Abstract
Pressure ulcer (PU) remains a common worldwide problem in all health care settings, it is synonymous with suffering. PU is a complex disease that is dependent on a number of interrelated factors. It involves multiple mechanisms such as physiological risk factors, chronic inflammation, oxidant–antioxidant imbalance and proteolytic attack on extracellular matrix by matrix metalloproteinases (MMP). Therefore, we propose that these wounds lead to molecular variations that can be detected by assessing biomarkers. In this study, we aimed to evaluate the major clinical elements and biological scars in Tunisian patients suffering from PU. Consistently, non-healing wound remains a challenging clinical problem. The complex challenges of the wound environment, involving nutrient deficiencies, bacterial infection, as well as the critical role played by inflammatory cells, should be considered because of their negative impact on wound healing. In addition, an imbalance between pro-oxidants and antioxidant systems seems to be more aggravated in patients with PU compared to healthy subjects. Of interest, this study provides further evidence to support a core role of the biological activity of MMP-9 in the pathogenesis of PU and indicates that the MMP9-1562 C/T (rs 3918242) functional polymorphism is associated with protection against this disease.
Similar content being viewed by others
Introduction
Being bedridden can be very difficult for many patients to adjust to, it can also cause other health problems1. The most common health risk for bedridden patients is pressure ulcer (PU)2. PU is commonly termed as bedsore, reflects a localized damage to the skin and underlying tissues, as a result of prolonged pressure higher, occurring when soft tissue is compressed between a bony prominence and an external surface. Heightened pressure, and/or in combination with torsion forces, can leads to decreased oxygen and nutrients reaching the tissues in combination with interruption of blood flow to a given area3,4.
The danger to being affected by PU is well known and it is a long standing problem. PU causes pain, increase morbidity and mortality rates, a high financial burden for the healthcare system and diminishes patient’s quality of life. It can develop quickly and is often difficult to treat5. PU is synonymous with suffering.
Despite diverse research, accumulated knowledge concerning these wounds and developing treatments, the number of PU is still increasing6,7,8,9. The National Pressure Ulcer Advisory Panel says the incidence ranges from 0.4% to 38% in hospitals, from 2.2% to 23.9% in skilled nursing facilities and from 0% to 17% for home health agencies10. There are wide variations between intra- and inter-country from 3.9% to over 18%11,12. However, the optimal incidence rate may vary depending on patient case mix, severity of illness, methodology for each survey and other contextual factors13.
The formation and molecular mechanisms underlying causes of PU are quite complex, with multiple influencing factors14. Extensive studies have identified several factors that increase the risk of PU10. The list of factors associated with PU risk is long, numbering more than 100 and includes previous medical events, patient demographic characteristics, anthropometric characteristics, functional status, physiological status, nutritional status, infectious agents, cognition, psychological status, immunological factors and more3,15.
Usually, any chronic wound damages the tissue and affects the local environment. The host’s response to wounding involves a series of coordinated interactions between diverse immunological and biological systems. This process can lead to a cascade of carefully and precisely regulated steps and events that correlate with the appearance of both resident and migratory cell populations, as well as the extracellular matrix and the action of soluble mediators such as growth factors and cytokines16.
Additionally, a variety of studies that analyzed blood, fluids and biopsies collected from chronic, nonhealing wounds found elevated levels of inflammatory cytokines, elevated levels of matrix metalloproteinases (MMP) and low levels of growth factors compared with acute, healing wounds. These signaling pathways might impede the wound healing process17,18. Moreover, prolonged, elevated levels of the gelatinase subset, MMP-9, a member of the MMP family of zinc-endopeptidases, are found in patients with chronic wounds that appear to have detrimental effects on wound healing19,20.
In particular, MMP-9 expression and/or activity under non-remodeling conditions are low, but are highly inducible following injury in response to a variety of damaging agents or myopathic conditions18. It seems likely that MMP-9 activity plays several key roles in extracellular matrix remodeling and immune cell migration during wound repair21. However, the protein is secreted as a pro-enzyme, activated when the N-terminus pro-domain unfolds and is cleaved by activator proteases exposing the catalytic domain, adding a significant post-transcriptional element to its adjustment22. Transcriptional regulation of MMP-9 by various inflammatory factors and developmental queues is considered to be the predominant mechanism of controlling expression of this pleiotropic molecule21.
Polymorphisms in the promoter of MMP-9 have been implicated in the regulation of gene expression and susceptibility to various diseases23. In the main, some polymorphisms have influence on gene expression, protein stability, protein activity, protein-protein interactions and some of them are associated with an increased risk for diseases. Notably, a single nucleotide polymorphism (SNP) -1562C/T MMP9 results in a loss of binding of a nuclear protein and an increase in transcriptional activity in macrophages24. However, little is known about association of SNP -1562C/T MMP9 with PU.
Therefore, we conducted a case control study to determine some physiological risk factors related to PU and the involvement of inflammation and oxidative stress in the development of PU. Besides, we aimed to investigate whether the MMP-9 proteolytic activity and the SNP -1562C>T in the promoter region of MMP9 gene are associated with the risk of developing PU in bedridden Tunisian patients.
