Abstract
We aimed to describe the ethnic variations in ocular dimensions among three ethnic groups with similar genetic ancestry from mainland of China. We included 2119 ethnic Bai, 2202 ethnic Yi and 2183 ethnic Han adults aged 50 years or older in the study. Ocular dimensions including axial length (AL), anterior chamber depth (ACD), vitreous chamber depth (VCD) and lens thickness (LT) were measured using A-scan ultrasonography. Bai Chinese had longer ALs (P < 0.001), deeper ACDs (P < 0.001) but shallower VCDs (P < 0.001) compared with the other two ethnic groups. There were no ethnic variations in LTs. Diabetes was associated with shallower ACDs and this association was stronger in Bai Chinese compared with Yi or Han Chinese (P for interaction = 0.02). Thicker lenses were associated with younger age (P = 0.04), male gender (P < 0.001), smoking history (P = 0.01), alcohol intake (P = 0.03), the presence of cataract (P < 0.001) and the presence of diabetes (P < 0.001). There were significant differences in ocular dimensions among different ethnic groups with small differences in genetics but large variations in cultures and lifestyles.
Similar content being viewed by others
Introduction
Numerous studies have tried to elucidate the etiologies of age-related eye disorders including refractive errors, age-related macular degeneration, age-related cataract and glaucoma, which are the major causes of visual impairment and blindness in older people1. Potential ethnic variations in the risk of these age-related eye disorders have been reported. For example, myopia seems to be more prevalent in East Asians including Chinese, Japanese or Koreans2,3. The prevalence of primary open angle glaucoma is higher in Africans while the prevalence of primary angle closure glaucoma is higher in Asians compared with Europeans4. Anatomically, these age-related eye disorders have been linked with ocular dimensions such as axial length (AL)5. Therefore, an in-depth knowledge of the potential ethic variations in ocular dimensions provides further insights into the etiologies of these eye disorders.
Up till now, population-based studies have reported a wide range of normative data on ocular dimensions among various ethnic groups in different areas of the world6,7,8,9,10,11. However, inter-study comparisons of these estimates are difficult considering the methodological disparities among different studies including sampling strategies, age ranges of the study subjects and measurements of ocular dimensions. The Singapore Epidemiology of Eye Diseases (SEED) study provided initial evidence on a possible ethnic difference in the ocular dimensions measured by IOL master among the three major ethnic groups including Chinese, Malays and Indians in this city state by collecting data using the same study protocols12. It is interesting to understand whether ethnic differences exist in multiethnic population with relatively smaller variations in genetics. In addition, IOL master does not provide important ocular dimension data of lens thickness (LT) or vitreous chamber depth (VCD) and whether there are ethnic differences in these ocular dimensions remains unclear.
China is the world’s most populous country with a multiethnic population including Han ethnicity and another 55 ethnic minorities. Han ethnicity is the major ethnic group which accounts for about 90% of the entire national population. The Yi and Bai ethnicities are the major ethnic minorities in China. These ethnic groups have different cultures, languages and lifestyles, yet relatively similar genetic ancestry13. In this study, we describe the ethnic variations in the distributions and determinants of ocular dimensions measured by an Echoscan among the three ethnic groups (Bai, Yi and Han ethnicities) in rural China.
