positive and MRD-negative status; 2/association of MRD status with the allele frequency and allele positivity (genotypes pooled into binary groups and analyzed in dominant and recessive mode, e.g. GG + AG < > AA and AA + AG < > GG); odds ratio (OR) and confidence intervals (CI) for MRD-positivity calculated for the allele frequency and allele positivity; 3/association of the clinical features with MRD status, defined as ‘MRD-associated clinical covariates’; 4/additive effects between polymorphic variants (differences between MRD-positive and MRD-negative patient groups in the distribution of patients carrying risk allele in 0, 1 or 2 loci identified to be associated with the MRD status at day 33).
Univariate logistic regression was used to confirm the association of polymorphic variants with MRD status. Multivariate logistic regression was used to adjust for MRD-associated clinical covariates and for identification of the best regression models predicting the MRD status.
Non-parametric test (Kruskal-Wallis ANOVA on ranks) was used for analysis of association of polymorphic variants (genotypes and binary groups representing allele positivity) with MRD levels (MRD as a continuous variable).
Two-sided analysis of statistical power was performed using Quanto software v.1.2.4.
P-values < 0.05 defined statistical significance in all tests applied.
Benjamini-Hochberg procedure was applied to control for false discovery rate (FDR) in case of multiple comparison tests (association of the MRD status with the distribution of genotypes, allele frequency and allele positivity)27,28. This adjustment was not applied to tests involving clinical covariates and additive effects of carrying risk alleles, since they did not comply with the Benjamini-Hochberg assumption of the independence of multiple tests.
Statistica v. 10 (StatSoft Inc.) and VassarStats: Website for Statistical Computation (http://vassarstats.net/) were used for statistical analyses.
Results
MRD-associated clinical covariates
There are several clinical covariates of prognostic significance that have been widely used for risk group classification in ALL (e.g. in the ALL IC-BFM 2002 protocol). Many of them have been retained in the recent protocols that include MRD monitoring (such as ALL IC-BFM 2009). They include parameters identified at diagnosis, such as: age, white blood cell count (WBC), the presence of translocations t(9;22)/BCR-ABL, t(4;11)/MLL-AF, or both, (further referred to as ‘fusion genes’), and factors assessed early during therapy, such as ALL blast count after 8 days of prednisone treatment (prednisone response) and bone marrow morphology (M1, M2, M3) assessed at day 15 and day 33.
Distribution of our patients according to the clinical features at diagnosis and early induction, presented as prognostic categories, is shown in Table 1. Although the study group did not consist of consecutive patients (see Methods, section Patients), their distribution into high risk (HR), intermediate (IR) and standard risk (SR) groups (Table 1) did not differ from that reported for a cohort of 5060 patients treated according to the ALL IC-BFM 2002 protocol19 (P = 0.2265).
The distribution of patients according to the MRD status assessed at day 15, day 33 and week 12 following the beginning of the treatment, measured by FC (MRDFC) and – in an enlarged group of patients – by FC or RQ (MRDFC/RQ), is presented in Table 2.
The analysis of association between the clinical covariates and the MRD status (MRDFC and MRDFC/RQ) was estimated at three time points (Table 3).
The risk group (according to ALL IC-BFM criteria, Table 1) was the only covariate associated with MRDFC/RQ positivity at day 15 (P = 0.044); there was no association (P = 0.067) with MRDFC.
The risk group was also significantly associated with MRDFC at day 33 and at week 12 (P < 0.001, P < 0.001, respectively). Significant associations with MRDFC at these time points were also found for the status of the ‘fusion genes’ (P = 0.001, P = 0.021, respectively) and bone marrow morphology at day 15 (P = 0.002, P = 0.001, respectively). The same clinical covariates were found significantly associated with MRD at these time points in the enlarged group of patients (MRDFC/RQ), with one additional covariate (prednisone response) at day 33.
All these covariates were further used in multivariate analysis (logistic regression) with polymorphic loci associated with MRD status. Risk group was assessed separately in logistic regression model, since it is related to the presence of fusion genes and bone marrow morphology at day 15.
Identification of MRD-associated polymorphic loci
All but two polymorphic loci from the 23 analyzed in our study were in Hardy-Weinberg (HW) equilibrium. The rs1142345 in TPMT gene deviated from the HW equilibrium, but was not associated with the MRD status in our study group. The rs1800460 in the same gene, found non-polymorphic in our cohort, was excluded from the analyses. No linkage disequilibrium (LD) between any of the polymorphic loci was observed.
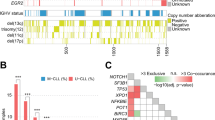
The association of all polymorphic loci with MRDFC was initially tested by analyzing the distribution of genotypes among patients with MRD-positive and MRD-negative status. Two loci were significantly associated with the MRDFC status: rs10519613 in IL15 with MRD at day 33 (P = 0.029) and rs1051266 in RFC with MRD at week 12 (P = 0.004). The 2-sided Z-test for difference in proportions revealed that CC and AC genotypes of the IL15 locus were significantly more frequent among patients with the negative MRD status at day 33 (P = 0.019) and the positive MRD status at day 33 (P = 0.013), respectively; while there was no significant difference in the distribution of AA genotype (P = 0.079). AA genotype of the RFC locus was significantly more frequent among patients with the positive MRD status at week 12 (P = 0.001), while there was no significant difference in the distribution of AG and GG genotypes (P = 0.082 and P = 0.170, respectively). A marginally significant associations (P values < 0.08) were also observed for rs1544410 in VDR with MRD at day 15 and at week 12 (P = 0.078 and P = 0.064, respectively) (Table 4). All the associated loci are further often referred to by the gene names only, with the omission of ‘rs’ identifiers.
