Abstract
Progressive hearing loss is very common in the population but we still know little about the underlying pathology. A new spontaneous mouse mutation (stonedeaf, stdf ) leading to recessive, early-onset progressive hearing loss was detected and exome sequencing revealed a Thr289Arg substitution in Sphingosine-1-Phosphate Receptor-2 (S1pr2). Mutants aged 2 weeks had normal hearing sensitivity, but at 4 weeks most showed variable degrees of hearing impairment, which became severe or profound in all mutants by 14 weeks. Endocochlear potential (EP) was normal at 2 weeks old but was reduced by 4 and 8 weeks old in mutants and the stria vascularis, which generates the EP, showed degenerative changes. Three independent mouse knockout alleles of S1pr2 have been described previously, but this is the first time that a reduced EP has been reported. Genomic markers close to the human S1PR2 gene were significantly associated with auditory thresholds in the 1958 British Birth Cohort (n = 6099), suggesting involvement of S1P signalling in human hearing loss. The finding of early onset loss of EP gives new mechanistic insight into the disease process and suggests that therapies for humans with hearing loss due to S1P signalling defects need to target strial function.
Similar content being viewed by others
Introduction
Progressive hearing loss is the most common sensory deficit in the human population and can begin at any age, but we know very little of the underlying molecular or cellular mechanisms involved. Any genes found to be involved in progressive hearing loss can give insight into the molecular pathways and pathological processes leading to deafness. Mouse mutants are valuable tools to provide candidate genes as well as opportunities for detailed mechanistic investigation of the disease process.
Sphingosine-1-phosphate (S1P) signalling is known to be required for normal auditory function from studies of deaf mouse mutants. Mutation of the S1P transporter Spns2 leads to rapidly-progressive loss of auditory sensitivity1 and three independent null mutations of the S1P receptor S1pr2 have severe elevations in auditory thresholds before 4 weeks old2,3,4. S1P is a lysophospholipid intermediate in the process of degradation of sphingolipids, but it also acts as a signalling molecule with effects both within the cell and outside5,6. Extracellular S1P signals through five different receptors, S1pr1–5, which in turn activate a variety of intracellular signalling pathways via G-proteins7. S1P signalling has been implicated in a range of functions including lymphocyte trafficking6,8,9, macrophage and mast cell function10,11, angiogenesis12, vascular permeability and tone13 and bone remodelling14. It is not clear which if any of these functions is involved in normal hearing.
Here we report a missense mutation in S1pr2 that arose spontaneously in mice generated by a large scale targeted mutagenesis program15,16. We describe the identification of the causative mutation in the S1pr2 gene by linkage analysis and exome sequencing, the rapidly progressive hearing loss associated with a decline in the endocochlear potential and subsequent loss of cochlear hair cells. Furthermore, we found that genomic variants close to the human S1PR2 gene were significantly associated with auditory thresholds in a large population sample, the 1958 British Birth Cohort. The new mouse mutant we report here provides mechanistic insight into the pathological processes underlying S1PR2-related hearing loss.
Results
As part of the Sanger Institute Mouse Genetics Project, new lines of mutant mice on a C57BL/6N genetic background are screened at 14 weeks old using an electrophysiological test of hearing, the Auditory Brainstem Response (ABR)16,17. In one line carrying a targeted disruption of the Mms22l gene (MMS22-like, DNA repair protein), most mice had normal ABR thresholds (n = 7), but others (n = 4) showed no response to sound stimuli, including one wildtype littermate used as a control. The deafness phenotype was isolated in a new mouse colony and showed transmission consistent with monogenic autosomal recessive inheritance with full penetrance. We named the mutant allele stonedeaf (stdf ).
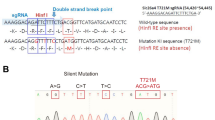
The stdf mutation was mapped to a 10 Mbp interval of proximal chromosome 9 by linkage analysis of offspring from a [(stdf/stdf x C3HeB/FeJ)F1 x stdf/stdf ] backcross. DNA from two distantly-related affected mice was submitted for exome sequencing and the data filtered and analysed (Tables 1, 2, 3, 4, 5). A large number of small structural variations were detected by Pindel across the whole genome. After filtering, 4 remained in the critical 10 Mbp region, but they were not located in coding regions and were not confirmed by capillary sequencing. Two were present in the ancestral ES cell line (Table 3). Single nucleotide variants (SNVs) called by SAMtools were filtered as described (Table 4). Only 7 were within the critical 10 Mbp region (Tables 4 and 5). Of those 7 SNVs, only three were in coding regions; one was synonymous (in Rdh8) and the other two resulted in amino acid changes. One of the two nonsynonymous SNVs (in Bmper) was found in the ancestral ES cell line used in the creation of the knockout from which the stonedeaf allele arose (Table 5) and the SNV (A > C substitution producing an amino acid change of T570P) was predicted to be neutral, so we considered this to be an unlikely candidate. The remaining SNV (a G > C transition in S1pr2; Fig. 1A), resulted in a threonine to arginine change (T289R), which was predicted by both NetDiseaseSNP18 and PhD-SNP19,20 to be deleterious. The affected threonine residue is highly conserved (Fig. 1B,D), located in a transmembrane domain and was predicted by ConSurf 21,22 to be structural (Fig. 1C). Genotyping a large population (n = 204) of mice from the stonedeaf colony for this mutation by capillary sequencing supported its causative nature; all mice with raised thresholds (>4 weeks old) were homozygous for the mutation, whereas mice with normal thresholds were either S1pr2+/stdf or S1pr2+/+.
The stonedeaf mutation is a G > C transition in S1pr2 leading to a threonine to arginine substitution.
