Abstract
The aims of this study were to investigate the correlation between renal and cardiac STIs, including pre-ejection period (PEP), ejection time (ET), and PEP/ET, and to assess the diagnostic values of renal STIs in predicting left ventricular ejection fraction (LVEF) <50%. The cross sectional observation study enrolled 230 participants. The renal STIs, including renal PEP (rPEP), renal ET (rET), and rPEP/rET, were measured from electrocardiographic gated renal Doppler ultrasound and cardiac PEP, ET, and PEP/ET were measured from echocardiography. Renal STIs were correlated with cardiac STIs (all P < 0.001). Multivariate analyses showed that rPEP/rET was independently associated with LVEF (unstandardized coefficient β = −0.116, P = 0.046) and LVEF <50% (odds ratio = 2.145, per 0.11 increase; P = 0.017). The areas under the curve for rPEP, 1/rET, and rPEP/rET in predicting LVEF <50% were 0.773, 0.764, and 0.821, respectively. The sensitivity and specificity of rPEP/rET > 0.46 in prediction of LVEF <50% were 76.7% and 78.1%, respectively. Our study demonstrated that the novel parameters of renal STIs were significantly associated with cardiac STIs. However, the clinical application of renal STIs needs to be investigated in future studies.
Similar content being viewed by others
Introduction
Periods of cardiac cycles, particularity left ventricular systolic time intervals (STIs), were established for fifty years ago1,2. STIs, including pre-ejection period (PEP), ejection time (ET), and ratio of PEP to ET measured from invasive intra-cardiac hemodynamic technique, non-invasive arterial pulse recording, or echocardiography, were useful parameters of cardiac systolic performance1,2,3. PEP measured from onset of electrocardiographic QRS complex to aortic valve opening is meaning of the time interval from onset of ventricular depolarization to the start of ventricular ejection. ET is the time period from beginning to termination of ventricular ejection or arterial upstroke3,4. Increased PEP, decreased ET, and increased PEP/ET have been reported to be significantly correlated with decreased left ventricular ejection fraction (LVEF)5,6,7. STIs were widely measured from pulse Doppler or tissue Doppler echocardiography8,9. Echocardiography derived STIs were investigated in patients with heart failure, coronary diseases, or under cardiac resynchronization therapy10,11,12. STIs were also measured from non-invasive arterial pulse recording, phonocardiography, and electrocardiography. Our previous study demonstrated that brachial PEP, brachial ET, and brachial PEP/ET measured from an automatic device were significant associated with LVEF13. Recently, Polak et al. found ET measured from only Doppler waveform of carotid artery was also significantly associated with LVEF14. However, Polak et al. did not investigate PEP and PEP/ET from arterial Doppler waveform. The applications of STIs are makers of global cardiac systolic function and predictors of adverse cardiac outcome in patients with heart failure3,4,15.
Owing to high cardiovascular morbidity and mortality, the increasing number of patients with chronic kidney disease (CKD) is an important healthcare issue in the world16,17. Renal ultrasonography is an useful image tool in noninvasive evaluation of renal anatomic and vascular information in patients with renal injury18. In addition to conventional gray-scale image, renal Doppler ultrasound can help to evaluate intra-renal vascular information. The popular parameter measured from renal Doppler ultrasound is renal resistive index (RI). Renal RI can reflect vascular resistance and serve as a predictor of renal damage and poor cardiovascular outcome19,20,21. Furthermore, renal RI was associated with left ventricular diastolic dysfunction20, but not associated with LVEF22.
Although STIs measured from Doppler ultrasound were associated with global cardiac systolic function, there was no study to evaluate whether renal STIs measured from renal Doppler ultrasound were also associated with cardiac systolic function. Hence, the aims of this study were to investigate the relationship between renal STIs measured from real-time internal electrocardiographic (ECG) gated renal Doppler ultrasound and cardiac STIs measured from echocardiography and to assess the diagnostic values of renal STIs in prediction of LVEF <50%23.
