Abstract
Acute hyperglycemia is a frequent finding in patients presenting to the emergency department (ED) with acute myocardial infarction (AMI). The prognostic role of hyperglycemia in diabetic patients with AMI remains controversial. We retrospectively reviewed patients’ medical records to obtain demographic data, clinical presentation, major adverse cardiac events (MACEs), several clinical scores and laboratory data, including the plasma glucose level at initial presentation and HbA1c levels. The glycemic gap, which represents changes in serum glucose levels during the index event, was calculated from the glucose level upon ED admission minus the HbA1c-derived average glucose (ADAG). We enrolled 331 patients after the review of medical records. An elevated glycemic gap between admission serum glucose levels and ADAG were associated with an increased risk of mortality in patients. The glycemic gap showed superior discriminative power regarding the development of MACEs when compared with the admission glucose level. The calculation of the glycemic gap may increase the discriminative powers of established clinical scoring systems in diabetic patients presenting to the ED with AMI. In conclusion, the glycemic gap could be used as an adjunct parameter to assess the severity and prognosis of diabetic patients presenting with AMI. However, the usefulness of the glycemic gap should be further explored in prospective longitudinal studies.
Similar content being viewed by others
Introduction
Acute hyperglycemia is a frequent finding in patients presenting to the emergency department (ED) with acute myocardial infarction (AMI). The admission blood glucose level after AMI is an independent predictor of long-term mortality in patients with or without diagnosed diabetes1,2. An elevated blood glucose level may reflect a stress response and/or an underlying abnormal glucometabolic state. Regardless of the mechanism, an AMI complicated by hyperglycemia is associated with an inflammatory and prothrombotic state, depressed myocardial contractility and increased short- and long-term mortality3,4.
Stress-induced hyperglycemia (SIH) commonly occurs in patients with critical illnesses, such as sepsis, multiple trauma, burn injuries, major surgeries, and AMI5. Nonetheless, there are discordant findings on the correlation between hyperglycemia and adverse outcomes in acutely ill patients with or without preexisting diabetes6,7,8.
Because hyperglycemia is the cardinal feature of diabetes, it is necessary to consider pre-existing hyperglycemia in diabetic patients when investigating the association between SIH and adverse outcomes. There is a well-known correlation between glycated hemoglobin (HbA1c) and the long-term mean plasma glucose levels from the preceding 3 months. As estimated long-term average glucose level can be calculated from the HbA1c value with the equation derived from an international multicenter study of HbA1c-derived average glucose (ADAG)9. Therefore, we aimed to identify the major contributor to acute serum glucose levels. In acutely ill diabetic patients, the epiphenomenon of admission hyperglycemia may be caused by acute physiological stress and/or higher chronic baseline blood glucose levels10.
Although the role of hyperglycemia has been well studied as an index for poor prognosis in non-diabetic patients with AMI, the prognostic role of hyperglycemia in diabetic patients remains controversial. We hypothesized that an elevated glycemic gap is associated with an increased risk of developing major adverse cardiac events (MACEs) in diabetic patients presenting to the ED with AMI. The aim of the present study was to explore the correlation between the glycemic gap and adverse clinical outcomes; in addition, we sought to justify the use of the glycemic gap as a biomarker for the severity of diabetic patients presenting to the ED with AMI.
Materials and Methods
Patients
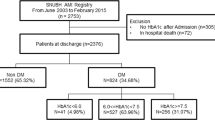
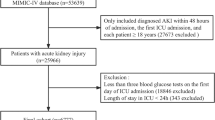
We conducted a retrospective observational study of consecutive patients with diabetes mellitus (DM) admitted for AMI between June 1, 2011 and June 31, 2015. The institutional review board for human investigations of a tertiary referral medical center at Tri-Service General Hospital approved this study and waived the necessity for informed consent. The methods were carried out in accordance with approved guidelines. The identification of patients with DM and AMI was performed by searching for the International Classification of Diseases (9th revision) codes 410 and 250.2–8. Diabetes was considered to be present if a patient was discharged from a hospital with a diagnosis of type 1 or type 2 diabetes, at least 1 prescription for insulin or an oral antidiabetic agent, and/or an HbA1c level ≥6.5% during the preceding 2 months11,12. In accordance with the global taskforce recommendation, AMI was diagnosed based on clinical and laboratory evidence of myocardial necrosis and ischemia13. The records of identified patients were reviewed manually to select AMI patients with data for plasma glucose levels at initial presentation and HbA1c levels obtained between 1 month prior to or immediately after their admission. We excluded patients with missing HbA1c or initial serum glucose levels, those on steroid treatments or presenting with hypoglycemia (blood glucose <70 mg/dL) and patients who received a blood transfusion.
Methods
We retrospectively reviewed patients’ medical records to determine age, sex, underlying comorbidities, clinical presentation, and laboratory data, including B-type natriuretic peptide (BNP) and plasma glucose levels at initial ED presentation, HbA1c levels, and lengths of stay in the intensive care unit (ICU) and hospital. In-hospital MACEs, including AMI, emergency revascularization, cardiogenic shock or death (unless established as non-cardiac in origin), were used as the primary end point. We quantified the severity of the index AMI events using Global Registry of Acute Coronary Events (GRACE) scores and the Killip classification. GRACE scores were calculated as previously described using specific variables, including age, heart rate, systolic blood pressure, creatinine cardiac arrest at admission, ST segment deviation on ECG and elevated cardiac troponins14. AMI severity was determined using the Killip classification: Killip class I includes individuals with no clinical signs of heart failure; Killip class II includes individuals with rales or crackles in the lungs, an S3, and elevated jugular venous pressure; Killip class III describes individuals with frank acute pulmonary edema; and Killip class IV describes individuals in cardiogenic shock or hypotension (measured as a systolic blood pressure lower than 90 mmHg) and evidence of peripheral vasoconstriction (oliguria, cyanosis or sweating)15. Additional adverse outcomes included acute respiratory failure (ARF) that required ventilation support, failure of weaning from a ventilator (defined as administering mechanical ventilation during discharge), acute kidney injury (AKI, defined as serum creatinine elevated >0.3 mg/dl or 50% from baseline)16, and upper gastrointestinal bleeding (UBIG, defined as melena with positive occult blood examination, bright-red blood discharged from the nasogastric tube, or endoscopic evidence of mucosal bleeding).