The above associations of genotypes with the MRDFC status were subsequently analyzed in univariate logistic regression, and were confirmed for: VDR and MRD at day 15 (P = 0.034), IL15 and MRD at day 33 (P = 0.039) and RFC and MRD at day 33 (P = 0.047). A significant association with MRD was also confirmed in the enlarged group of patients (MRDFC/RQ) for: VDR and MRD at day15 (P = 0.026), RFC and MRD at day 33 and at week 12 (P = 0.048 and P = 0.037, respectively).
The association of all the loci under study with MRDFC status was subsequently investigated by the analysis of differences in allele frequencies (not applicable to GSTM1 and GSTT1 gene deletions) (Table 5). Significant difference in the allele frequency in MRD-positive and MRD-negative patients was found for: VDR (allele A and positive MRD status at day 15; OR = 2.37, 95% CI = 1.07–5.21, P = 0.03), RFC (allele A and positive MRD status at day 33; OR = 1.93, 95% CI = 1.05–3.52, P = 0.03) and IL15 (allele A and positive MRD status at day 33; OR = 2.30, 95% CI = 1.02–5.18, P = 0.04). These results were confirmed by 2-sided Z-test for difference in proportions: for the association of allele frequencies in VDR with MRD at day 15, IL15 with MRD at day 33 and RFC with MRD at day 33 (P = 0.028, P = 0.039, P = 0.030, respectively).
Significant difference was also found for RFC allele frequencies in patients with MRD-positive and MRD-negative status at week 12 (P < 0.01). Although it was not possible to calculate OR due to 0 value in one of the cells, the association of A allele with positive MRD status at week 12 was confirmed with 2-sided Z-test for difference in proportions: P = 0.003.
Statistical power for these associations ranged from 70% for the VDR locus (MRD at day 15) to 57% and 56% for RFC and IL15 loci (MRD at day 33). It was not possible to calculate statistical power for RFC locus associated with MRD at week 12 (OR was non evaluable).
The associations of VDR, IL15 and RFC alleles with the MRDFC status were further investigated by the analysis of differences in allele positivity (genotypes represented as binary groups) in patients with the MRD-positive and MRD-negative status (Table 6). A significant association was found for IL15 (positivity for the minor allele A with the positive MRD status at day 33, as revealed by AA + AC < > CC analysis, OR = 2.91, 95% CI = 1.17–7.27, P = 0.024, confirming A as the risk allele) and RFC (positivity for the major allele G associated with the negative MRD status at day 33; GG + AG < > AA, OR = 0.37, 95% CI = 0.15–0.92, P = 0.043, indicating G as a protective allele. Positivity for the G allele was also associated with the negative MRD status at week 12, P = 0.004, with no possibility to calculate OR due to 0 value in one of the cells). These results were confirmed by 2-sided Z-test for difference in proportions: for IL15 locus (association with the MRD status at day 33, P = 0.019) and RFC locus (association with the MRD status at day 33 and week 12, P = 0.029 and P = 0.001, respectively).
The VDR, IL15, and RFC loci were also analyzed for association with the MRD regarded as a continuous variable (MRD levels tested with the use of Kruskal-Wallis ANOVA on ranks). The following associations with MRDFC were found: IL15 with the MRD status at day 33 (P = 0.037 for genotypes distribution, and P = 0.013 for AA + AC < > CC); RFC with the MRD status at day 33 (P = 0.049 for GG + GA < > AA), and RFC with the MRD status at week 12 (P = 0.003 for genotypes distribution; P = 0.001 for GG + GA < > AA). The associations of RFC with the MRD status at week 12 were also confirmed in the enlarged group of patients (MRDFC/RQ; P = 0.030 for genotypes distribution and P = 0.009 for GG + GA < > AA). These results were consistent with our findings on the association of these variants with MRD as a categorical variable (MRD-positive vs. MRD-negative status). No statistically significant association was found between MRD levels and VDR locus.
Adjustment for MRD-associated clinical covariates
MRD-associated loci (genotypes and/or binary groups) were then analyzed in multivariate analysis to adjust for clinical covariates significantly associated with the MRD status in our cohort of patients (Table 3), and to assess if the inclusion of these loci improves prediction of the MRD status in logistic regression models.
Association of RFC genotypes and binary groups with the MRD status at day 33 remained significant after adjustment for the clinically assessed risk group (ALL IC-BFM 2002/2009 risk group). Inclusion of data on the distribution of RFC genotypes or binary groups improved logistic regression models for the MRD status prediction (in the group of patients with the MRDFC data: P < 0.00001 for the models combining RFC data with the risk group vs. P = 0.00001 for the model including risk group alone). However, in the larger cohort of patients (MRDFC/RQ data), the model including risk group alone was the best model predicting the MRD status. After adjustment for the fusion genes and the bone marrow morphology at day 15, RFC locus had no significance in association with the MRD status at day 33.
