Abstract
Schizophrenia (SCZ) is a serious psychiatric disease with strong heritability. Its complexity is reflected by extensive genetic heterogeneity and much of the genetic liability remains unaccounted for. We applied a combined strategy involving detection of copy number variants (CNVs), whole-genome mapping and exome sequencing to identify the genetic basis of autosomal-dominant SCZ in a Chinese family. To rule out pathogenic CNVs, we first performed Illumina single nucleotide polymorphism (SNP) array analysis on samples from two patients and one psychiatrically healthy family member, but no pathogenic CNVs were detected. In order to further narrow down the susceptible region, we conducted genome-wide linkage analysis and mapped the disease locus to chromosome 7q21.13-22.3, with a maximum multipoint logarithm of odds score of 2.144. Whole-exome sequencing was then carried out with samples from three affected individuals and one unaffected individual in the family. A missense variation c.9575 C > G (p.Thr3192Ser) was identified in RELN, which is known as a risk gene for SCZ, located on chromosome 7q22, in the pedigree. This rare variant, as a highly penetrant risk variant, co-segregated with the phenotype. Our results provide genetic evidence that RELN may be one of pathogenic gene in SCZ.
Similar content being viewed by others
Introduction
Schizophrenia (SCZ [OMIM 181500]) is a severe psychiatric disease that begins in adolescence or early adulthood, characterized by positive symptoms (e.g. delusions, hallucinations and disorganized thinking), negative symptoms (e.g. flat affect, loss of spontaneity, diminished initiative and capacity for pleasure and impaired volition), numerous cognitive dysfunctions of varying severity and mood disturbances. The lifetime prevalence of SCZ is approximately 1% in the general population worldwide. Genetic causes play an important role in the pathogenesis of SCZ, which is strongly suggested by high heritability estimates (0.64 in a national family study1, 0.81 in a meta-analysis of twin studies2).
Pedigrees with multiple affected individuals serve as a valuable tool for discovery of rare and highly penetrant mutations which upon identification will shed light onto biological pathways involved in the pathogenesis of diseases. In pedigree studies, linkage analysis as traditional positional cloning method has been used to identify causal genes of several rare monogenic diseases. This method is also applicable to complex neuropsychiatric diseases, etc, Alzheimer’s disease3. Based on linkage analysis, St Clair et al.4 discovered a balanced translocation (1;11)(q42.1;q14.3) segregated with SCZ and related psychiatric disorders in a large and unique Scottish family4. As translocation directly disrupts the disrupted-in-schizophrenia 1 gene (DISC1), it is usually considered one of the candidate genes for susceptibility to psychiatric illnesses5. Apart from the 1q42 region, other suspected regions, including 1q21-22, 5q21-q33, 6p24-22, 6q21-25, 8p21-22, 10p15-p11, 13q32-34 and 22q11-12, have been reported to correlate with SCZ using linkage analysis6. With the application of high-throughput sequencing, a few studies have employed complementary approaches (e.g. linkage analysis, exome sequencing in pedigrees with multiple affected individuals) to identify private, highly penetrant mutations that co-segregate with psychiatric disease7,8,9. A deletion at the SLC1A1 glutamate transporter gene has been reported to co-segregate with schizophrenia and bipolar schizoaffective disorder in an extended five-generation family7. Most specifically, exome sequencing of multiplex pedigrees further supported the N-methyl-D-aspartate (NMDA) receptor hypofunction hypothesis of SCZ8. These studies have generated interesting data on contributions of rare genetic variations to psychiatric disease risk.
Because of the need for larger sample sizes to achieve sufficient statistical power to derive any disease association, recent genetic studies of SCZ have shifted away from family-based to population-based studies. Genetic risk for SCZ is conferred by common variants and rare variants. Genome-wide association studies (GWAS) based largely on common variants have identified over 100 schizophrenia risk loci, some of which are the most reproducible and reliable ones in the field of SCZ genetics10,11 (PGC is now known as the Psychiatric Genomics Consortium). But contribution of common variants toward schizophrenia risk has been modest. Compared with SCZ-associated common variants of small effect, rare variants with relatively high penetrance significantly increase risk of illness12,13,14,15,16,17. Very large number of rare variants, including copy number variants (CNVs)12,13,14,15 and single-nucleotide variants (SNVs)16,17, were involved in the etiology of SCZ. For example, CNVs finding from an enlarged case-control sample indicated that the strong functional links, between the major inhibitory GABAergic and excitatory glutamatergic systems, may be proposed to explain some of disease mechanisms18. In an analysis of exome sequencing data of 2,536 SCZ cases and 2,543 controls, Purcell et al.19. estimated that rare (less than 1 in 10,000), disruptive mutations account for a broadly comparable proportion of SCZ risk as do CNVs19. Although recent researches have considerably advanced our understanding of the genetic architecture of SCZ, the complete spectrum of SCZ susceptibility genes has not been completely discovered yet.