Determination of serum glucose levels, HbA1c and glycemic gaps
The glucose level upon admission was determined upon admission to the ED. HbA1c assays were performed using a blood analyzer (Primus CLC 385; Primus Corporation, Kansas City, MO, USA) equipped with a high-performance liquid chromatography system. The equation AG = 28.7 × HbA1c–46.7 was used to convert HbA1c levels to the estimated long-term average glucose levels (eAG) for the preceding 3 months9. The glycemic gap represents changes in serum glucose levels during the index event and was calculated from the glucose level at ED admission minus the eAG.
Statistical analysis
Continuous data are expressed as the mean ± standard deviation and were analyzed using the two-tailed Student t-test. Categorical data are expressed as frequencies (%) and were evaluated using the chi-square test or Fisher’s exact test. A one-way analysis of variance was used to assess the significance of various characteristics, laboratory data, and adverse outcomes. A post-hoc analysis was performed using the Bonferroni test. A receiver–operator characteristic curve (ROC) curve was plotted to analyze the discriminative power of the prediction tools, and the area under the ROC (AUROC) and the corresponding 95% confidence intervals (CI) were calculated. Univariate and multivariate Cox hazard regression analyses were performed to identify the risk factors associated with MACEs. Variables with a p < 0.05 in the univariate analysis were entered into the multivariate Cox hazard regression analysis. The correlation between glycemic gap and continuous variables, such as BNP and GRACE scores, was evaluated by the Pearson product-moment correlation. The correlation between the glycemic gap and ordinal variables, such as Killip classes, was evaluated by the Spearman’s rank-order correlation. The data were analyzed using Statistical Package for the Social Sciences version 17.0 statistical software (SPSS, Inc., Chicago, IL, USA), and differences with p values < 0.05 were considered statistically significant. The log-rank test was used to determine the statistical significance of survival curves. The net reclassification improvement (NRI) was used to assess the improvement in model performance after adding parameters (MATLAB, MathWorks, Natick, MA, USA)17.
Results
Patient study population and clinical outcomes
We initially identified 441 patients with AMI and type 2 diabetes. One-hundred and ten patients were excluded because of missing HbA1c levels within 1 month prior to or immediately after admission (n = 92), the absence of plasma glucose levels at initial ED presentation (n = 6), hypoglycemia (n = 8), treatment with steroids (n = 2), or severe anemia requiring a blood transfusion (n = 2). Thus, we enrolled 331 patients after the chart review. Two hundred and fifty-four (76.7%) patients had NSTEMI, whereas 77 (23.3%) patients had STEMI. The demographic data and AMI-related clinical features, including GRACE scores and Killip classification, of the enrolled patients are shown in Table 1. Of these patients, 43 (13.0%) died during hospitalization and 61 (18.4%) experienced MACEs. Compared with survivors, non-survivors had a statistically significant older age, higher glycemic gap, maximal blood glucose during the first 48 hours and BNP level, and longer hospital stay.
Correlations among acute hyperglycemia, glycemic gaps, long-term blood glucose control and major adverse cardiac events
As shown in Table 2, the Cox proportional hazard model revealed that the hazard ratio of the glycemic gap (mg/dL) for MACEs was 1.003 (95% CI: 1.000–1.005, p = 0.02). Compared with acute hyperglycemia (defined as blood glucose level of ≥250 mg/dL) and long-term glycemic controls, glycemic gaps showed greater AUROC values (0.591, 95%CI: 0.510–0.671) for MACEs occurrence (Fig. 1). We determined an optimal cutoff value of 42 mg/dL using the maximal Youden’s index with a sensitivity, specificity, positive predictive value and negative predictive value of 68.9%, 50.7%, 23.9% and 50.4%, respectively, for occurrence. There was no statistically significant difference in the comorbidity of patients with or without an elevated glycemic gap. As shown in Fig. 2, there were statistically significant correlations between the glycemic gap and GRACE score (r = 0.170, p < 0.05), Killip classification (r = 0.135, p < 0.05) and BNP (r = 0.180, p < 0.05). Only 164 patients (49.5%) had a BNP measurement because the levels of BNP were not routinely determined in ACS patients. As shown in Table 3, a further analysis revealed that an elevated glycemic gap (>42 mg/dL) was associated with males and cardiac arrest at ED admission. Patients with glycemic gaps >42 mg/dL showed a significantly higher incidence of in-hospital ARF (p = 0.003), mortality (p = 0.044), cardiogenic shock (p = 0.03), composed MACEs (p = 0.007), and GRACE scores (p < 0.001) and a lower LVEF (p = 0.04) when compared with patients with glycemic gaps <42 mg/dL. As shown in Fig. 3, a Kaplan–Meier survival curve showed that a glycemic gap > 42 mg/dL was associated with a significantly shorter survival when compared with a gap <42 mg/dL (log-rank test p < 0.05).
