Abstract
This study aimed to investigate the occurrence of and determine the risk factors for steatorrhea in chronic pancreatitis (CP). It was based on analysis of both retrospectively and prospectively acquired database for CP patients admitted to our center from January 2000 to December 2013. Demographic data, course of disease, medical history and follow-up evaluations of patients were documented in detail. Cumulative rate of steatorrhea was calculated by using the Kaplan–Meier method. For risk factor analysis, multivariate analysis by Cox proportional hazards regression model was performed. A total of 2,153 CP patients were included with a mean follow-up duration of 9.3 years. Approximately 14% (291/2,153) of CP patients presented with steatorrhea at diagnosis of CP. Cumulative rates of steatorrhea at 1, 5, 10 and 20 years after diagnosis of CP were 4.27% (95% CI: 3.42%–5.34%), 12.53% (95% CI: 10.74%–14.59%), 20.44% (95% CI: 17.37%–23.98%) and 30.82% (95% CI: 20.20%–45.21%), respectively. Male gender (HR = 1.771, p = 0.004), diabetes (HR = 1.923, p < 0.001), alcohol abuse (HR = 1.503, p = 0.025) and pancreaticoduodenectomy (HR = 2.901, p < 0.001) were independent risk factors for steatorrhea while CP in adolescents (HR = 0.433, p = 0.009) was a protective factor. In conclusion, male gender, adult, diabetes, alcohol abuse and pancreaticoduodenectomy lead to increased risk of steatorrhea in CP patients.
Similar content being viewed by others
Introduction
Chronic pancreatitis (CP) is a progressive condition characterized by pancreatic acinar atrophy and fibrosis, which leads to irreversible damage of pancreatic endocrine and exocrine function. CP patients with pancreatic exocrine insufficiency (PEI) usually present with nutrition malabsorption which leads to vitamin and micronutrient deficiency and weight loss1,2 and have increased risks of developing premature atherosclerosis, cardiovascular events, osteoporosis, fracture, immune deficiency and infection3,4,5.
It has been reported that 42%–99% of CP patients may develop PEI6,7,8,9,10. Although several direct and indirect function tests are available for the assessment of pancreatic function, diagnosis of mild/moderate PEI is difficult as these pancreatic function tests are either invasive or have limited diagnostic accuracy11,12. Steatorrhea, an overt presentation of severe PEI, is commonly observed in CP patients and occurs at the late stage of disease course when less than 10% of the pancreatic exocrine function is preserved13,14. Identifying the risk factors for steatorrhea might be helpful for indicating mild/moderate PEI.
Factors concerning disease duration and etiology might be associated with increased/decreased risk of developing steatorrhea. For example, steatorrhea is more common during the second decade after the onset of CP7. In alcoholic chronic pancreatitis (ACP), the interval between the first attack of a CP symptom and steatorrhea is around 13 years, which is substantially shorter than that in hereditary pancreatitis (HP) (≥26 years)6,15. The effect of pancreatic ductal morphology and calcification on the development of steatorrhea is currently a subject of debate8,16,17,18. Other patient-related factors, such as the initial symptom of CP, type of abdominal pain, severe acute pancreatitis attack and treatment strategy, might also be related to steatorrhea development.
This study was based on a retrospective-prospective cohort of 2,153 CP patients with a long duration of follow-up after the onset of CP. We aimed to determine the prevalence of steatorrhea in CP patients and identify the risk factors, which might help to improve the outcome of CP patients with PEI.
Results
General characteristics of patients
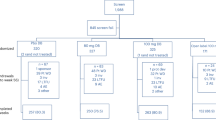
From January 2000 to December 2013, a total of 2,287 CP patients were enrolled in Changhai CP Database. A total of 134 patients, which consisted of 16 patients diagnosed with pancreatic cancer within two years after the diagnosis of CP, 108 AIP patients and 10 GP patients, were excluded from this study (Fig. 1). The general characteristics of the remaining 2,153 patients were presented in Table 1. We lost contact with 260 patients (12.1%) during follow-up and the mean duration of follow-up was 9.3 years (SD 7.2 years). Idiopathic chronic pancreatitis (ICP) was most common (76.27%) in this study, whereas the proportion of ACP was 18.81% only. Among the 2,153 CP patients, a total of 493 (22.90%) developed steatorrhea during follow-up.