Methods
Study cohort
The Yunnan Minority Eye Studies (YMES) are population-based studies conducted among different ethnic groups including the Han ethnicity (the major ethnic group) and other ethnic minorities in Southwestern China using the same study protocols for data collection. The YMES were conducted from 2011 to 2014. In a previous report, we have described the detailed methodology of YMES and some major findings in a single ethnic group, that is, the Bai ethnicity14,15,16,17. Now, we have finished the data collection for the other two ethnic groups: Yi and Han ethnicities, which allowed for multiethnic comparisons. Briefly, random cluster sampling strategies were adopted to select ethnic Bai, Yi and Han adults aged 50 years or older living in a rural community. These three ethnic groups resided in separate towns within a rural community in Yunnan Province. Information regarding ethnicity was collected from the study participants’ identity cards. Different ethnic groups were not living in the same villages and there were few inter-marriages among different ethnic groups. Each village in the study site with a population of approximately 1000 was considered as a cluster during the sampling procedure. Villages with a population of less than 750 were combined and those of more than 1500 were divided and regrouped. Subsequently, 10% of the total clusters were randomly selected using a computer-assisted program. In the end of the study, 2133 (77.8%) ethnic Bai, 2208 (82.0%) ethnic Yi and 2205 (80.5%) ethnic Han adults participated in this study, respectively. There were no age or gender differences between study participants and non-participants among all ethnic groups (all P > 0.05). The same research team collected data from all three ethnic groups using the same equipment.
All studies were approved by the Kunming Medical University Institutional Review Board and the conduct of the studies adhered to the Declaration of Helsinki. The study methods were carried out in accordance with the approved guidelines. Informed consent was obtained from all study participants.
Clinical Examinations
Ocular dimensions including AL, anterior chamber depth (ACD), VCD and LT were measured using an Echoscan (US-800; Nidek Co., Ltd, Tokyo, Japan) and the mean of the 5 readings was used for data analysis. Non-cycloplegic autorefraction was performed using an autorefractor (RM-8000; Topcon Corp., Tokyo, Japan) and refraction was subjectively refined until the best visual acuity was obtained.
Information regarding participants’ educational level, socioeconomic status, lifestyle-related factors (e.g., smoking, alcohol intake), disease history and medication intake was collected using a detailed questionnaire by a trained research assistant. Height was measured in centimeters using a wall-mounted measuring tape after removing shoes while weight was measured in kilograms after taking off heavy clothing. Systolic blood pressure, diastolic blood pressure and pulse rate for all participants were recorded using a standardized mercuric-column sphygmomanometer and one of four cuff sizes (pediatric, regular adult, large, or thigh) was selected based on the circumference of the participant’s arm. Hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or a physician diagnosis. Diabetes mellitus was defined as non-fasting glucose levels higher than 200 mg/dL (11.1 mmol/L) or previous physician diagnosis of diabetes or use of anti-diabetic medications based on the American Diabetes Association guidelines18. Slit-lamp examination (model SL-1E; Topcon) was performed by trained study ophthalmologists and included a clinical grading of cataract according to the Lens Opacities Classification System (LOCS) III19.
Statistical analyses
Data analyses were performed using STATA version 11.0 (StataCorp, College Station, Tex., USA). Since ocular dimensions for both eyes were highly correlated (Pearson correlation coefficient for AL = 0.96, P < 0.001; ACD = 0.91, P < 0.001; VCD = 0.95, P < 0.001; LT = 0.90, P < 0.001) and the results of analysis for both eyes were similar, results were presented for right eyes only.
Mean ocular dimension parameters were compared across each age group using the Analysis of Variance (ANOVA) test. Age-sex-adjusted mean values were calculated using a covariance model. Associations between factors of interest and ocular dimension parameters were initially assessed using univariate regression analyses. Besides age, sex and ethnicity, factors with a P value of less than 0.10 in univariate models were retained in the multivariate models. To determine whether ethnicity modified associations between factors of interest and a specific ocular dimension parameter, a linear regression model was established with interaction terms between ethnicity and each potential risk factor and a likelihood ratio test was performed on the interaction terms. If the interaction term was statistically significant (P < 0.05), stratified analysis were performed subsequently.
Results
Table 1 compares the demographic and systematic parameters among the three ethnic groups. In brief, adults of Bai ethnicity were youngest, best educated, heaviest, had the highest blood pressure and were least likely to smoke or take alcohol drinks. Adults of Yi ethnicity were shortest, lightest and were most likely take alcohol drinks. Adults of Han ethnicity had the lowest blood pressures.