Chronic blood glucose controls in diabetic patients with AMI
Unexpectedly, we found that chronic glycemic controls affected adverse outcomes and the length of ICU and hospital stays. Patients with good glycemic control, as determined by HbA1c values of <7%, had a statistically significant higher risk for AKI (p = 0.001), GRACE scores (p = 0.01) and hospital stays (p = 0.04) (Table 4). There were no statistically significant differences in glycemic gaps between these three HbA1c groups (p = 0.39). Admission hyperglycemia was statistically significantly associated with the development of MACEs only in patients with HbA1c ≤ 7% (HR: 1.003, 95% CI: 1.000–1.006, p=0.032), whereas there were no association between admission hyperglycemia and the development of MACEs in patients with 7% < HbA1c < 9% (HR: 1.002, 95% CI: 0.997–1.006, p = 0.47) and HbA1c ≥ 9% (HR: 1.004, 95% CI: 0.997–1.011, p = 0.22).
Incorporating the glycemic gap into the TIMI and GRACE scores
Consistent with previous studies, we found that GRACE scores and the Killip classification showed a superior discriminative performance at predicting MACEs in diabetic patients presenting to the ED with AMI. Incorporating the glycemic gap into the GRACE score significantly increased the AUROC from 0.873 (95% CI = 0.823−0.922) to 0.877 (95% CI = 0.829−0.925, NRI, 0.072, p: 0.028); however, the incorporation of the glycemic gap into the Killip classification did not result in a significant change in the AUROC: 0.904 (95% CI = 0.850−0.958) to 0.917 (95% CI = 0.865−0.968, p = 0.99) (Fig. 4).
Discussion
There were three major findings in the present study, as follows: 1) the glycemic gap, by eliminating the possible influences of chronic blood glucose controls, supports the possible deteriorating effects of SIH on the early stage of AMI; 2) an elevated glycemic gap but not acute hyperglycemia was associated with increased mortality and the glycemic gap itself showed superior discriminative power for MACEs occurrence; and 3) the addition of the glycemic gap increased the discriminative power of the GRACE score in diabetic patients presenting to the ED with AMI.
Stress induced hyperglycemia can be attributed to the presence of excess levels of counter-regulatory hormones, anti-inflammatory cytokines, and increased gluconeogenesis and hepatic insulin resistance5,18,19. SIH could be a vicious cycle by increasing free fatty acids, insulin resistance, chemical inactivation of nitric oxide and the production of reactive oxygen species, a prothrombotic state, and vascular inflammation20. Patients with SIH could have increased susceptibility to myocardial ischemia-reperfusion injury due to increased oxidative stress, inflammation, and activation of stress-responsive kinases21. Acute hyperglycemia during coronary revascularization causes endothelial dysfunction and is associated with plaque instability and infarct size22. Even in non-diabetic patients with hip fracture, SIH was associated with increased risk of AMI23. Mechanistically, hyperglycemia decreases vascular dilation and increase permeability during the initial inflammatory responses, possibly through protein kinase C activation24. Glucose fluctuation can activate nuclear factor-kB and protein kinase C pathway, leading an increased expression of the adhesion molecules and excess formation of advanced glycation end products than stable glucose in vitro25,26. In addition, recent studies have shown that dermcidin, a stress induced protein, can inhibit glucose-induced insulin synthesis and result in hyperglycemia in patients with AMI and stress-induced type 1 diabetes27,28. Insulin can activate nitric oxide synthase and inhibit platelet aggregation and thus produce a beneficial effect on cardiovascular disease29. Aspirin can further increase plasma insulin levels by decreasing plasma dermcidin levels and reducing the infarct size in patients with AMI27,30. Our finding of that admission hyperglycemia was statistical significantly associated with the development of MACEs only in patients with HbA1c ≤ 7% further supported the hypothesis that SIH would worsen the prognosis. Recent clinical trials of insulin treatment in AMI patients have resulted in varying levels of benefit, but the clinical benefit of an aggressive insulin treatment remains unproven4,20,31. We thought that reevaluation of those trials by using glycemic gap might also help in elucidating the potential benefits in acute control of blood glucose. In non-diabetic or mixed populations, elevated admission glucose levels are common in patients with AMI and are strongly associated with an increased risk of poorer outcomes and mortality2,32. Acute and mean hyperglycemia during hospitalization is associated with adverse clinical outcomes2,33,34,35. Elevated admission hyperglycemia was associated with in-hospital mortality, a lower myocardial salvage index and composite MACEs in acute ST-segment elevation myocardial infarction (STEMI) patients36,37,38,39,40. Patients with a Killip class of III or IV had statistically significant higher first blood glucose levels and higher in-hospital mortality when compared with Killip class I patients15. Nonetheless, several studies revealed that acute hyperglycemia may not reflect the severity of AMI in patients with diabetes36,41. A prospective multicenter Korean study found that admission hyperglycemia predicted the 30-day mortality in 816 non-diabetic STEMI patients with cardiogenic shock but not diabetic patients42. There was no significant difference in myocardial salvage after PCI between diabetic patients with or without SIH36. Intensive glucose regulation did not reduce the infarct size in hyperglycemic patients with AMI treated with PCI but rather was associated with harm43. We believe that one explanation for these discordant study results could be lack of consideration of the chronic blood glucose levels in patients with diabetes. By using the glycemic gap, we eliminated the possible influence of chronic hyperglycemia in diabetic patients. The glycemic gap may explain the “diabetes paradox” and the association between acute hyperglycemia, long-term glucose controls, and certain adverse clinical outcomes. Once a novel biomarker becomes available to facilitate risk prediction, it is essential to compare this marker with existing tools, i.e., combining different biomarkers and clinical scores to further increase the AUROC44,45. In the NRI analysis, incorporation of the glycemic gap into the GRACE score could increase the AUROC for the development of MACEs, suggesting that the glycemic gap may be used as an additional prognostic marker in diabetic patients under physiological stress.