As Changhai Hospital is a tertiary medical center, almost 30% of the patients admitted to our center had received interventional procedures in primary medical centers. Minimally invasive interventions were used as principle methods prior to surgery in our center and the overall treatment strategy was classified as endotherapy (including ESWL) alone (1524, 70.78%), surgery alone (236, 10.96%), both endotherapy and surgery (162, 7.52%) and no interventions due to lack of clinical symptoms (231, 10.73%). A total of 70 patients died during the follow-up period and the causes of death were pancreatic cancer (19, 27.14%), complications of CP (17, 24.29%), non-pancreatic diseases (28, 40%) and accidental death (6, 8.75%).
Clinical characteristics of steatorrhea and non-steatorrhea patients
Steatorrhea patients differed from non-steatorrhea patients in the following aspects: more male patients, fewer adolescent patients, higher prevalence of diabetes mellitus (DM), more ACP, more patients with initial manifestations of DM or steatorrhea and different types of abdominal pain. No significant differences between these two groups were detected in terms of age at the onset or diagnosis of CP, common bile duct (CBD) stricture, pancreatic pseudocyst, stone, development of cancer, interventional treatment strategy and death (Table 1).
Cumulative rate of steatorrhea
After the onset of CP
Steatorrhea developed in 22.90% (493/2153) of the 2,153 eligible patients after the onset of CP; the rates were 24.83% in male patients (369/1486) and 19.19% in female patients (128/667). Steatorrhea developed in 200, 298, 381 and 466 patients at 1, 5, 10 and 20 years after the onset of CP, with the cumulative rates being 9.34% (95% CI: 8.18%–10.66%), 14.76% (95% CI: 13.27%–16.40%), 21.87% (95% CI: 19.89%–24.03%) and 41.14% (95% CI: 36.94%–45.62%), respectively. Moreover, a significant difference in the rate of steatorrhea was observed between male and female patients (p = 0.003, Fig. 2a,b).
Cumulative rates of steatorrhea.
(a) Overall cumulative rate of steatorrhea after the onset of chronic pancreatitis (CP); (b) Cumulative rates of steatorrhea stratified by gender (male vs. female) after the onset of CP; (c) Overall cumulative rate of steatorrhea after the diagnosis of CP; (d) Cumulative rates of steatorrhea stratified by gender (male vs. female) after the diagnosis of CP; (e) Overall cumulative rate of steatorrhea after successful main pancreatic duct (MPD) drainage; (f) Cumulative rates of steatorrhea stratified by method for MPD drainage (ERCP/ESWL vs. surgery).
After the diagnosis of CP
Fourteen percent (291/2153) of patients manifested with steatorrhea at the diagnosis of CP. After excluding these patients, the remaining 1,862 patients were included to calculate the cumulative rate of steatorrhea after the diagnosis of CP. Steatorrhea developed in 74, 165, 198 and 201 patients 1, 5, 10 and 20 years after the diagnosis of CP, with the cumulative rates being 4.27% (95% CI: 3.42%–5.34%), 12.53% (95% CI: 10.74%–14.59%), 20.44% (95% CI: 17.37%–23.98%) and 30.82% (95% CI: 20.20%–45.21%), respectively. Male patients had a significantly higher rate of steatorrhea compared with female patients (p < 0.001, Fig. 2c,d).
After the first successful MPD drainage
For 1,544 patients who showed no signs of steatorrhea when successful drainage of MPD was performed by interventions, the cumulative rate of steatorrhea after the first successful intervention that achieved MPD drainage was described. Steatorrhea developed in 54, 109 and 123 patients at 1, 5 and 10 years after intervention treatment, with the cumulative rates being 3.91% (95% CI: 3.00%–5.07%), 10.86% (95% CI: 8.93%–13.17%) and 15.09% (95% CI: 12.34%–18.39%), respectively (Fig. 2e). Among the 1,544 patients, 82.19% (1269/1544) achieved successful drainage of MPD via endotherapy and the remaining 17.81% (275/1544) via surgery. Log-rank test showed that endotherapy group had lower cumulative rate of steatorrhea than the surgery group (mean interval of steatorrhea: 12.93 years vs. 12.17 years, p < 0.001, Fig. 2f).