In the present study, we enrolled a large Chinese family with multiple affected subjects with SCZ in which its genetic transmission appeared most consistent with autosomal-dominant inheritance. Thus, we used a combined strategy to determine the genetic basis of SCZ in this family, involving CNV genome-wide microarray analysis, linkage analysis and exome sequencing.
Results
Clinical manifestation
The proband (III:4) was a 47-year-old male, diagnosed with SCZ at the age of 36 years (Fig. 1A). He was born after an uneventful, full-term pregnancy, with normal birth weight and did not exhibit motor or verbal delay. He exhibited extremely severe positive symptoms at 36 years of age, including formication, auditory hallucinations of threatening and commanding voices, persecutory delusions, self-talk and impulsive behavior. Treatment with sulpiride resulted in a significant improvement of his psychiatric symptoms, while discontinuation of sulpiride led to aggravation of symptoms. On examination at our facility, he showed moderate psychotic symptoms (auditory hallucinations and persecutory delusions) at the age of 42 years. Findings from general physical and neurological examinations were normal. On cognitive testing, the patient’s Minimum Mental State Examination (MMSE) score was 27 and Montreal Cognitive Assessment (MoCA) score was 20. Laboratory examinations were unremarkable. Magnetic resonance imaging (MRI) of the brain did not show gross structural abnormalities or significant atrophy in the hippocampus and frontal temporal lobe. The clinical features of the 6 affected patients included in this study are summarized in Table 1. The age of onset ranged from 31 to 39 years (mean 35 ± 3.0 years).
Linkage analysis mapped the schizophrenia (SCZ) family to a region on chromosome 7q21.13-22.3.
(A) A 3-generation Chinese family with autosomal-dominant SCZ is shown and haplotype analysis is indicated on chromosome 7 using partial single nucleotide polymorphism (SNP). Squares and circles indicate males and females, respectively. The black symbols represent the affected members and open symbols represent the unaffected individuals. The diagonal line indicates a deceased family member and the black arrow indicates the proband. Minus indicates the wild-type allele; plus indicates the heterozygous missense variant in RELN (c.9575 C > G). The family members enrolled in this study are marked with asterisks. Names of SNPs are given on the left. Haplotype alleles appear on one side. The black bar indicates the haplotype assumed to carry the disease allele. The bars with black and white haplotypes indicate a recombination event. (B) The diagram of chromosome 7 indicates the relative position of SCZ locus. The minimal linkage interval of SCZ is 15.072 cM, between rs758706 and rs1476878, on chromosome 7q21.13-22.3. The RELN position is indicated with a black arrow. (C) Multipoint logarithm of odds (LOD) scores for chromosome 7q are shown (frequency of 0.01 and 80% penetrance). SNPs locations are indicated by ticks at the top.
CNVs detection
We analyzed DNA from two subjects with SCZ and one 70-year-old psychiatrically healthy control using Human660W-Quad Chip. From the total of 1189 CNVs, only 46 CNVs were consistent with clinical phenotype. After comparison with the Database of Genomic Variants (DGV, http://projects.tcag.ca/variation/), all the 46 CNVs referred to common copy number polymorphisms. Furthermore, no previously reported pathogenic large rare CNVs were identified in the affected individuals (II:5 and III:1)18,20,21,22. Therefore, we concluded that rare CNVs were not responsible for schizophrenia in this family.