Association of RFC genotypes with the MRD status at week 12 remained significant after adjustment for the fusion genes combined with the bone marrow morphology at day 15, as well as after adjustment for the risk group. Inclusion of RFC genotypes data resulted in the improvement of the logistic regression model (in the group of patients with the MRDFC/RQ data, P < 0.00001 vs. P = 0.00001 for the model with fusion genes combined with bone marrow morphology alone; P < 0.00001 also for the model with the risk group alone). Distribution of the binary groups (GG + AG < > AA) in RFC locus remained significantly associated with the MRDFC status at week 12 after adjustment for the clinical covariates: fusion genes and bone marrow morphology (P = 0.0078) or the risk group (P = 0.0012). However, inclusion of RFC binary groups did not improve the logistic regression models as compared to those with clinical covariates only (P = 0.0001 for the model including fusion genes and bone marrow morphology alone, and P = 0.00004 for the model including risk group alone). In the enlarged group of patients with MRDFC/RQ results, the association of GG + AG < > AA distribution in RFC locus remained significant only after adjustment for the risk group (P = 0.03848) but did not improve the logistic regression model including risk group alone (P < 0.00001).
The distribution of VDR genotypes remained significantly associated with the MRDFC/RQ status at day 15 after the adjustment for the risk group (P = 0.01720, for logistic regression model).
Association of genotypes and binary groups in IL15 locus with the MRD status at day 33 did not remain significant (neither for MRDFC nor MRDFC/RQ) after adjustment for the clinical covariates.
Additive effect of IL15 and RFC regarding MRD status at day 33
IL15 and RFC loci, with the identified risk alleles associated with the positive MRDFC status at day 33, were analyzed for a possible additive effect (Table 7). A significant difference in the distribution of patients carrying genotypes with risk alleles in both these loci, in only one or in none of these two loci (further referred to as 2, 1 and 0 risk allele-carrying genotypes, respectively) was found between patients with MRD-positive and MRD-negative status (P = 0.017). A significant difference was also found in the distribution of patients with 2 vs. 1 and 2 vs. 0 genotypes among groups with positive and negative MRDFC. Odds ratio for the positive MRD status was: OR = 3.94 (95% CI = 1.28–12.11, P = 0.024) for patients with 2 risk allele-carrying genotypes compared to those with 1 risk allele-carrying genotype, and OR = 6.75 (95% CI = 1.61–28.39, P = 0.012) for patients with 2 risk allele-carrying genotype compared to patients carrying no risk allele. These findings were confirmed in the enlarged group of patients (association with the positive MRDFC/RQ status): the significant difference in the distribution of patients with 2 vs. 1 vs. 0 risk allele-carrying genotypes among MRD-positive and MRD-negative groups (P = 0.031); OR = 2.90 (95% CI = 1.09–7.68, P = 0.038) for 2 vs. 1; OR = 4.56 (95% CI = 1.39–14.97, P = 0.017) for 2 vs. 0. This additive effect of RFC and IL15 remained significant in multivariate analysis (logistic regression) after adjustment for the MRD-associated clinical covariates: fusion genes and bone marrow morphology at day 15 (P = 0.00002 and P < 0.00001 for models analyzing association with MRDFC and MRDFC/RQ, respectively) and after adjustment for the risk group (P < 0.00001 for logistic regression model analyzing association with MRDFC).
Discussion
Most of the data on the association of germline genetic variation in ALL patients with the treatment outcome comes from the research focused on the genes involved in metabolic pathways of drugs used in ALL therapy (a candidate gene approach), with standard indicators (survival analysis) used as a measure of therapy efficacy10,11,12,13,14.
Despite the fact that MRD status is a direct and rapid indicator of treatment results, the association of polymorphic variants with MRD has not been extensively investigated, with only three studies published so far16,17,18. The existing scarce data on the MRD-associated genetic variants have been obtained in groups of patients of diverse ethnic composition and treated with various therapeutic protocols, therefore with different time points of MRD assessment used. These factors might substantially influence the results of a pharmacogenetics analysis.
In contrast, our study was performed in the ethnically homogeneous patient group (Caucasians of Slavic origin), using uniform time points of MRD assessment and the cut-off level of 10−4 . Comparison of our study design with other studies16,17,18 focused on MRD-associated germline polymorphisms is presented in Table 8.
We searched for the association of the germline genetic variants in selected genomic regions with the MRD status, used as a direct measure of the ALL therapy outcome. The cohort comprised 159 patients, diagnosed with pediatric BCP-ALL and treated according to ALL IC-BFM 2002 and ALL IC-BFM 2009 protocols. The regimen used in both protocols enables direct inclusion into the association analysis of MRD results at two of the three time points assessed in our study; for the analysis of the third time point, several patients treated with the ALL IC-BFM 2009 protocol were excluded. The time points used in the present study were: early assessment of the response to initial treatment (remission induction, day 15), the end of remission induction (day 33), and the time point before introduction of the consolidation treatment (week 12). MRD was assessed by FC (in the majority of patients) and by RQ-PCR (to extend the number of patients with available MRD results); in both groups the common cut-off level was10−4.