Methods
This is a cross-sectional observation study enrolled participants who received echocardiographic examination due to suspected cardiovascular diseases in a regional hospital in Taiwan from June 2012 to December 2012 (Fig. 1). Patients with atrial fibrillation (number, n = 4), significant aortic or mitral valve diseases (n = 2), left bundle branch block (n = 1), inadequate image visualization (n = 3), history of unilateral or bilateral renal artery stenosis (n = 0), unilateral or bilateral nephrectomy (n = 2), end stage renal disease receiving renal replacement or renal transplantation therapy (n = 3), acute kidney injury (n = 2), and acute unilateral or bilateral hydronephrosis (n = 5) were excluded.
Ethics statement
The study methods were carried out in accordance with the approved guidelines. The study protocols were approved by the institutional review board committee of the Kaohsiung Medical University Hospital (KMUHIRB-E(II)-20160015). Written informed consent was obtained from all subjects.
Renal Doppler ultrasound study
Ultrasonographic examinations were performed using multi-functional duplex Doppler ultrasonography with a CX50 (Philips) ultrasound machine with a 2.5-MHz pulsed Doppler frequency and a 3.5-MHz convex array transducer. The image of the kidneys was determined by B-mode and renal blood flow was visualized with color-Doppler sonography superimposed on B-mode image while the patient was in the supine position. We applied internal ECG signal into Doppler ultrasound. Then, intra-renal Doppler signals were obtained from the arcuate arteries at the cortico-medullary junction. The renal RI was calculated as (peak systolic velocity – minimum diastolic velocity)/peak systolic velocity24. The renal PEP (rPEP) was measured from the onset of the QRS complex to the foot of the renal pulse Doppler waveform. The renal ET (rET) was measured from the foot to the dicrotic notch of the renal pulse Doppler waveform (Fig. 2). The rPEP and rET were determined three times for each kidney and then the values from bilateral kidneys were averaged to obtain the mean value for later analysis. All measurements were performed by one experienced physician who was blinded to the other data of the subjects.
Echocardiographic assessment
A single experienced cardiologist performed all echocardiographic examination and acquired image using the Vivid 7 (General Electrics). Left ventricular internal diameter (LVID), interventricular septal wall thickness (IVST), left ventricular posterior wall thickness (LVPWT), trans-mitral E wave velocity (E), E-wave deceleration time, trans-mitral A wave velocity and early diastolic mitral velocity (Ea), were measured by standard chamber quantification and measurement13,25. We calculated LVEF and Left ventricular mass by the modified Simpson’s method and the Devereux-modified method, respectively26. Left ventricular mass index was calculated by dividing left ventricular mass by body surface area. PEP was measured from the onset of the QRS complex on the electrocardiogram to the onset of systolic flow from the left ventricular outflow tract (LVOT). ET was measured from the onset to the end of LVOT systolic flow13. The PEP and ET were obtained from 3 consecutive beats and then the data were averaged to give the mean value for later analysis. All echocardiographic parameters were acquired from 3 continued beats and measured from offline EchoPAC software by a single experienced cardiologist.
Collection of demographic, medical, and laboratory data
Baseline medication, personal characteristic, and laboratory data were collected from medical records. The value of estimated glomerular filtration rate (eGFR) was calculated by the equation of Modification of Diet in Renal Disease study27. Participants with CKD were defined as those with evidence of kidney damage lasting for more than 3 months28 and an eGFR <60 ml/min/1.73m2.
Reproducibility
Thirty patients were randomly selected for evaluation of the interobserver variability of renal STIs measurement by two independent observers. To obtain intraobserver variability, the same measurement was repeated 1 week apart. Mean percentage error was calculated as the absolute difference divided by the average of the two observations.