Linkage mapping
Genome-wide linkage mapping with SNP markers covering all chromosomes was undertaken to localize the mutation responsible for the disease. Parallel inspection of SNP data from the family identified a single shared region on chromosome 7q21.13-q22.3, flanked by SNP markers rs758706 and rs1476878, with a maximum multipoint LOD score of 2.144 (θ = 0.00) between rs234 and rs887882, when penetrance was assumed to be 0.8 (Fig. 1B,C, Supplementary Table 1). The highest probability haplotype in the family was reconstructed using best haplotype from the Merlin and Cyrillic programs and some key recombinant events were identified (Fig. 1A). All affected offspring of the patient (II:2) carried the same pathogenic haplotype. However, recombination was observed between rs887882 and rs1476878 in the unaffected posterity (III:5). Compared with the pathogenic haplotype of patient (II:5), recombination was ascertained between rs758706 and rs10234074 in the unaffected descendent (III:6) of this patient. Together with the results, it was suggested that in this family, the pathogenic gene was located at a region between rs758706 and rs1476878, which was co-segregated with the phenotype in all examined patients with SCZ. Therefore, the haplotype analyses traced SCZ to chromosome 7q21.13-q22.3, which was found to span a 15.072-cM region (Fig. 1B).
Exome sequencing and co-segregation analysis
Assuming that these three patients have the same genetic cause of disease reduced the number of variants to 6,106 common to all affected individuals. As the hereditary mode in the family is autosomal-dominant, the candidate variants were expected to be heterozygous in the three patients. To distinguish potentially pathogenic mutations from other variants, we focused only on functional variants (non-synonymous, nonsense, located in the canonical splice sites, or coding indels), anticipating that synonymous variants were far less likely to be pathogenic. On the basis of the genotypes of available public data-sets, additional polymorphisms were excluded, leaving 33 novel variants. Considering that most pathogenic variants either affected highly conserved sequences and/or were predicted to be deleterious, we used the ANNOVAR package, which contains 23 types of software to assess the remaining variants for a likely functional impact. As a result of the filtering steps above, the candidate pool was reduced to 19 variants (19 genes). To identify rare variants co-segregating with SCZ for the kindred, we have performed variant detection in all available members of the pedigree. The missense variant (c.9575C > G, p.Thr3192Ser) in RELN (chr7:103131145, RefSeq NM_005045/ NM_173054) was the only co-segregating mutation among these candidate variants tested by Sanger sequencing (Fig. 2A). The variant status of all tested individuals was depicted in Fig. 1A. Additionally, this variant was not found in the NHLBI Exome Sequencing Project (ESP6500), the 1000 Genomes Project and the Single Nucleotide Polymorphism Database (dbSNP137), while the allele frequency of this variant was 8.24 × 10−6 in the ExAC database. Moreover, the missense substitute was also not detected in the 500 unaffected control individuals, indicating the rarity of the variation in the same geographic population. Thr3192 was found at a highly conserved position, indicating an important role for this residue. (Fig. 2B). Apart from these, the mutation we identified using exome sequencing is located in the same chromosomal region (7q21.13-q22.3) as that identified by linkage analysis, which cross-validated RELN as the potentially causative SCZ gene in this family (Fig. 1B).
Heterozygous missense mutation of RELN in SCZ family and genomic organization of the human RELN.
(A) Sequence analysis of exon 59 of RELN in a normal control and the affected proband of this family is shown. The DNA sequence chromatogram shows a heterozygous C > G nucleotide change (black arrow) in exon 59 of RELN (c.9575C > G), which leads to the replacement of threonine (ACC) with serine (AGC) at codon 3192 (p.Thr3192Ser). (B) Protein sequence alignment of RELN orthologs shows the region surrounding the mutated T3192S. Homo = Homo sapiens; Mus = Mus musculus; Rattus = Rattus norvegicus; Pan = Pan troglodytes; Macaca = Macaca mulatta; Canis = Canis lupus; Bos = Bos taurus; Gallus = Gallus domesticu.