Predictors for steatorrhea
All 20 variables in Table 2 were considered potential predictors of newly occurring steatorrhea and were analyzed in the univariate analysis. Eight variables showed a p value less than 0.10. These eight variables were selected as candidates for multivariate analysis by the Cox proportional hazards regression model. The results showed that five factors were independent predictors of newly onset steatorrhea. The risk factors were male gender (hazard ratio (HR) = 1.771, p = 0.004), DM (HR = 1.923, p < 0.001), alcohol abuse (HR = 1.503, p = 0.025) and pancreaticoduodenectomy (HR = 2.901, p < 0.001) and the protective factor was CP in adolescents (HR = 0.433, p = 0.009).
Discussion
PEI, which has a negative effect on nutrition absorption, is rarely confirmed at the early stage for CP patients. Severe PEI, namely, pancreatic exocrine failure, which manifests as clinical steatorrhea, is commonly diagnosed in CP patients. A substantial proportion of CP patients had PEI without overt steatorrhea and detection of risk factors for PEI would be clinically important. But direct function tests available for PEI are invasive and with risk of complications, which makes them difficult to be used in clinical practice as well as in clinical research. For the current study, we focused on severe PEI and presence of steatorrhea was set as the sign of severe PEI. Steatorrhea is related to increased risks of cardiovascular events, osteoporosis, fracture et al. and is a direct and decisive evidence of PEI for CP in clinical practice. We detected the prevalence of steatorrhea in CP and its predictors with a relatively large sample size (Table 3), which may help improve the outcome of CP patients with PEI.
For 2,153 CP patients, the overall incidence rate of steatorrhea was 22.9% over a median follow-up period of 7.8 years after the onset of CP. The cumulative rate of steatorrhea after the diagnosis of CP was 12.5% at 5 years, whereas Sandhu et al. reported a risk rate of 28% over a median follow-up period of 3.7 years (including 159 patients)16. We reported a lower rate of steatorrhea with longer disease course, which might be due to fewer ACP patients in our study. Pancreatic exocrine function is dependent on adequate acinar mass and function and alcohol is toxic to the pancreas and is likely to severely damage the pancreatic parenchyma.
We identified several predictors for steatorrhea. Possible explanations for decreased risk of steatorrhea for CP in adolescents were: (1) compared to adult CP patients, adolescent CP patients have better preservation of pancreatic function and also better repair capacity after injury; (2) most of adolescent CP cases were followed up in less than 20 years and we expect similar cumulative risk of steatorrhea with a long-term follow-up. A previous study also showed that exocrine and endocrine insufficiency developed more slowly in early-onset CP than in late-onset CP6. Therefore, adolescent CP patients had a reduced risk of steatorrhea compared to adult CP patients during the equivalent period of CP course.
Pancreaticoduodenectomy was identified as an independent risk factor for steatorrhea, while drainage of pancreatic duct (by ESWL/ERCP or LPJ) or partial resection of pancreas (head resection or tail resection) seemed not to increase the risk of steatorrhea. This indicates that steatorrhea as a sign of pancreatic exocrine function failure is due to diffuse and severe loss of pancreatic parenchyma. CP being a progressive disease with loss of pancreatic acinar tissue, minimally invasive method rather than resectional procedures may be a better choice given the advantage of preservation of pancreatic parenchyma19.
In the current study, ACP was considered when alcohol intake exceeded 80 g/d for male and 60 g/d for female for at least 2 years for CP patients in the absence of other causes, respectively. ACP patients showed a higher risk of steatorrhea, but the risk might be underestimated. There might be a proportion of patients considered as ICP who might probably have ACP. The Oriental population might be more sensitive to alcohol-related injuries than the Caucasian population because they tend to have a less-active aldehyde dehydrogenase, which is a key detoxifying enzyme for alcohol20,21.
Patients with DM showed higher risk for steatorrhea. Considerable evidence suggests important functional interactions between the exocrine and endocrine pancreas. The interactions occur at several regulatory levels and the true dimension is still unknown22.
Pancreatic stone was analyzed as one of the potential predictors of steatorrhea, which was indicated in several studies7,23,24. However, we were unable to find a relationship between pancreatic stone and steatorrhea risk in the context of ductal drainage, which is in agreement with the findings of Lankisch et al.18. Stone in CP is commonly considered to be associated with an abnormal constitution of proteins and supersaturation of calcium carbonate in pancreatic juice. However, the detailed mechanism is still unknown and the interaction between stone and PEI is poorly understood.
