Abstract
The dipping variations of circadian blood pressure (BP) correlate closely with target-organ damages and cardiovascular events. The aim of this study was to investigate the relationship between BP reverse dipping and the prevalence of stable coronary artery disease (sCAD) in hypertensive patients. Clinical data and the results of 24-hour ambulatory BP monitoring (ABPM) were obtained from 718 hypertensive patients (390 males, mean age 59.6 ± 13.8 years) in a single centre in Northern China. Reverse dipping pattern was defined as nocturnal systolic BP (SBP) was higher than daytime SBP. A logistic regression model was applied to explore the independent risk factors of sCAD. The patients with BP reverse dipping accounted for 31.5% in sCAD group and 19.5% in control group (P < 0.05). In multivariate analysis, BP reverse dipping remained significantly associated with the prevalence of sCAD (Odds ratio [OR], 1.772; p = 0.027). Furthermore, the circadian decline rate of SBP was independently associated with sCAD (OR, 0.975; p = 0.043). The hypertensive patients with reverse BP dipping were found to be more frequently suffering from sCAD. BP reverse dipping examined with 24-hour ABPM may indicate sCAD.
Similar content being viewed by others
Introduction
Blood pressure (BP) presents a reproducible circadian pattern, which is normally lower at night than during the day by approximately 10–20%, mostly due to endogenous neuroendocrine rhythms and other variables1. Circadian BP variations have been gradually realized as an important predictor for a range of organ damages and cardiovascular events2,3,4. According to the nocturnal BP dipping, circadian BP patterns are classified as extreme dipping (night/day ratio ≤ 0.8), dipping (0.8< ratio ≤ 0.9), nondipping (0.9< ratio ≤ 1.0) and reverse dipping (ratio >1.0)5. BP reverse dipping, with higher mean night SBP than daytime, was previously categorized as part of “nondipping”6,7. Recently, the growing numbers of studies have shown that BP reverse dipping is an independent risk factor for a range of cardiovascular and other morbidities7,8,9.
Our previous studies have demonstrated that BP reverse dipping was exposed to higher risks for lacuna infarction and carotid plaque formation, which was shown to be able to predict coronary artery disease (CAD) accurately10,11,12. CAD is the most common type of cardiovascular disease, resulting in millions of death across the world13. It is well substantiated that hypertension is one of the most important risk factors for CAD14. Furthermore, while blunted nocturnal BP dipping has also been proved to be a cardiovascular risk predictor, a previous study reported myocardial ischemia might follow certain type of circadian BP changes6,15.
There are published evidences indicating carotid plaque could predict ischemic stroke and CAD accurately in clinical practice11,16,17. Therefore, we hypothesize a potential link between reverse dipping of BP and CAD. The aim of this cross-sectional study was to investigate whether or not the hypertensive patient with BP reverse dipping status had higher prevalence of stable CAD (sCAD). The results may further strengthen the necessity of circadian BP rhythm administration, especially in hypertensive patients with reverse dipping.
Results
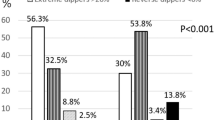
The age of all hypertensive patients (257 sCAD and 461 non-sCAD) is 59.6 ± 13.8 years (range: 21 to 87) in average, 54.3% of the participates were males, 29.9% were current smokers, 26.3% had diabetes mellitus and 24-hour SBP were 134.6 ± 14.0 mmHg. Hypertensive patients with sCAD (31.5%) had higher percentage of BP reverse dipping pattern than control group (19.5%) (p = 0.004). In the meanwhile, the proportion of dipping pattern was 18.3% in sCAD group and 28.2% in non-sCAD group. Moreover, the ratio of nondipping pattern was similar between sCAD (50.2%) and non-sCAD (52.3%). Other clinical characteristics of the participates are shown in Table 1. There was no gender difference in the circadian BP patterns (Supplement Table 1).
The distribution of hypertensive patients with sCAD in dipping, nondipping and reverse dipping group was 26.6%, 34.9% and 47.4%, respectively. After using chi-squared test, the difference between dipping and non-dipping (p = 0.031), dipping and reverse dipping (p < 0.001), non-dipping and reverse dipping (p = 0.004) were statistically significant. Patients with reverse dipping pattern had a lowest prevalence of non-sCAD while had a highest prevalence of sCAD (Fig. 1, p < 0.01).