(A) Trace showing the G > C SNV in wildtype (top), heterozygote (middle) and homozygote mutant (bottom) mice. (B) The base at 9:20772109 (indicated in red) is conserved between mouse, human, xenopus and zebrafish. Note that S1pr2 is on the reverse strand and so the G > C SNV appears as C > G when the sequence is oriented in the direction of reading of the gene, as in A and B in this figure. (C) ConSurf analysis of the residues; 289T is predicted to be buried (b) and highly conserved and thus likely to be a structural residue (s). (D) ConSurf-annotated clustal of S1pr2 protein sequences. 289T is highly conserved. In (C,D), yellow lettering indicates insufficient data for a reliable calculation of conservation. (E) Structural model of the wildtype S1pr2 protein based on Phyre2 modelling from the S1pr1 structure. The seven transmembrane helices are shown in different colours. A black arrow points to the snorkelling helix (coloured red) referred to in the text. (F) A zoomed view of the wildtype 289T residue (green stick form) (G). A zoomed view of the Arginine residue (red stick form) in the T289R substitution of S1pr2stdf. The effect of the mutation on the S1pr2 hydrogen bond network (based on Phyre2 modelling) is shown in H and I. (H) In the wildtype, T289 (purple) forms a single hydrogen bond (dotted line) with V286 (brown). (I) In the S1pr2stdf mutation, R289 (purple) can no longer form a hydrogen bond with V286 (brown) or any other residues.
S1pr2 was subjected to protein structure prediction using Phyre223, based on the X-Ray crystal structure of homologous receptor, S1pr124 and the T289R mutation was introduced using Pymol™ (DeLano Scientific LLC) (Fig. 1E–I). The mutation sits within a hydrophobic pocket and is likely to cause some local disruption including changing available hydrogen bonds (Fig. 1H,I). The mutation site (289T) is situated on the boundary between the membrane and intracellular region of the receptor. It might be anticipated that the replacement of threonine at position 289 with an arginine residue would have little effect on the protein’s position within the membrane. However, membrane proteins are often highly sensitive to mutation and modest differences in the tilt angle of the transmembrane region relative to the membrane surface, or slight changes in insertion depth have been known to cause significant effects on function (several such cases have been reviewed25). In S1pr2, the position of the snorkelling helix just above the aberrant arginine residue may be affected which might perturb intracellular signalling function (See Fig. 1E–G). The structural modelling therefore supports our conclusion that the T289R mutation is the stdf causal mutation.
Immunohistochemistry was used at postnatal day (P)5 and P14 (Fig. 2) to reveal expression of S1pr2 mainly in the cell bodies of inner and outer hair cells (Fig. 2C,D) and in the stria vascularis and spiral ligament fibrocytes which are important for the recycling of ions into the scala media (Fig. 2B,F) and in spiral ganglion cells. The same pattern of expression was observed at P28 (data not shown). S1pr2 expression was detected with a similar distribution in the S1pr2stdf/stdf mutants (Fig. 2E), which is not surprising as the point mutation is unlikely to stop protein translation.
Immunohistochemical localisation of S1pr2.
(A–C) Expression pattern of S1pr2 in the wildtype cochlea at P5 (brown staining indicates S1pr2 labelling). S1pr2 is mainly expressed in scattered cells of the stria vascularis (black arrowheads in C), the developing spiral ligament (red arrowheads in C), Outer Hair Cells (OHCs, black arrowheads in B), cells of the spiral ganglion (arrows in B) and spiral ganglion neuron terminals innervating the Inner Hair Cells (IHCs, open arrowheads in B). (D,E) S1pr2 cochlear expression at P14 in stonedeaf mutant (S1pr2stdf/stdf ) and littermate controls (S1pr2+/stdf ). We detect expression of S1pr2 mainly in spiral ligament fibrocytes (red arrowheads), OHCs (bracket), individual cells in the stria vascularis (black arrowhead), basilar membrane (red arrows) spiral ganglion cells (arrows) and spiral ganglion neuron terminals below the IHCs (green arrowheads). We did not detect a difference in S1pr2 expression distribution, or any obvious difference in labelling intensity, between stonedeaf mutants and littermate controls. F: Expanded view of S1pr2 expression in the spiral ligament fibrocytes (red arrowheads). Scale Bars: (A,D–F) 20 μm. (B,C) 10 μm.
Changes in auditory sensitivity with age were assessed by ABRs17, using capillary sequencing to assign genotype (Fig. 3A–C). Mice homozygous for the stonedeaf mutation demonstrated a wide range of auditory sensitivity at 4 weeks old (Fig. 3A), while thresholds were higher at 8 and 14 weeks old (Fig. 3A–C). For some of these mice (n = 62), ABR measurements were made longitudinally at 4, 8 and 14 weeks old (Fig. 3D). A progressive deterioration in threshold with increasing age was apparent in S1pr2stdf/stdf mice (n = 28). Wildtype (n = 7) and heterozygous (n = 27, not shown) mice maintained good sensitivity of threshold as age increased.
Auditory Brainstem Response (ABR) thresholds in S1pr2stdf mice.
(A–C) Mean ABR thresholds (±SD) recorded in S1pr2+/+ (green), S1pr2+/stdf (blue) and S1pr2stdf/stdf (red) mice aged 4 weeks old (A, S1pr2+/+ n = 7, S1pr2+/stdf n = 34, S1pr2stdf/stdf n = 44), 8 weeks old (B, S1pr2+/+ n = 20, S1pr2+/stdf n = 75, S1pr2stdf/stdf n = 71) and 14 weeks old (C, S1pr2+/+ n = 7, S1pr2+/stdf n = 26, S1pr2stdf/stdf n = 25). Individual homozygous mouse thresholds are plotted as grey symbols and lines to emphasise the scatter of the data. (D) Click thresholds recorded longitudinally in S1pr2+/+ (green, n = 7) and S1pr2stdf/stdf (red, n = 28) mice are plotted as a function of age (from 4–14 weeks).