The Changhai CP Database established in 2005 has been collecting clinical data of CP patients since January 2000 and data have been collected retrospectively before January 2005 and prospectively ever since. Statistical analysis showed that there was no significant difference between the clinical characteristics of patients who were first admitted before January 2005 and those admitted after that date. Therefore, the recall bias minimally influenced the results of the study.
Our study has some limitations. First, clinical steatorrhea was used as a sign of severe PEI; dietary habits and celiac disease-related steatorrhea were not considered. Second, the retrospectively acquired data collected between 2000 and 2004 might introduce recall bias. Prospective data collection since January 2005 minimized the chance of incomplete or inaccurate data collection. Third, risk factor analysis did not include all potential factors related to the development of steatorrhea. Fourth, 603 CP patients were followed up for less than 2 years after the diagnosis of CP; among these patients, several pancreatic cancer patients may have been misdiagnosed as CP25. However, these limitations minimally influence the results considering the relatively large sample size of the study.
In conclusion, CP patients showed increased risk of steatorrhea for those of male gender, adults, DM, alcohol abuse and pancreaticoduodenectomy. The evaluation of risk factors in CP patients before the occurrence of steatorrhea might help determine the replacement therapy of pancreatic enzyme earlier, which ensures that severe complications related to PEI can be avoided. Prospectively conducted studies are expected to confirm the benefit of early treatment of PEI on CP patients.
Methods
This study was based on analysis of both retrospectively and prospectively acquired database.
Patients and database
Since the 1990s, an electronic medical record system (GOODWILL Inc., Beijing, China) has been used in Changhai Hospital (Shanghai, China), which has facilitated several studies on CP26,27,28,29. In order to track changes consistently throughout the course of CP and to facilitate the evaluation and study of the disease, a dedicated database, Changhai CP Database (version number 2.1, YINMA Information Technology Inc., Shanghai, China), was established in 2005 to collect clinical data of CP patients ever since. Data from January 2000 to December 2004 were retrospectively collected according to the electronic medical record system and additional data were collected through telephone, letter and e-mail inquiries. Data were prospectively collected since January 2005. The following information was documented in detail: demographic data (age, sex, birthplace, et al.), course of CP, medical history, history of other diseases, smoking history/status, alcohol history/status, family history of pancreatic diseases and DM, laboratory and imaging findings and treatment strategy.
The database system was also set a reminder for investigators to call patients for clinical checkups. Aside from visits due to complaints of discomfort related to CP, all patients were periodically (at least once a year) recalled for clinical checkup and investigations. Ultrasound, MRI, or CT was selected as an evaluation modality during each follow-up visit. An evaluation of each revisit, or an evaluation via telephone inquiries for patients who did not have follow-up visits to Changhai Hospital, was added to the CP database.
In December 2013, we contacted all the patients in our database for a final evaluation, except those who were lost to follow-up or died. The duration of follow-up is defined as the duration from the onset of CP to the date of the last personal contact, death, or December 2013, whichever came first.
The study was approved by the Ethics Committee of Changhai Hospital, The Second Military Medical University, Shanghai, China according to the Helsinki Declaration. Written informed consent was obtained from all participating patients. All of the diagnostic and therapeutic modalities were carried out in accordance to the approved guidelines.
Definitions
CP was diagnosed according to the Asia-Pacific consensus of CP30. ACP was diagnosed when alcohol intake exceeded 80 g/d for male and 60 g/d for female for at least two years in the absence of other causes, respectively27,31. HP was diagnosed when the CP patient had no less than two first-degree relatives with CP or recurrent acute pancreatitis (AP), or no less than three second-degree relatives with CP or recurrent AP32. We defined abnormal anatomy of pancreatic duct system (including pancreas divisum and anomalous pancreaticobiliary junction) as an etiology of CP in our study, although it still remains a controversy33. A patient was defined as post-traumatic CP due to a definite history of abdominal trauma with imaging evidence of pancreatic injury and subsequent ductal dilation. Hyperlipidemia was considered as an etiology when blood triglyceride was higher than 1,000 mg/dL at the diagnosis of CP34. CP patients were considered idiopathic when none of the above etiologies were found.
