Abstract
The colorectal carcinogenesis is a complex process encompassing genetic alterations. The oncoprotein AEG-1, encoded by the MTDH gene, was shown previously to be involved in colorectal cancer (CRC). The aim of this study was to determine the frequency and the spectrum of MTDH variants in tumor tissue, and their relationship to clinicopathological variables in CRC patients. The study included tumors from 356 unselected CRC patients. Mutation analysis of the MTDH gene, including coding region and adjacent intronic sequences, was performed by direct DNA sequencing. The corresponding normal colorectal tissue was analyzed in the carriers of exonic variant to confirm germline or somatic origin. We detected 42 intronic variants, where 25 were novel. Furthermore, we found 8 exonic variants of which four, one missense (c.977C > G-germline) and three frameshift mutations (c.533delA-somatic, c.1340dupA-unknown origin, c.1731delA-unknown origin), were novel. In silico prediction analyses suggested four deleterious variants (c.232G > T, c.533delA, c.1340dupA, and c.1731delA). There were no correlations between the MTDH variants and tumor stage, differentiation or patient survival. We described several novel exonic and intronic variants of the MTDH gene. The detection of likely pathogenic truncating mutations and alterations in functional protein domains indicate their clinical significance, although none of the variants had prognostic potential.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third most common cancer in men and the second in women with 1.36 million incidences per year worldwide. About 700,000 estimated deaths per year caused by CRC making it the fourth most common cause of cancer death, accounting for about 8.5% worldwide1. Around 75% of the CRC incidences are sporadic, and the rest of the cases are hereditary or familial CRC, associated with inherited genetic aberrations2. As first proposed by Fearon and Vogelstein in 1990, colorectal carcinogenesis is a complex process implicating accumulation of genetic alterations in oncogenes and tumor suppressor genes3. Several oncogenic aberrations including point mutations, insertions, deletions and gene amplification in KRAS, NRAS, BRAF, MYC, WNT and PIK3CA have been linked to colorectal carcinogenesis and are therefore promising genetic markers for early cancer detection, treatment selection and prognosis3,4,5.
Current research is devoted to search for new prognostic and predictive biomarkers. The Metadherin gene (MTDH; MIM#610323) encodes for the lysine-rich oncoprotein Astrocyte elevated gene 1 (AEG-1), also called LYRIC, which is highly basic 582 amino acid protein with a molecular mass of 64 kDa6,7. The gene is located at chromosome 8q22 and comprises 12 (coding) exons and spans around 95 kb (PMID: 14980505)8. Amplification of genomic loci 8q22 has been correlated to increased AEG-1 expression9,10,11,12,13. Several functional regions in the AEG-1 protein have been discovered. The AEG-1 protein contains an N-terminal transmembrane domain (amino acid (aa)51–72), three putative nuclear localization signals (aa79–91, aa432–451 and aa561–580) and several protein interaction sites14.
We and others have shown that the AEG-1 mRNA and protein are overexpressed in CRC and other types of cancer compared with the corresponding non-tumor tissue15,16,17,18,19. The AEG-1 protein has been found to be involved in cell proliferation, survival, migration, invasion, apoptosis, angiogenesis, metastasis and treatment resistance when interacting with a variety of proteins and protein complexes11,13,17,20,21,22,23. Two studies conducted on blood samples from breast and ovarian cancer patients have analyzed the coding sequence of MTDH, and identified a correlation between the polymorphisms c.1353G > A (rs2331652, p.K451K), and c.1679–6 T > C (rs117026063), and breast cancer susceptibility as well as between the polymorphism −470 G > A and ovarian cancer susceptibility20,24.
However, it is unknown whether mutations in the MTDH gene contribute to tumor progression and have prognostic potential for CRC. The aim of this study was to determine the frequency and the spectrum of MTDH variants in tumor tissue and their relationship to clinicopathological variables (patient gender, age at diagnosis, tumor location, tumor stage, grade of differentiation, recurrence and survival) of CRC patients. To our knowledge, this is the first study analyzing mutations of MTDH in tumor tissue.