We demonstrated the association of the MRD status with the genetic variants in three genes: VDR, RFC and IL15. The rs1544410 variant in VDR was significantly associated with the MRD status at day 15. VDR (vitamin D receptor) locus encodes a steroid hormone receptor, which upon binding an active metabolite of vitamin D (1 alpha, 25-dihydroxyvitamin D-3) exerts a pleiotropic effect on a wide range of biological processes, including calcium homeostasis but also modulation of immune response, cell differentiation and proliferation29. VDR, in complex with the active form of vitamin D, acts as a trans-acting transcriptional regulatory factor through binding to ‘vitamin D response elements’ (VDRE). VDRE are present in promoter regions of over 150 human target genes30, including CYP3A4, which metabolizes a number of therapeutic agents used in ALL treatment31. Due to the role of vitamin D in the immune system homeostatis, the genetic variation in VDR has also been studied in association with the outcome of autoimmune diseases32.
Two VDR gene variants analyzed in the present study (rs1544410 also named BsmI, and rs2228570 named FokI, both localized in the 3′ end of VDR gene, though in different LD blocks) are among VDR variants broadly investigated for association with the risk and outcome of several malignancies, including glioma33, colon cancer34 and ALL13. In the latter study, T allele of rs2228570 and GG genotype of rs1544410 have been associated with the increased risk of central nervous system relapse in pediatric ALL patients in the higher-risk arm13. This contradicts our study results based on the allele frequency analysis in MRD-positive vs. MRD-negative groups, whereby no significant association of rs2228570 was found and the opposite A allele of rs1544410 was identified as a risk allele. The possibility that these discrepant findings are due to the ethnic differences between the groups studied (a non-uniform group of patients with Caucasian, African American and other ethnicities studied by Rocha et al.13 and the homogeneous group of Slavic patients studied by us) could be related to the fact that the composition of LD blocks in the VDR gene is different in Caucasians, African Americans and Asians. However, in all these populations the rs2228570 variant is not assigned to any of the LD blocks, while the rs1544410 variant resides in the distal 3′ haplotype block35. The discrepant results regarding the risk alleles in VDR variants might be due to the different phenotypes analyzed: MRD positive status in the bone marrow in our study and central nervous system relapse in the study by Rocha et al.13. In fact, although no functional effect of the rs1544410 variant is known so far, it has been postulated that association with various phenotypes might reflect linkage disequilibrium of this marker variant with a causative variant in or near the VDR gene36. The pleiotropic regulatory function of VDR gene might explain why the same allele is identified as a risk allele for one phenotype, while being a protective allele for another.
Two other variants, rs10519613 in IL15 and rs1051266 in RFC, were found to be significantly associated in our cohort with the MRD status at day 33 (and at week 12, for RFC).
The association of RFC with MRD was very consistent throughout all the analyses. It was found both in the smaller group of patients assessed by FC only and in the enlarged group assesses by FC/RQ. It was shown both for MRD considered as a categorical variable (positive vs. negative) and as a continuous variable, and for RFC genotypes distribution, allele frequency and allele positivity. In multivariate analysis, RFC remained significantly associated with the MRDFC and MRDFC/RQ status at day 33 after adjustment for the risk group; also the association of the RFC genotypes and binary groups with MRD at week 12 remained significant after adjustment for MRD-associated clinical covariates. The inclusion of RFC data improved the logistic regression model for the MRD status at day 33 and at week 12, as compared to the models containing clinical covariates alone.
RFC gene (reduced folate carrier, also named SLC19A1 for solute carrier family 19 member 1), encodes the membrane protein responsible for carrier-mediated transport of folate, which is essential for DNA synthesis, DNA repair and DNA methylation. Methotrexate (MTX), a key anti-metabolite component of chemotherapeutic protocols used in ALL, is also actively transported by RFC protein.
The rs1051266 variant (80G > A; Arg27His in exon 2 of RFC) has been widely studied for correlation with MTX efficacy and toxicity in various diseases, including rheumatoid arthritis, colorectal neoplasms and ALL. Some studies investigated its association with ALL susceptibility37 and outcome38,39, with contradictory results. The A allele of rs1051266 has been shown to be associated with better response to MTX treatment and improved outcome in rheumatoid arthritis40 and in ALL38,39,41. None of these ALL studies used MRD as an indicator of the ALL outcome. In a single study, rs1051266 has been studied in relation to MRD levels in children with ALL treated according to Pediatric Oncology Group protocols, but no association was found16.
In contrast to these findings, we demonstrated that A allele of rs1051266 was associated with the MRD positive status at day 33 and week 12, indicating that it is a risk allele for the inferior response to treatment in ALL. Our results are in line with those of two other groups, who did not use MRD as an indicator of ALL outcome, but have indicated A allele of rs1051266 as a risk allele for the pediatric ALL outcome42,43. One has demonstrated poorer survival and significantly increased chance for ALL relapse in patients with GA and AA genotype as compared to patients with GG genotype42. In the other study, significantly higher risk of event in EFS analysis has been shown for patients carrying A allele as compared to GG genotype; this remained significant after adjustment for other prognostic factors that influence ALL outcome43. The authors have also shown higher MTX plasma levels in patients with AA genotype than in patients with other genotypes, and speculated that the impaired intracellular uptake might be due to the lower affinity of the resulting variant of RFC protein to MTX. However, in vitro study has shown no significant differences in MTX uptake between transport-impaired K562 cells transfected with either 80GG or 80AA RFC cDNA44. The latter observation is in line with our in silico prediction of a functional effect of rs1051266 in RFC, which was ‘benign’ according to PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/) and ‘tolerated’ according to SIFT algorithms (http://sift.jcvi.org/).