Results
Clinical and epidemiological characteristics of the subjects suffering from pressure ulcer
Demographic and pressure injury risk assessment details of enrolled subjects suffering from PU are summarized in Supplementary Table S1. From those subjects, 50% were admitted to the emergency unit (27% in coma). The patients reported having at least 1 chronic health condition in addition to PU and this indicates polypathology which aggravate their state and sphincter incontinence. Indeed, there are several factors that increase the risk of developing PU in our patients such as impaired mobility, health conditions, poor nutrition, sepsis, urinary and fecal incontinence, lack of healthcare and consciousness.
PU can develop in any area of the body and the damage usually occurs over bony prominences. Our patients have generated 25% to 70% of wounds in the pelvic girdle (lower back, buttocks and greater trochanter), 5% to 55% of wounds occur in the lower legs, heel and lateral area of the foot and 5% to 15% occur in the upper (back of head, the headset and shoulder) (Fig. 1; Supplementary Fig. S1). PU stages (I to IV) (Fig. 2) and change color of tissue injury (Pink-Red-Green-Yellow-Black) are shown (Fig. 3).
Malnutrition may decrease the body’s ability to fight infections and have a negative impact on PU healing. The evaluation of nutritional status, using a variety of indexes and cutoff values used for anthropometric and biological assessment, demonstrates a bad nutrition state for our patients suffering from PU (Table 1).
Most patients (80%) had bacterial infections, caused mainly by gram-negative bacilli. However, the results of smear performed on surface wounds indicate that 1 to 2 species are present at the same time. During our study, it was found that enterobacteria represents the majority of isolated germ most of them are proteus mirabilis followed by stuartii providencia, pseudomonas aeruginosa, staphylococcus aureus, escherichia coli, klebsiella pneumonia, aciretobacterium baumanni and we also note the presence of staphylococcus haemolyticus, coagulase-negative staphylococci, serratia marcescens and polymorphic flora.
During stages of PU, some germs are most frequently found and the microflora of chronic wound fluctuates over time. By bacteriological examination guide carried out in the file of some patients, taking the example of results on a young sacred wound predominant gram-positive cocci (staphylococcus aureus). After week, it is the gram-negative bacilli which colonized the wound (escherichia coli and klebsiella pneumoniae). After a few weeks the two genera colonizing (staphylococcus aureus and pseudomonas aeruginosa) change after a few weeks to acetobacterium baumannii. Following our bacterial examination of a sacred necrotic wound and exposure of bone (stage IV), it is the gram-negative bacilli enterobacteriaceae colonizing the wound (klebsiella pneumoniae and pseudomonas aeruginosa). In total and according to records, 8 patients suffering from PU have presented this fluctuation. There is a limitation on this part because some patients do not present the bacteriological examination guide in their records.
The bacteria are subject to identification tests and in some cases of antibiotic sensitivity (antibiogram). The interpretation of the results of an antibiogram is extremely complex and is based on a comparison with known resistance phenotypes. For the majority of gram-negative bacilli belonging to enterobacteriaceae, which constitute the majority of germs identified in our study, amoxicillin and clavulanic acid association, the aminoglycosides, quinolones and cephalosporins may still be first-line prescribed in first intention for which there is a rise of resistance. For the gram-positive cocci represented in our study by the only staphylococcus, penicillin G, oxacilin M, amikacin (aminoglycoside) and quinolones can still be used as first intention with a wide margin of efficiency.
Demographic and biological characteristics of study population
The epidemiological and important biochemical characteristics of the participants are presented in Table 2 and are expressed as means ± standard deviations (SD) for quantitative variables.
Briefly, differences for fasting glucose, urea, creatinine levels, protide levels, cholesterol, triglycerides, high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), C-reactive protein (CRP), α1‐acid glycoprotein, albumin and prealbumin levels were detected between the two groups.
Subsequently, an imbalance between pro-oxidant and antioxidant systems seems to be more aggravated in patients with PU compared than healthy subjects. Serum homocysteine levels tended to be increased in patients whereas serum total antioxidant capacity (TAS) concentrations and thiobarbituric acid reactive substances (TBARS) were found lower than in controls.
Zymographic activity of matrix metalloproteinase-9
A representative gelatin zymogram of serum samples with all forms of MMP-9 commonly found in human is shown in Fig. 4. Three forms of MMP-9 were detected, including the homodimer of the pro-MMP-9 form (225 kDa), the pro-MMP-9 complexed with neutrophil gelatinase-associated lipocalin (NGAL) form (130 kDa) and the monomeric form of the pro-MMP-9 (92 kDa). The results of densitometry analysis are indicated in Supplementary Figs S2–S4 respectively. In our data, a statistically significant increase in protein activity of homodimer pro-MMP-9 (225 kDa) was noted in patients (25.7 ± 2.92%) compared with healthy subjects (16.78 ± 3.15%). The serum activity of the pro-MMP-9 complexed with NGAL (130 kDa) was significantly higher in patients with PU (9.37 ± 3.17%) compared to controls (6.2 ± 1.32%). Furthermore, a statistically significant increase in mean serum activity of the monomeric of pro-MMP-9 form (92 kDa) was present in patients with PU (58.32 ± 16.99%) than in controls (34.71 ± 10.33%).
Allele and genotype frequencies of the MMP9 -1562C/T polymorphism and risk of PU
In the current study, evaluation of Hardy-Weinberg equilibrium showed that the genotype frequencies of the MMP9 -1562C/T polymorphism were in Hardy-Weinberg equilibrium in both groups (p ≤ 0.05) (Supplementary Table S2).