Statistical analyses
Baseline data are expressed as percentages or mean ± standard error. The differences in items between renal and echocardiographic STIs were checked by Student’s t-test. The relationship between two continuous variables was assessed using a bivariate correlation method (Pearson’s correlation). Bland-Altman plots were used to assess the agreements between renal and echocardiographic STIs. The regression of the average and the difference between renal and echocardiographic STIs (renal STIs minus echocardiographic STIs) was analyzed. Significant variables in the univariate analysis were further analyzed by multivariate stepwise linear regression and backward logistic regression to identify the determinants of LVEF and LVEF <50%, respectively. Receiver operating characteristic (ROC) curve was constructed for the prediction of LVEF <50%. A difference was considered significant if the P value was less than 0.05. Statistical analysis was performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 230 participants (age 64.0 ± 12.2 years, male 61.5%) enrolled in this study. Table 1 shows the clinical, echocardiographic, and renal Doppler ultrasonographic characteristics of these patients. The mean values of renal RI, rPEP, rET, and rPEP/rET were 0.69 ± 0.08, 123.7 ± 23.7 ms, 303.0 ± 36.8 ms, and 0.42 ± 0.11, respectively. The mean values of PEP, ET, and PEP/ET were 67.7 ± 15.1 ms, 294.8 ± 34.5 ms, and 0.23 ± 0.07, respectively.
Table 2 displays the determinants of LVEF and LVEF <50% according to univariate analysis in the study subjects. Male gender, diabetes, congestive heart failure, increased heart rate, increased triglyceride, decreased eGFR, increased glucose, use of β-blockers, no use of calcium channel blockers, use of diuretics, increased rPEP, decreased rET, increased rPEP/rET, increased PEP, decreased ET, and increased PEP/ET were significantly associated with decreased LVEF in the univariate linear analysis (P ≦ 0.017). Additionally, male gender, diabetes, congestive heart failure, increased heart rate, increased triglyceride, decreased eGFR, increased glucose, use of β-blockers, use of diuretics, increased rPEP, decreased rET, increased rPEP/rET, increased PEP, decreased ET, and increased PEP/ET were significantly associated with LVEF <50% in the univariate logistic analysis (P ≦ 0.032).
Table 3 shows the determinants of LVEF and LVEV <50% by multivariable linear and logistic analyses. In the linear and logistic multivariate models, covariates included the significant variables in univariate analysis (in Table 2) plus rPEP, rET, rPEP/rET and PEP, ET, PEP/ET, respectively. In multivariable linear model, rPEP/rET (unstandardized coefficient β = −0.116, P = 0.046), PEP (unstandardized coefficient β = −0.002, P < 0.001), and PEP/ET (unstandardized coefficient β = −0.508, P < 0.001) were significantly associated with increased LVEF. In multivariable logistic model, rET (odds ratio = 0.970, P = 0.008), rPEP/rET (odds ratio = 2.145 per 0.11 increase, P = 0.017), PEP (odds ratio = 1.105, P = 0.007), ET (odds ratio = 0.970, P = 0.028), and PEP/ET (odds ratio = 5.114 per 0.07 increase, P = 0.004) were significantly associated with LVEF <50%.
In the Pearson’s correlation analyses, LVEF was significantly correlated with rPEP (r = −0.338), rET (r = 0.317), rPEP/rET (r = −0.430), PEP (r = −0.477), ET (r = 0.251), and PEP/ET (r = −0.517) (all P < 0.001). However, LVEF was not significantly associated with renal RI (r = −0.046, P = 0.482). Figure 3 shows the scatter plots between rPEP and PEP (r = 0.477, P < 0.001) (Fig. 3A), rET and ET (r = 0.799, P < 0.001) (Fig. 3B), and rPEP/rET and PEP/ET (r = 0.619, P < 0.001) (Fig. 3C). To assess the agreement between renal and echocardiographic STIs, Bland-Altman plots were produced. The mean value of rPEP minus PEP was 56.13 ms and the 95% limit of agreement was 14.56 to 97.90 ms (Fig. 3D). The mean value of rET minus ET was 7.96 ms and the 95% limit of agreement was −36.33 to 52.25 ms (Fig. 3E). Finally, the mean value of rPEP/rET minus PEP/ET was 0.19 and the 95% limit of agreement was 0.01 to 0.37 (Fig. 3F).