Results
Frequency of MTDH variants in CRC patients and cell lines
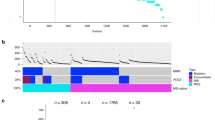
By direct DNA sequencing of the complete coding sequence of the MTDH gene, we found 50 single nucleotide variants in 356 CRC patient samples (Supplementary Table 1). Eight of the variants were exonic and 42 were in a non-coding region adjacent to an exon. Among them, there were four novel exonic variants (Table 1, Fig. 1) [c.533delA (p.N178Tfs34), c.977C > G (p.T326S), c.1340dupA (p.K447Efs7) and c.1731delA (p.A578Profs29)], and 25 novel variants in a non-coding region adjacent to exons. All variants found were heterozygous, except for the seven variants c.232G > T, c.382–50C > T, c.568 + 213delT, c.949A > G, c.1048 + 131T > G, c.1049–97delA and c.1147 + 28delT. The genotypic frequency is stated in Supplementary Table 1. There was no MTDH variant in the colon cancer cell lines SW480, SW620 and HCT116 (data not shown).
Several variants co-occurred and two clusters were identified (Supplementary Table 2 and 3). The first cluster of variants with a high linkage included the variants c.160G > A (rs140652237, p.V54M), c.568 + 213delT (rs34735761) and c.1353G > A (rs2331652, p.K451K), and showed a significant correlation to each other (p < 0.05). The second cluster of variants with a high linkage included c.232G > T (rs17854373, p.A78S), c.382–50C > T (rs16896067), c.949A > G (rs17854374, p.T317A), c.1048 + 131T > G (rs12675731), c.1049–97delA (rs150495888), and c.1147 + 28delT (rs76537339; p < 0.05). Each variant of both clusters was also detected in the corresponding normal mucosa, which corresponded with their germline origin.
Intronic MTDH variants in relation to clinicopathological variables
The intronic variants c.382–50C > T (rs16896067), c.1048 + 131T > G (rs12675731) and c.1353G > A (rs2331652, p.K451K) were more frequent in the patients <72 years old compared to the age group ≥72 years old (p = 0.019, p = 0.047 and p = 0.021, respectively; Supplementary Table 4). The variant c.1048 + 82 delA (rs149869061) was only detected in tumors located in the colon but not those located in the rectum (p = 0.013). We did not find any relationship between the variants and the gender, tumor stage, grade of differentiation, recurrence and patient survival (p > 0.05).
Exonic variants in relation to clinicopathological variables and location in functional protein domains
Among the 8 exonic variants detected in this study, four were missense [c.160G > A (rs140652237, p.V54M), c.232G > T (rs17854373, p.A78S), c.949A > G (rs17854374, p.T317A) and c.977C > G, (p.T326S)], one silent [c.1353G > A (rs23316529, p.K451K)], and three frame shift mutations [c.533delA (p.N178Tfs34), c.1340dupA (p.K448Efs7), and c.1731delA (p.A578Pfs29)]. To evaluate whether the exonic variants occurred during colorectal carcinogenesis or whether they are inherited, we analyzed the corresponding normal mucosa of the colon and rectum from the same patients. Frame-shift mutation c.533delA was not detected in the corresponding normal mucosa, and therefore considered as a somatic mutation. The corresponding normal mucosa for the other two frameshift variants was not available, therefore we were not able to assess the somatic or germline status. The other exonic variants were detected also in the corresponding normal mucosa (Table 1). The variant c.232G > T (rs17854373, p.A78S) was more frequent in the patients <72 years old compared to the age group ≥72 years old (p = 0.001; Supplementary Table 4). To evaluate the predicted effects of exonic variants on protein function, six in silico prediction tools were used. The in silico prediction analyses revealed that four of these variants c.232G > T (rs17854373, p.A78S), c.533delA, c.1340dupA and c.1731delA, were deleterious (Table 1, Fig. 1, Supplementary Table 5). The variants, c.533delA, and c.1340dupA, lead to a truncation of the protein while the variant, c.1731delA, is predicted to lead to protein prolongation. All three variants were heterozygotic and detected in stage I or II colon cancer with moderate or poor differentiation (Table 2).
We discovered two variants which are located in at least one functional region of the AEG-1 protein. The variant c.160G > A (rs140652237, p.V54M), is located in the transmembrane domain and in the CBP and PLZF binding region. The variant, c.232G > T (rs17854373, p.A78S) is located one amino acid before the N-terminal nuclear localization signal and in the YY1, BCCIP and PLZF binding region. The missense variants, c.949A > G (rs17854374, p.T317A) and c.977C > G (p.T326S), are in an area without known protein interaction.