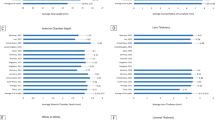
Of the total 6546 study participants, 63 who had missing data in the right eye were excluded, leaving 6483 (99%) for further analysis. ALs, ACDs and VCDs were not normally distributed in any ethnic groups (all P for K-S test < 0.05). LTs followed a normal distribution in all ethnic groups (all P for K-S test > 0.05). The mean age- and sex-adjusted AL were 23.15 ± 1.23 mm (95% confidence interval [CI] 23.11, 23.20), 23.04 ± 1.03 mm (95% CI 23.00, 23.08) and 22.95 ± 1.21 mm (95% CI 22.86, 22.95) in ethnic Bai, Yi and Han adults, respectively (P < 0.001). These figures were 3.42 ± 0.54 mm (95% CI 3.38, 3.46), 2.98 mm ± 0.38 (95% CI 2.94, 3.02) and 2.86 ± 0.40 mm (95% CI 2.81, 2.90) for ACD (P < 0.001), 15.35 ± 1.35 mm (95% CI 15.31, 15.40), 15.73 ± 1.02 mm (95% CI 15.69, 15.77) and 15.70 ± 1.26 mm (95% CI 15.66, 15.74) for VCD (P < 0.001) and 4.35 ± 0.62 mm (95% CI 4.30, 4.39), 4.48 mm ± 0.43 (95% CI 4.44, 4.52) and 4.47 mm ± 0.48 (95% CI 4.45, 4.52) for LT (P = 0.01). After adjusting for the effect of height, the magnitude of differences in the mean values of ocular dimensions did not change significantly (Table 2). The age-specific mean ocular biometric data are shown in Figs 1, 2, 3, 4.
In univariate regression analyses, longer ALs were associated with older age (P < 0.001), male sex (P < 0.001), Bai (P < 0.001) ethnicity, formal education (P = 0.005), taller stature (P < 0.001), greater weight (P < 0.001), the presence of hypertension (P = 0.01) and the absence of smoking history (P < 0.001). Deeper anterior chambers were associated with male sex (P < 0.001), Bai (P < 0.001) or Yi (P < 0.001) ethnicity, taller stature (P < 0.001), formal education (P = 0.01) and the absence of diabetes (P < 0.001). Deeper vitreous chambers were associated with older age (P < 0.001), male sex (P < 0.001), Han ethnicity (P < 0.001), formal education (P < 0.001), taller stature (P < 0.001), greater weight (P < 0.001) and the presence of hypertension (P < 0.001). Thicker lenses were associated with younger age (P < 0.001), male sex (P < 0.001), formal education (P < 0.001), taller stature (P < 0.001), greater weight (P < 0.001) and the presence of smoking history (P < 0.001), alcohol intake (P = 0.001), the presence of cataract (P < 0.001) and the presence of diabetes (P = 0.004).
In multivariate linear regression models adjusting for age, sex, ethnicity and factors with a P value of less than 0.10 in univariate models, longer ALs were associated with older age, male sex, Bai or Yi ethnicity, formal education, taller stature, greater weight and the absence of smoking history. Deeper anterior chambers were associated with male sex, Bai or Yi ethnicity and the absence of diabetes. Deeper vitreous chambers were associated with older age, male sex, Han ethnicity, formal education, taller stature and greater weight. Thicker lenses were associated with younger age, male sex, the presence of smoking history, alcohol intake, the presence of cataract and the presence of diabetes (Table 3).
A significant joint effect of diabetes with ethnicity on ACD (P for interaction = 0.02) was detected using a likelihood ratio test. Further ethnicity-stratified analysis indicated the association of diabetes with ACD (regression coefficient = −0.039 mm for Bai ethnicity; regression coefficient = −0.025 mm for Yi ethnicity; regression coefficient = −0.017 mm for Han ethnicity) was stronger in adults of Bai ethnicity compared with those of Yi or Han ethnicities in multivariate analyses.