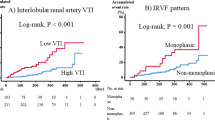
Figure 4 shows the ROC curves for rPEP, 1/rET, and rPEP/rET (Fig. 4A) and PEP, 1/ET, and PEP/ET (Fig. 4B) in prediction of LVEF <50%. The areas under the curve (AUCs) for rPEP, 1/rET, and rPEP/rET in prediction of LVEF <50% were 0.773, 0.764, and 0.821, respectively (all P < 0.001). In addition, the AUCs for PEP, ET, and PEP/ET in prediction of LVEF <50% were 0.826, 0.716, and 0.860, respectively (all P < 0.001).
The areas under the curve (AUCs) for renal pre-ejection period (rPEP), 1/renal ejection time (rET), and rPEP/rET measured from renal Doppler ultrasound (A) and pre-ejection period (PEP), 1/ejection time (ET), and PEP/ET measured from echocardiography (B) in prediction of left ventricular ejection fraction <50%.
Table 4 shows the statistical values of rPEP, rET, rPEP/rET, PEP, ET, and PEP/ET in prediction of LVEF <50%.
The intra-observer mean percentage errors (95% confidence interval) for renal PEP, renal ET, and renal PEP/ET measurement were 3.7 ± 4.1% (<0.1%, 13.9%), 2.0 ± 1.9% (<0.1%, 6.3%), and 5.0 ± 5.3% (<0.1%, 14.3%), respectively. The inter-observer mean percentage errors (95% confidence interval) for renal PEP, renal ET, and renal PEP/ET measurement were 4.1 ± 5.3% (<0.1%, 14.6%), 3.3 ± 1.8% (<0.1%, 8.9%), and 8.4 ± 5.7% (<0.1%, 19.8%), respectively.
Discussion
In the present study, we found that renal STIs derived from ECG gated renal Doppler ultrasonography were significantly associated with cardiac STIs measured from echocardiography and were useful in identification of patients with LVEF <50%.
Cardiac STIs affected by many physiological and pharmacologic factors are well-established parameters in assessment of global cardiac performance3,29,30,31,32. In general, cardiac STIs may be affected by several medications, such as digitalis glycosides, catecholamines, propranolol, amyl nitrate, and calcium gluconate, through positive or negative inotropic effects31,32. The physiological meaning of cardiac PEP is composed of isovolumetric contraction time and electromechanical delay, i.e. time interval between initiation of ventricular depolarization and aortic valve opening3,29,33. Regardless of causes of heart failure, increased cardiac PEP is resulted from a decreased rate of left ventricular pressure rise (dP/dt) during isovolumic contraction period3,34. The PEP may prolong when patients with impairment of cardiac contractility, left bundle branch block, use of negative inotropic agents, decreased preload status, or increased afterload pressure31,32. The PEP may shorten when patients with aortic valve disease, use of positive inotropic agents, increased preload status, or decreased afterload pressure. Although the physiological meaning of cardiac ET is the period from beginning to finishing of left ventricular ejection, the factors contributed to ET are more complex3. The length of PEP, preload condition, strength of myocardial fiber, and inotropic agents are associated with ET period3,29. Unlike PEP, which respectively became shorten and lengthen by positive and negative inotropic agents, ET became shorten both by positive and negative inotropic agents35,36. Although Polak et al. showed ET measured from Doppler waveform of carotid artery was significantly associated with LVEF, they did not further evaluate their relationship by multivariate analysis14. In this study, all the parameters of renal STIs were correlated with LVEF and useful in prediction of LVEF <50% in the univaiable analyses. Because gender, heart rate, clinical comorbidity, and medication use might influence STIs, we also assessed the determinants of renal STIs from different multivariate models3,13,31. Instead of rPEP and rET, rPEP/rET was still an independent determinant of LVEF and useful in prediction of patients with LVEF <50% in the multivariable analyses.