Discussion
In the Chinese family with autosomal-dominant SCZ, we identified a rare SCZ-related genetic variation (c.9575 C > G, p.Thr3192Ser) in RELN gene. It was detected using complementary genome-wide screening methods, validated by Sanger sequencing and rarely found in large sequencing databases of controls. To our knowledge, rare variations of RELN gene have not been detected in familial SCZ. Here, we conducted CNV study, linkage analysis and whole genome sequencing to confirm that the rare highly penetrant variation in RELN gene predisposed to SCZ in a Han Chinese pedigree. Similar to Timms et al. study8, we also didn’t discover any pathogenic CNV. Timms et al. provided one possible explanation that large rare CNVs confer risk for a more severe form of the disease (childhood onset or with associated comorbid intellectual disability), limiting reproductive fitness and subsequent familial transmission. Linkage analysis traced SCZ to chromosome 7q21.13-q22.3, which showed considerable overlap with the region reported by Ekelund et al. in Finnish SCZ patients23. Replication in independent studies demonstrates that the region 7q22 may contain a SCZ susceptibility gene, wherein, interestingly, RELN is located. Subsequently, the missense substitution of RELN was also identified via exome sequencing, further providing two separate experimental methods for localizing the gene of interest.
For sporadic SCZ, previous studies reported the contribution of rare variants and common variants to SCZ. Several exome sequencing studies in large SCZ cohorts already addressed the role of RELN rare variation in SCZ. For example, a rare missense variant (chr7:103194134 T > C, p.Tyr1981Cys) was detected in Bulgarian trio de novo exome sequencing SCZ sample24; some rare non-synonymous and disruptive mutations of RELN gene were found in Swedish SCZ patients19 (See Schizophrenia Exome Sequencing Genebook). On the other hand, common variants in RELN gene were also associated with SCZ. Firstly, SNP (rs2229860) has been described as a risk allele in relation to SCZ in a meta-analysis across three independent Caucasian case-control cohorts25. In addition, Shifman et al. reported a SNP (rs7341475) in RELN, which showed female-specific association with SCZ in Ashkenazi Jews26. This group also successfully replicated the association in a sample from the United Kingdom. Recently, rs7341475 was described as associated with the risk of paranoid SCZ27. Another common variant (rs362719) of RELN was also identified to be associated with SCZ in female Han Chinese28, but the results of association studies between RELN and SCZ were not exactly replicable in different populations. The reported association of rs7341475 in Ashkenazi Jews is not significant in Han Chinese29. These studies have illustrated that RELN is a convincing vulnerability factor for sporadic SCZ25,26,27,28,29,30,31.
RELN, located at 7q22 in humans32, is a strong susceptibility gene in diverse psychiatric diseases including SCZ, major depression, bipolar disorder and autism33,34. RELN codes for reelin, which is a prominent component of the extracellular matrix and serves different functions during brain development and adulthood. During embryonic development, reelin is crucial for accurate cytoarchitecture of laminated structures35,36, demonstrated by reports of mutations in the RELN gene being associated with lissencephaly with cerebellar hypoplasia (LIS-CH)37. At postnatal and adult stages, reelin contributes to synapse formation38,39 and acts as a modulator of synaptic transmission and synaptic plasticity40,41,42. It is notable that in the postnatal brain, reelin is required for maintaining the mature subunit composition of N-methyl-D-aspartate receptors (NMDARs)43,44,45. Reelin binding to its receptors (very low-density lipoprotein receptor [VLDLR], apolipoprotein E receptor 2 [APOER2] and potentially a3b1 integrin) results in phosphorylation of NMDAR subunits, NR2A and NR2B. This process is mediated by the cytoplasmic adaptor protein Disabled-1 (DAB1) and Src-tyrosine kinase family/Fyn-kinase (SRC/FYN) activation46. Increasingly compelling reports suggest that synaptic dysfunction, particularly related to NMDAR signaling, is part of SCZ pathophysiology10,11,12,13,14,15,16,17,18,19,20,21,22,23,24. In addition, reelin is highly expressed in the normal human brain. However, a series of postmortem studies have demonstrated reductions in reelin protein levels at multiple brain sites (layers I and II of the prefrontal cortex, interstitial white matter neurons of the superior temporal cortex, hippocampus and cerebellum) of subjects with SCZ when compared with controls33,47,48,49,50,51. Finally, animal models showing reelin deficit provide further evidence for symptoms of SCZ. Knockdown of reelin in the medial prefrontal cortex (mPFC) of Wistar rats during puberty or adulthood results in abnormal behavioral tasks with relevance to SCZ52. In a mouse model of prenatal restraint stress (PRS), offspring indicated a SCZ-like phenotype in behavior and displayed reduced expression of reelin in early life as well as adulthood, with increased DNA methyltransferase (DNMT) expression53. Teixeira et al. showed that a transgenic mouse model of reelin overexpression displayed resistance to developing psychiatric disorders such as SCZ, mood and anxiety disorders, which indicated that reelin might have a protective role in these conditions54.