Discussion
In this multiethnic population of adults aged 50 years or older, we found significant differences in ocular dimensions such as ALs, ACDs and VCDs but not LTs among various ethnic groups with small genetic differences. Adults of Bai ethnicity had the deepest anterior but shallowest vitreous chambers among the three ethnic groups. Further well-designed cohort studies are warranted to assess whether the observed ethnic variations in ocular dimensions are related to different risks of age-related eye disorders in this population.
The take-home message of our study was that people of different ethnicities with small genetic differences may also have large differences in ocular dimensions. Previous multiethnic studies have shown a significant ethnic variation in ocular dimensions among different ethnic groups, which was considered to be attributed to the variations in genetics among different ethnic groups. Although previous data indicated that genetic differences in ethnic groups in Southwestern China are relatively smaller13, it needs to be recognized that statements about commonality are based on the overall genome and a close global relationship does not preclude very specific differentiation between populations. Thus, based on the data in this study, we could not conclude that interplay and effects of cultures, lifestyles, or socioeconomic status in early life might affect the growth of eyeball, resulting in different ocular dimensions in adulthood.
We observed that ethnic Bai people had the longest ALs after adjusting for height among the three ethnic groups. AL is known to be composed of ACD, VCD and LT and the longest ALs observed in Bai people were mainly explained by that they had the deepest ACDs. The explanation for this interesting finding was unclear. It is likely that Bai people were inherently born with a deeper ACD and a shallower VCD compared with other ethnic groups in this study. Further studies are warranted to examine whether the differences in ocular biometry observed in this study had functional implications. For example, shallower ACDs are associated with a higher risk of angle closure glaucoma. Therefore, whether Bai people are more susceptible to angle closure glaucoma compared with the other two groups needs to be investigated.
Another interesting finding of this study was that patients with diabetes were more likely to have shallower anterior chambers and this association was modified by ethnicity. A recent meta-analysis of 47 individual studies indicated that diabetes is an independent risk factor for glaucoma20. Some individual studies have also reported that diabetes could increase the risk of open angle glaucoma21,22. Considering that the magnitude of difference was small, we cannot conclude that diabetes is a risk factor for angle closure glaucoma. Further well-designed cohort studies are warranted to confirm this finding and basic research is needed to elucidate the biological mechanism behind this association.
We observed a slightly increasing trend of AL and VCD with age in this study. VCD is a major part of AL. This age-related pattern of AL was different from other studies in Asians living in urban areas, which revealed an inverse relationship between older age and increasing AL6,7,23. Considering that AL is a major determinant for refractive status, the namely “cohort effect” on myopia prevalence found in many other population-based studies12,24,25,26,27,28 was not observed in this study. The possible explanation for this result is that the study area is an inland rural town located in the southwest part of China and has not experienced a dramatic change in social and environmental factors during the past few decades as compared with many metropolises in China and other countries in East Asia.
There were few studies exploring the ethnic variations in LTs and their associated factors. We found that ethnic variations in LTs were not significant after adjusting for the effects of a wide range of confounders. The major determinants for LTs are lifestyle-related factors (e.g. smoking, alcohol intake) or metabolic disorders such as cataract or diabetes, suggesting that metabolism plays a major role in crystalline lens growth. Smoking is a well-established risk factor for cataract29. Heavy alcohol drinking was found to be associated with cataract in a recently published meta-analysis30. There is a need to identify the specific metabolic biomarkers which are linked with the growth of crystalline lens. In addition, it is a surprising to find that LTs decreased slightly with increasing age, which contradicted previous view that LTs decrease with increasing age. However, the aged effect on LT was very small and the P value was marginally significant in this study (P = 0.04). This observation may be explained by the increases in height and biometry which overshadow the effects of longitudinal change. It was also likely to be a chance finding.