The rs10519613 variant in IL15, has been previously shown to be associated with MRD levels in pediatric ALL. In GWAS analysis, performed in pediatric ALL patients treated according to St Jude Total Therapy and Children’s Oncology Group protocols, rs10519613 (together with five other SNPs in IL15, all in strong LD, r2 > 0.5) was among the top 102 variants associated with the MRD levels at the end of induction18. The A allele of rs10519613 has been identified as a risk allele for MRD-positive status, which is in line with our findings. Recently, IL15 locus has been demonstrated to be associated with EFS in pediatric patients treated according to Malaysia-Singapore ALL 2003 protocol (a modification of ALL IC-BFM 2002 protocol)10. The rs17015014 variant of IL15 reported to be associated with ALL outcome10, was also one of the five linked SNPs previously reported to be MRD-associated18. Although the study design differed from ours, being focused on monitoring survival rather than MRD as the end point for the studied associations, our results remain in line with these findings. Thus, we provide additional data supporting the role of IL15 polymorphisms in the treatment response in pediatric ALL.
IL15, interleukin 15, encodes the cytokine that regulates activation and proliferation of T lymphocytes and natural killer (NK) cells, and thus is involved in immune response, including anti-tumor response45,46. Natural killer cells are key players in the innate immune response against cancer and virus-infected cells47,48. There has been recently an increasing number of data on the use of genetically manipulated NK cells, including NK cells expressing membrane-bound IL15 for autocrine stimulation. This results in better persistence and expansion of NK cells following infusion into the patient and improves their anti-tumor potential in adoptive immunotherapy48,49,50,51. These very latest functional experiments are an elegant evidence for the role of IL15 gene in anti-tumor response, and are in line with our results on the association of IL15 polymorphism with MRD-status.
An important finding of our study concerns the additive effect of risk alleles in RFC locus (allele A of rs1051266) and IL15 (allele A of rs10519613) for the association with the positive MRDFC status at day 33 (the end of remission induction in ALL IC-BFM protocols 2002 and 2009). Patients carrying at least two risk alleles in these two loci had a significantly higher (nearly 4-fold difference) chance for the positive MRD status as compared to patients with risk allele/s in any of these two genes and to those with no risk alleles (over 6-fold difference). This additive effect was confirmed in the enlarged cohort of patients with MRDFC/RQ results and remained significant after the adjustment for MRD-associated clinical covariates in multivariate analysis.
There are some limitations of the current study that should be noted. The main limitation is a relatively small sample size, related to the inclusion criteria we used: Caucasian patients of Slavic origin, treated according to ALL IC BFM protocols, with MRD data available for three time points during the treatment. Due to the limited sample size, the statistical power of the tests for associations ranged from 5% to 99% (Table 5). The power of tests regarding VDR, RFC and IL15 loci (found to be associated with the MRD status) ranged from 56–70%, but was still lower than the 80%, usually appreciated in association studies. As a consequence, the study could only offer a limited possibility to detect MRD association with small-effect polymorphisms (OR: 1.1–1.5; this translated to the increased risk of false negatives) and low positive predictive value (PPV, the probability that an observed effect is a true positive).
However, as in any association study, the consequences of the low power should be weighted in light of the study goals52,53. Here we aimed to identify candidate polymorphic variants that might serve as potential prognostic markers of the MRD status. Confronted with the rarity of patients satisfying the inclusion criteria on one side and the substantial impact that could be potentially gained from the identification of novel genetic predictors of the therapy efficacy, we reported our findings in spite of being aware of the power limitations.
In particular, the association with the MRD status was reported for three loci: VDR, IL15 and RFC, of which only one (RFC) remained significant upon Benjamini-Hochberg adjustment for multiple testing. The advantage of reporting marginally significant results was substantiated by our finding of the additive effect of carrying risk alleles in IL15 and RFC loci. This indicated that while a single polymorphic locus may add little to the prognostic significance of the existing prognostic factors, concurrent analysis of several MRD-associated loci might improve risk assessment in ALL patients. Obviously, our findings require confirmation in larger cohorts of patients, taking into account different ethnicities and treatment protocols.
Another limitation of our study is associated with the use of arbitrary cut-off level of 10−4, which was chosen to categorize MRD results (MRD-positivity vs. MRD-negativity) and to compare with the results of others, but which does not fully reflect MRD-based classification into three risk groups, used in the clinical practice.
Conclusions
Our results indicate associations of polymorphic variants in three genes with the MRD-status in pediatric ALL patents: rs1544410 in VDR with MRD at day 15; rs1051266 in RFC, independently and in combination with rs10519613 in IL15 with MRD at day 33; and rs1051266 in RFC with MRD at week 12. The association of the RFC variant was the most consistent in our study, and remained significant also upon the adjustment for multiple testing. We showed an additive effect of the risk alleles in RFC and IL15 on the strength of their association with MRD at day 33. We also identified clinical features associated with the MRD status in ALL IC-BFM 2002 and 2009 protocols.