Expression of S1pr2 in the lateral wall of the cochlear duct suggested a potential role for S1P signalling in generation of the high resting potential, the endocochlear potential (EP), in the endolymph bathing the upper surface of the sensory hair cells. EP is essential for normal hair cell function, providing a strong driving force across transduction channels. We measured EP in mice aged P14, P28 and P56, in some cases following ABR recording. In P14 mice, ABR thresholds of S1pr2stdf/stdf mice were comparable to those recorded in S1pr2+/stdf littermate controls (Fig. 4A). EPs recorded were also of comparable magnitude in S1pr2stdf/stdf mice (98.0 ± 12.5 mV) and S1pr2+/stdf littermate controls (100.0 ± 11.8 mV) (Fig. 4D). At P28, ABR thresholds of control mice were maturing towards adult levels, but homozygous mutants demonstrated a wide range of sensitivity (Fig. 4B). At P28, EP in control (heterozygote) mice had reached fully mature levels (125.5 ± 6.5 mV) but mutants demonstrated a reduced and variable EP (47.9 ± 22.2 mV) (Fig. 4E). At P56, ABR thresholds of mutants showed further elevations compared to littermate controls (Fig. 4C) and EP remained low (53.7 ± 17.9 mV). Littermate control heterozygotes maintained normal EPs at P56 (120.5 ± 9.8 mV) (Fig. 4F). In summary, at early stages of the pathological process, ABR thresholds increase in line with the reduction in EP.
Auditory Brainstem Responses (ABR), Endocochlear Potential (EP) and strial structure in stonedeaf mice.
Left column: Mean ABR thresholds are plotted for mice aged P14 (A), P28 (B) and P56 (C), for control S1pr2+/stdf mice (blue) and for mutant S1pr2stdf/stdf (red). Individual S1pr2stdf/stdf thresholds are given shown as grey symbols and lines , to illustrate the range of data. Middle column: EP measurements with mean ±SD. Right columns: Whole mounts of middle turn stria vascularis with filamentous actin (green) and marginal cell nuclei (blue); scale bar = 20 μm. (A) In P14 mice, ABR thresholds of S1pr2stdf/stdf mice (red) (n = 6) were comparable to those recorded in S1pr2+/stdf littermate controls (blue) (n = 10). (D) P14 EPs recorded were also of comparable magnitude in S1pr2stdf/stdf mice (n = 13; mean EP ± SD = 98.0 ± 12.5 mV; range 81.3–114.9 mV) and S1pr2+/stdf littermate controls (n = 20; mean EP ± SD = 100.0 ± 11.8mV; range 88.9–120.9 mV). (G,H) P14 strial marginal cell boundaries had a similar appearance in S1pr2+/stdf controls and in S1pr2stdf/stdf mice. (B) At P28, ABR thresholds of S1pr2+/stdf control mice were maturing towards adult levels (n = 16), but those of S1pr2stdf/stdf mutants (n = 16) demonstrated a wide range of sensitivity. (E) At P28, EP in S1pr2+/stdf control mice had reached fully mature levels (n = 16; 125.5 ± 6.5 mV, range 116.0–136.6 mV) but S1pr2stdf/stdf mutants demonstrated a reduced and variable EP (n = 16; 47.9 ± 22.2 mV, range 22.4–98.5 mV). (I,J) Strial marginal cell boundaries in P28 S1pr2stdf/stdf mice started to become less regular (panel J) compared to those of S1pr2+/stdf controls (panel I). (C) At P56, ABR thresholds of S1pr2stdf/stdf mutants (n = 14) showed further elevations compared to littermate controls (n = 7). (F) Mean EP from P56 mutant mice remained low (n = 20; 53.7 ± 17.9 mV, range 1.6–84.2 mV) while S1pr2+/stdf control mice maintained normal EPs (n = 12; 120.5 ± 9.8 mV, range 91.8–130.9 mV). (K,L) Strial marginal cell boundaries became more irregular at P56 in mutants.
The stria vascularis on the lateral wall of the cochlear duct is the major site of EP generation, through active pumping of K+ ions into the endolymph. As EP was reduced in mutants, we examined the stria vascularis in whole mount preparations labelled with isolectin GS-IB4 to highlight capillaries and phalloidin to indicate filamentous actin at the boundaries of the marginal cells lining the luminal surface of the stria1. We examined strial samples from mice aged P14, P28 and P56. Strial marginal cell boundaries appeared normal in stonedeaf homozygotes at P14 (Fig. 4G,H). However, at P28, these boundaries were less regular in mutants than in heterozygous controls, showing a mixture of larger and smaller boundaries, typically losing their normal hexagonal/pentagonal shapes (Fig. 4I,J). These changes were seen intermittently with some normal segments in between. This structural defect progressed with age. At P56, some extremely large or small marginal cell boundaries were seen (Fig. 4K,L). Strial capillaries displayed clear dilation in patches in some of the mutants, which was not seen in any of the controls (Fig. 5A–F).
Capillary expansion and Kcnj10 expression in the stria vascularis of S1pr2stdf mice.
Capillaries in the middle turn stria vascularis of mutants, shown for S1pr2stdf/stdf mutants (B,D,F) and in S1pr2+/+ littermate controls (A,C,E) at P14 (A,B), P28 (C,D) and P56 (E,F). Capillaries appeared swollen at P28 and P56 in S1pr2stdf/stdf mutants (D) compared to S1pr2+/+ littermate controls (C). Panels A–F were imaged at the same magnification; scale bar (in F): 20 μm. Kcnj10 (brown label) was expressed at P28 in the stria vascularis intermediate cells in both S1pr2stdf/stdf mutants (H,J) and in S1pr2+/+ littermate controls (G,I), in the apical and basal turns of the cochlea. Labelling appeared strongest towards the apex (G,H) and less strong towards the base (I,J). Scale Bars (G–J): 10 μm. Sections of the entire inner ear were examined, n = 3 mice for each genotype.