The “diabetes paradox,” i.e., diabetes and glycemic control are not independently associated with mortality in critical ill patients, was proposed by Krinsly et al. and has been continuously observed in other settings8,46,47. The HbA1c level is characterized by lower biological variability and is relatively unaffected by acute stress or sepsis12. Notably, HbA1c values can be affected by anemia and blood transfusion48,49. In patients without diabetes, elevated glucose at admission or acute hyperglycemia was associated with adverse outcomes in patients with acute critical illnesses. Acute hyperglycemia is linked to increased adverse outcomes in patients with trauma42,50, poorer neurological improvement and symptomatic hemorrhage in patients with acute ischemic stroke51, and increased risk of nosocomial complications in patients with community acquired pneumonia (CAP)10,52. Admission basal glucose levels were independently associated with increased mortality in ED patients without a diagnosis of diabetes53. Nonetheless, several studies have reported that the relationship between hyperglycemia and acute illness-related mortality is relatively weak in diabetic critically ill patients54,55,56,57,58. There was no independent association between hyperglycemia and mortality once lactate levels were controlled58. Egi et al. reported that ICU mortality was not associated with diabetes per se or chronic blood glucose control. Freire et al. demonstrated that the highest glucose value during the first 24 h after ICU admission did not predict hospital mortality in the medical ICU59. Patients with chronic obstructive lung diseases treated with corticosteroids developed significant hyperglycemia, but the increase in blood glucose levels did not correlate with the maximum dose of corticosteroids and were not associated with mortality, length of hospital stay, or re-admission rates60. The duration of hyperglycemia or the amount of insulin given did not have a major impact on the outcome of patients with primary acute neuromuscular respiratory failure61. Consistent with our previous work that showed elevated glycemic gaps were associated with adverse outcomes in diabetic patients with liver abscesses, CAP and ICU stays62,63,64, we found that elevated glycemic gaps were also associated with MACEs in diabetic patients with AMI. We speculate that the acute surge of glucose levels beyond the long-term average (or in nondiabetic patients) should be used as a surrogate marker for acute physiological stress. Furthermore, pre-existing hyperglycemia in diabetic patients may be a confounding factor for the prediction of MACEs in patients with AMI.
Chronic hyperglycemia had been shown to associate with smaller peak creatine kinase levels in patients with acute hyperglycemia65. Consistent with previous studies regarding chronic hyperglycemia assessed by HbA1c could not predict infarct size, short-term outcomes or in-hospital mortality in patients with AMI65,66,67,68, we again revealed that improved blood glucose control was not associated with superior outcomes in patients with AMI. While HbA1c has strong association with long-term prognosis, the short-term prognostic effects might have been weakened by the relative shorter study period in a limited number of patients69,70. An elevated HbA1c level had also been shown to not associated with a higher incidence of contrast induced-acute kidney injury compared to optimal HbA1c levels in patients with type 2 diabetes71. The possible adverse consequences of more stringent glycemic controls in diabetic patients have been further illustrated in two studies. In the Action in Diabetes and Vascular Diseases: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) and Action to Control Cardiovascular Risk in Diabetes (ACCORD) studies, aggressive glucose control to reduce the HbA1c levels from 7.5 to 6.5% and 8.3 to 6.4% had resulted in only nonsignificant beneficial trend in mortality and even significantly increased mortality respectively72,73. Several hypothetical reasons have been proposed to explain the lack of an association between HbA1c levels and outcomes in previously mentioned and current studies. Physiological and cellular readjustments in response to hyperglycemia occur over time in diabetic patients and the speed of correction of hyperglycemia in readjusted diabetic patients with higher HbA1c might adversely affect the outcomes74. We speculate that the readjustment of the blood glucose to a higher set-point value might influence the subsequent biological and clinical effects of acute fluctuation of blood glucose, possibly exert paradoxical protective effects during an acute stress, and hence result in lower GRACE scores and shorter hospital stays. The potential adverse influence of uncontrolled DM on platelet reactivity might have been mitigated by dual antiplatelet therapy used universally in the reperfusion era75,76,77. Mechanistically, decreased activity of the sodium proton exchanger in diabetic myocardium might attenuate reperfusion injury and therefore paradoxically prevents the diabetic heart from ischemic insults78. Since there were no statistically significant differences in the levels of glycemic gaps between HbA1c groups, higher MACEs in patients with better chronic blood glucose control cannot be attributed to lower ADAG levels alone.
Limitations
Our study has several limitations. First, it was a retrospective design and thus may have been subjected to selection bias. We believe that a prospective study of glycemic gaps in both diabetic and non-diabetes patients should be conducted to clarify the usefulness of the glycemic gap as a biomarker. Second, the adequacy of glycemic control during hospitalization might have influenced the outcomes. In the present study, we did not specifically address the effect of glycemic control during hospitalization. Although the diagnostic performance of glycemic gaps in this AMI setting was unfavorable when compared with our previous studies62,63,64, we demonstrated that glycemic gaps were superior to acute hyperglycemia as a risk predictor in diabetic patients. We acknowledge that the ADAG study was originally designed to investigate the correlation between HbA1c levels and average capillary glucose levels9. The capillary glucose level is slightly higher than serum glucose levels in critically ill ICU patients. The correlation coefficient between capillary and serum glucose levels was 0.91179. Another study revealed that the association between venous and capillary glucose values varied. In people with type 2 diabetes, venous plasma was higher than capillary blood for random and fasting samples and lower for samples collected 2 hours after oral glucose80. The discrepancy between serum blood glucose levels and capillary whole blood glucose levels was less than 5% during a semiannual quality control project conducted at our institution. Although the correlation between capillary and serum glucose levels was good, the data should be interpreted with caution. The serum levels of insulin were not routinely determined in patients with AMI; thus, we were unable to elucidate the association between glycemic gaps and hyperinsulinemia. We believe that incorporating serum insulin levels and insulin resistance studies would provide insight into the pathophysiology of SIH. Notably, our study population had higher levels of creatinine and BNP when compared with other AMI studies. One explanation for this finding is that there were 50.1% of the patients in the present study had chronic kidney disease (CKD). The prevalence of CKD was compatible with previous studies regarding diabetic patients presenting with AMI (39.9 to 77%)81,82,83,84. The plasma concentration of BNP is commonly elevated in patients with CKD and correlates weakly with renal function85. Nonetheless, the plasma BNP level is a reliable marker of left ventricle overload in patients with CKD86. The selection bias of BNP measurements might have resulted in higher values in our study, i.e., those patients who had plasma BNP determinations in the ER (49.5%) might have had more severe heart failure.