Although renal Doppler ultrasound was a popular image modality for evaluation of intra-renal hemodynamics, there were few studies researching the relationship between parameters of renal Doppler ultrasound and cardiac systolic function20,37. In our present study, renal RI was not significantly associated with LVEF. Hence, renal RI might be not a useful parameter in identification of patients with impaired left ventricular systolic function. Additionally, in the present study, cardiac PEP was calculated from onset of QRS to beginning of flow of left ventricular outflow tract. However, rPEP was calculated from onset of QRS to the foot of renal Doppler waveform. Because of the delay of arterial pulse wave from aorta to renal arcuate artery, rPEP was longer (mean difference 56.13 ms) than cardiac PEP in the present study. The physiological meaning of rPEP is composed of isovolumetric contraction time, electromechanical delay, and transmission of arterial pulse wave, i.e. time interval from initiation of ventricular depolarization to the foot of renal pulse Doppler waveform. Hence, renal STIs may be influenced by cardiac systolic function and arterial stiffness.
There were several different measurement methods of STIs. In the method developed by Weissle et al., they simultaneously recorded carotid pulse tracing, phonocardiography, and electrocardiography and then calculated STIs1. Recently, a radial artery tonometry was also used to evaluate STIs. In this method, they used high-fidelity pressure transducer, electrocardiography, and special software program to measure STIs38. In addition, brachial STIs could be automatically measured from an ABI-form device by an oscillometric method13. In the above methods, the high quality and complex equipments were needed to acquire the STIs. In the present study, when performing the renal echo, we used internal ECG signal and renal Doppler waveform to measure renal STIs. This method did not require additional complex equipment and software. Hence, our measurement of renal STIs had several advantages including cost-effectiveness, no need of extra operation, and renal-time calculation. Although echocardiography has been widely used for diagnosis and assessment of global cardiac function, the measurement of LVEF is difficult in patients with poor image visualization, extreme obesity, and severe pulmonary diseases33. Cardiac STIs and perhaps renal STIs were alternative parameters for evaluation of global left ventricular systolic function in these patients33. Hence, using renal Doppler ultrasonography, in addition to calculation RI to evaluate intra-renal vascular information, we can extra measure renal STIs to roughly assess global left ventricular systolic function.
Study limitations
There were several limitations to our study. First, our study was a cross-sectional observation design and only enrolled small number of cases in one regional hospital, which might limit study generality and cause selected bias. Second, due to lack of laboratory biomarkers of heart failure39, such as brain natriuretic peptide, N-terminal pro-brain natriuretic peptide, galectin-3, or N-terminal propeptide of procollagen type III, we did not know the relationship between those biomarkers and renal STIs. Finally, lack of echocardiographic parameters of right ventricle40, we did not recognize the associations between renal STIs and right ventricular function.
Conclusions
Our study demonstrated that the novel parameters of renal STIs were significantly associated with cardiac STIs. Additionally, rPEP/rET was associated with LVEF and useful in prediction of patients with LVEF <50%. However, the clinical application of renal STIs needs to be investigated in future large-scale studies.
Additional Information
How to cite this article: Lee, W.-H. et al. Systolic time intervals derived from electrocardiographic gated intra-renal artery Doppler waveform associated with left ventricular systolic function. Sci. Rep. 6, 29293; doi: 10.1038/srep29293 (2016).
References
Weissler, A. M., Harris, W. S. & Schoenfeld, C. D. Systolic time intervals in heart failure in man. Circulation 37, 149–159 (1968).
Van de Werf, F., Piessens, J., Kesteloot, H. & De Geest, H. A comparison of systolic time intervals derived from the central aortic pressure and from the external carotid pulse tracing. Circulation 51, 310–316 (1975).