Discussion
Overexpression of the oncogene AEG-1 has been reported in several types of cancers and was correlated to increased cell proliferation, invasion, survival and treatment resistance11,13,17,20,21,22,23. Numerous studies have shown that overexpression of AEG-1 is due to amplification of the genomic loci at chromosome 8q22, activation of up-stream signaling as well as deregulation of several miRNAs9,10,11,12,13,25,26,27,28,29,30,31,32. However, it remains largely unclear whether mutations in the MTDH gene contribute to its oncogenic properties. In the present study, we therefore examined the frequency and spectrum of MTDH variants, and their relationship to clinicopathological variables in 356 CRC patients including tumor tissue as well as in three colon cancer cell lines. In total, we detected 42 intronic variants, whereof 25 were novel. Furthermore, we found eight exonic variants of which four variants, one missense (c.977C > G) and three frameshift mutations (c.533delA, c.1731delA, c.1340dupA), were novel. The three frameshift variants are likely pathogenic.
Correlation analyses between recurrent variants and clinicopathological variables revealed that the intronic variant, c.1048 + 82 delA (rs149869061), was only detected in tumors located in the colon but not those located in the rectum. In a previous study, we found significantly lower expression of the AEG-1 mRNA in the colon compared to the rectum16. Whether the intronic variant has an influence on the mRNA expression or stability needs further investigation.
The variants, c.232G > T (rs17854373, p.A78S), c.382–50C > T (rs16896067), c.1048 + 131T > G (rs12675731) and c.1353G > A (rs2331652, p.K451K), were found to be more frequent in the patients <72 years old than those ≥72 years old. However, these variants are hereditary and their impact of the early onset is questionable.
The variants c.1353G > A (rs2331652) and c.1679–6T > C (rs117026063) were both frequently detected in blood samples from breast cancer patients (52% and 22%, respectively) and from healthy controls (36% and 11%, respectively), and both variants have been correlated to breast cancer susceptibility in a Chinese study24. Compared to their results, in the present study the variants, c.1353G > A (rs2331652) and c.1679–6T > C (rs117026063), were very rare (2.5% and 0.3%, respectively). The different frequencies in the two studies could be due to the divergence between the ethnical groups (Chinese versus Caucasian), DNA origins and disease mechanisms etc. However, there were no correlations between these two variants and clinicopathological variables, neither in breast cancer24 nor in our study.
Several detected exonic variants in this study are located in a functional- or protein binding region of the AEG-1 protein. Even though the three-dimensional structure of AEG-1 is not completely solved, a transmembrane domain, three putative nuclear localization signals as well as several protein interaction regions have been identified7,33. Variant, c.160G > A (rs140652237, p.V54M), is located in the transmembrane domain which spans the aa51–72 as well as in the CBP and PLZF binding region. Two programs, Polyphen-2 and MUpro, predict this mutation as possibly damaging or lowering stability of the AEG-1 protein. Another variant, c.232G > T (rs17854373, p.A78S), is located one amino acid before the N-terminal nuclear localization signal (aa79–91) and in the YY1, BCCIP and PLZF binding region. Previously, it has been shown that the extended nuclear localization region between aa78–130 regulates the nucleolar localization of AEG-133. Three programs, Mutation Taster, Polyphen-2 and MUpro, predict this mutation to be possibly disease causing or damaging or reducing the protein stability. However, whether these two missense variants have an impact on the protein function has to be experimentally validated.
In conclusion, this is the first study analyzing MTDH mutations in tumor tissue. We found 29 novel MTDH variants. The three frameshift variants detected in tumor tissue are likely pathogenic, and the other variants detected in functional protein regions suggest their role in CRC tumorigenesis, although none of the variants had prognostic potential. These results suggest that genetic variants of MTDH are probably not of high clinical importance in CRC, even though our sample set is relatively small in order to show significance of rare variants.
Material and Methods
Patients
This study included primary CRC tissue and distant normal mucosa from 356 CRC patients diagnosed at the University Hospital in Linköping and Vrinnevi Hospital in Norrköping. Tissues were collected during primary surgery between 1989 and 2004. Samples from the corresponding normal tissue of the colon or rectum were taken at least 10 cm from the tumor margins. Representative tumor tissues, evaluated by pathologist, were stored for subsequent analyses at −70 °C. Characteristics of the patients are shown in Table 3. The mean age at diagnosis was 72 years. The tumors with better differentiation included well and moderately differentiated tumors, and worse differentiation included poorly differentiated, mucinous or signet-ring cells carcinomas. Information was lacking about tumor differentiation in four patients and recurrence in 169 patients. The study was approved by the Regional Ethical Review Board in Linköping and an informed consent document was signed by participants. The methods were carried out according to the approved ethical guidelines.