Although association studies do not necessarily need to reveal biological mechanisms behind the observed associations, possible mechanisms of the MRD dynamics in treatment response can be proposed based on our results. In particular, the MRD status appears to be influenced by the genetic variation of genes involved in pharmacokinetics/pharmacodynamics of anti-leukemic drugs (RFC and potentially VDR, acting as pleiotropic transcriptional regulator) as well as the genes involved in anti-tumor immunity of the host (IL15 and potentially VDR).
MRD-associated polymorphisms, being accessible for the uncomplicated and cost-effective analysis at the time of diagnosis, and adding prognostic information to the existing prognostic factors, might potentially improve the risk assignment in pediatric ALL.
Additional Information
How to cite this article: Dawidowska, M. et al. Association of germline genetic variants in RFC, IL15 and VDR genes with minimal residual disease in pediatric B-cell precursor ALL. Sci. Rep. 6, 29427; doi: 10.1038/srep29427 (2016).
References
Inaba, H., Greaves, M. & Mullighan, C. G. Acute lymphoblastic leukaemia. Lancet 381, 1943–1955, doi: 10.1016/s0140-6736(12)62187-4 (2013).
Gatta, G. et al. Childhood cancer survival in Europe 1999–2007: results of EUROCARE-5-a population-based study. Lancet Oncology 15, 35–47, doi: 10.1016/s1470-2045(13)70548-5 (2014).
van Dongen, J. J. et al. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet 352, 1731–1738, doi: 10.1016/S0140-6736(98)04058-6 (1998).
Cavé, H. et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of Cancer–Childhood Leukemia Cooperative Group. N Engl J Med 339, 591–598, doi: 10.1056/NEJM199808273390904 (1998).
Coustan-Smith, E. et al. Immunological detection of minimal residual disease in children with acute lymphoblastic leukaemia. Lancet 351, 550–554, doi: 10.1016/S0140-6736(97)10295-1 (1998).
Borowitz, M. J. et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia and its relationship to other prognostic factors: a Children’s Oncology Group study. Blood 111, 5477–5485, doi: 10.1182/blood-2008-01-132837 (2008).
Conter, V. et al. Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: results in 3184 patients of the AIEOP-BFM ALL 2000 study. Blood 115, 3206–3214, doi: 10.1182/blood-2009-10-248146 (2010).
Chen, I. M. et al. Outcome modeling with CRLF2, IKZF1, JAK and minimal residual disease Study in pediatric acute lymphoblastic leukemia: a Children’s Oncology Group. Blood 119, 3512–3522, doi: 10.1182/blood-2011-11-394221 (2012).
Yamashita, Y. et al. IKZF1 and CRLF2 gene alterations correlate with poor prognosis in Japanese BCR-ABL1-negative high-risk B-cell precursor acute lymphoblastic leukemia. Pediatric Blood & Cancer 60, 1587–1592, doi: 10.1002/pbc.24571 (2013).
Lu, Y. et al. Host genetic variants of ABCB1 and IL15 influence treatment outcome in paediatric acute lymphoblastic leukaemia. British Journal of Cancer 110, 1673–1680, doi: 10.1038/bjc.2014.7 (2014).
Radtke, S. et al. Germline genetic variations in methotrexate candidate genes are associated with pharmacokinetics, toxicity, and outcome in childhood acute lymphoblastic leukemia. Blood 121, 5145–5153, doi: 10.1182/blood-2013-01-480335 (2013).
Yang, J. J. et al. Genome-wide association study identifies germline polymorphisms associated with relapse of childhood acute lymphoblastic leukemia. Blood 120, 4197–4204, doi: 10.1182/blood-2012-07-440107 (2012).
Rocha, J. C. C. et al. Pharmacogenetics of outcome in children with acute lymphoblastic leukemia. Blood 105, 4752–4758, doi: 10.1182/blood-2004-11-4544 (2005).
Aplenc, R. et al. Methylenetetrahydrofolate reductase polymorphisms and therapy response in pediatric acute lymphoblastic leukemia. Cancer Research 65, 2482–2487, doi: 10.1158/0008-5472.can-04-2606 (2005).
van Dongen, J. J. M., van der Velden, V. H. J., Brueggemann, M. & Orfao, A. Minimal residual disease diagnostics in acute lymphoblastic leukemia: need for sensitive, fast, and standardized technologies. Blood 125, 3996–4009, doi: 10.1182/blood-2015-03-580027 (2015).
Davies, S. M. et al. Pharmacogenetics of minimal residual disease response in children with B-precursor acute lymphoblastic leukemia: a report from the Children’s Oncology Group. Blood 111, 2984–2990, doi: 10.1182/blood-2007-09-114082 (2008).
Stanulla, M. et al. Thiopurine methyltransferase (TPMT) genotype and early treatment response to mercaptopurine in childhood acute lymphoblastic leukemia. Jama-Journal of the American Medical Association 293, 1485–1489, doi: 10.1001/jama.293.12.1485 (2005).
Yang, J. J. et al. Genome-wide Interrogation of Germline Genetic Variation Associated With Treatment Response in Childhood Acute Lymphoblastic Leukemia. Jama-Journal of the American Medical Association 301, 393–403, doi: 10.1001/jama.2009.7 (2009).