The study’s strengths included a large sample size, multiethnic study participants, reasonable response rates, standardized clinical measurements for ocular dimensions and the usage of the same study protocols for data collection across different ethnic groups. There were also some limitations for this study, which should be acknowledged. First, A-scan ultrasonography may not be precise in measuring some of the ocular dimensions such as LT, especially when cataract is present. Second, we were unable to identify the full set of explanatory factors for the observed ethnic differences in AL, ACD and VCD. Third, ethnicity was identified by official records in this study. Genetic measures of ancestry may be more accurate for ethnicity identification but was not performed in this study due to limited resources. Finally, the cross-sectional design limited the ability to assess causal relationship when analyzing risk factors.
In conclusion, this study of multiethnic participants living in the same geographic location in rural China found significant ethnic variations in ocular dimensions including ALs, ACDs and VCDs but not LTs, with Bai Chinese having deeper anterior but shallower vitreous chambers as compared with the other two ethnic groups. Our study also provided the normative data for ocular dimensions in ethnic minorities in China, which are important to guide future clinical practice (e.g., cataract or refractive surgery) or research (e.g., designing multi-ethnic clinical trials on AL or ACD-related conditions such as retinal disorders and glaucoma).
Additional Information
How to cite this article: Niu, Z. et al. Large variations in ocular dimensions in a multiethnic population with similar genetic background. Sci. Rep. 6, 22931; doi: 10.1038/srep22931 (2016).
References
Wong, T. Y. & Hyman, L. Population-based studies in ophthalmology. Am J Ophthalmol 146, 656–663 (2008).
Morgan, I. & Rose, K. How genetic is school myopia? Prog Retin Eye Res 24, 1–38 (2005).
Pan, C. W., Dirani, M., Cheng, C. Y., Wong, T. Y. & Saw, S. M. The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci 92, 258–266 (2015).
Tham, Y. C., Li, X., Wong, T. Y., Quigley, H. A., Aung, T. & Cheng, C. Y. Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040 A Systematic Review and Meta-Analysis. Ophthalmology 121, 2081–2090 (2014).
Pan, C. W. et al. Differential associations of myopia with major age-related eye diseases: the Singapore Indian Eye Study. Ophthalmology 120, 284–291 (2013).
Wong, T. Y., Foster, P. J., Ng, T. P., Tielsch, J. M., Johnson, G. J. & Seah, S. K. Variations in ocular biometry in an adult Chinese population in Singapore: the Tanjong Pagar Survey. Invest Ophthalmol Vis Sci 42, 73–80 (2001).
Lim, L. S. et al. Distribution and determinants of ocular biometric parameters in an Asian population: the Singapore Malay eye study. Invest Ophthalmol Vis Sci 51, 103–109 (2009).
Bhatt, A. B., Schefler, A. C., Feuer, W. J., Yoo, S. H. & Murray, T. G. Comparison of predictions made by the intraocular lens master and ultrasound biometry. Arch Ophthalmol 126, 929–933 (2008).
Shufelt, C., Fraser-Bell, S., Ying-Lai, M., Torres, M. & Varma, R. Refractive error, ocular biometry and lens opalescence in an adult population: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci 46, 4450–4460 (2005).
Warrier, S. et al. Ocular biometry and determinants of refractive error in rural Myanmar: the Meiktila Eye Study. Br J Ophthalmol 92, 1591–1594 (2008).
Wickremasinghe, S. et al. Ocular biometry and refraction in Mongolian adults. Invest Ophthalmol Vis Sci 45, 776–783 (2004).
Pan, C. W. et al. Prevalence of refractive errors in a multiethnic Asian population: the Singapore epidemiology of eye disease study. Invest Ophthalmol Vis Sci 54, 2590–2598 (2013).