Kcnj10 is an ATP-sensitive inward rectifying K+ channel which plays a crucial role in the movement of K+ into the endolymph to establish the high [K+] and positive EP26, so we looked for expression in the stria vascularis of stonedeaf mutants at P5 and P28. Expression appeared as strong in mutants as in controls at P5 but by P28, immunolabelling was weaker in the basal turn of mutants compared with controls (Fig. 5G–J).
No gross anatomical defects were found in the middle ear, ossicles or inner ear in stonedeaf mutants. The organ of Corti was then examined by scanning electron microscopy. All mice were ABR-tested one week before fixation and later genotyped by sequencing. In five-week-old mutants, some abnormalities of the organ of Corti were noted only in severely impaired S1pr2stdf/stdf mice. Homozygotes with click thresholds of 95dB SPL, or with no ABRs at all, showed OHC degeneration from the middle turn of the cochlea towards the base, while homozygotes with click thresholds at or better than 80dB SPL appeared to have largely normal organs of Corti (Fig. 6). Degeneration of hair cells was much more extensive in 9-week-old affected mice. Only the extreme apical 10–20% of the organ of Corti retained some inner and outer hair cells in S1pr2stdf/stdf mice at this age and there was extensive degeneration in more basal regions (data not shown). A base-to-apex gradient in hair cell degeneration is a common pathological pattern.
ABR data from individual mice with corresponding scanning electron micrographs.
ABR thresholds from one S1pr2+/stdf mouse (A) and two S1pr2stdf/stdf mice (E,I) recorded at four weeks with scanning electron micrographs from the same mice at five weeks old. (B–D) show the apical, middle and basal turns respectively of the S1pr2+/stdf mouse; the corresponding best frequency for each region illustrated is indicated on the audiogram (A). (F–H) likewise show the apical, middle and basal turns of the S1pr2stdf/stdf mouse whose audiogram is shown in (E), with the corresponding frequencies marked. Although this mouse has raised thresholds, the organ of Corti appears normal. (J–L) show the apical, middle and basal turns of a S1pr2stdf/stdf mouse with no response to stimuli at all (I). No hair cells are visible in the basal turn (L), but some remain in the mid-apical (K) and apical (J) turns. Scale bar = 10 μm.
We next asked if the targeted Mms22l mutation had any impact upon the auditory phenotype. Following identification of the stdf mutation, mice with ABR data were divided according to both the S1pr2 genotype and the Mms22l genotype (n = 73 mice aged 4 weeks, 118 mice aged 8–10 weeks, 14 mice aged 44 weeks). However, the presence or absence of the targeted Mms22l allele did not significantly affect ABR thresholds within any S1pr2 genotype and age group (Mann-Whitney Rank Sum Test, p > 0.05 in all cases).
To assess the possibility that other phenotypes were associated with the S1pr2stdf mutation, we obtained DNA samples from 39 mice from the Mms22l line that had been screened as part of the Mouse Genetics Project16. These samples were genotyped for the S1pr2stdf mutation and mice grouped into new cohorts that were wildtype (n = 10), heterozygous (n = 17) and homozygous (n = 12) for the S1pr2stdf mutation. Phenotyping data for 252 parameters measured across 22 broad assay groups16 were obtained for these 39 mice and analysed to determine significant phenotypes. A summary of these data are shown in Fig. 7 as a heatmap, with data for the stonedeaf mutants alongside that of the Mms22l mutants and of Spns2, another mutant line affecting an S1P transporter protein involved in the same signalling pathway and with a similar auditory phenotype1. The S1pr2stdf mutation had a selective effect only on hearing and showed no other abnormalities over the range of phenotyping tests (the red box in Fig. 7 indicating abnormal neurological features results from a lack of Preyer reflex, the ear flick response to sound, which is part of the neurological assessment). The targeted Mms22l allele led to lethality in homozygotes, so heterozygotes were screened but no other anomalies were detected other than the three individuals that were deaf and later proved to be homozygous for the stonedeaf mutation. In contrast, the Spns2 mutants showed deafness and a number of additional abnormal phenotypes (Fig. 7), including eye defects1 and various anomalies of the immune system, especially associated with leucocytes9. S1P signalling effects on the immune system and on retinal angiogenesis are mediated through the S1pr1 gene (for example27,28,29,30) and similar deficiencies would not be expected in the S1pr2stdf mutant mouse.
A heatmap to indicate significant phenotyping parameters obtained for the spontaneous mutant line S1pr2 and 2 targeted mutant lines, Spns2 and Mms22l.
Red cells indicate which of 22 phenotyping assays had at least one parameter that was significantly affected compared to controls. Blue cells indicate no difference to controls. The yellow cell for Mms22l indicates the assay (ABR) where results did not segregate with the targeted genotype and led to the identification of the stonedeaf mutation. The red cell indicating abnormal neurological features results from a lack of startle response or Preyer reflex, the ear flick response to sound, which is part of the neurological assessment; all other neurological tests gave normal responses. The phenotypic differences noted are numbered as follows: 1. Elevated ABR thresholds, 2. Abnormal Bacterial Shedding, 3. Abnormal eye coloration, 4. Abnormal corneal opacity, corneal vascularisation, eyelid closure, iris pupil shape, 5. Abnormal startle response, 6. Abnormal % B Cell CD19+, % Granulocyte Gr1+, % Mature B Cell IgD+, % Monocyte, % NK Cell, % NKT Cell, % T Cell CD3+, % T Cell CD4+, % T Cell CD8+, 7. Abnormal % B Cell CD19+, % Granulocyte Gr1+, % Mature B Cell IgD+, % Monocyte, % T Cell CD3+, % T Cell CD4+, % T Cell CD8+, 8. Abnormal glucose, total bilirubin, 9. Abnormal white blood cell count, 10. Abnormal viability at weaning, 11. Homozygotes show recessive lethality. (Details of these phenotyping platforms can be found in ref. 16).