Three distinct genotypes, based on the two alleles found, CC, CT and TT were observed in all analyzed populations (Fig. 5). The frequency distributions of different MMP9-1562C/T genotypes and alleles are summarized in Table 3.
Comparison of allele T frequencies showed statistically significant difference between patients suffering from PU in comparison with healthy subjects (odds ratio (OR) = 0.55, 95% confidence interval (CI) = [0.33–0.92], p = 0.021). The combined risk genotype (CT + TT) frequencies of SNP -1562 MMP9 also differed significantly between patients and controls (OR = 0.53, 95% CI = [0.3–0.93], p = 0.025). Therefore, the results indicated that the MMP9-1562C/T polymorphism is associated with PU and that the minor T allele may be a protective factor for this condition.
Discussion
PU causes serious complication that lead to severe or intolerable pain and increased morbidity and mortality rates affecting approximately 3 million adults25,26. These elevated rates indicate the existence of a problem that merits investigation, since it is known that in the majority of cases PU can be avoided by identification of risk factors and initiation of preventative measures27. Furthermore, PU is wound with multifactorial origins in which the cellular and molecular mechanisms contributing to massive destruction of deeper tissues need to be more defined. The present study was based on the assumption to evaluate the possible role of the predisposing factors in PU.
Although there is little reference in the literature regarding a relationship between PU and gender, among 15 studies included in the systematic review of Coleman et al. only four of them have shown an association between PU and gender28. In more recent studies, Ek et al. observed a greater occurrence of PU in women but gender is not considered to be a risk factor29 whereas Brandeis et al. find male gender was a risk factor for conversion and complications of PU30.
In 2004, Blanes et al. analyzed the relationship between age, gender and PU risk factors in a group of hospitalized patients with PU, they found a mean age of 64 years or women were 67.9 years old and were slightly older than the men 60.4 years31. In fact, older people are more susceptible to developing skin wounds because of age related skin changes, immobility that increases the risk of incontinence, cognitive impairment, lose muscle mass and gain weight.
Interestingly, our patients group comprises 44% of subjects over 60 years of age, 7% of them are aged more than 80 years and we state that men (74%) are at a higher risk of developing PU than women.
In addition, bedridden patients and those with cognitive impairment are more susceptible to PU development32. Indeed, almost all chronic wounds occur in a host with a predisposing condition such as venous disease, arterial and vascular compromise and neuropathy disease33. In the present study, neuropathy and cardiovascular diseases (cerebral vascular accident, heart failure, diabetes, hypertension and renal insufficiency) were the most frequently seen pre-existing diseases in the patient group.
Although the prevention of PU is a multidisciplinary responsibility, nutrition plays a fundamental part in wound healing, with malnutrition, dehydration and recent weight loss identified as independent risk factors for the development of PU. While the low levels of cholesterol, hemoglobin, albumin and micronutrients (vitamins A and C and zinc) are often quoted as independent predictors of PU risk28.
In particular, albuminemia remains an unreliable indicator of nutritional status because it may be more related to inflammation or hydration status than to malnutrition34. Other studies showed a lower albumin to be related to higher stages of PU. A low serum albumin has been suggested to promote PU formation through interstitial edema, reduced tissue oxygenation and nutrient flow35. In fact, our data showed that 41% of patients with hypoalbuminemia.
Subsequently, 48% of our patients with PU were found to be at severe nutritional risk according to NRI score. However, this is in agreement with the higher proportion of patient (52%) were found to be at severe nutritional condition according to PINI score (21 < PINI < 30 and PINI > 30). Our findings are in agreement with the results of previous studies displaying higher risk of various complications in malnourished patients with PU as compared to normal volunteers non-malnourished36,37. Poor nutritional status can lead to delay wound healing and increase risk of infection.
Chronic wounds are colonized by polymicrobial flora, originating from the external environment, local skin flora, the enteric tract, the vagina and oral mucosa38. In our study, we have isolated 10 bacterial strains, proteus mirabilis was the most common germ. Microflora of chronic wound fluctuates over time. Thus, on young wound predominantly gram-positive cocci. After a few weeks, the bacilli are gram negative which colonizes the wound.
The proliferation of gram-negative bacilli often manifests as a color change of wound and they appear to play a particularly important role during the detersion phase. However, infections by gram-positive cocci respect the appearance of the wound. They evolved towards the formation of a purulent pocket. This pocket can cause a fever and also be the starting point for the bacterial invasion of adjacent tissues38.
Indeed, infection is a common complication of PU and may be local (cellulitis, joints and bones) or distant. Joint infections (septic or infectious arthritis) can damage cartilage and tissue within days, whereas bone infections (osteomyelitis) may reduce the function of joints and limbs for years if not treated. One of the greatest dangers of an advanced PU, sepsis occurs when bacteria from a massive infection enter the bloodstream through broken skin and spread throughout the body. Such infections can lead to life-threatening complications that can cause shock and organ failure39. In the present study and according to their medical records, 21 patients have sepsis and clinical signs that the PU may be infected include malodorous, pain, purulent exudates and excessive bleeding in the ulcer.
Moreover, chronic wounds lead to persistent bacterial populations that are typically arranged into highly organized biofilms. The importance of biofilms in chronic wounds has been recently reviewed in detail40. High microbial burden leads to the presence of toxins or other factors within and around the wound. This process can lead to an excessive inflammatory reaction involved in the development of PU and other subsequent complications.