Patients who were diagnosed with pancreatic cancer less than two years after the diagnosis of CP were excluded from this study26,35. Autoimmune pancreatitis (AIP) and groove pancreatitis (GP) were also excluded from this study: AIP is different from typical CP in terms of pathophysiology, clinical manifestations and prognosis, while GP could hardly be differentiated from pancreatic head carcinoma until pancreaticoduodenectomy and confirmed histological findings36.
Diagnosis of steatorrhea was established when either of the following conditions was met: (1) chronic diarrhea with foul-smelling, oily bowel movements37; (2) a positive result in quantification of fecal fat determination (fecal fat quantification was performed over a period of three days; steatorrhea was defined as a fecal fat excretion of more than 14 g/day).
Treatment strategy
As a tertiary medical center, Changhai Hospital admitted patients with previous pancreas-related surgical, endoscopic, or other invasive procedures from primary medical centers. In our center, minimally invasive interventions were taken as principle methods prior to surgery: extracorporeal shock wave lithotripsy (ESWL)/endoscopic retrograde cholangiopancreatography (ERCP) for stone removal and main pancreatic duct (MPD) drainage, insertion of stents to treat dominant MPD stricture and biliary duct stricture and endoscopic drainage for uncomplicated pseudocyst with endoscopic reach28,35,38,39,40,41,42,43,44,45. For CP patients who did not experience pain, interventions were performed only when CP was complicated by CBD stricture, pancreatic portal hypertension, et al.; DM or steatorrhea was not an indication for invasive treatment of CP13.
Data management and statistical analysis (Fig. 1)
Continuous and categorical variables were presented as mean ± SD and counts (percentages), respectively. Student’s t-test or Mann–Whitney U test and χ-square test or Fisher’s exact test were used as indicated. Cumulative rates of steatorrhea were calculated by using the Kaplan–Meier method after the onset of CP (all CP patients were included), after the diagnosis of CP (patients with steatorrhea at the diagnosis of CP were excluded) and after the first successful drainage of MPD (only patients who without steatorrhea at the time of the first successful drainage of MPD were included). Log-rank test was used to further analyze the difference of cumulative rates of steatorrhea between two groups (e.g., male vs. female, endotherapy vs. surgical treatment). For risk factor analysis, multivariate analysis by Cox proportional hazards regression model was performed to identify the independent predictors based on the results of univariable analyses (factors with a significance level of p < 0.10 were included in the multivariate analysis). Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. Statistical analyses were conducted at a significance level of 0.05 for all analyses. Data were analyzed by using SPSS 18.0 (SPSS, Chicago, IL, USA).
Additional Information
How to cite this article: Li, B.-R. et al. Risk Factors for Steatorrhea in Chronic Pancreatitis: A Cohort of 2,153 Patients. Sci. Rep. 6, 21381; doi: 10.1038/srep21381 (2016).
References
Dominguez-Munoz, J. E., Iglesias-Garcia, J., Vilarino-Insua, M. & Iglesias-Rey, M. 13C-mixed triglyceride breath test to assess oral enzyme substitution therapy in patients with chronic pancreatitis. Clin Gastroenterol Hepatol. 5, 484–488 (2007).
Dominguez-Munoz, J. E. & Iglesias-Garcia, J. Oral pancreatic enzyme substitution therapy in chronic pancreatitis: is clinical response an appropriate marker for evaluation of therapeutic efficacy? JOP. 11, 158–162 (2010).
Pongprasobchai, S. Maldigestion from pancreatic exocrine insufficiency. J Gastroenterol Hepatol. 28 Suppl 4, 99–102 (2013).
Montalto, G. et al. Lipoproteins and chronic pancreatitis. Pancreas. 9, 137–138 (1994).
Tignor, A. S. et al. High prevalence of low-trauma fracture in chronic pancreatitis. Am J Gastroenterol. 105, 2680–2686 (2010).
Layer, P. et al. The different courses of early- and late-onset idiopathic and alcoholic chronic pancreatitis. Gastroenterology. 107, 1481–1487 (1994).
Ammann, R. W., Akovbiantz, A., Largiader, F. & Schueler, G. Course and outcome of chronic pancreatitis. Longitudinal study of a mixed medical-surgical series of 245 patients. Gastroenterology. 86, 820–828 (1984).
Braganza, J. M., Hunt, L. P. & Warwick, F. Relationship between pancreatic exocrine function and ductal morphology in chronic pancreatitis. Gastroenterology. 82, 1341–1347 (1982).