This study had certain limitations. To confirm statistical evidence for the observed variation, large case-control studies will be required to estimate its frequency and odds ratios (OR). Moreover, our study lacked functional evidences supporting the effects of the discovered variant. Furthermore, additional unrelated autosomal-dominant SCZ pedigrees were needed to evaluate whether other rare variants in RELN are responsible for familial SCZ.
Taken together, we identified a rare, missense mutation (c.9575 C > G, p.Thr3192Ser) within the RELN gene which might confer risk for SCZ in a Han Chinese pedigree. Our result provides genetic evidence that RELN can be implicated in the pathogenesis of SCZ.
Subjects and methods
Subjects
A total of three generations of a Chinese Han family with autosomal-dominant SCZ were enrolled in this study (Fig. 1A). The pedigree included 12 members, including 6 patients with SCZ. All affected individuals were diagnosed independently by at least two well-experienced psychiatrists according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria (DSM-IV). Alternative conditions such as head injuries, substance-induced psychotic disorders, alcoholic psychosis and other symptomatic psychoses have been excluded. Clinical data was collected by interviews and clinical questionnaires. A total of 500 unaffected individuals (mean age 30.0 ± 10.28 years) from the same geographic region as the schizophrenic patients, were recruited as normal controls. The study was approved by the Ethics Committee of Xiangya Hospital of the Central South University in China (equivalent to an Institutional Review Board) and carried out in accordance with the approved guidelines. A written informed consent was obtained from each subject. Genomic DNA was extracted from peripheral blood leukocytes using a standard salt precipitation protocol.
CNV detection
To identify possible pathogenic CNVs, we examined genomic DNA samples from two affected individuals (II:5 and III:1) and one unaffected individual (II:3) in the family (Fig. 1A). The Human660W-Quad Chip (Illumina Inc., San Diego, USA) and the Illumina BeadScan genotyping system (Beadstation Scanner) were employed to obtain the signal intensities of single nucleotide polymorphism (SNP) probes following the manufacturer instructions. Genome Studio genotyping module software (Illumina) was used to analyze the genotypes (human genome build 37/Hg19) and evaluate experimental quality. The call rates of the samples were greater than 99.0%.
Genome-wide genotyping for linkage analysis
To localize rare disease-related gene, we carried out whole-genome genotyping in the family using the Infinium HumanLinkage-12 Genotyping BeadChip (Illumina Inc., San Diego, USA). The BeadChip included 6090 SNP markers with an average gap of 441 kb and 0.58 cM across the genome. The genotype assignments were determined with Genome Studio genotyping module software (Illumina). Relative positions were derived from the human genome draft sequence and the Marshfield map (www.ncbi.nlm.nih.gov). Multipoint linkage analysis and reconstruction of the most likely haplotypes were performed using the linkage program, Merlin. The allele frequencies of markers, as well as the recombination fractions in males and females, were assumed to be equal. The disease was modeled as an autosomal-dominant trait with a disease allele frequency equal to 0.01. For calculating the logarithm of odds (LOD) scores, the disease penetrance was assumed to be 80%55 (Supplementary Table 1).