Lin, H. et al. Genetic relationships of ethnic minorities in Southwest China revealed by microsatellite markers. Plos One 5, e9895 (2010)
Li, J. et al. The prevalence and causes of visual impairment in an elderly Chinese Bai ethnic rural population: the Yunnan minority eye study. Invest Ophthalmol Vis Sci 53, 4498–4504 (2012).
Shen, W. et al. Prevalence and outcomes of cataract surgery in adult rural Chinese populations of the Bai nationality in Dali: the Yunnan minority eye study. Plos One 8, e60236 (2013).
Zhong, H. et al. Prevalence of and risk factors for pterygium in rural adult chinese populations of the Bai nationality in Dali: the Yunnan Minority Eye Study. Invest Ophthalmol Vis Sci 53, 6617–6621 (2012).
Zhong, H. et al. The prevalence of glaucoma in adult rural Chinese populations of the Bai nationality in Dali: the Yunnan Minority Eye Study. Invest Ophthalmol Vis Sci 53, 3221–3225 (2012).
Diagnosis and classification of diabetes mellitus. Diabetes Care 33 Suppl 1, S62–69 (2010).
Chylack, L. T. Jr. et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 111, 831–836 (1993).
Zhao, D., Cho, J., Kim, M. H., Friedman, D. S. & Guallar, E. Diabetes, fasting glucose and the risk of glaucoma: a meta-analysis. Ophthalmology 122, 72–78 (2015).
Mitchell, P., Smith, W., Chey, T. & Healey, P. R. Open-angle glaucoma and diabetes: the Blue Mountains eye study, Australia. Ophthalmology 104, 712–718 (1997).
Friedman, D. S., Wilson, M. R., Liebmann, J. M., Fechtner, R. D. & Weinreb, R. N. An evidence-based assessment of risk factors for the progression of ocular hypertension and glaucoma. Am J Ophthalmol 138, S19–31 (2004).
Pan, C. W. et al. Ocular biometry in an urban Indian population: the Singapore Indian Eye Study (SINDI). Invest Ophthalmol Vis Sci 52, 6636–6642 (2011).
Saw, S. M. et al. Prevalence and risk factors for refractive errors in the Singapore Malay Eye Survey. Ophthalmology 115, 1713–1719 (2008).
Attebo, K., Ivers, R. Q. & Mitchell, P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology 106, 1066–1072 (1999).
Wensor, M., McCarty, C. A. & Taylor, H. R. Prevalence and risk factors of myopia in Victoria, Australia. Arch Ophthalmol 117, 658–663 (1999).
Sawada, A., Tomidokoro, A., Araie, M., Iwase, A. & Yamamoto, T. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology 115, 363–370 e363 (2008).
Pan, C. W. et al. Prevalence and risk factors for refractive errors in Indians: the Singapore Indian Eye Study (SINDI). Invest Ophthalmol Vis Sci 52, 3166–3173 (2011).
Ye, J. et al. Smoking and risk of age-related cataract: a meta-analysis. Invest Ophthalmol Vis Sci 53, 3885–3895 (2012).
Gong, Y., Feng, K., Yan, N., Xu, Y. & Pan, C. W. Different amounts of alcohol consumption and cataract: a meta-analysis. Optom Vis Sci 92, 471–479 (2015).
Acknowledgements
This study was funded by the National Natural Science Foundation of China under grant No. 81460085, No. 81160121 and No. 81371016. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
H.Z. and C.-W.P. conceived of and designed the study. Z.N., J.L., H.Z., Z.Y., H.Z., Y.Z., Y.Y., Q.C. and C.-W.P. performed the experiments. C.-W.P. analyzed the dataset. Z.N. and J.L. wrote the manuscript. Z.N., J.L., H.Z., Z.Y., H.Z., Y.Z., Y.Y., Q.C. and C.-W.P. reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Niu, Z., Li, J., Zhong, H. et al. Large variations in ocular dimensions in a multiethnic population with similar genetic background. Sci Rep 6, 22931 (2016). https://doi.org/10.1038/srep22931
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep22931
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.