Finally, we investigated the potential involvement of S1PR2 in human hearing loss by asking if variants in this gene show association with auditory thresholds in the 1958 British Birth Cohort31. Hearing thresholds measured at 1 and 4 kHz at the age of 44–45 and genotype data imputed to the 1000 Genomes dataset (March 2012 release) were used in this association study. Both datasets were available for 6,099 individuals. SNPs within 0.1 Mb of the S1PR2 gene as well as within the gene itself were interrogated as a candidate gene association. For 1 kHz audiometric thresholds, the adjacent SNP rs74930654 (which is 27 kb from the end of S1PR2, on the reverse strand) showed the most significant association, with a p value of 0.001644. For 4 kHz thresholds, the most significant association was with rs201930568 (located 100 kb before the start of S1PR2, on the reverse strand), with a p value 0.001105. These findings suggest that variants affecting the S1PR2 gene do contribute to auditory thresholds in the UK population.
Discussion
Stonedeaf is a new missense mutation of S1pr2 with early-onset, progressive hearing loss with no other phenotypes apparent besides the hearing defect. The earliest detected changes in the cochlea were the reduced EP measurements and morphological changes of the stria vascularis. The appearance of hair cell degeneration in stonedeaf mice appeared to be a secondary phenomenon, occurring after the onset of pathological changes to the stria vascularis, EP and ABR thresholds. Indeed, normal-looking hair cells were seen in the apex of the cochlea in 5- and 9-week-old mice with no measureable ABRs. Secondary hair cell degeneration resulting from a reduced EP has been described before in mouse mutants where (unlike S1pr2) there is no expression of the mutant gene in the hair cells, such as in mice with mutations of the Kit gene32. A normal EP level may be critical for the maintenance of the sensory hair cells, which are specialised to survive in an environment where their upper surface is bathed in endolymph, so any change in voltage or ionic composition of endolymph may disrupt their homeostasis. S1pr2 is expressed in hair cells so we cannot rule out a direct effect of the mutation on hair cells, but as the earliest cochlear defect we saw was the reduction in EP, this is likely to be the primary pathological event leading to raised ABR thresholds and secondary hair cell degeneration.
The changes we observed in the strial blood vessels may reflect a primary change due to abnormal S1P signalling, which has previously been reported to have an impact on vascular tone of the modiolar artery33. Alternatively, the dilation we see may be a consequence of abnormal strial function, leading to both reduced EP and compensatory changes of the vasculature in response to local metabolic demand. Previous reports of mutants with strial dysfunction due to a lack of intermediate cells suggest that the strial vasculature responds to metabolic demand leading to small capillaries where the stria is not functional34.
The pattern of reduced EP and altered strial morphology early in the progression of the hearing loss is very similar to that seen in mice with a mutation of Spns2, another component of S1P signalling1. A progression to fewer, larger marginal cells has been described previously in ageing BALBc and CBA/CaJ mice as their EP becomes lower35,36 and in other mutant mice with EP defects such as the pendrin mutant37. Three independent knockout alleles of S1pr2 have been reported previously2,3,4 and disrupted marginal cell boundaries and expanded strial capillaries were described in one of these mutant lines3 although no EP measurements were made. These knockout mice all showed more severe hearing impairment than we see in the stonedeaf mutant, although none of them reported thresholds as early as P14 so it is not clear if there was normal development followed by very rapid loss of sensitivity. We find thresholds are normal in S1pr2stdf homozygotes at P14 and by P28 there is considerable variability in thresholds despite all the mice having the same genetic background (C57BL/6N) and being housed in identical environmental conditions. In two targeted null alleles of S1pr2, severe hearing impairment was reported in all mice tested at P222 or 4 weeks old3, so the stonedeaf missense mutation may produce a hypomorphic effect on S1pr2 function and slower progression of the phenotype. The three null alleles of S1pr2 were also reported to show severely abnormal stria vascularis morphology, vestibular defects and progressive spiral ganglion loss. We did not see any indications of vestibular defects in S1pr2stdf homozygotes, but we did find stria vascularis structural defects that progressed with age and were similar to those previously reported in a null allele3.
In conclusion, we report here for the first time that EP is reduced resulting from an S1pr2 mutation, a feature that was not reported in the three knockout S1pr2 mutants. Furthermore, we found that the S1pr2stdf homozygotes show normal thresholds and EP around the onset of hearing, progressing over the following few weeks to severe or profound deafness, greatly reduced EP and presumed secondary hair cell degeneration. The delayed loss of auditory function seen in S1pr2stdf homozygotes suggests that the functional processes mediated through S1P-signalling are not critical for the development of hearing, but instead are required for the ongoing maintenance of cochlear function once hearing has been established. This suggests the possibility of therapeutic intervention to prevent the hearing loss if diagnosed early in the pathological process. This is particularly relevant given the recent discovery of missense mutations in human S1PR2 38 and our discovery of significant association between genomic markers close to the S1PR2 gene and auditory thresholds in the human population. These findings emphasize the need for accurate diagnosis and development of treatments to restore EP in such cases where S1P signalling is implicated; simply attempting to regenerate hair cells, for example, would not restore hearing if a patient has a pathology involving EP decline. Discussion and research on developing treatments for hearing loss often focus on sensory hair cells, but our report provides the first clear example of the involvement of S1PR2 in EP generation and the need to restore EP if treatments are to be successful.
Materials and Methods
Ethics statement
Mouse studies were carried out in accordance with UK Home Office regulations and the UK Animals (Scientific Procedures) Act of 1986 (ASPA) under UK Home Office licences and the study was approved by the King’s College London Ethical Review Committees. Mice were culled using methods approved under these licences to minimize any possibility of suffering.