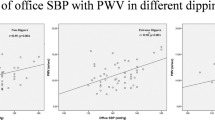
In univariate analysis, the risk factor related to the presence of sCAD were age, gender, smoking, diabetes, cholesterol, triglycerides, 24-hour SBP, 24-hour DBP, nondipping and reverse dipping of BP. For further multivariate logistic regression analysis, BP reverse dipping (OR = 1.772, P = 0.027), age (OR = 1.064, P < 0.001) and total cholesterol (OR = 1.226, P = 0.035) were significantly correlated with sCAD (Table 2). In addition to this, circadian decline rate of SBP (OR = 0.975, P = 0.043) was significantly related to sCAD (Fig. 2).
Our previous study revealed that diabetes and reverse dipping were interrelated risk factor for each other. This study also found that diabetes (OR = 1.588, P = 0.020) and age (OR = 1.034, P < 0.001) were significantly associated with reverse dipping (Supplement Table 2). After exclusion of sCAD patient with diabetes, reverse dipping was still an independent risk factor for sCAD (OR 1.673, P = 0.038; data not shown).
Discussion
Hypertension is a well-recognized risk factor for CAD14. Although not written into guidelines, amount of evidences indicated the fluctuations of BP over a certain period could provide additional prognostic value. For example, visit-to-visit BP variability, a type of long-term variability, was previously considered to be non-specific but now shown to be associated with stroke, in most studies, if not all18. Circadian and minute-to-minute BP variability revealed by ABPM have both been studied and gradually recognized as important cardiovascular risk factors as well2,19. ABPM is a noninvasive examination of circadian BP over a span of 24 hours, providing valuable diagnostic information for patients with fluctuating BP and circadian BP profile20,21,22.
Circadian BP variations were used to be divided into dipper (mean nocturnal BP drops 10 mmHg or more than that in daytime) and “non-dipper”23,24. Previously, there has been a series reports demonstrating the relationship between “non-dipper” and cardiovascular complications such as lacunar infarction, metabolic syndrome and myocardial ischemia in hypertensive patients with CAD15,24,25. Other reports also stressed on the important prognostic value of “non-dipper”25,26,27. Unfortunately, conflicts exist, especially when comparing our clinical observations with those findings.
We have previously found “non-dippers” had significant heterogeneity in complications among a small population of hypertensive patients. To further clarify the impact of different circadian BP patterns, we divided the patients into normal dipping (night-to-day SBP ratio ≤ 0.9 and >0.8), extreme dipping (night-to-day SBP ratio ≤ 0.8), nondipping (night-to-day SBP ratio ≤ 1.0 and >0.9) and reverse dipping (night-to-day SBP ratio >1.0) according to previous literature28. After analysis of multivariate logistic regression, reverse-dipper pattern (OR 2.677; 95%CI 1.226–5.842; p < 0.05), not non-dipper pattern, was directly associated with lacunar infarction12.
As a particular portion of non-dipper pattern, reverse dipper pattern has been shown to correlate with the highest incidence of cardiovascular events and worst prognosis in hypertensive patients, comparing with the dippers and non-dippers5. Our cross-sectional studies in patients comprising dipper, non-dipper and reverse dipper groups further confirmed, instead of non-dipper, nocturnal rise of BP may associate with MetS in male20 and early formation of carotid plaque in senior hypertensive patients10. Additionally, in the current study, our results showed that reverse dipper pattern of BP was positively associated with the prevalence of sCAD. Therefore, reverse dipper pattern of BP may be an independent risk factor to predict the incidence of CAD.
Although the relationship may be present between reverse dipper pattern of BP and CAD, the pathophysiological mechanism is far more to be investigated. We would like to propose that the higher risk of atherosclerosis associated with reverse dipper pattern of BP may relate to relatively higher blood mechanical forces on endothelial cells, leading to the damage of vascular integrity. It has been revealed that BP variability may correlate with aortic wall remodeling and reduced aortic compliance in the animal experiment29. On the other hand, the sensitivity of arterial baroreceptor could be compromised due to large arterial stiffness and resulted in abnormal BP variability18. Another report suggested that coronary artery calcium might serve as a potential mediator involved in the relationship between abnormal nighttime BP pattern and cardiovascular disease30. In addition, the Sympathetic Nervous System (SNS) also plays important roles in the regulation of blood pressure and chronic SNS overactivity could contribute to the development of hypertension and may change the BP pattern31. SNS also result in an elevated inflammatory response and destabilization of atherosclerotic plaques32. Therefore, the SNS may be a significant link between BP variation and CAD, which worth to be studied in the future33,34.