Lankisch, M. R., Imoto, M., Layer, P. & DiMagno, E. P. The effect of small amounts of alcohol on the clinical course of chronic pancreatitis. Mayo Clin Proc. 76, 242–251 (2001).
Ammann, R. W., Buehler, H., Muench, R., Freiburghaus, A. W. & Siegenthaler, W. Differences in the (Nonalcoholic) and Natural History of Idiopathic Alcoholic Chronic Pancreatitis. A Comparative Long-Term Study of 287 Patients. Pancreas. 2, 368–377 (1987).
Nojgaard, C., Olesen, S. S., Frokjaer, J. B. & Drewes, A. M. Update of exocrine functional diagnostics in chronic pancreatitis. Clin Physiol Funct Imaging. 33, 167–172 (2013).
Keller, J., Aghdassi, A. A., Lerch, M. M., Mayerle, J. V. & Layer, P. Tests of pancreatic exocrine function - clinical significance in pancreatic and non-pancreatic disorders. Best Pract Res Clin Gastroenterol. 23, 425–439 (2009).
Mergener, K. & Baillie, J. Chronic pancreatitis. Lancet. 350, 1379–1385 (1997).
DiMagno, E. P., Go, V. L. & Summerskill, W. H. Relations between pancreatic enzyme ouputs and malabsorption in severe pancreatic insufficiency. N Engl J Med. 288, 813–815 (1973).
Ammann, R. W. Diagnosis and management of chronic pancreatitis: current knowledge. Swiss medical weekly. 136, 166 (2006).
Sandhu, B. S. et al. Recurrent flares of pancreatitis predict development of exocrine insufficiency in chronic pancreatitis. Clin Gastroenterol Hepatol. 5, 1085–1091; quiz 1007 (2007).
Hayakawa, T. et al. Relationship between pancreatic exocrine function and histological changes in chronic pancreatitis. Am J Gastroenterol. 87, 1170–1174 (1992).
Lankisch, P. G., Otto, J., Erkelenz, I. & Lembcke, B. Pancreatic calcifications: no indicator of severe exocrine pancreatic insufficiency. Gastroenterology. 90, 617–621 (1986).
Dumonceau, J. M. et al. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 44, 784–800 (2012).
Perez-Miller, S. et al. Alda-1 is an agonist and chemical chaperone for the common human aldehyde dehydrogenase 2 variant. Nat Struct Mol Biol. 17, 159–164 (2010).
Chan, A. W. Racial differences in alcohol sensitivity. Alcohol Alcohol. 21, 93–104 (1986).
Nunes, A. C. et al. Screening for pancreatic exocrine insufficiency in patients with diabetes mellitus. Am J Gastroenterol. 98, 2672–2675 (2003).
Scuro, L. A. et al. Pancreatic calcifications in patients with chronic pancreatitis. Int J Pancreatol. 6, 139–150 (1990).
Bhasin, D. K. et al. Clinical profile of calcific and noncalcific chronic pancreatitis in north India. J Clin Gastroenterol. 45, 546–550 (2011).
Wang, W. et al. Incidence of pancreatic cancer in chinese patients with chronic pancreatitis. Pancreatology. 11, 16–23 (2011).
Wang, W. et al. Incidence of pancreatic cancer in chinese patients with chronic pancreatitis. Pancreatology. 11, 16–23 (2011).
Wang, W. et al. Occurrence of and risk factors for diabetes mellitus in Chinese patients with chronic pancreatitis. Pancreas. 40, 206–212 (2011).
Li, Z. S. et al. A long-term follow-up study on endoscopic management of children and adolescents with chronic pancreatitis. Am J Gastroenterol. 105, 1884–1892 (2010).
Wang, W. et al. Chronic pancreatitis in Chinese children: etiology, clinical presentation and imaging diagnosis. J Gastroenterol Hepatol. 24, 1862–1868 (2009).
Tandon, R. K., Sato, N. & Garg, P. K. Chronic pancreatitis: Asia–Pacific consensus report. J Gastroenterol Hepatol. 17, 508–518 (2002).
Witt, H. et al. A degradation-sensitive anionic trypsinogen (PRSS2) variant protects against chronic pancreatitis. Nat Genet. 38, 668–673 (2006).