Conclusion
Elevated glycemic gaps between admission serum glucose levels and the ADAG were associated with an increased risk of mortality in patients with diabetes presenting with AMI. We suggest that the glycemic gap could be further studied as an adjunct assessment to determine the severity and prognosis of diabetic patients presenting with AMI. The association between glycemic gap, chronic blood glucose controls and the outcomes should be further explored in prospective longitudinal studies.
Additional Information
How to cite this article: Liao, W.-I. et al. An Elevated Glycemic Gap is Associated with Adverse Outcomes in Diabetic Patients with Acute Myocardial Infarction. Sci. Rep. 6, 27770; doi: 10.1038/srep27770 (2016).
References
Stranders, I. et al. Admission blood glucose level as risk indicator of death after myocardial infarction in patients with and without diabetes mellitus. Arch Intern Med 164, 982–988, 10.1001/archinte.164.9.982 (2004).
Deckers, J. W., van Domburg, R. T., Akkerhuis, M. & Nauta, S. T. Relation of admission glucose levels, short- and long-term (20-year) mortality after acute myocardial infarction. Am J Cardiol 112, 1306–1310, 10.1016/j.amjcard.2013.06.007 (2013).
Shah, B., Amoroso, N. S. & Sedlis, S. P. Hyperglycemia in nondiabetic patients presenting with acute myocardial infarction. Am J Med Sci 343, 321–326, 10.1097/MAJ.0b013e31822fb423 (2012).
Dandona, P. & Chaudhuri, A. Diabetes: Glycaemia and insulin after acute myocardial infarction. Nat Rev Endocrinol 10, 448–450, 10.1038/nrendo.2014.101 (2014).
Marik, P. E. & Raghavan, M. Stress-hyperglycemia, insulin and immunomodulation in sepsis. Intensive Care Med 30, 748–756, 10.1007/s00134-004-2167-y (2004).
Schuetz, P. et al. Initial management of septic patients with hyperglycemia in the noncritical care inpatient setting. Am J Med 125, 670–678, 10.1016/j.amjmed.2012.03.001 (2012).
Tiruvoipati, R. et al. Stress hyperglycemia may not be harmful in critically ill patients with sepsis. J Crit Care 27, 153–158, 10.1016/j.jcrc.2011.06.011 (2012).
Egi, M. et al. Blood glucose concentration and outcome of critical illness: the impact of diabetes. Crit Care Med 36, 2249–2255, 10.1097/CCM.0b013e318181039a (2008).
Nathan, D. M. et al. Translating the A1C assay into estimated average glucose values. Diabetes Care 31, 1473–1478, 10.2337/dc08-0545 (2008).
McAlister, F. A. et al. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care 28, 810–815 (2005).
Standards of medical care in diabetes–2014. Diabetes Care 37 Suppl 1, S14–80, 10.2337/dc14-S014 (2014).
Gillett, M. J. International Expert Committee report on the role of the A1c assay in the diagnosis of diabetes: Diabetes Care 2009; 32(7): 1327–1334. Clin Biochem Rev 30, 197–200 (2009).
Thygesen, K. et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 60, 1581–1598, 10.1016/j.jacc.2012.08.001 (2012).
Backus, B. E. et al. Risk scores for patients with chest pain: evaluation in the emergency department. Curr Cardiol Rev 7, 2–8, 10.2174/157340311795677662 (2011).
El-Menyar, A. et al. Killip classification in patients with acute coronary syndrome: insight from a multicenter registry. Am J Emerg Med 30, 97–103, 10.1016/j.ajem.2010.10.011 (2012).
Thomas, M. E. et al. The definition of acute kidney injury and its use in practice. Kidney Int 87, 62–73, 10.1038/ki.2014.328 (2015).
Pencina, M. J., D’Agostino, R. B. Sr., D’Agostino, R. B. Jr. & Vasan, R. S. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27, 157–172; discussion 207-112, 10.1002/sim.2929 (2008).
McCowen, K. C., Malhotra, A. & Bistrian, B. R. Stress-induced hyperglycemia. Crit Care Clin 17, 107–124 (2001).
Leonidou, L. et al. Cytokine production and hospital mortality in patients with sepsis-induced stress hyperglycemia. J Infect 55, 340–346, 10.1016/j.jinf.2007.05.177 (2007).
Angeli, F. et al. Hyperglycemia in acute coronary syndromes: from mechanisms to prognostic implications. Ther Adv Cardiovasc Dis, 10.1177/1753944715594528 (2015).
Webster, K. A. Stress hyperglycemia and enhanced sensitivity to myocardial infarction. Curr Hypertens Rep 10, 78–84 (2008).
Ujueta, F., Weiss, E. N., Sedlis, S. P. & Shah, B. Glycemic Control in Coronary Revascularization. Curr Treat Options Cardiovasc Med 18, 12, 10.1007/s11936-015-0434-6 (2016).