Origin and identification of mutant allele
The stonedeaf (stdf ) mutation arose in mice derived from the Sanger Institute Mouse Genetics Project, which uses targeted ES cells to generate new mutant lines as described previously15,16. The mutation was mapped by linkage analysis of offspring from a [(stdf/stdf x C3HeB/FeJ)F1 x stdf/stdf ] backcross using ABR thresholds at 8–10 weeks old to assign phenotype (n = 79 affected and 82 unaffected offspring). DNA from two distantly-related affected mice was submitted for exome sequencing using the Agilent SureSelectXT mouse all exon kit for sequence capture, sequenced on the Illumina HiSeq 2000 platform and the data filtered and analysed as specified in Tables 1, 2, 3, 4, 5. The sequences have been deposited at ENA, accession number ERP000739. Mutant mice are available through EMMA.
Modelling the mutation
S1pr2 was subjected to protein structure prediction using Phyre2 (Protein Homology/analogY Recognition Engine version 2.023). The coordinates corresponding to the top hit, which was based on the X-Ray crystal structure of homologous receptor, S1pr124, were used to produce a model of S1pr2 and to introduce the T289R mutation using Pymol™ (DeLano Scientific LLC).
Immunohistochemistry
Inner ears of wildtype mice from the C57BL/6J strain carrying an albino mutation (C57BL/6BrdTyrc-Brd) at postnatal day five (P5) and S1pr2stdf/stdf mutants (with littermate S1pr2+/stdf controls) at P14 and P28 were fixed and processed for immunohistochemistry. Sagittal wax sections, 8 μm thick, were exposed to rabbit anti-S1pr2 (21180-1-AP; Proteintech, Chicago, USA, 1:25), or anti-KcnJ10 (APC-035, Alomone Labs, Jerusalem, 1:300) antibody, before undergoing a DAB reaction and counterstaining with hematoxylin on a Ventana Discovery machine. Sections covering the entire inner ear for three different mouse samples of each genotype/age were examined.
Electrophysiology
Auditory sensitivity was assessed using measurements of Auditory Brainstem Responses (ABRs)17. ABRs were recorded from Ketamine/Xylazine anaesthetised mice aged 4, 8 and 14 weeks, evoked by clicks and tone pip (6–30 kHz) stimuli presented freefield at 0–95 dB SPL in 5 dB steps to determine threshold sensitivity. EPs were measured under urethane anaesthesia (2 mg/g) in a different group of mice, in some cases following ABR threshold measurement. After these ABR recordings, a tracheal cannula was inserted and the bulla was opened to allow fenestration of the cochlear wall and insertion of a 150 mM KCl-filled glass micropipette into the scala media. The EP was measured as the potential difference between the scala media and a reference silver/silver chloride pellet under the dorsal skin of the neck39.
Stria vascularis analysis
Inner ears were fixed in 4% paraformaldehyde at room temperature for 2 hours before the lateral walls were dissected out in PBS. Samples for cell boundary analysis were incubated with 488 phalloidin (1:400, Molecular Probes) in PBS at room temperature for 2 hours (P14, S1pr2+/stdf n = 4; S1pr2stdf/stdf n = 3; P28, S1pr2+/stdf n = 7; S1pr2stdf/stdf n = 7; P56, S1pr2+/stdf n = 6; L, S1pr2stdf/stdf n = 6). For capillary analysis, whole mount samples were isolated and incubated with isolectin GS-IB4, 594 (Molecular Probes, 1:50) at 4 °C, overnight in PBS with 3% BSA, to visualise capillaries (P14, S1pr2+/stdf , n = 4; S1pr2stdf/stdf, n = 3; P28, S1pr2+/stdf , n = 4; S1pr2stdf/stdf, n = 5; P56, S1pr2+/stdf , n = 4; S1pr2stdf/stdf, n = 5). The samples were mounted with Vectashield Mounting medium with DAPI (Vector, Cat. No: H-1200) and imaged by confocal microscopy (Zeiss LSM 510 & 710). The numbers of capillary branch points per field (200 × 200 μm fields) in the middle turn of the cochlear duct was quantified using image J (controls, n = 4; homozygotes, n = 5, at P28).
Scanning electron microscopy
Samples were taken from S1pr2+/stdf and S1pr2stdf/stdf mice aged 5 and 9 weeks old, a week after ABR testing at 4 and 8 weeks old respectively and processed for scanning electron microscopy of the apical surface of the organ of Corti using the OTOTO methodology40. Samples were analysed according to their percentage distance from the cochlear base.
Human population analysis
The 1958 British Birth Cohort and the collection of hearing data and analysis have been described previously41. Participants were drawn up from 17,638 individuals born in England, Scotland and Wales in 1 week of March 1958. Of the original cohort, 9377 members were revisited by a research nurse for a biomedical follow-up in 2002–2004. Hearing measure consisted of pure tone audiometry at 1 kHz and 4 kHz at age 44–45 years and were adjusted for sex, nuisance variables (noise at test, nurse performing test, audiometer used in test), conductive loss and hearing loss in childhood. DNA was collected from 6099 individuals and genotyped on various Illumina and Affymetrix SNP chips (for detail see http://www2.le.ac.uk/projects/birthcohort/1958bc/available-resources/genetic). These data were then imputed to the 1000 Genomes haplotypes (release March 2012) using MACH and Minimac. Measured SNPs with >95% call rate and Hardy–Weinberg p-value >0.0001 were included as input set. In subsequent analysis imputed SNPs with low imputation quality (r2-hat < 0.3 or MAF < 1%) were omitted. Individual associations were performed to hearing thresholds at 1 kHz and 4 kHz.