The inflammatory response can ultimately lead to the development of complex lesions and encourages a sustained release of cytotoxic enzymes, pro-inflammatory cytokines (interleukin-1, tumour necrosis factor-alpha) and free oxygen radicals41. This was illustrated by the significantly higher serum levels of nontraditional markers of subclinical inflammation, including CRP and α1‐acid glycoprotein, in our group of patients compared to controls. Additionally, inflammation is a key component against infection upon tissue injury in the pathogenesis of PU and is thought to play a key promoting role in oxidative stress42.
Oxidative stress is a state of altered physiological equilibrium within a cell or tissue/organ, defined as a condition arising when there is a serious imbalance between the levels of free radicals in a cell and its antioxidant defenses in favor of the former43. It not only causes hazardous events such as lipid peroxidation and oxidative deoxyribonucleic acid (DNA), ribonucleic acid (RNA) and proteins damage, but also physiologic adaptation phenomena and regulation of intracellular signal transduction44,45.
In our data, investigation about oxidative stress parameters shows a decreased serum TBARS level, as a lipid peroxidation marker and a drop in the TAS in patients with PU compared to healthy subjects. According to our observation, Taylor et al. have considered that the TBARS levels measured were predictive of the development of PU independently of lipids levels (total cholesterol, HDL-C, LDL-C and triglycerides), blood pressure, inflammatory markers, age and body mass index (BMI)46.
Furthermore, our patients with PU have significantly hyperhomocysteinaemia. Homocysteine reduces the transition metal ion (Mn+) to generate a thioyl radical (Hcy°). It is thought to react with homocysteine to generate a free radical intermediate that reduces oxygen to superoxide anion and then to peroxide hydrogen generation. The imbalance between pro-oxidant and antioxidant systems can be aggravated by homocysteine which is readily oxidized47.
Interestingly, several studies have investigated the expression and activity of MMP-9 in many physiological and pathological processes15,18,20. When present in the bed skin in large quantities and for long periods in the wrong places, it begins to degrade the extracellular matrix, inhibit cell migration and prevent wound closure48. However, Gumieiro et al. reported that pro-MMP-9 was associated with gait status recovery 6 months after hip fracture but was not associated with PU and mortality in hip fracture patients49. Some studies analyzing fluids and wound biopsies collected from PU patients showed overexpression of the active forms MMP-9. These data suggest that this protease could destroy the growth factors, receptors and extracellular proteins essential for the healing of PU19,21,50.
In the present study, our data revealed that the serum activity of the pro-MMP-9 increased more in the patients suffering from PU than the healthy subjects. This phenomenon can be explained by certain cells that secrete an excessive amount of MMP-9 into the circulation and also the decreased transformation from the inactive form to the active form of MMP-9. To our knowledge, our findings gave unprecedented evidence that the overexpression of MMP-9 protein is associated with PU. As a result, the serum pro-MMP-9 is a predictor of the wound healing process.
Because the expression of MMP-9 is primarily controlled by the rate of gene transcription, differences in promoter activity should be reflected in levels of MMP-9. Therefore, it is important to understand the factors that control the transcriptional response of this gene. Several SNP have been identified in the MMP-9 gene, including polymorphisms in the proximal promoter51.
Among these polymorphisms, the -1562C/T polymorphism in the MMP-9 promoter may reduce the rate of transcription by inhibiting protein binding, which down regulates MMP-9 expression52,53. Blankenberg et al. showed that -1562C>T polymorphism has an influence on MMP-9 transcription and that this effect is translated into differences in MMP-9 protein level and activity between individuals of different genotypes54.
A positive association of SNP -1562C>T in the MMP-9 gene has been reported with many diseases53. However no previous study investigated the relationship between PU and MMP-9 polymorphisms. In the present study, we assessed the association between MMP9 -1562C/T polymorphism and PU in Tunisian patients. Interestingly, the distribution of MMP9 -1562C/T genotypes and alleles frequencies were significantly different between PU patients and controls with the T allele conferring a lower risk for PU. These results suggest that a common functional MMP-9 promoter polymorphism (rs3918242) protects against PU and indicate that a rather modest change due to an SNP may result in considerable biological differences.
In summary, in medicine we must know the causes of disease and health. PU requires a large variety of medical care and patient with PU in Tunisia hospitals suffer from lack of healthcare and consciousness. The present data suggest that PU is a complex clinical problem with multiple influencing factors. Furthermore, the conventional risk factors such as age, gender, serum lipid levels and oxidative stress parameters showed different in our patient and control groups. Various molecules found in serum may be reliable markers for early diagnosis of PU. Measurements of albumin, CRP and homocysteine have been proposed as biochemical parameters able to increase diagnostic certainty.
In addition, MMP-9 is a gelatinase that exerts a variety of immunoregulatory activities and is thought to play a critical role in a number of pathophysiological conditions like PU and its acute complications. Therefore, an excess in MMP-9 appears to be an accurate prognostic markers of wound repair. Moreover, our study provided potential evidence of the association between MMP9-1562C/T polymorphism and the risk of PU and supported the hypothesis that the MMP9-1562 T allele variant might be a genetic marker for the risk of this disease. So the missing determination of plasma levels of MMP-9 and testing only SNP in the investigated gene represent the limitations of this study.