Howes, N. et al. Clinical and genetic characteristics of hereditary pancreatitis in Europe. Clin Gastroenterol Hepatol. 2, 252–261 (2004).
Lu, W.-F. ERCP and CT diagnosis of pancreas divisum and its relation to etiology of chronic pancreatitis. World J Gastroenterol. 4, 150–152 (1998).
Yadav, D. & Pitchumoni, C. Issues in hyperlipidemic pancreatitis. J Clin Gastroenterol. 36, 54–62 (2003).
Li, B. R., Hu, L. H. & Li, Z. S. Chronic pancreatitis and pancreatic cancer. Gastroenterology. 147, 541–542 (2014).
Malde, D. J., Oliveira-Cunha, M. & Smith, A. M. Pancreatic carcinoma masquerading as groove pancreatitis: case report and review of literature. JOP. 12, 598–602 (2011).
Affronti, J. Chronic pancreatitis and exocrine insufficiency. Prim Care. 38, 515–537; ix (2011).
Sun, X. T. et al. Clinical Features and Endoscopic Treatment of Chinese Patients With Hereditary Pancreatitis. Pancreas. 44, 59–63 (2015).
Li, B. R. et al. Risk factors for complications of pancreatic extracorporeal shock wave lithotripsy. Endoscopy. 46, 1092–1100 (2014).
Hu, L. H. et al. Extracorporeal shock wave lithotripsy as a rescue for a trapped stone basket in the pancreatic duct. Endoscopy. 46 Suppl 1 UCTN, E332–333 (2014).
He, Y. X. et al. Endoscopic management of early-stage chronic pancreatitis based on M-ANNHEIM classification system: a prospective study. Pancreas. 43, 829–833 (2014).
Zou, W. B., Hu, L. H., Liao, Z. & Li, Z. S. Obscure hemosuccus pancreaticus due to dorsal pancreatic arteriorrhexis. Dig Liver Dis. 45, 346 (2013).
Hu, L.-H., Liao, Z. & Li, Z.-S. Rolling in the deep: a quaint sphere rolling in the deep pancreatic duct. Gastroenterology. 145, e7–e8 (2013).
Hu, L. H., Liao, Z. & Li, Z. S. Spontaneous clearance of pancreatic stones. Clin Gastroenterol Hepatol. 11, e9–10 (2013).
Ceppa, E. P. et al. Hereditary pancreatitis: endoscopic and surgical management. J Gastrointest Surg. 17, 847-856; discussion 856–847 (2013).
Ammann, A. R. W. et al. Evolution and regression of pancreatic calcification in chronic pancreatitis. A prospective long-term study of 107 patients. Gastroenterology. 95, 1018–1028 (1988).
Acknowledgements
This study was supported by the National Natural Science Foundation of China [Grant Nos 81422010 (Z.L.), 81100316 (L.-H.H.) and 81470883 (L.-H.H.)], the Shanghai ChenGuang Program [Grant No. 12CG40 (L.-H.H.)] and the Shanghai Rising-Star Program [Grant No. 13QA1404600 (Z.L.)].
Author information
Authors and Affiliations
Contributions
B.-R.L., J.P. and T.-T.D. participated in the acquisition, analysis and interpretation of data, as well as in the manuscript drafting; Z.L., B.Y., W.-B.Z., H.C., J.-T.J., Z.-H.Z., D.W., J.-H.L. and S.-B.N. participated in data acquisition and manuscript drafting; L.-H.H. and Z.-S.L. contributed to the conception, design and data interpretation, as well as revised the manuscript for important intellectual content.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Li, BR., Pan, J., Du, TT. et al. Risk Factors for Steatorrhea in Chronic Pancreatitis: A Cohort of 2,153 Patients. Sci Rep 6, 21381 (2016). https://doi.org/10.1038/srep21381
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep21381
This article is cited by
-
Clinical significance of pancreatic calcifications: a 15-year single-center observational study
European Journal of Medical Research (2022)
-
Classification of Early-Onset and Late-Onset Idiopathic Chronic Pancreatitis Needs Reconsideration
Scientific Reports (2020)
-
A mountable toilet system for personalized health monitoring via the analysis of excreta
Nature Biomedical Engineering (2020)
-
Risk factor for steatorrhea in pediatric chronic pancreatitis patients
BMC Gastroenterology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.