Chen, Y. et al. Stress-induced hyperglycemia after hip fracture and the increased risk of acute myocardial infarction in nondiabetic patients. Diabetes Care 36, 3328–3332, 10.2337/dc13-0119 (2013).
Jafar, N., Edriss, H. & Nugent, K. The Effect of Short-Term Hyperglycemia on the Innate Immune System. Am J Med Sci 351, 201–211, 10.1016/j.amjms.2015.11.011 (2016).
Otsuka, A. et al. Temporary hyperglycaemia provokes monocyte adhesion to endothelial cells in rat thoracic aorta. Diabetologia 48, 2667–2674, 10.1007/s00125-005-0005-6 (2005).
Azuma, K. et al. Repetitive fluctuations in blood glucose enhance monocyte adhesion to the endothelium of rat thoracic aorta. Arterioscler Thromb Vasc Biol 26, 2275–2280, 10.1161/01.atv.0000239488.05069.03 (2006).
Ghosh, R. et al. The appearance of dermcidin isoform 2, a novel platelet aggregating agent in the circulation in acute myocardial infarction that inhibits insulin synthesis and the restoration by acetyl salicylic acid of its effects. J Thromb Thrombolysis 31, 13–21, 10.1007/s11239-010-0515-z (2011).
Ghosh, R., Bhattacharya, R., Bhattacharya, G. & Sinha, A. K. The Control of Stress Induced Type I Diabetes Mellitus in Humans through the Hepatic Synthesis of Insulin by the Stimulation of Nitric Oxide Production. Int J Biomed Sci 8, 171–182 (2012).
Ray, U. et al. Isolation and study of insulin activated nitric oxide synthase inhibitory protein in acute myocardial infarction subjects. J Thromb Thrombolysis 33, 218–229, 10.1007/s11239-011-0672-8 (2012).
Ghosh, R., Maji, U. K., Bhattacharya, R. & Sinha, A. K. The role of dermcidin isoform 2: a two-faceted atherosclerotic risk factor for coronary artery disease and the effect of acetyl salicylic Acid on it. Thrombosis 2012, 987932, 10.1155/2012/987932 (2012).
Marik, P. E. & Bellomo, R. Stress hyperglycemia: an essential survival response! Crit Care 17, 305, 10.1186/cc12514 (2013).
Oswald, G. A., Smith, C. C., Betteridge, D. J. & Yudkin, J. S. Determinants and importance of stress hyperglycaemia in non-diabetic patients with myocardial infarction. Br Med J (Clin Res Ed) 293, 917–922 (1986).
Schuetz, P. et al. Effect of hyperglycaemia on inflammatory and stress responses and clinical outcome of pneumonia in non-critical-care inpatients: results from an observational cohort study. Diabetologia 57, 275–284, 10.1007/s00125-013-3112-9 (2014).
Hirata, Y. et al. Association of hyperglycemia on admission and during hospitalization with mortality in diabetic patients admitted for pneumonia. Intern Med 52, 2431–2438 (2013).
Lepper, P. M. et al. Serum glucose levels for predicting death in patients admitted to hospital for community acquired pneumonia: prospective cohort study. BMJ 344, e3397, 10.1136/bmj.e3397 (2012).
Teraguchi, I. et al. Impact of stress hyperglycemia on myocardial salvage following successfully recanalized primary acute myocardial infarction. Circ J 76, 2690–2696 (2012).
Kavanagh, B. P. & McCowen, K. C. Glycemic Control in the ICU. New England Journal of Medicine 363, 2540–2546, 10.1056/NEJMcp1001115 (2010).
Ekmekci, A. et al. Admission hyperglycemia predicts inhospital mortality and major adverse cardiac events after primary percutaneous coronary intervention in patients without diabetes mellitus. Angiology 65, 154–159, 10.1177/0003319713488930 (2014).
Zhang, J. W. et al. Impact of stress hyperglycemia on in-hospital stent thrombosis and prognosis in nondiabetic patients with ST-segment elevation myocardial infarction undergoing a primary percutaneous coronary intervention. Coron Artery Dis 24, 352–356, 10.1097/MCA.0b013e328361a942 (2013).
Hoebers, L. P. et al. Predictive value of plasma glucose level on admission for short and long term mortality in patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention. Am J Cardiol 109, 53–59, 10.1016/j.amjcard.2011.07.067 (2012).
Lazaros, G. et al. Distinct association of admission hyperglycemia with one-year adverse outcome in diabetic and non-diabetic patients with acute ST-elevation myocardial infarction. Hellenic J Cardiol 54, 119–125 (2013).
Yang, J. H. et al. Prognostic value of admission blood glucose level in patients with and without diabetes mellitus who sustain ST segment elevation myocardial infarction complicated by cardiogenic shock. Crit Care 17, R218, 10.1186/cc13035 (2013).
de Mulder, M. et al. Intensive glucose regulation in hyperglycemic acute coronary syndrome: results of the randomized BIOMarker study to identify the acute risk of a coronary syndrome-2 (BIOMArCS-2) glucose trial. JAMA Intern Med 173, 1896–1904, 10.1001/jamainternmed.2013.10074 (2013).
Viasus, D., Simonetti, A., Garcia-Vidal, C. & Carratala, J. Prediction of prognosis by markers in community-acquired pneumonia. Expert Rev Anti Infect Ther 11, 917–929, 10.1586/14787210.2013.825442 (2013).
Schuetz, P., Litke, A., Albrich, W. C. & Mueller, B. Blood biomarkers for personalized treatment and patient management decisions in community-acquired pneumonia. Curr Opin Infect Dis 26, 159–167, 10.1097/QCO.0b013e32835d0bec (2013).