Lewis, R. P., Rittogers, S. E., Froester, W. F. & Boudoulas, H. A critical review of the systolic time intervals. Circulation 56, 146–158 (1977).
Ahmed, S. S., Levinson, G. E., Schwartz, C. J. & Ettinger, P. O. Systolic time intervals as measures of the contractile state of the left ventricular myocardium in man. Circulation 46, 559–571 (1972).
Garrard, C. L. Jr., Weissler, A. M. & Dodge, H. T. The relationship of alterations in systolic time intervals to ejection fraction in patients with cardiac disease. Circulation 42, 455–462 (1970).
Veyrat, C., Larrazet, F. & Pellerin, D. Renewed interest in preejectional isovolumic phase: new applications of tissue Doppler indexes: implications to ventricular dyssynchrony. Am J Cardiol 96, 1022–1030 (2005).
Gillebert, T. C., Van de Veire, N., De Buyzere, M. L. & De Sutter, J. Time intervals and global cardiac function. Use and limitations. Eur Heart J 25, 2185–2186 (2004).
Su, H. M. et al. Correlation of Tei index obtained from tissue Doppler echocardiography with invasive measurements of left ventricular performance. Echocardiography 24, 252–257 (2007).
Chu, C. Y. et al. Myocardial performance index derived from pre-ejection period as a novel and useful predictor of cardiovascular events in atrial fibrillation. J Cardiol 65, 466–473 (2015).
Reant, P. et al. Systolic time intervals as simple echocardiographic parameters of left ventricular systolic performance: correlation with ejection fraction and longitudinal two-dimensional strain. Eur J Echocardiogr 11, 834–844 (2010).
Chirife, R. et al. The systolic index: a noninvasive approach for the assessment of cardiac function: implications for patients with DDD and CRT devices. Pacing Clin Electrophysiol 36, 1284–1293 (2013).
Lewis, R. P., Boudoulas, H., Welch, T. G. & Forester, W. F. Usefulness of systolic time intervals in coronary artery disease. Am J Cardiol 37, 787–796 (1976).
Su, H. M. et al. A comparison between brachial and echocardiographic systolic time intervals. Plos One 8, e55840 (2013).
Polak, J. F., Alessi-Chinetti, J. M., Estes, J. M. & Patel, A. R. Left Ventricular Ejection Time Derived From the Common Carotid Artery Doppler Waveform: Association With Left Ventricular Ejection Fraction and Prediction of Heart Failure. J Ultrasound Med 34, 1237–1242 (2015).
Shapiro, M. et al. Diagnostic characteristics of combining phonocardiographic third heart sound and systolic time intervals for the prediction of left ventricular dysfunction. J Card Fail 13, 18–24 (2007).
Levey, A. S. et al. Chronic kidney disease as a global public health problem: approaches and initiatives - a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 72, 247–259 (2007).
Meguid El Nahas, A. & Bello, A. K. Chronic kidney disease: the global challenge. Lancet 365, 331–340 (2005).
Bude, R. O. & Rubin, J. M. Relationship between the resistive index and vascular compliance and resistance. Radiology 211, 411–417 (1999).
Ikee, R. et al. Correlation between the resistive index by Doppler ultrasound and kidney function and histology. Am J Kidney Dis 46, 603–609 (2005).
Tedesco, M. A., Natale, F., Mocerino, R., Tassinario, G. & Calabro, R. Renal resistive index and cardiovascular organ damage in a large population of hypertensive patients. J Hum Hypertens 21, 291–296 (2007).
Krumme, B. Renal Doppler sonography–update in clinical nephrology. Nephron Clin Pract 103, c24–c28 (2006).
Raff, U. et al. Renal resistive index in addition to low-grade albuminuria complements screening for target organ damage in therapy-resistant hypertension. J Hypertens 28, 608–614 (2010).