Cell culture
The SW480 and SW620 cell lines were obtained from American Type Culture Collection.
The cell lines were maintained at 37 °C and 5% CO2 in Eagles MEM (Sigma-Aldrich, St. Louis, MO), supplemented with 10% heat inactivated fetal bovine serum albumin (GIBCO, Invitrogen, Paisley, UK) and 1% L-glutamin (GIBCO). The HCT116 cell line was obtained from the Core cell center (Johns Hopkins University, Baltimore, MD) and was maintained in McCoy’s 5A medium (Sigma-Aldrich) supplemented with 10% heat inactivated fetal bovine serum albumin (GIBCO) at 37 °C and 5% CO2. Cells growing exponentially were harvested when 80% confluence was achieved. All cells were tested for Mycoplasma by using a commercially available PCR kit (PromoKine, Heidelberg, Germany). The morphology and growth rate of all cell lines were controlled during the whole experimental period.
Isolation of DNA and mutation analysis
DNA was isolated from fresh frozen tissue and lysate from cell lines using standard procedures implementing DNeasy Blood & Tissue Kit (Qiagen, Hilden, Germany). The coding region of the MTDH gene was analyzed by using PCR and direct DNA Sanger sequencing in 356 tumors. The exons 1 to 12 and adjacent intronic sequences were amplified using FastStart High Fidelity PCR System (Roche Applied Science, Germany) according to the manufacturer’s instructions. BigDye Terminator v3.1 Ready Reaction Mix (Applied Biosystems, Foster City, CA) was used for sequencing reaction, and separation was performed on ABI 3500 genetic analyzer (Applied Biosystems). The collected data were analyzed by using Sequence analyzer software (Applied Biosystems). Designed primers used for amplification and sequencing analysis are shown in Table 4. Each variant or suspicious fragment was verified by independent PCR amplification and sequence analysis in tumor. Exonic variants that were detected in tumor tissue were analyzed also in the corresponding normal tissue (when available) from the same patients. All detected variants were confirmed by sequencing of forward and reverse strands.
Nomenclature of mutations
Mutations were described according to the nomenclature system recommended by the Human Genome Variation Society (HGVS)34. Designation of the genomic alterations in the MTDH gene is based on the GenBank reference sequences NM_178812. Mutations which were not found in the literature, the Single Nucleotide Polymorphism Database (dbSNP, http://www.ncbi.nlm.nih.gov/SNP/, (accessed in June, 2015)35, or in the Catalogue of Somatic Mutations in Cancer (COSMIC, http://www.sanger.ac.uk/cosmic, accessed in June, 2015)36 were considered as novel.
Statistical analyses
Importance of frequent variants was analyzed by using the STATISTICA 10 (StatSoft, Tulsa, OK). The chi-square test was applied to determine the relationship of MTDH variants with clinicopathological variables. Cox’s Proportional Hazard Model was used to test the relationship between the variants and the patient survival. All tests were two sided, and a P-value less than 0.05 was considered as significant.
In silico prediction of impact of the variants on protein function
Exonic variants were evaluated by widely used programs for prediction of possible interference with the function, structure or stability of a protein (Supplementary Table 5): Mutation Taster (http://www.mutationtaster.org; Ensembl transcript ENST00000336273, NM_178812; GRCh37/ Ensembl 69), SIFT and GVGD as a part of commercial Alamut 2.0 (Interactive Biosoftware, Roven, France), PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/; UniProt peptide Q86UE4), PROVEAN (http://provean.jcvi.org/index.php; Human GRCh37/Ensemble 66) and, MUpro (http://mupro.proteomics.ics.uci.edu).
Additional Information
How to cite this article: Gnosa, S. et al. MTDH genetic variants in colorectal cancer patients. Sci. Rep. 6, 23163; doi: 10.1038/srep23163 (2016).
References
Ferlay, J. et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer, doi: 10.1002/ijc.29210 (2014).
Amersi, F., Agustin, M. & Ko, C. Y. Colorectal cancer: epidemiology, risk factors, and health services. Clin Colon Rectal Surg 18, 133–140, doi: 10.1055/s-2005-916274 (2005).
Fearon, E. R. & Vogelstein, B. A genetic model for colorectal tumorigenesis. Cell 61, 759–767 (1990).