Ultrasound assessment of carotid plaque is a non-invasive imaging test to evaluate the cardiovascular complications of patient35. Ellisiv et al.16 suggested that total plaque area and carotid intima-media thickness (CIMT), were closely related to ischemic stroke. Moreover, accumulating evidences indicated that the carotid plaque represent atherosclerotic pathogenesis more accurately than CIMT17. Previous meta-analysis also revealed that the ultrasound detection of carotid plaque had a higher prognostic accuracy for the prediction of future CAD events than CIMT11. Together with our previous discovery about reverse BP dipping and carotid plaque, it is reasonable to hypothesize that reverse dipping may serve as a risk factor for CAD. Therefore, future prospective studies in human are needed to look into the potential network of regulation36.
To our knowledge, this is the first study to report the association between reverse dipper pattern of BP and the incidence of sCAD in individuals with hypertension. Therefore, the development of antihypertensive medicine with an effect on decreased fall of nocturnal BP may influence the development of sCAD. Further studies are needed to address the differing impact of extreme-dipper pattern on CAD in hypertensive patients. In addition, multiple ABPM over a longer period of time may provide more information.
Methods
Study Population
Hypertensive patient selection and data retrieval were extracted from ABPM database from April 2012 to June 2013 (n = 1740) in the Second Affiliated Hospital, Xi’an Jiaotong University School of Medicine, Northern China. Hypertensive patients were defined as office BP ≥ 140/90 mmHg or 24-hour ABPM ≥ 135/85 mmHg37. Because the treatments of hypertension have influence on the circadian BP variation, we selected patients who were not treated with antihypertensive drug or first detected hypertension. 718 patients (390 men and 328 women) with essential hypertension who fulfilled exclusion criteria were eventually included in our cross-sectional study (Fig. 3). All patients were referred due to standard indications that have been shown to use ABPM for appropriate clinical circumstances20,38. ABPM were carried out for diagnosis of hypertension and assessment of vascular risk in adults with the approved guidelines39. The study protocol was approved by the Ethics Committee of the Second Affiliated Hospital, Xi’an Jiaotong University School of Medicine. All the participants read the purpose statement of the investigation and each provided a written informed consent.
ABPM measurement
Ambulatory BP was monitored over a 24-hour period using an oscillometric device (Spacelabs 90207; Spacelabs, Redmond, WA, USA). All the participants were asked to record their activities, sleep times and sleep quality during the monitoring session. Strenuous physical activity was discouraged during the monitoring period. The BP recording was made every 30 min from 7:00 AM till 11:00 PM and every 60 min from 11:00 PM till 7:00 AM. The parameters evaluated were mean 24-hour systolic and diastolic BP (SBP and DBP), SBP- and DBP-awakening, SBP- and DBP-bedtime. We divided the patient according to nocturnal BP reduction as follow: normal dipping (night-to-day SBP ratio ≤ 0.9 and >0.8), extreme dipping (night-to-day SBP ratio ≤ 0.8), nondipping (night-to-day SBP ratio ≤ 1.0 and >0.9) and reverse dipping (night-to-day SBP ratio >1.0)28.
The diagnosis and assessment of sCAD
The initial diagnostic approach for CAD encompasses syndrome, identifying significant dyslipidaemia, hyperglycaemia or other biochemical risk factors, chest radiography, echocardiography and an electrocardiogram. Once this initial evaluation is performed stress testing, CT angiography and a coronary angiogram may be necessary to obtain further diagnostic insight40.
Statistical Analysis
All the data was analyzed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Bivariate comparisons between patients with and without sCAD were performed by unpaired t-test (continuous variables) and by χ2-test (categorical variables), respectively. A logistic regression model was utilized to analyze the relationship between sCAD and age, gender, smoking, diabetes, cholesterol, triglycerides, circadian blood pressure variation and ABPM results. Variables with statistical significance in univariate models were then included in the multivariate analyses. A two-tailed P value of less than 0.05 was considered statistically significant.
Additional Information
How to cite this article: Yan, B. et al. Blood pressure reverse dipping may associate with stable coronary artery disease in patients with essential hypertension: a cross-sectional study. Sci. Rep. 6, 25410; doi: 10.1038/srep25410 (2016).
References
Izzedine, H., Launay-Vacher, V. & Deray, G. Abnormal blood pressure circadian rhythm: a target organ damage? Int J Cardiol. 107, 343–349, doi: 10.1016/j.ijcard.2005.03.046 (2006).
Fagard, R. H. et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 51, 55–61, doi: 10.1161/hypertensionaha.107.100727 (2008).