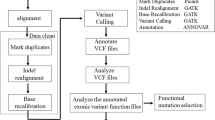
Whole-exome sequencing and mutation sequencing
To identify the pathogenic mutation causing SCZ in this Chinese kindred, we performed exome sequencing analysis in three affected individuals (II:5, III:2, III:4) and one unaffected family member (III:5) (Fig. 1A). NimbleGen Sequence Capture Arrays were used to isolate the genomic coding regions to be sequenced. For enrichment, paired-end libraries were hybridized with the NimbleGen SeqCap EZ v2.0, which contains 2.1 million probes that capture a total of 44.1 Mb regions. Sequencing was subsequently performed using a HiSeq 2000 platform with 90-bp, paired-end reads. The mean coverage per targeted base was 70.10-fold. R20-fold coverage of bases was 89.2% for II:5, 92.1% for III:2, 90.1% for III:4 and 92.5% for III:5, respectively. The coverage of target region was 98.9%, 98.8%, 98.9% and 99.1%, respectively. Clean data were obtained by removing adaptor and low quality reads, followed by aligning to the human genome reference assembly (USCS hg19) using Burrows-Wheeler Aligner (BWA). We performed data preprocessing involving removal of polymerase chain reaction (PCR) duplications using Picards, followed by indel realignment and base quality score recalibration by GATK. Haplotypecaller and variant quality score recalibration were adopted to identify the variants and recalculate their quality scores. This analysis identified a total of 29,964, 34,257, 35,754 and 34,746 variants, respectively, for II:5, III:2, III:4 and III:5. All variants were annotated with variants alleles frequency (VAF) in the NHLBI Exome Sequencing Project (ESP6500), the 1000 Genomes Project and the Single Nucleotide Polymorphism Database (dbSNP137). Possible pathogenic variants were confirmed by Sanger sequencing using ABI 3730 DNA sequencer (PE Applied Biosystems), following the manufacturer protocol. Sequencing data was analyzed by DNA Star software (DNASTAR, Inc. Madison, Wisconsin, USA).
Additional Information
How to cite this article: Zhou, Z. et al. Identification of RELN variation p.Thr3192Ser in a Chinese family with schizophrenia. Sci. Rep. 6, 24327; doi: 10.1038/srep24327 (2016).
References
Lichtenstein, P. et al. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 373, 234–9 (2009).
Sullivan, P. F., Kendler, K. S. & Neale, M. C. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 60, 1187–92 (2003).
Sherrington, R. et al. Cloning of a gene bearing missense mutations in early-onset familial Alzheimer’s disease. Nature 375, 754–60 (1995).
St Clair, D. et al. Association within a family of a balanced autosomal translocation with major mental illness. Lancet 336, 13–6 (1990).
Millar, J. K. et al. Disruption of two novel genes by a translocation co-segregating with schizophrenia. Hum Mol Genet 9, 1415–23 (2000).
O’Donovan, M. C., Williams, N. M. & Owen, M. J. Recent advances in the genetics of schizophrenia. Hum Mol Genet 12 Spec No 2, R125–33 (2003).
Myles-Worsley, M. et al. Deletion at the SLC1A1 glutamate transporter gene co-segregates with schizophrenia and bipolar schizoaffective disorder in a 5-generation family. Am J Med Genet B Neuropsychiatr Genet 162B, 87–95 (2013).
Timms, A. E. et al. Support for the N-methyl-D-aspartate receptor hypofunction hypothesis of schizophrenia from exome sequencing in multiplex families. JAMA Psychiatry 70, 582–90 (2013).
Collins, A. The genomic and functional characteristics of disease genes. Brief Bioinform 16, 16–23 (2015).
PGC. Biological insights from 108 schizophrenia-associated genetic loci. Nature 511, 421–7 (2014).
PGC.Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nat Neurosci 18, 199–209 (2015).
The International Schizophrenia Consortium, Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature 455, 237–41 (2008).
Walsh, T. et al. Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science 320, 539–43 (2008).
Xu, B. et al. Strong association of de novo copy number mutations with sporadic schizophrenia. Nat Genet 40, 880–5 (2008).
Kirov, G. et al. De novo CNV analysis implicates specific abnormalities of postsynaptic signalling complexes in the pathogenesis of schizophrenia. Mol Psychiatry 17, 142–53 (2012).
Xu, B. et al. Exome sequencing supports a de novo mutational paradigm for schizophrenia. Nat Genet 43, 864–8 (2011).
Girard, S. L. et al. Increased exonic de novo mutation rate in individuals with schizophrenia. Nat Genet 43, 860–3 (2011).
Pocklington, A. J. et al. Novel Findings from CNVs Implicate Inhibitory and Excitatory Signaling Complexes in Schizophrenia. Neuron 86, 1203–14 (2015).
Purcell, S. M. et al. A polygenic burden of rare disruptive mutations in schizophrenia. Nature 506, 185–90 (2014).
Malhotra, D. & Sebat, J. CNVs: harbingers of a rare variant revolution in psychiatric genetics. Cell 148, 1223–41 (2012).
Rees, E. et al. Analysis of copy number variations at 15 schizophrenia-associated loci. Br J Psychiatry 204, 108–14 (2014).