Takeda, Y. et al. Competing risks of heart failure with preserved ejection fraction in diabetic patients. Eur J Heart Fail 13, 664–669 (2011).
Gerhard-Herman, M. et al. Guidelines for noninvasive vascular laboratory testing: a report from the American Society of Echocardiography and the Society for Vascular Medicine and Biology. Vasc Med 11, 183–200 (2006).
Lang, R. M. et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18, 1440–1463 (2005).
Devereux, R. B. et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57, 450–458 (1986).
Vickery, S., Stevens, P. E., Dalton, R. N., van Lente, F. & Lamb, E. J. Does the ID-MS traceable MDRD equation work and is it suitable for use with compensated Jaffe and enzymatic creatinine assays? Nephrol Dial Transplant 21, 2439–2445 (2006).
Levey, A. S. et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 67, 2089–2100 (2005).
Tavakolian, K. Systolic Time Intervals and New Measurement Methods. Cardiovascular engineering and technology 7, 118–125 (2016).
Weissler, A. M., Harris, W. S. & Schoenfeld, C. D. Bedside technics for the evaluation of ventricular function in man. Am J Cardiol 23, 577–583 (1969).
Boudoulas, H. Systolic time intervals. Eur Heart J 11 (Suppl I), 93–104 (1990).
Hassan, S. & Turner, P. Systolic time intervals: a review of the method in the non-invasive investigation of cardiac function in health, disease and clinical pharmacology. Postgrad Med J 59, 423–434 (1983).
Hu, K. et al. Methods for assessment of left ventricular systolic function in technically difficult patients with poor imaging quality. J Am Soc Echocardiogr 26, 105–113 (2013).
Tei, C., Nishimura, R. A., Seward, J. B. & Tajik, A. J. Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurements of cardiac catheterization measurements. J Am Soc Echocardiogr 10, 169–178 (1997).
Salzman, S. H., Wolfson, S., Jackson, B. & Schechter, E. Epinephrine infusion in man. Standardization, normal response, and abnormal response in idiopathic hypertrophic subaortic stenosis. Circulation 43, 137–144 (1971).
Hunt, D., Sloman, G., Clark, R. M. & Hoffmann, G. Effects of beta-adrenergic blockade on the systolic time intervals. Am J Med Sci 259, 97–113 (1970).
Schnell, D. et al. Renal perfusion assessment by renal Doppler during fluid challenge in sepsis. Crit Care Med 41, 1214–1220 (2013).
Taha, N. et al. Pre-ejection period by radial artery tonometry supplements echo Doppler findings during biventricular pacemaker optimization. Cardiovasc Ultrasound 9, 20 (2011).
Bielecka-Dabrowa, A. et al. Biomarkers and echocardiographic predictors of myocardial dysfunction in patients with hypertension. Scientific reports 5, 8916 (2015).
Kusiak, A. et al. Echocardiographic assessment of right ventricular function in responders and non-responders to cardiac resynchronization therapy. Arch Med Sci 11, 736–742 (2015).
Acknowledgements
The research presented in this article is supported by the grant from Kaohsiung Municipal Hsiao-Kang Hospital (kmhk-104-014), Kaohsiung Medical University, Kaohsiung, Taiwan.
Author information
Authors and Affiliations
Contributions
W.-H.L., P.-C.H. and H.-M.S. drafted the manuscript. C.-Y.C., S.-C.C., H.-H.L. and M.-K.L. prepared tables and helped statistical analysis. C.-S.L., H.-W.Y. and T.-H.L. prepared Figures. W.-C.V., W.-T.L., S.-H.S. and H.-M.S. conceived of the study, and participated in its design and coordination. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lee, WH., Hsu, PC., Chu, CY. et al. Systolic time intervals derived from electrocardiographic gated intra-renal artery Doppler waveform associated with left ventricular systolic function. Sci Rep 6, 29293 (2016). https://doi.org/10.1038/srep29293
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29293
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.