Hermida, R. C. Ambulatory blood pressure monitoring in the prediction of cardiovascular events and effects of chronotherapy: rationale and design of the MAPEC study. Chronobiol Int. 24, 749–775, doi: 10.1080/07420520701535837 (2007).
Manfredini, R. et al. Twenty-four-hour patterns in occurrence and pathophysiology of acute cardiovascular events and ischemic heart disease. Chronobiol Int. 30, 6–16, doi: 10.3109/07420528.2012.715843 (2013).
Fagard, R. H. Dipping pattern of nocturnal blood pressure in patients with hypertension. Expert rev Cardiovasc Ther. 7, 599–605, doi: 10.1586/erc.09.35 (2009).
de la Sierra, A. et al. Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 53, 466–472, doi: 10.1161/HYPERTENSIONAHA.108.124008 (2009).
Grassi, G. et al. Adrenergic, metabolic and reflex abnormalities in reverse and extreme dipper hypertensives. Hypertension. 52, 925–931, doi: 10.1161/HYPERTENSIONAHA.108.116368 (2008).
Wang, C. et al. Reversed dipper blood-pressure pattern is closely related to severe renal and cardiovascular damage in patients with chronic kidney disease. Plos One. 8, e55419, doi: 10.1371/journal.pone.0055419 (2013).
Kario, K. et al. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 38, 852–857 (2001).
Yan, B. et al. Blood Pressure Reverse-Dipping is Associated With Early Formation of Carotid Plaque in Senior Hypertensive Patients. Medicine. 94, e604, doi: 10.1097/md.0000000000000604 (2015).
Inaba, Y., Chen, J. A. & Bergmann, S. R. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. 220, 128–133, doi: 10.1016/j.atherosclerosis.2011.06.044 (2012).
Yan, B. et al. Reverse-dipper pattern of blood pressure may predict lacunar infarction in patients with essential hypertension. Eur J Neurol. 22, 1022–1025, doi: 10.1111/ene.12659 (2015).
Ross, R. The pathogenesis of atherosclerosis: a perspective for the 1990 s. Nature. 362, 801–809, doi: 10.1038/362801a0 (1993).
Drozda, J. Jr. et al. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation 124, 248–270, doi: 10.1161/CIR.0b013e31821d9ef2 (2011).
Pierdomenico, S. D. et al. Circadian blood pressure changes and myocardial ischemia in hypertensive patients with coronary artery disease. J Am Coll Cardiol. 31, 1627–1634 (1998).
Mathiesen, E. B. et al. Carotid plaque area and intima-media thickness in prediction of first-ever ischemic stroke: a 10-year follow-up of 6584 men and women: the Tromso Study. Stroke 42, 972–978, doi: 10.1161/strokeaha.110.589754 (2011).
Plichart, M. et al. Carotid intima-media thickness in plaque-free site, carotid plaques and coronary heart disease risk prediction in older adults. The Three-City Study. Atherosclerosis. 219, 917–924, doi: 10.1016/j.atherosclerosis.2011.09.024 (2011).
Nagai, M. & Kario, K. Visit-to-visit blood pressure variability, silent cerebral injury and risk of stroke. Am J Hypertens. 26, 1369–1376, doi: 10.1093/ajh/hpt167 (2013).
Schillaci, G. & Parati, G. Determinants of blood pressure variability in youth: at the roots of hypertension. J Hypertens. 28, 660–664, doi: 10.1097/HJH.0b013e3283391950 (2010).
Pickering, T. G., Shimbo, D. & Haas, D. Ambulatory blood-pressure monitoring. New Engl J Med. 354, 2368–2374, doi: 10.1056/NEJMra060433 (2006).
Verdecchia, P. et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension 24, 793–801 (1994).
Hansen, T. W. et al. Predictive role of the nighttime blood pressure. Hypertension. 57, 3–10, doi: 10.1161/HYPERTENSIONAHA.109.133900 (2011).
O’Brien, E., Sheridan, J. & O’Malley, K. Dippers and non-dippers. Lancet. 2, 397 (1988).
McAlister, F. A. & Straus, S. E. Evidence based treatment of hypertension. Measurement of blood pressure: an evidence based review. BMJ. 322, 908–911 (2001).
Yokota, H. et al. Nocturnal Blood Pressure Pattern Affects Left Ventricular Remodeling and Late Gadolinium Enhancement in Patients with Hypertension and Left Ventricular Hypertrophy. Plos One. 8, e67825, doi: 10.1371/journal.pone.0067825 (2013).