Additional Information
How to cite this article: Ingham, N. J. et al. S1PR2 variants associated with auditory function in humans and endocochlear potential decline in mouse. Sci. Rep. 6, 28964; doi: 10.1038/srep28964 (2016).
References
Chen, J. et al. Spinster homolog 2 (Spns2) deficiency causes early onset progressive hearing loss. PLoS Genet. 30, e1004688 (2014).
MacLennan, A. et al. The S1P2 sphingosine 1-phosphate receptor is essential for auditory and vestibular function. Hear. Res. 220, 38–48 (2006).
Kono, M. et al. Deafness and Stria Vascularis Defects in S1P2 Receptor-null mice. J. Biol. Chem. 282, 10690–10696 (2007).
Herr, D. R. et al. Sphingosine 1-Phosphate (S1P) Signaling Is Required for Maintenance of Hair Cells Mainly via Activation of S1P2. J. Neurosci. 27, 1474–1478 (2007).
Fyrst, H. & Saba, J. D. An update on sphingosine-1-phosphate and other sphingolipid mediators. Nat. Chem. Biol. 6, 489–497 (2010).
Maceyka, M. & Spiegel, S. Spingolipid metabolites in inflammatory disease. Nature 510, 58–67 (2014).
Rosen, H. et al. Spingosine 1-phosphate receptor signaling Annu. Rev. Biochem. 78, 743–68 (2009).
Pappu, R. et al. Promotion of lymphocyte egress into blood and lymph by distinct sources of sphingosine-1-phosphate. Science 316, 295–298 (2007).
Nijnik, A. et al. The role of sphingosine-1-phosphate transporter Spns2 in immune system function. J. Immunol. 189, 102–11 (2012).
Michuad, J., Im, D. S. & Hla, T. Inhibitory role of sphingosine 1-phosphate receptor 2 in macrophage recruitment during inflammation J. Immunol. 184, 1475–83 (2010).
Oskeritzian, C. A. et al. Essential roles of sphingosine-1-phosphate receptor 2 in human mast cell activation, anaphylaxis and pulmonary edema. J. Exp. Med. 207, 465–74 (2010).
Skoura, A. et al. Essential role of sphingosine-1-phosphate receptor 2 in pathological angiogenesis of the mouse retina. J. Clin. Invest. 117, 2506–2516 (2007).
Skoura, A. & Hla, T. Regulation of vascular physiology and pathology by the S1P2 receptor subtype. Cardiovasc. Res. 82, 221–228 (2009).
Ishii, M., Chemorepulsion by blood S1P regulates osteoclast precursor mobilization and bone remodeling in vivo. J. Exp. Med. 207, 2793–2798 (2010).
Skarnes, W. C. et al. A conditional knockout resource for the genome-wide study of mouse gene function. Nature 474, 337–43 (2011).
White, J. K. et al. Genome-wide generation and systematic phenotyping of knockout mice reveals new roles for many genes. Cell 154, 452–64 (2013).
Ingham, N. J., Pearson, S. & Steel, K. P. Using the auditory brainstem response (ABR) to determine sensitivity of hearing in mutant mice. Curr. Protoc. Mouse Biol. 1, 270–287 (2011).
Petersen, B., Petersen, T. N., Andersen, P., Nielsen, M. & Lundegaard, C. A generic method for assignment of reliability scores applied to solvent accessibility predictions. BMC Struct. Biol. 9, 51 (2009).
PhD-SNP. Predictor of Human Deleterious Single Nucleotide Polymorphisms [updated 2010 Jan 18; cited 2015 Nov 5]. Available from http://snps.biofold.org/phd-snp/phd-snp.html.
Capriotti, E., Calabrese, R. & Casadio, R. Predicting the insurgence of human genetic diseases associated to single point protein mutations with support vector machines and evolutionary information. Bioinformatics 22, 2729–2734, http://snps.biofold.org/phd-snp/phd-snp.html (2006).
Ashkenazy, H., Erez, E., Martz, E., Pupko, T. & Ben-Tal, N. ConSurf 2010: calculating evolutionary conservation in sequence and structure of proteins and nucleic acids. Nucl. Acids Res. 38, W529–533 (2010).
Berezin, C. et al. ConSeq: The Identification of Functionally and Structurally Important Residues in Protein Sequences. Bioinformatics 20, 1322–1324 (2004).
Kelley, L. A. & Sternberg, M. J. Protein structure prediction on the Web: a case study using the Phyre server. Nat. Protoc. 4, 363–71 (2009).
Hanson, M. A. et al. Crystal structure of a lipid G protein-coupled receptor. Science 335, 851–5 (2012).
Simpson, P. J. NMR of proteins and nucleic acids. Nuc. Mag. Res. 41, 290–319 (2012).
Marcus, D. C., Wu, T., Wangemann, P. & Kofuji, P. KCNJ10 (Kir4.1) potassium channel knockout abolishes endocochlear potential. Am. J. Physiol. - Cell Physiology 282, C403–C407 (2002).
Brinkmann, V. et al. The immune modulator FTY720 targets sphingosine 1-phosphate receptors. J. Biol. Chem. 277, 21453–21457 (2002).
Mandula, S. et al. Alteration of lymphocyte trafficking by sphingosine-1-phosphate receptor agonists. Science 296, 346–9 (2002).
Jung, B. et al. Flow-regulated endothelial S1P receptor-1 signalling sustains vascular development. Dev. Cell 23, 600–610 (2012).
Mendelson, K., Zygmunt, T., Torres-Vazquez, J., Evans, T. & Hla, T. Sphingosine 1-phosphate receptor signaling regulates proper embryonic vascular patterning. J. Biol. Chem. 288, 2143–2156 (2013)
Ecob, R. et al. Is the relation of social class to change in hearing threshold levels from childhood to middle age explained by noise, smoking and drinking behaviour? Int. J. Audiol. 47, 100–108 (2008).