Egi, M., Bellomo, R., Stachowski, E., French, C. J. & Hart, G. Variability of blood glucose concentration and short-term mortality in critically ill patients. Anesthesiology 105, 244–252 (2006).
Egi, M. et al. The interaction of chronic and acute glycemia with mortality in critically ill patients with diabetes. Crit Care Med 39, 105–111, 10.1097/CCM.0b013e3181feb5ea (2011).
English, E. et al. The effect of anaemia and abnormalities of erythrocyte indices on HbA1c analysis: a systematic review. Diabetologia 58, 1409–1421, 10.1007/s00125-015-3599-3 (2015).
Spencer, D. H., Grossman, B. J. & Scott, M. G. Red cell transfusion decreases hemoglobin A1c in patients with diabetes. Clin Chem 57, 344–346, 10.1373/clinchem.2010.157321 (2011).
Bruno, A. et al. Admission glucose level and clinical outcomes in the NINDS rt-PA Stroke Trial. Neurology 59, 669–674 (2002).
Kamouchi, M. et al. Prestroke glycemic control is associated with the functional outcome in acute ischemic stroke: the Fukuoka Stroke Registry. Stroke 42, 2788–2794, 10.1161/STROKEAHA.111.617415 (2011).
Rueda, A. M. et al. Hyperglycemia in diabetics and non-diabetics: effect on the risk for and severity of pneumococcal pneumonia. J Infect 60, 99–105, 10.1016/j.jinf.2009.12.003 (2010).
Martin, W. G., Galligan, J., Simpson, S. Jr., Greenaway, T. & Burgess, J. Admission blood glucose predicts mortality and length of stay in patients admitted through the emergency department. Intern Med J, 10.1111/imj.12841 (2015).
Falciglia, M., Freyberg, R. W., Almenoff, P. L., D’Alessio, D. A. & Render, M. L. Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Crit Care Med 37, 3001–3009, 10.1097/CCM.0b013e3181b083f7 (2009).
Lheureux, O. & Preiser, J. C. Year in review 2013: Critical Care–metabolism. Crit Care 18, 571, 10.1186/s13054-014-0571-4 (2014).
Krinsley, J. S. et al. Diabetic status and the relation of the three domains of glycemic control to mortality in critically ill patients: an international multicenter cohort study. Crit Care 17, R37, 10.1186/cc12547 (2013).
Sechterberger, M. K. et al. The effect of diabetes mellitus on the association between measures of glycaemic control and ICU mortality: a retrospective cohort study. Crit Care 17, R52, 10.1186/cc12572 (2013).
Kaukonen, K. M. et al. Stress hyperlactatemia modifies the relationship between stress hyperglycemia and outcome: a retrospective observational study. Crit Care Med 42, 1379–1385, 10.1097/CCM.0000000000000214 (2014).
Freire, A. X., Bridges, L., Umpierrez, G. E., Kuhl, D. & Kitabchi, A. E. Admission hyperglycemia and other risk factors as predictors of hospital mortality in a medical ICU population. Chest 128, 3109–3116, 10.1378/chest.128.5.3109 (2005).
Islam, E. A., Limsuwat, C., Nantsupawat, T., Berdine, G. G. & Nugent, K. M. The association between glucose levels and hospital outcomes in patients with acute exacerbations of chronic obstructive pulmonary disease. Ann Thorac Med 10, 94–99, 10.4103/1817-1737.151439 (2015).
Cabrera-Serrano, M., Fugate, J. E., Mandrekar, J. & Rabinstein, A. A. Impact of Hyperglycemia in the Outcome of Patients with Primary Neuromuscular Respiratory Failure. Neurocrit Care, 10.1007/s12028-015-0114-0 (2015).
Liao, W. I. et al. An elevated gap between admission and A1C-derived average glucose levels is associated with adverse outcomes in diabetic patients with pyogenic liver abscess. PLos One 8, e64476, 10.1371/journal.pone.0064476 (2013).
Chen, P. C. et al. An Elevated Glycemic Gap is Associated With Adverse Outcomes in Diabetic Patients With Community-Acquired Pneumonia. Medicine (Baltimore) 94, e1456, 10.1097/md.0000000000001456 (2015).
Liao, W. I. et al. Usefulness of Glycemic Gap to Predict ICU Mortality in Critically Ill Patients With Diabetes. Medicine (Baltimore) 94, e1525, 10.1097/md.0000000000001525 (2015).
Fujino, M. et al. Impact of acute and chronic hyperglycemia on in-hospital outcomes of patients with acute myocardial infarction. Am J Cardiol 114, 1789–1793, 10.1016/j.amjcard.2014.09.015 (2014).
Liu, Y. et al. Haemoglobin A(1c), acute hyperglycaemia and short-term prognosis in patients without diabetes following acute ST-segment elevation myocardial infarction. Diabet Med 29, 1493–1500, 10.1111/j.1464-5491.2012.03641.x (2012).
Cao, J. J., Hudson, M., Jankowski, M., Whitehouse, F. & Weaver, W. D. Relation of chronic and acute glycemic control on mortality in acute myocardial infarction with diabetes mellitus. Am J Cardiol 96, 183–186, 10.1016/j.amjcard.2005.03.040 (2005).
Britton, K. A. et al. No association between hemoglobin A1c and in-hospital mortality in patients with diabetes and acute myocardial infarction. Am Heart J 161, 657–663.e651, 10.1016/j.ahj.2010.12.004 (2011).
Su, G. et al. Impact of admission glycemic variability, glucose, and glycosylated hemoglobin on major adverse cardiac events after acute myocardial infarction. Diabetes Care 36, 1026–1032, 10.2337/dc12-0925 (2013).