Lievre, A., Blons, H. & Laurent-Puig, P. Oncogenic mutations as predictive factors in colorectal cancer. Oncogene 29, 3033–3043, doi: 10.1038/Onc.2010.89 (2010).
Pritchard, C. C. & Grady, W. M. Colorectal cancer molecular biology moves into clinical practice. Gut 60, 116–129, doi: 10.1136/gut.2009.206250 (2011).
Kang, D. C. et al. Cloning and characterization of HIV-1-inducible astrocyte elevated gene-1, AEG-1. Gene 353, 8–15, doi: 10.1016/j.gene.2005.04.006 (2005).
Britt, D. E. et al. Identification of a novel protein, LYRIC, localized to tight junctions of polarized epithelial cells. Exp Cell Res 300, 134–148, doi: 10.1016/j.yexcr.2004.06.026 (2004).
Sutherland, H. G., Lam, Y. W., Briers, S., Lamond, A. I. & Bickmore, W. A. 3D3/lyric: a novel transmembrane protein of the endoplasmic reticulum and nuclear envelope, which is also present in the nucleolus. Exp Cell Res 294, 94–105, doi: 10.1016/j.yexcr.2003.11.020 (2004).
Warr, T. et al. Identification of extensive genomic loss and gain by comparative genomic hybridisation in malignant astrocytoma in children and young adults. Genes Chromosomes Cancer 31, 15–22, doi: 10.1002/gcc.1113 (2001).
Wang, K. et al. Genomic landscape of copy number aberrations enables the identification of oncogenic drivers in hepatocellular carcinoma. Hepatology 58, 706–717, doi: 10.1002/hep.26402 (2013).
Yoo, B. K. et al. Astrocyte elevated gene-1 regulates hepatocellular carcinoma development and progression. J Clin Invest 119, 465–477, doi: 10.1172/JCI36460 (2009).
Casimiro, S. et al. Metadherin expression and lung relapse in patients with colorectal carcinoma. Clin Exp Metastasis 31, 689–696, doi: 10.1007/s10585-014-9659-0 (2014).
Hu, G. et al. MTDH activation by 8q22 genomic gain promotes chemoresistance and metastasis of poor-prognosis breast cancer. Cancer Cell 15, 9–20, doi: 10.1016/j.ccr.2008.11.013 (2009).
Emdad, L. et al. AEG-1/MTDH/LYRIC: signaling pathways, downstream genes, interacting proteins, and regulation of tumor angiogenesis. Adv Cancer Res 120, 75–111, doi: 10.1016/B978-0-12-401676-7.00003-6 (2013).
Sarkar, D. & Fisher, P. B. AEG-1/MTDH/LYRIC: clinical significance. Adv Cancer Res 120, 39–74, doi: 10.1016/B978-0-12-401676-7.00002-4 (2013).
Gnosa, S. et al. Expression of AEG-1 mRNA and protein in colorectal cancer patients and colon cancer cell lines. J Transl Med 10, 109, doi: 10.1186/1479-5876-10-109 (2012).
Gnosa, S. et al. AEG-1 expression is an independent prognostic factor in rectal cancer patients with preoperative radiotherapy: a study in a Swedish clinical trial. Br J Cancer 111, 166–173, doi: 10.1038/bjc.2014.250 (2014).
Song, H., Li, C., Li, R. & Geng, J. Prognostic significance of AEG-1 expression in colorectal carcinoma. Int J Colorectal Dis 25, 1201–1209, doi: 10.1007/s00384-010-1009-3 (2010).
Jiang, T., Zhu, A., Zhu, Y. & Piao, D. Clinical implications of AEG-1 in liver metastasis of colorectal cancer. Med Oncol 29, 2858–2863, doi: 10.1007/s12032-012-0186-z (2012).
Yuan, C. et al. The MTDH (−470G > A) polymorphism is associated with ovarian cancer susceptibility. plos One 7, e51561, doi: 10.1371/journal.pone.0051561 (2012).
Lee, S. G. et al. Astrocyte elevated gene-1 contributes to the pathogenesis of neuroblastoma. Oncogene 28, 2476–2484, doi: 10.1038/onc.2009.93 (2009).
Kikuno, N. et al. Knockdown of astrocyte-elevated gene-1 inhibits prostate cancer progression through upregulation of FOXO3a activity. Oncogene 26, 7647–7655, doi: 10.1038/sj.onc.1210572 (2007).