Steel, K. P., Barkway, C. & Bock, G. R. Strial dysfunction in mice with cochleo-saccular abnormalities. Hear Res. 27, 11–26 (1987).
Scherer E. Q., Lidington D., Oestreicher E., Arnold W., Pohl U. & Bolz S. S. Sphingosine-1-phosphate modulates spiral modiolar artery tone: A potential role in vascular-based inner ear pathologies? Cardiovasc Res. 70, 79–87 (2006).
Cable J., Huszar D., Jaenisch R. & Steel K. P. Effects of mutations at the W locus (c-kit) on inner ear pigmentation and function in the mouse. Pigment Cell Res. 7, 17–32 (1994).
Ohlemiller, K. K., Lett, J. M. & Gagnon, P. M. Cellular correlates of age-related endocochlear potential reduction in a mouse model. Hear Res. 220, 10–26 (2006).
Ohlemiller, K. K. Mechanisms and genes in human strial presbycusis from animal models. Brain Res. 1277, 70–83 (2009).
Wangemann, P. et al. Loss of KCNJ10 protein expression abolishes endocochlear potential and causes deafness in Pendred syndrome mouse model. BMC Med. 2, 30 (2004).
Santos-Cortez, R. L. P. et al. Autosomal recessive hearing impairment due to rare missense variants within S1PR2. Am. J. Hum. Genet. 98, 331–338 (2016).
Steel, K. P. & Barkway, C. Another role for melanocytes: their importance for normal stria vascularis development in the mammalian inner ear. Development 107, 453–463 (1989).
Hunter-Duvar, I. M. A technique for preparation of cochlear specimens for assessment with the scanning electron microscope. Acta Oto-laryngol. 351, 3–23 (1978).
Nolan, L. S. et al. Estrogen-related receptor gamma and hearing function: evidence of a role in humans and mice. Neurobiol Aging. 34, 2077, e1-9 (2013).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Keane, T. M. et al. Mouse genomic variation and its effect on phenotypes and gene regulation. Nature 477, 289–294 (2011).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res 20, 1297–1303 (2010).
Picard Tools: A set of Java command line tools for manipulating high-throughput sequencing data (HTS) data and formats [cited 2015 Nov 5]. Available from http://broadinstitute.github.io/picard/.
Li, H. et al. 1000 Genome Project Data Processing Subgroup. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Ye, K., Schulz, M. H., Long, Q., Apweiler, R. & Ning, Z. Pindel: a pattern growth approach to detect break points of large deletions and medium sized insertions from paired-end short reads. Bioinformatics 25, 2865–2871 (2009).
Acknowledgements
We thank the Wellcome Trust Sanger Institute and members of the Mouse Genetics Project for access to Mms22l targeted mutant mice, their DNA samples and phenotypic information from individual mice; Roz Lacey for colony management and help with ABR screening; Zahra Hance for assistance with inner and middle ear dissections and scanning electron microscopy; Peter Simpson for advice on protein structure; and David Adams for supporting the exome sequencing. This work was supported by The Wellcome Trust (grant no. 098051, 100699 and 089622AIA), the Medical Research Council (KPS), Action on Hearing Loss (KPS), the Haigh Fellowship in age related deafness (SD) and Deafness Research UK (444:UEI:SD). For the 1958 British Birth Cohort analysis, we acknowledge use of phenotype and genotype data from the British 1958 Birth Cohort DNA collection, funded by the Medical Research Council grant G0000934 and the Wellcome Trust grant 068545/Z/02. Genotyping for the B58C-WTCCC subset was funded by the Wellcome Trust grant 076113/B/04/Z. The B58C-T1DGC genotyping used resources provided by the Type 1 Diabetes Genetics Consortium, a collaborative clinical study sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Allergy and Infectious Diseases (NIAID), National Human Genome Research Institute (NHGRI), National Institute of Child Health and Human Development (NICHD) and Juvenile Diabetes Research Foundation International (JDRF) and supported by U01 DK062418. B58C-T1DGC GWAS data were deposited by the Diabetes and Inflammation Laboratory, Cambridge Institute for Medical Research (CIMR), University of Cambridge, which is funded by Juvenile Diabetes Research Foundation International, the Wellcome Trust and the National Institute for Health Research Cambridge Biomedical Research Centre; the CIMR is in receipt of a Wellcome Trust Strategic Award (079895). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
N.J.I. and S.P. carried out the electrophysiology, F.C. carried out the linkage analysis and scanning electron microscopy, M.A.L. carried out the sequencing and identification of the mutation, J.C. developed the genotyping tool and carried out most of the genotyping, A.B. did the immunocytochemistry, J.C. analysed the stria vascularis, R.L.I. carried out the molecular modelling, J.K.W. and K.P.S. led the large-scale phenotypic screen, N.J.I. re-sorted the phenotypic data from the screen, S.J.D. carried out the analysis of the 1958 British Birth Cohort, all authors contributed to the data analysis, N.J.I., M.A.L. and K.P.S. drafted the paper and all authors contributed to the final version of the report.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Ingham, N., Carlisle, F., Pearson, S. et al. S1PR2 variants associated with auditory function in humans and endocochlear potential decline in mouse. Sci Rep 6, 28964 (2016). https://doi.org/10.1038/srep28964
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep28964
This article is cited by
-
Identification and characterisation of spontaneous mutations causing deafness from a targeted knockout programme
BMC Biology (2022)
-
Preclinical and Clinical Evidence for the Involvement of Sphingosine 1-Phosphate Signaling in the Pathophysiology of Vascular Cognitive Impairment
NeuroMolecular Medicine (2021)
-
Platelet-Derived Growth Factor Subunit B Signaling Promotes Pericyte Migration in Response to Loud Sound in the Cochlear Stria Vascularis
Journal of the Association for Research in Otolaryngology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.