Borel, A. L. et al. Short sleep duration is associated with a blood pressure nondipping pattern in type 1 diabetes: the DIAPASOM study. Diabetes care. 32, 1713–1715, doi: 10.2337/dc09-0422 (2009).
Routledge, F. & McFetridge-Durdle, J. Nondipping blood pressure patterns among individuals with essential hypertension: a review of the literature. Eur J Cardiovasc Nurs. 6, 9–26, doi: 10.1016/j.ejcnurse.2006.05.001 (2007).
Castelpoggi, C. H. et al. A blunted decrease in nocturnal blood pressure is independently associated with increased aortic stiffness in patients with resistant hypertension. Hypertens Res. 32, 591–596, doi: 10.1038/hr.2009.71 (2009).
Lacolley, P. et al. Aortic distensibility and structural changes in sinoaortic-denervated rats. Hypertension. 26, 337–340 (1995).
Viera, A. J. et al. Nighttime blood pressure dipping in young adults and coronary artery calcium 10–15 years later: the coronary artery risk development in young adults study. Hypertension 59, 1157–1163, doi: 10.1161/hypertensionaha.112.191536 (2012).
Grassi, G., Bombelli, M., Seravalle, G., Dell’Oro, R. & Quarti-Trevano, F. Diurnal blood pressure variation and sympathetic activity. Hypertens Res. 33, 381–385, doi: 10.1038/hr.2010.26 (2010).
Yang, Y. et al. Perceived stress status and sympathetic nervous system activation in young male patients with coronary artery disease in China. Eur J Int Med. 26, 726–730, doi: 10.1016/j.ejim.2015.08.005 (2015).
Lymperopoulos, A., Rengo, G. & Koch, W. J. Adrenergic nervous system in heart failure: pathophysiology and therapy. Circ Res. 113, 739–753, doi: 10.1161/circresaha.113.300308 (2013).
Preckel, D. & von Kanel, R. Regulation of Hemostasis by the Sympathetic Nervous System: Any Contribution to Coronary Artery Disease? Heartdrug. 4, 123–130, doi: 000078415 (2004).
Wyman, R. A., Mays, M. E., McBride, P. E. & Stein, J. H. Ultrasound-detected carotid plaque as a predictor of cardiovascular events. Vasc Med. 11, 123–130 (2006).
Schillaci, G. et al. Relationship between short-term blood pressure variability and large-artery stiffness in human hypertension: findings from 2 large databases. Hypertension. 60, 369–377, doi: 10.1161/hypertensionaha.112.197491 (2012).
Mancia, G. et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 31, 1281–1357, doi: 10.1097/01.hjh.0000431740.32696.cc (2013).
Head, G.A. et al. Ambulatory blood pressure monitoring. Aust Fam Physician. 40, 877-880 (2011).
Hermida, R. C., Smolensky, M. H., Ayala, D. E. & Portaluppi, F. Ambulatory Blood Pressure Monitoring (ABPM) as the reference standard for diagnosis of hypertension and assessment of vascular risk in adults. Chronobiol Int. 32, 1329–1342, doi: 10.3109/07420528.2015.1113804 (2015).
Montalescot, G. et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. EurHeart J. 34, 2949–3003, doi: 10.1093/eurheartj/eht296 (2013).
Acknowledgements
We acknowledge the cooperation from the patients who participated in our research. This research was sponsored by National Natural Science Foundation of China (No. 81300116), Research Fund of Young Scholars for the Doctoral Program of Higher Education of China (No. 20120201120083), the Fundamental Research Funds for the Central Universities (No. XJJ2013062) and the Scientific Fund for the Young talent of Shaanxi Province (2015KJXX-06).
Author information
Authors and Affiliations
Contributions
G.W. and B.Y. initialized the effort, B.Y., Q.G. and L.G. analyzed the data. B.Y., L.S. and Y.G. compiled the data and helped with the data interpretation. B.Y. and L.S. led the writing of the paper with substantial inputs and prepared figures and tables. G.W. and X.W. made significant contribution to the revision.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Yan, B., Sun, L., Gao, Y. et al. Blood pressure reverse dipping may associate with stable coronary artery disease in patients with essential hypertension: a cross-sectional study. Sci Rep 6, 25410 (2016). https://doi.org/10.1038/srep25410
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep25410
This article is cited by
-
Association between non-dipping blood pressure pattern and different glucometabolic profile during oral glucose tolerance test
Internal and Emergency Medicine (2024)
-
Higher Frequency of Nocturnal Blood Pressure Dipping but Not Heart Rate Dipping in Inflammatory Bowel Disease
Digestive Diseases and Sciences (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.