Su, G. et al. Prognostic value of early in-hospital glycemic excursion in elderly patients with acute myocardial infarction. Cardiovasc Diabetol 12, 33, 10.1186/1475-2840-12-33 (2013).
Akyuz, S. et al. Association between Glycosylated Haemoglobin Level and Contrast-Induced Acute Kidney Injury in Patients with Type 2 Diabetes Mellitus. Cardiorenal Med 4, 95–102 (2014).
Patel, A. et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358, 2560–2572, 10.1056/NEJMoa0802987 (2008).
Gerstein, H. C. et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358, 2545–2559, 10.1056/NEJMoa0802743 (2008).
Krinsley, J. S., Meyfroidt, G., van den Berghe, G., Egi, M. & Bellomo, R. The impact of premorbid diabetic status on the relationship between the three domains of glycemic control and mortality in critically ill patients. Curr Opin Clin Nutr Metab Care 15, 151–160, 10.1097/MCO.0b013e32834f0009 (2012).
Angiolillo, D. J. et al. Platelet function profiles in patients with type 2 diabetes and coronary artery disease on combined aspirin and clopidogrel treatment. Diabetes 54, 2430–2435 (2005).
Singla, A., Orshaw, P., Boura, J. & Harjai, K. J. Glycosylated hemoglobin and outcomes in diabetic patients with acute myocardial infarction after successful revascularization with stent placement: findings from the guthrie health off-label stent (GHOST) investigators. J Interv Cardiol 25, 262–269, 10.1111/j.1540-8183.2011.00715.x (2012).
Gaborit, B., Frere, C., Cuisset, T., Alessi, M. C. & Dutour, A. Enhanced post-clopidogrel platelet reactivity in diabetic patients is independently related to plasma fibrinogen level but not to glycemic control. J Thromb Haemost 7, 1939–1941, 10.1111/j.1538-7836.2009.03599.x (2009).
Ramasamy, R. & Schaefer, S. Inhibition of Na+-H+Exchanger Protects Diabetic and Non-Diabetic Hearts From Ischemic Injury: Insight into Altered Susceptibility of Diabetic Hearts to Ischemic Injury. Journal of Molecular and Cellular Cardiology 31, 785–797, http://dx.doi.org/10.1006/jmcc.1998.0908 (1999).
Critchell, C. D. et al. Accuracy of bedside capillary blood glucose measurements in critically ill patients. Intensive Care Med 33, 2079–2084, 10.1007/s00134-007-0835-4 (2007).
Colagiuri, S. et al. Comparability of venous and capillary glucose measurements in blood. Diabet Med 20, 953–956 (2003).
Kim, C. S. et al. Association of metabolic syndrome and renal insufficiency with clinical outcome in acute myocardial infarction. Metabolism 62, 669–676, 10.1016/j.metabol.2012.11.002 (2013).
Vichova, T., Knot, J., Ulman, J., Maly, M. & Motovska, Z. The impact of stage of chronic kidney disease on the outcomes of diabetics with acute myocardial infarction treated with percutaneous coronary intervention. Int Urol Nephrol, 10.1007/s11255-016-1260-9 (2016).
Han, J. H. et al. Chronic kidney disease in patients with non-ST-segment elevation acute coronary syndromes. Am J Med 119, 248–254, 10.1016/j.amjmed.2005.08.057 (2006).
Liu, Y. et al. Impact of renal dysfunction on long-term outcomes of elderly patients with acute coronary syndrome: a longitudinal, prospective observational study. BMC Nephrol 15, 78, 10.1186/1471-2369-15-78 (2014).
McCullough, P. A. et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis 41, 571–579, 10.1053/ajkd.2003.50118 (2003).
Takami, Y. et al. Diagnostic and prognostic value of plasma brain natriuretic peptide in non-dialysis-dependent CRF. Am J Kidney Dis 44, 420–428 (2004).
Acknowledgements
This study was supported by a grant from the Tri-Service General Hospital of the National Defense Medical Center in Taipei, Taiwan (TSGH-C105-056) and the Ministry of Science and Technology in Taiwan (MOST-104-2314-B-106-043-MY2).
Author information
Authors and Affiliations
Contributions
W.-I.L. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. C.-S.L., C.-W.H. and S.-H.T. contributed to the design of the study. J.-C.W., C.-H.L. and S.-H.T. contributed to the literature review and writing of the manuscript. Y.-C.W. and W.-C.C. contributed to the data collection. W.-I.L. contributed to the statistical analysis. All authors contributed to the review and approval of the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Liao, WI., Lin, CS., Lee, CH. et al. An Elevated Glycemic Gap is Associated with Adverse Outcomes in Diabetic Patients with Acute Myocardial Infarction. Sci Rep 6, 27770 (2016). https://doi.org/10.1038/srep27770
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep27770
This article is cited by
-
Predictive value of glycemic gap and stress glycemia ratio among critically ill patients with acute kidney injury: a retrospective analysis of the MIMIC-III database
BMC Nephrology (2023)
-
The relationship between glycated hemoglobin A1c levels and exacerbation status in the patients with chronic obstructive pulmonary disease
BMC Research Notes (2022)
-
Quantitative Analysis of Stress-Induced Hyperglycemia and Intracranial Blood Volumes for Predicting Mortality After Intracerebral Hemorrhage
Translational Stroke Research (2022)
-
Elevated Glycemic Gap Predicts Acute Respiratory Failure and In-hospital Mortality in Acute Heart Failure Patients with Diabetes
Scientific Reports (2019)
-
Association of multiple glycemic parameters at intensive care unit admission with mortality and clinical outcomes in critically ill patients
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.