Szatkiewicz, J. P. et al. Copy number variation in schizophrenia in Sweden. Mol Psychiatry 19, 762–73 (2014).
Ekelund, J. et al. Genome-wide scan for schizophrenia in the Finnish population: evidence for a locus on chromosome 7q22. Hum Mol Genet 9, 1049–57 (2000).
Fromer, M. et al. De novo mutations in schizophrenia implicate synaptic networks. Nature 506, 179–84 (2014).
van Schijndel, J. E. et al. Three-cohort targeted gene screening reveals a non-synonymous TRKA polymorphism associated with schizophrenia. J Psychiatr Res 43, 1195–9 (2009).
Shifman, S. et al. Genome-wide association identifies a common variant in the reelin gene that increases the risk of schizophrenia only in women. PLoS Genet 4, e28 (2008).
Galaktionova, D., Gareeva, A. E., Khusnutdinova, E. K. & Nasedkina, T. V. [The association of polymorphisms in SLC18A1, TPH1 and RELN genes with risk of paranoid schizophrenia]. Mol Biol (Mosk) 48, 629–39 (2014).
Kuang, W. J., Sun, R. F., Zhu, Y. S. & Li, S. B. A new single-nucleotide mutation (rs362719) of the reelin (RELN) gene associated with schizophrenia in female Chinese Han. Genet Mol Res 10, 1650–8 (2011).
Li, M. et al. Analysis of common genetic variants identifies RELN as a risk gene for schizophrenia in Chinese population. World J Biol Psychiatry 14, 91–9 (2013).
Pisante, A., Bronstein, M., Yakir, B. & Darvasi, A. A variant in the reelin gene increases the risk of schizophrenia and schizoaffective disorder but not bipolar disorder. Psychiatr Genet 19, 212 (2009).
Hall, H. et al. Potential genetic variants in schizophrenia: a Bayesian analysis. World J Biol Psychiatry 8, 12–22 (2007).
DeSilva, U. et al. The human reelin gene: isolation, sequencing and mapping on chromosome 7. Genome Res 7, 157–64 (1997).
Fatemi, S. H., Earle, J. A. & McMenomy, T. Reduction in Reelin immunoreactivity in hippocampus of subjects with schizophrenia, bipolar disorder and major depression. Mol Psychiatry 5, 654–63 571 (2000).
Iafrati, J. et al. Reelin, an extracellular matrix protein linked to early onset psychiatric diseases, drives postnatal development of the prefrontal cortex via GluN2B-NMDARs and the mTOR pathway. Mol Psychiatry 19, 417–26 (2014).
Ogawa, M. et al. The reeler gene-associated antigen on Cajal-Retzius neurons is a crucial molecule for laminar organization of cortical neurons. Neuron 14, 899–912 (1995).
Tissir, F. & Goffinet, A. M. Reelin and brain development. Nat Rev Neurosci 4, 496–505 (2003).
Hong, S. E. et al. Autosomal recessive lissencephaly with cerebellar hypoplasia is associated with human RELN mutations. Nat Genet 26, 93–6 (2000).
Niu, S., Renfro, A., Quattrocchi, C. C., Sheldon, M. & D’Arcangelo, G. Reelin promotes hippocampal dendrite development through the VLDLR/ApoER2-Dab1 pathway. Neuron 41, 71–84 (2004).
Niu, S., Yabut, O. & D’Arcangelo, G. The Reelin signaling pathway promotes dendritic spine development in hippocampal neurons. J Neurosci 28, 10339–48 (2008).
Beffert, U. et al. Modulation of synaptic plasticity and memory by Reelin involves differential splicing of the lipoprotein receptor Apoer2. Neuron 47, 567–79 (2005).
Weeber, E. J. et al. Reelin and ApoE receptors cooperate to enhance hippocampal synaptic plasticity and learning. J Biol Chem 277, 39944–52 (2002).
Qiu, S., Zhao, L. F., Korwek, K. M. & Weeber, E. J. Differential reelin-induced enhancement of NMDA and AMPA receptor activity in the adult hippocampus. J Neurosci 26, 12943–55 (2006).
Ventruti, A., Kazdoba, T. M., Niu, S. & D’Arcangelo, G. Reelin deficiency causes specific defects in the molecular composition of the synapses in the adult brain. Neuroscience 189, 32–42 (2011).