Of interest, these variables can be used as references to determine the priority needed to be given to some preventive measures and treatments and to identify the patients at risk. Future research should better establish the signaling pathway as well as predisposing factors to systemic infection and other studies need to be performed to investigate thoroughly the underlying cellular mechanisms and whether this knowledge can be used to develop novel therapeutic approaches.
Methods
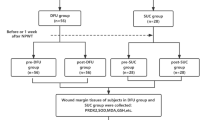
Study population
A total of 313 individuals, comprising 100 patients suffering from PU and 213 healthy controls, were enrolled in this study. Controls and patients were selected from the same population living in the central coast of Tunisia and including only unrelated subjects. 100 patients suffering from PU that met the following inclusion criteria: presenting at least a wound and confirmed diagnosis of PU, aged ≥18 years old, bedridden, not feeds only and without trophic and mental disorders. Exclusion criteria: pediatric study population, age >90 years old, allergy to wound products, malignant origin, obstetric and psychiatric patients were excluded55. These patients were recruited from the medical care units (emergency, orthopedic, physical medicine and surgical) at three University Regional hospitals in Tunisia (Farhat Hached/Sahloul Sousse and Fattouma Bourguiba Monastir). Healthy individuals (n = 213) were recruited from the outpatient services at the Farhat Hached Hospital (Sousse, Tunisia) and they were considered clinically free of PU and tissue necrosis. Informed consent was obtained from each participant or his legal representative. The study was approved by the national committee for medical and research ethics of the university hospital Farhat Hached in sousse - Tunisia and complied with the ethical principles of the WMA Declaration of Helsinki. The methods carried out in the study are in accordance with the approved relevant guidelines and regulations.
Blood collection and biochemical methods
Fasting venous blood samples were collected and immediately centrifuged at room temperature for 10 minute (mn) at 3000 rpm. Plasma levels glucose, total serum cholesterol, serum triglycerides, HDL-C and a renal profile (urea, creatinine and uric acid) levels were measured by a standard spectrophotometric method using reagents in a fully automated analyzer (Randox Antrim, UK; CX5 and CX9-BECKMANN). LDL-C was determined by Friedewald formula. Positive acute phase proteins such as CRP and α1‐acid glycoprotein were measured using immunoturbidimetric method (COBAS INTEGRA 400 Roche). Markers of nutritional status, albumin and prealbumin (negative acute phase proteins) were measured using the dry chemistry method (BN prospec, siemens). Total homocysteine in serum was measured by the Abbott homocysteine assay (AXSYM).
Evidence of lipid peroxidation was detected by measurement of TBARS in serum according to the fluorimetric method of Yagi56. The principle for the TBARS is based on TBA reacting with the LDL oxidation product, malondialdehyde (MDA), to produce TBA-reactive substances. Serum TBARS levels were measured at 515 nm excitation and 553 nm emission with the reference to a standard MDA solution prepared by acid hydrolysis of 1,1,3,3-tetraethoxypropane. The TAS was measured by colorimetric method at 600 nm according to the method of Miller et al. (Cat. No. NZ 2332; Randox Labs Ltd., Crumlin, UK). This test can evaluate the total capacity of all antioxidants found in biological sample to neutralize the oxidative action of free radicals57.
Swab sample collection
Only one wound per patient was cultured by swab to determine the bacterial species of the infection and help guide antibiotic therapy. The representative sample is collected before topical or systemic antibiotics are initiated and pain assessment should be conducted prior to wound procedures such as dressing changes and debridement. Immediately, the quantitative results of surface swab culture were evaluated at the microbiology laboratory of Farhat Hached Hospital in Sousse.
Nutritional status assessment
Malnutrition was determined by the presence of at least one of the following elements based on the previous studies in hospitals. Anthropometric evaluation was performed by the usual parameters: body weight (BW, Kg), body height (BH, m) and BMI was calculated using the formula: BMI (Kg/m2) = BW (Kg)/BH2 (m2). Biochemical evaluation of negative acute phase protein such as albumin (chronic marker of nutritional status) was measured by immunoenzymatic method.
Patients were scored according to Nutritional Risk Index (NRI) [NRI = (1.489× albumin) + (41.7× present weight/ideal body weight)] and categorized as follows: severe risk (NRI < 83.5), moderate risk (83.5 < NRI < 97.5) and no risk (NRI > 97.5). Prognostic Inflammatory and Nutritional Index (PINI) is a simple clinical assessment [PINI = α1‐acid glycoprotein × CRP/albumine × prealbumin] and classificated as follows to 4 categories: normal (1 < PINI score < 10), mild malnutrition (11 < PINI score < 20), severe malnutrition (21 < PINI score < 30) and risk for death when PINI score >30. These scores gained in popularity as it uses an objective rather than subjective measurements to determine nutritional risk in hospitalized patient populations58,59.
Mortality of patients with PU
For information on post discharge mortality, the hospital database was interrogated to determine patient’s vital status. Individuals who were noted to be alive on the database were contacted at least after 3 months after discharge via telephone to verify their status.