Stary, J. et al. Intensive Chemotherapy for Childhood Acute Lymphoblastic Leukemia: Results of the Randomized Intercontinental Trial ALL IC-BFM 2002. Journal of Clinical Oncology 32, 174–184, doi: 10.1200/jco.2013.48.6522 (2014).
Scrideli, C. A. et al. A simplified minimal residual disease polymerase chain reaction method at early treatment points can stratify children with acute lymphoblastic leukemia into good and poor outcome groups. Haematologica-the Hematology Journal 94, 781–789, doi: 10.3324/haematol.2008.003137 (2009).
van Dongen, J. J. M. et al. EuroFlow antibody panels for standardized n-dimensional flow cytometric immunophenotyping of normal, reactive and malignant leukocytes. Leukemia 26, 1908–1975, doi: 10.1038/leu.2012.120 (2012).
Kalina, T. et al. EuroFlow standardization of flow cytometer instrument settings and immunophenotyping protocols. Leukemia 26, 1986–2010, doi: 10.1038/leu.2012.122 (2012).
van der Velden, V. H. J. et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 21, 604–611, doi: 10.1038/sj.leu.2404586 (2007).
Pongers-Willemse, M. J. et al. Primers and protocols for standardized detection of minimal residual disease in acute lymphoblastic leukemia using immunoglobulin and T cell receptor gene rearrangements and TAL1 deletions as PCR targets - Report of the BIOMED-1 CONCERTED ACTION: Investigation of minimal residual disease in acute leukemia. Leukemia 13, 110–118, doi: 10.1038/sj.leu.2401245 (1999).
van Dongen, J. J. M. et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: Report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 17, 2257–2317, doi: 10.1038/sj.leu.2403202 (2003).
Johnson, A. D. et al. SNAP: a web-based tool for identification and annotation of proxy SNPs using HapMap. Bioinformatics 24, 2938–2939, doi: 10.1093/bioinformatics/btn564 (2008).
McDonald, J. H. Handbook of Biological Statistics. 3rd ed. edn, (Sparky House Publishing, 2014).
Glickman, M. E., Rao, S. R. & Schultz, M. R. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. Journal of Clinical Epidemiology 67, 850–857, doi: 10.1016/j.jclinepi.2014.03.012 (2014).
Poon, A. H. et al. Very important pharmacogene summary for VDR. Pharmacogenetics and Genomics 22, 758–763, doi: 10.1097/FPC.0b013e328354455c (2012).
Wang, T. T. et al. Large-scale in silico and microarray-based identification of direct 1,25-dihydroxyvitamin D-3 target genes. Molecular Endocrinology 19, 2685–2695, doi: 10.1210/me.2005-0106 (2005).
Drocourt, L., Ourlin, J. C., Pascussi, J. M., Maurel, P. & Vilarem, M. J. Expression of CYP3A4, CYP2B6, and CYP2C9 is regulated by the vitamin D receptor pathway in primary human hepatocytes. Journal of Biological Chemistry 277, 25125–25132, doi: 10.1074/jbc.M201323200 (2002).
Carvalho, C. et al. Association between vitamin D receptor (VDR) gene polymorphisms and systemic lupus erythematosus in Portuguese patients. Lupus 24, 846–853, doi: 10.1177/0961203314566636 (2015).
Anic, G. M. et al. An exploratory analysis of common genetic variants in the vitamin D pathway including genome-wide associated variants in relation to glioma risk and outcome. Cancer Causes & Control 23, 1443–1449, doi: 10.1007/s10552-012-0018-7 (2012).
Touvier, M. et al. Meta-Analyses of Vitamin D Intake, 25-Hydroxyvitamin D Status, Vitamin D Receptor Polymorphisms, and Colorectal Cancer Risk. Cancer Epidemiology Biomarkers & Prevention 20, 1003–1016, doi: 10.1158/1055-9965.epi-10-1141 (2011).
Fang, Y. et al. Promoter and 3′-untranslated-region haplotypes in the vitamin D receptor gene predispose to osteoporotic fracture: The Rotterdam study. American Journal of Human Genetics 77, 807–823, doi: 10.1086/497438 (2005).
Uitterlinden, A. G., Fang, Y., van Meurs, J. B. J., van Leeuwen, H. & Pols, H. A. P. Vitamin D receptor gene polymorphisms in relation to vitamin D related disease states. Journal of Steroid Biochemistry and Molecular Biology 89–90, 187–193, doi: 10.1016/j.jsbmb.2004.03.083 (2004).
Koppen, I. J. N., Hermans, F. J. R. & Kaspers, G. J. L. Folate related gene polymorphisms and susceptibility to develop childhood acute lymphoblastic leukaemia. British Journal of Haematology 148, 3–14, doi: 10.1111/j.1365-2141.2009.07898.x (2010).
Gregers, J. et al. The association of reduced folate carrier 80G > A polymorphism to outcome in childhood acute lymphoblastic leukemia interacts with chromosome 21 copy number. Blood 115, 4671–4677, doi: 10.1182/blood-2010-01-256958 (2010).