Groc, L. et al. NMDA receptor surface trafficking and synaptic subunit composition are developmentally regulated by the extracellular matrix protein Reelin. J Neurosci 27, 10165–75 (2007).
Sinagra, M. et al. Reelin, very-low-density lipoprotein receptor and apolipoprotein E receptor 2 control somatic NMDA receptor composition during hippocampal maturation in vitro. J Neurosci 25, 6127–36 (2005).
Chen, Y. et al. Reelin modulates NMDA receptor activity in cortical neurons. J Neurosci 25, 8209–16 (2005).
Impagnatiello, F. et al. A decrease of reelin expression as a putative vulnerability factor in schizophrenia. Proc Natl Acad Sci USA 95, 15718–23 (1998).
Eastwood, S. L. & Harrison, P. J. Cellular basis of reduced cortical reelin expression in schizophrenia. Am J Psychiatry 163, 540–2 (2006).
Guidotti, A. et al. Decrease in reelin and glutamic acid decarboxylase67 (GAD67) expression in schizophrenia and bipolar disorder: a postmortem brain study. Arch Gen Psychiatry 57, 1061–9 (2000).
Eastwood, S. L. & Harrison, P. J. Interstitial white matter neurons express less reelin and are abnormally distributed in schizophrenia: towards an integration of molecular and morphologic aspects of the neurodevelopmental hypothesis. Mol Psychiatry 8 769, 821–31 (2003).
Fatemi, S. H., Stary, J. M., Earle, J. A., Araghi-Niknam, M. & Eagan, E. GABAergic dysfunction in schizophrenia and mood disorders as reflected by decreased levels of glutamic acid decarboxylase 65 and 67 kDa and Reelin proteins in cerebellum. Schizophr Res 72, 109–22 (2005).
Brosda, J., Dietz, F. & Koch, M. Impairment of cognitive performance after reelin knockdown in the medial prefrontal cortex of pubertal or adult rats. Neurobiol Dis 44, 239–47 (2011).
Matrisciano, F. et al. Epigenetic modifications of GABAergic interneurons are associated with the schizophrenia-like phenotype induced by prenatal stress in mice. Neuropharmacology 68, 184–94 (2013).
Teixeira, C. M. et al. Overexpression of Reelin prevents the manifestation of behavioral phenotypes related to schizophrenia and bipolar disorder. Neuropsychopharmacology 36, 2395–405 (2011).
Coon, H. et al. Use of a neurophysiological trait in linkage analysis of schizophrenia. Biol Psychiatry 34, 277–89 (1993).
Acknowledgements
We are grateful to all subjects for participation in our study. This study was supported by the National Basic Research Program (973 Program) (No. 2011CB707800, awarded to Lu Shen), the National Natural Science Foundation of China (No. 81171068 and No. 81471295, awarded to Lu Shen) and the Natural Science Foundation of Hunan Provincial (No. 14JJ7011, awarded to Lin Zhou).
Author information
Authors and Affiliations
Contributions
Z.Z., Zhengmao Hu and L.S. designed the study. Z.Z., Zhengmao Hu, L.Z., Zhaoting Hu, H.L., Z.L. and J.D. conducted the experiments, analyzed and interpreted the data. Z.Z. and L.S. wrote the manuscript. J.Z., L.Z., K.X., B.T. and L.S. supervised the study. L.Z. and L.S. provided financial support.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhou, Z., Hu, Z., Zhang, L. et al. Identification of RELN variation p.Thr3192Ser in a Chinese family with schizophrenia. Sci Rep 6, 24327 (2016). https://doi.org/10.1038/srep24327
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep24327
This article is cited by
-
Association Between REELIN Gene Polymorphisms (rs7341475 and rs262355) and Risk of Schizophrenia: an Updated Meta-analysis
Journal of Molecular Neuroscience (2021)
-
Exploring the mRNA expression level of RELN in peripheral blood of schizophrenia patients before and after antipsychotic treatment
Hereditas (2020)
-
Single-cell trajectory analysis of human homogenous neurons carrying a rare RELN variant
Translational Psychiatry (2018)
-
Genetic and animal model analyses reveal the pathogenic role of a novel deletion of RELN in schizophrenia
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.