Gelatin Zymography of MMP-9
Previously, the MMP-9 proteolytic activity was measured by a relatively easy yet powerful technique known as zymography49. Each serum sample is mixed with 2x sample buffer consisting of 0.5 M Tris, pH 6.8, 100% glycerol and 0.5% bromophenol blue. Electrophoresis was carried into the wells of 8% sodium dodecyl sulfate-polyacrylamide gel (SDS-PAGE) containing 1% gelatin out using a mini protean II system (Bio-Rad) at 90 V for 2 hours. The run is complete when the bromophenol blue tracking dye reaches the bottom of the gel. After electrophoresis, the gel washed two steps in renaturing solution through 2.5% Triton X-100 and then with 50 mM Tris pH 8.4 on a rotatory shaker. For maximum sensitivity, each gel was incubated overnight (37 °C) in a developing solution and protect them with plastic film. After the water bath, the gel should be stained 2 times with 0.1% coomassie brilliant blue and then be stained twice more with bleach solution (40% methanol and 7% acetic acid) until reaching maximum objection to detect clear bands against a blue background of undegraded substrate. Moreover, the stained gels were scanned on Canon-Cano Scan LIDE 25 F91011 and the density of stained gelatinolytic band was measured by ImageJ or that rate was expressed as a percentage.
Genotyping of single nucleotide polymorphism (-1562C>T) MMP9
Genomic DNA was isolated from peripheral white blood cells using standard salting-out procedures. Genotyping of MMP9-1562C/T (rs 3918242) polymorphism in the study population (313 individuals) was performed using a polymerase chain reaction and restriction fragment length polymorphism (PCR-RFLP) method according to Wang et al.60 with the following changes: a 18 μl reaction volume mixture was prepared using sterile water, 3.6 μl of 5X buffer (50 mM KCl, 20 mM Tris-HCl, pH 8.4), 0.72 μl of 25 mM MgCl2, 0.36 μl of 10 uM of each allele specific primers [sense primer (5′-GCCTGGCACATAGTAGGCCC-3′) and antisense primer (5′-CTTCCTAGCCAGCCGGCATC 3′)], 0.36 μl of 20 mM dNTP, GoTaq® Flexi DNA Polymerase (0.09 U) (Promega, Madison, WI, USA) and 1 μl of 100 ng of genomic DNA.
Briefly, the PCR-RFLP consisted of a 5 mn denaturation step at 94 °C followed by 35 cycles at 94 °C for 30 second (s), 63.5° for 30 s, 72 °C for 50 s and a final extension at 72 °C for 10 mn.
The PCR products were digested overnight with 2 units of SphI (Jena Bioscience GmbH, Germany) at 37 °C and were analyzed by electrophoresis on a 2% agarose gel then stained with ethidium bromide before genotype assessment under ultraviolet light. The fragment sizes were 436 base pair (bp) (undigested) for the C allele whereas 194 and 242 bp for the polymorphic variant (T allele).
Data analysis
Database management and statistical analyses were carried out using Statistical Package for the Sociological Sciences (SPSS) version 18.0 and Epi info 6.0 softwares. Results are presented as means ± SD or the median and percentages. Means were compared using Student test. The significance threshold was set at 5% (p < 0.05).
Additional Information
How to cite this article: Latifa, K. et al. Evaluation of physiological risk factors, oxidant-antioxidant imbalance, proteolytic and genetic variations of matrix metalloproteinase-9 in patients with pressure ulcer. Sci. Rep. 6, 29371; doi: 10.1038/srep29371 (2016).
References
Black, J. M. et al. Medical device related pressure ulcers in hospitalized patients. Int Wound J. 7, 358–365 (2010).
Frankel, H., Sperry, J. & Kaplan, L. Risk factors for pressure ulcer development in a best practice surgical intensive care unit. Am Surg. 73, 1215–1217 (2007).
Campbell, K. E. A new model to identify shared risk factors for pressure ulcers and frailty in older adults. Rehabil Nurs. 34, 242–247 (2009).
Reddy, M., Gill, S. S. & Rochon, P. A. Preventing pressure ulcers: a systematic review. JAMA. 296, 974–984 (2006).
Vuagnat, H., Donnat, N. & Trombert, V. Elderly and bedsores: prevention and treatment. Rev Med Suisse. 8, 2295–2302 (2012).
Shahin, E. S., Dassen, T. & Halfens, R. J. Pressure ulcer prevalence and incidence in intensive care patients: a literature review. Nurs Crit Care. 13, 71–79 (2008).
Whitfield, M. D., Kaltenthaler, E. C., Akehurst, R. L., Walters, S. J. & Paisley, S. How effective are prevention strategies in reducing the prevalence of pressure ulcers? J. Wound Care. 9, 261–266 (2000).
Devillers, C., Piérard-Franchimont, C., Giet-Lesuisse, M. & Piérard, G. E. How I explore …. a pressure ulcer. Rev Med Liege. 64, 535–537 (2009).
Lahmann, N. A., Kottner, J., Dassen, T. & Tannen, A. Higher pressure ulcer risk on intensive care? Comparison between general wards and intensive care units. J. Clin Nurs. 21, 354–361 (2012).
Lyder, C. H. Pressure ulcer prevention and management. JAMA. 289, 223–226 (2003).
Nijs, N. et al. Incidence and risk factors for pressure ulcers in the intensive care unit. J. Clin Nurs. 18, 1258–1266 (2009).
Allman, R. M. Pressure ulcer prevalence, incidence, risk factors and impact. Clin Geriatr Med. 13, 421–437 (1997).
Lahmann, N. A., Dassen, T., Poehler, A. & Kottner, J. Pressure ulcer prevalence rates from 2002 to 2008 in German long-term care facilities. Aging Clin Exp Res. 22, 152–156 (2010).