Chiusolo, P. et al. The role of MTHFR and RFC1 polymorphisms on toxicity and outcome of adult patients with hematological malignancies treated with high-dose methotrexate followed by leucovorin rescue. Cancer Chemotherapy and Pharmacology 69, 691–696, doi: 10.1007/s00280-011-1751-4 (2012).
Drozdzik, M. et al. Reduced folate carrier-1 80G > A polymorphism affects methotrexate treatment outcome in rheumatoid arthritis.Pharmacogenomics Journal 7, 404–407, doi: 10.1038/sj.tpj.6500438 (2007).
Ashton, L. J. et al. Reduced folate carrier and methylenetetrahydrofolate reductase gene polymorphisms: associations with clinical outcome in childhood acute lymphoblastic leukemia. Leukemia 23, 1348–1351, doi: 10.1038/leu.2009.67 (2009).
Antonio Leyva-Vazquez, M. et al. Polymorphism G80A in the Reduced Folate Carrier Gene and its Relationship to Survival and Risk of Relapse in Acute Lymphoblastic Leukemia. Journal of Investigative Medicine 60, 1064–1067 (2012).
Laverdiere, C., Chiasson, S., Costea, I., Moghrabi, A. & Krajinovic, M. Polymorphism G(80)A in the reduced folate carrier gene and its relationship to methotrexate plasma levels and outcome of childhood acute lymphoblastic leukemia. Blood 100, 3832–3834, doi: 10.1182/blood.V100.10.3832 (2002).
Whetstine, J. R. et al. Single nucleotide polymorphisms in the human reduced folate carrier: Characterization of a high-frequency G/A variant at position 80 and transport properties of the His(27) and Arg(27) carriers. Clinical Cancer Research 7, 3416–3422 (2001).
Budagian, V., Bulanova, E., Paus, R. & Bulfone-Paus, S. IL-15/IL-15 receptor biology: A guided tour through an expanding universe. Cytokine & Growth Factor Reviews 17, 259–280, doi: 10.1016/j.cytogfr.2006.05.001 (2006).
Fehniger, T. A. & Caligiuri, M. A. Interleukin 15: biology and relevance to human disease. Blood 97, 14–32, doi: 10.1182/blood.V97.1.14 (2001).
Campbell, K. S. & Hasegawa, J. Natural killer cell biology: An update and future directions. Journal of Allergy and Clinical Immunology 132, 536–544, doi: 10.1016/j.jaci.2013.07.006 (2013).
Carlsten, M. & Childs, R. W. Genetic Manipulation of NK Cells for Cancer Immunotherapy: Techniques and Clinical Implications. Frontiers in immunology 6, 266–266, doi: 10.3389/fimmu.2015.00266 (2015).
Imamura, M. et al. Autonomous growth and increased cytotoxicity of natural killer cells expressing membrane-bound interleukin-15. Blood 124, 1081–1088, doi: 10.1182/blood-2014-02-556837 (2014).
Jiang, W., Zhang, C., Tian, Z. & Zhang, J. hIL-15 gene-modified human natural killer cells (NKL-IL15) augments the anti-human hepatocellular carcinoma effect in vivo . Immunobiology 219, 547–553, doi: 10.1016/j.imbio.2014.03.007 (2014).
Fujisaki, H. et al. Expansion of Highly Cytotoxic Human Natural Killer Cells for Cancer Cell Therapy. Cancer Research 69, 4010–4017, doi: 10.1158/0008-5472.can-08-3712 (2009).
Hozo, I., Schell, M. J. & Djulbegovic, B. Decision-making when data and inferences are not conclusive: Risk-benefit and acceptable regret approach. Seminars in Hematology 45, 150–159, doi: 10.1053/j.seminhematol.2008.04.006 (2008).
Ioannidis, J. P. A., Tarone, R. & McLaughlin, J. K. The False-positive to False-negative Ratio in Epidemiologic Studies. Epidemiology 22, 450–456, doi: 10.1097/EDE.0b013e31821b506e (2011).
Acknowledgements
This study was supported by National Science Centre Poland, grant numbers: N N407 311839 to Małgorzata Dawidowska and 2013/11/N/NZ5/03730 to Bronisława Szarzyńska-Zawadzka. Flow cytometry MRD assessment was possible thanks to internal grants from Medical University of Silesia.
Author information
Authors and Affiliations
Contributions
M.D. designed and coordinated the study. M.D., M.K. and B.S.-Z. performed genotyping of polymorphic variants and molecular MRD assessment. M.D. and A.S. performed statistical analyses. M.D. drafted the manuscript with contribution of M.W. and E.Z. and the input of other authors. Ł.S., M.T. and A.S., under supervision of T.S., performed FC-based immunophenotyping at diagnosis and FC-MRD assessment. K.D., M.L., K.P., A.O.-P., K.P.-W., K.K., A.K., A.D. and T.S. coordinated realization of the project in hemato-oncology units of their affiliation through sample and clinical data collection. W.G. supervised cell banking and DNA extraction. J.R.K. coordinated the realization of ALL IC-BFM 2002 and 2009 protocols in Poland. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Dawidowska, M., Kosmalska, M., Sędek, Ł. et al. Association of germline genetic variants in RFC, IL15 and VDR genes with minimal residual disease in pediatric B-cell precursor ALL. Sci Rep 6, 29427 (2016). https://doi.org/10.1038/srep29427
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29427
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.