Emdad, L. et al. Activation of the nuclear factor kappaB pathway by astrocyte elevated gene-1: implications for tumor progression and metastasis. Cancer Res 66, 1509–1516, doi: 10.1158/0008-5472.CAN-05-3029 (2006).
Liu, X. et al. Identification of novel variants of metadherin in breast cancer. PLoS One 6, e17582, doi: 10.1371/journal.pone.0017582 (2011).
Zhang, B. et al. Pathologically decreased miR-26a antagonizes apoptosis and facilitates carcinogenesis by targeting MTDH and EZH2 in breast cancer. Carcinogenesis 32, 2–9, doi: 10.1093/carcin/bgq209 (2011).
Li, J., Chen, Y., Zhao, J., Kong, F. & Zhang, Y. miR-203 reverses chemoresistance in p53-mutated colon cancer cells through downregulation of Akt2 expression. Cancer Lett 304, 52–59, doi: 10.1016/j.canlet.2011.02.003 (2011).
Hui, A. B. et al. Significance of dysregulated metadherin and microRNA-375 in head and neck cancer. Clin Cancer Res 17, 7539–7550, doi: 10.1158/1078-0432.CCR-11-2102 (2011).
Yang, Y. et al. MiR-136 promotes apoptosis of glioma cells by targeting AEG-1 and Bcl-2. FEBS Lett 586, 3608–3612, doi: 10.1016/j.febslet.2012.08.003 (2012).
Dong, R. et al. miR-145 inhibits tumor growth and metastasis by targeting metadherin in high-grade serous ovarian carcinoma. Oncotarget 5, 10816–10829 (2014).
Guo, J., Xia, B., Meng, F. & Lou, G. miR-137 suppresses cell growth in ovarian cancer by targeting AEG-1. Biochem Biophys Res Commun 441, 357–363, doi: 10.1016/j.bbrc.2013.10.052 (2013).
Zhang, N. et al. MicroRNA-30a suppresses breast tumor growth and metastasis by targeting metadherin. Oncogene 33, 3119–3128, doi: 10.1038/onc.2013.286 (2014).
Li, W., Zhai, L., Zhao, C. & Lv, S. miR-153 inhibits epithelial-mesenchymal transition by targeting metadherin in human breast cancer. Breast Cancer Res Treat, doi: 10.1007/s10549-015-3346-y (2015).
Thirkettle, H. J. et al. LYRIC/AEG-1 is targeted to different subcellular compartments by ubiquitinylation and intrinsic nuclear localization signals. Clin Cancer Res 15, 3003–3013, doi: 10.1158/1078-0432.CCR-08-2046 (2009).
den Dunnen, J. T. & Antonarakis, S. E. Mutation nomenclature extensions and suggestions to describe complex mutations: a discussion. Hum Mutat 15, 7–12, doi: 10.1002/(SICI)1098-1004(200001)15:1<7::AID-HUMU4>3.0.CO;2-N (2000).
Coordinators, N. R. Database resources of the National Center for Biotechnology Information. Nucleic Acids Res 41, D8–D20, doi: 10.1093/nar/gks1189 (2013).
Forbes, S. A. et al. COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res 39, D945–950, doi: 10.1093/nar/gkq929 (2011).
Acknowledgements
The study was supported by grants from the Swedish Cancer Foundation, Swedish Research Council, and the Health Research Council in South-East Sweden, and project RVO 64165 Ministry of Health, Czech Republic.
Author information
Authors and Affiliations
Contributions
Study concept and design: S.G., I.T., X.F.S. Acquisition of data: S.G., I.T. Analysis and interpretation of data: S.G., I.T., X.F.S. Statistical analyses: S.G. Contribution of the patient material with clinical data: S.H. Drafting of the manuscript: S.G., I.T., X.F.S. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Gnosa, S., Ticha, I., Haapaniemi, S. et al. MTDH genetic variants in colorectal cancer patients. Sci Rep 6, 23163 (2016). https://doi.org/10.1038/srep23163
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep23163
This article is cited by
-
Bioinformatic analysis reveals an association between Metadherin with breast cancer prognosis and tumor immune infiltration
Scientific Reports (2024)
-
Metadherin (MTDH) overexpression significantly correlates with advanced tumor grade and stages among colorectal cancer patients
Molecular Biology Reports (2021)
-
Activation of EMT in colorectal cancer by MTDH/NF-κB p65 pathway
Molecular and Cellular Biochemistry (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.