Sprigle, S. & Sonenblum, S. Assessing evidence supporting redistribution of pressure for pressure ulcer prevention: a review. J. Rehabil Res Dev. 48, 203–213 (2011).
Mast, B. A. & Schultz, G. S. Interactions of cytokines, growth factors and proteases in acute and chronic wounds. Wound Repair and Regeneration. 4, 411–420 (1996).
Velnar, T., Bailey, T. & Smrkolj, V. The wound healing process: an overview of the cellular and molecular mechanisms. J. Int Med Res. 37, 1528–1542 (2009).
Cox, J. Predictors of pressure ulcers in adult critical care patients. Am J Crit Care. 20, 364–375 (2011).
Stamenkovic, I. Extracellular matrix remodelling: the role of matrix metalloproteinases. J. Pathol. 200, 448–464 (2003).
Ladwig, G. P. et al. Ratios of activated matrix metalloproteinase-9 to tissue inhibitor of matrix metalloproteinase-1 in wound fluids are inversely correlated with healing of pressure ulcers. Wound Repair Regen. 10, 26–37 (2002).
Yager, D. R., Zhang, L. Y., Liang, H. X., Diegelmann, R. F. & Cohen, I. K. Wound fluids from human pressure ulcers contain elevated matrix metalloproteinase levels and activity compared to surgical wound fluids. J. Invest Dermatol. 107, 743–748 (1996).
Rayment, E. A., Upton, Z. & Shooter, G. K. Increased matrix metalloproteinase-9 (MMP-9) activity observed in chronic wound fluid is related to the clinical severity of the ulcer. Br J Dermatol. 158, 951–961 (2008).
Vandooren, J., Van den Steen, P. E. & Opdenakker, G. Biochemistry and molecular biology of gelatinase B or matrix metalloproteinase-9 (MMP-9): the next decade. Crit Rev Biochem Mol Biol. 48, 222–272 (2013).
Ye, S. Polymorphism in matrix metalloproteinase gene promoters: implication in regulation of gene expression and susceptibility of various diseases. Matrix Biol. 19, 623–629 (2000).
Skarmoutsou, E. et al. Analysis of matrix metalloproteinase-9 gene polymorphism -1562C/T in patients suffering from systemic sclerosis with and without ulcers. Int J Mol Med. 27, 873–877 (2011).
Oliveira Costa, A. C., Sabino Pinho, C. P., Almeida Dos Santos, A. D. & Santos do Nascimento, A. C. Pressure ulcer: incidence and demographic, clinical and nutrition factors associated in intensive care unit patients. Nutr Hosp. 32, 2242–2252 (2015).
Eckman, K. L. The prevalence of dermal ulcers among persons in the U.S. who have died. Decubitus. 2, 36–40 (1989).
Santos, C. T., Almeida Mde, A., Oliveira, M. C., Victor, M. A. & Lucena Ade, F. Development of the nursing diagnosis risk for pressure ulcer. Rev Gaucha Enferm. 36, 113–121 (2015).
Coleman, S. et al. Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. 50, 974–1003 (2013).
Ek, A. C. & Boman, G. A descriptive study of pressure sores: the prevalence of pressure sores and the characteristics of patients. J. Adv Nurs. 7, 51–57 (1982).
Brandeis, G. H., Ooi, W. L., Hossain, M., Morris, J. N. & Lipsitz, L. A. A longitudinal study of risk factors associated with the formation of pressure ulcers in nursing homes. J. Am Geriatr Soc. 42, 388–392 (1994).
Blanes, L., Duarte, I. S., Calil, J. A. & Ferreira, L. M. Clinical and epidemiological evaluation of pressure ulcers in hospitalized patients in the São Paulo hospital. Rev Assoc Med Bras. 50, 182–187 (2004).
O’Brien, S. P., Gahtan, V., Wind, S. & Kerstein, M. D. What is the paradigm: hospital or home health care for pressure ulcers? Am Surg. 65, 303–306 (1999).
Kemp, M. G., Keithley, J. K., Smith, D. W. & Morreale, B. Factors that contribute to pressure sores in surgical patients. Res Nurs Health. 13, 293–301 (1990).
Nonnemacher, M. et al. Predicting pressure ulcer risk: a multifactorial approach to assess risk factors in a large university hospital population. J. Clin Nurs. 18, 99–107 (2009).
Mathus-Vliegen, E. M. Old Age, malnutrition and pressure sores: an Ill-Fated Alliance. J. Gerontol A Biol Sci Med Sci. 59, 355–360 (2004).
Finucane, T. E. Malnutrition, tube feeding and pressure sores: data are incomplete. J. Am Geriatr Soc. 43, 447–451 (1995).
Roberts, S., Chaboyer, W. & Desbrow, B. Nutrition care-related practices and factors affecting nutritional intakes in hospital patients at risk of pressure ulcers. J. Hum Nutr Diet. 28, 357–365 (2015).
Ebright, J. R. Microbiology of chronic leg and pressure ulcers: clinical significance and implications for treatment. Nurs Clin North Am. 40, 207–216 (2005).
Daltrey, D. C., Rhodes, B. & Chattwood, J. G. Investigation into the microbial flora of healing and non-healing decubitus ulcers. J. Clin Pathol. 34, 701–705 (1981).
Percival, S. L., Hill, K. E., Williams, D. W., Hooper, S. J., Thomas, D. W. & Costerton, J. W. A review of the scientific evidence for biofilms in wounds. Wound Repair Regen. 20, 647–657 (2012).
Martin, J. M., Zenilman, J. M. & Lazarus, G. S. Molecular microbiology: new dimensions for cutaneous biology and wound healing. J. Invest Dermatol. 130, 38–48 (2010).
Gruys, E., Toussaint, M. J., Niewold, T. A. & Koopmans, S. J. Acute phase reaction and acute phase proteins. J. Zhejiang Univ Sci B. 6, 1045–1056 (2005).
Betteridge, D. J. What is oxidative stress? Metabolism. 49, 3–8 (2000).
Gutteridge, J. M. C. Free radicals in disease process a compilation of cause and consequence. Free Rad Res Comms. 19, 141–158 (1993).
Cordeiro, M. B. et al. Oxidative stress and acute-phase response in patients with pressure sores. Nutrition. 21, 901–907 (2005).
Taylor, R. & James, T. The role of oxidative stress in the development and persistence of pressure ulcers (eds Bader, D., Bouten, C., Colin, D. & Oomens, C. ) 205–232 (Springer Berlin Heidelberg, 2005).
Hogg, N. The effect of cyst(e)ine on the auto-oxidation of homocysteine. Free Radic Biol Med. 27, 28–33 (1999).
Sekhon, B. S. Matrix metalloproteinases – an overview. Res Rep Biol. 1, 11–20 (2010).
Gumieiro, D. N. et al. Serum metalloproteinases 2 and 9 as predictors of gait status, pressure ulcer and mortality after hip fracture. PLoS One. 8, e57424 (2013).
Mast, B. A. & Schultz, G. S. Interactions of cytokines, growth factors and proteases in acute and chronic wounds. Wound Rep Reg. 4, 411–420 (1996).
Yabluchanskiy, A., Ma, Y., Iyer, R. P., Hall, M. E. & Lindsey, M. L. Matrix metalloproteinase-9: many shades of function in cardiovascular disease. Physiology. 28, 391–403 (2013).
Zhang, X., Cao, X., Xu, X., Li, A. & Xu, Y. Correlation between the -1562C/T polymorphism in the matrix metalloproteinase-9 gene and hemorrhagic transformation of ischemic stroke. Exp Ther Med. 9, 1043–1047 (2015).
Singh, K., Agrawal, N. K., Gupta, S. K. & Singh, K. A functional single nucleotide polymorphism -1562C>T in the Matrix Metalloproteinase-9 promoter is associated with type 2 diabetes and diabetic foot ulcers. Int J Low Extrem Wound 12, 199–204 (2013).
Blankenberg, S. et al. Plasma concentrations and genetic variation of matrix metalloproteinase 9 and prognosis of patients with cardiovascular disease. Circulation. 107, 1579–1585 (2003).
Khlifi, L. et al. Analysis of tumor necrosis factor G238A and G308 A gene polymorphisms in Tunisian patients with pressure ulcers. IJPSR. 7, 976–983 (2016).
Yagi, K. A simple fluorometric assay for lipoperoxide in blood plasma. Biochem Med. 15, 212–216 (1976).
Miller, N. J., Rice-Evans, C., Davies, M. J., Gopinathan, V. & Milner, A. A novel method for measuring antioxidant capacity and its application to monitoring the antioxidant status in premature neonates. Clin Sci. 84, 407–412 (1993).
Prendergast, J. M. et al. Clinical validation of a nutritional risk index. J. Community Health. 14, 125–135 (1989).
Ingenbleek, Y. & Carpentier, Y. A. A prognostic inflammatory and nutritional index scoring critically ill patients. Int J Vitam Nutr Res. 55, 91–101 (1985).
Wang, L. et al. Association of MMP-9 gene polymorphisms with acute coronary syndrome in the Uygur population of China. World J Emerg Med. 2, 104–110 (2011).
Acknowledgements
We owe special thanks to the patients and volunteers for their collaboration and the staff of the biochemistry laboratory Farhat Hached University Hospital, Sousse (Tunisia) for their precious technical support and M. Jalel BOUKADIDA in laboratory of Microbiology and Immunology, CHU Farhat HACHED of Sousse (Tunisia) for their valuable contribution in this work.
Author information
Authors and Affiliations
Contributions
The idea for the research or article, framing of hypothesis: K.L. and M.A. Planning the methods to generate results: K.L. and F.S. Oversight and responsibility for the organization and course of the project and the manuscript: K.L. and M.A. Dollars, equipment, space, personnel vital to the project: K.L. and M.A. Biological materials, reagents, referred patients: K.L., M.A. and F.S. Responsibility for doing experiments, managing patients, organizing and reporting data: K.L., S.S., G.H. and B.N. Responsibility for making sense of and presenting the results: K.L., B.-H.-M.M, K.S. and A.G. Responsibility for this necessary function: M.A. All the authors contributed in manuscript writing. All authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Latifa, K., Sondess, S., Hajer, G. et al. Evaluation of physiological risk factors, oxidant-antioxidant imbalance, proteolytic and genetic variations of matrix metalloproteinase-9 in patients with pressure ulcer. Sci Rep 6, 29371 (2016). https://doi.org/10.1038/srep29371
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29371
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.