Abstract
Compound infantile hemangiomas (IHs) are problematic and usually require intervention. This retrospective study aimed to introduce a combined therapy of oral propranolol and topical timolol and evaluate its efficacy and safety. Eighty-nine infants with compound IHs were treated with oral propranolol 2 mg/kg/day divided 2 times per day and timolol maleate 0.5% gel 3 times per day, for at least 3 months. Two observers evaluated the hemangioma independently at 0, 1, 3, 6, 9 months after the initiation of treatment. Changes in the hemangioma score values were evaluated using paired t test. Rebound growth and adverse effects were recorded. After treatment was completed, this combined therapy achieved clinical response in 100% of the patients (89/89). Significant positive effects were demonstrated at 1, 3, 6 months (p < 0.001), but not obvious after 6 months (p = 0.06). The response of IHs to the therapy was depending on the age at initial treatment. The average treatment duration was 6.48 (5.77–7.19) months. One patient (1.1%) relapsed after cessation of 6-month treatment and 7 children (7.8%) developed side effects. Our study suggested that oral propranolol combined with topical timolol treatment is very effective and well-tolerated for compound IHs, which can be used as a first line treatment.
Similar content being viewed by others
Introduction
Infantile hemangiomas (IHs), the benign tumours of endothelial cells, is characterized by an initial proliferation during infancy followed by spontaneous involution over the following 5–10 years, often leaving fibro-fatty residues, atrophic scarring, or telangiectasia. The incidence varies from 4% to 10% of infants1,2,3. Problematic hemangiomas occur when they are accompanied with painful persistent skin ulceration, rapid growth, disfigurement, or compromise of normal function or cosmetic development. Common locations for problematic hemangiomas include the periorbital, oropharyngeal, preauricular, or parotid regions. These hemangiomas require early and effective treatment to prevent permanent sequelae. According to its depth of involvement, IH can be classified as superficial, deep and compound. Superficial IH originates from papillary dermis and presents as bright red macular or papular mass. Deep IH originates from reticular dermis or subcutaneous tissues and appears as bluish or relatively colorless mass. Compound IH is a combination of both superficial and deep components.
Compound IH was reported being treated with oral propranolol, long-pulse pulsed dye laser or intralesional corticosteroid treatment in previously published studies and the response rate ranged in 66.7%–100%4,5,6,7. However, corticosteroids have potential side effects and unknown long-term safety and long-pulse pulsed dye laser was effective to early hemangiomas only6. Hemangeol (propranolol hydrochloride) was FDA approved in the USA on March 17th, 2014 and marketed as the first and only FDA-approved treatment for proliferating IH requiring systemic therapy. However, approximately 13.7% of patients treated with oral propranolol were reported to experience systemic adverse effects8. Recently, locally administered timolol was proved as an intervention with acceptable efficacy and lower incidence of adverse effects for superficial IHs, but it has barely no effect on subcutaneous components9,10. Oral propranolol combined with topical timolol treatment, targeting at deep and superficial component of compound IHs respectively, may maintain clinical efficacy while avoid systemic adverse effects. However, medical literatures about this combined therapy are very limited and no consensus exists about the proper way to use and monitor this therapy in infants with compound IHs.
The purpose of this retrospective study was to evaluate the efficacy and safety of oral propranolol combined with topical timolol treatment in 89 children with compound IH.
Material and Methods
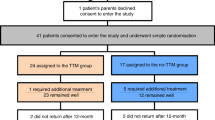
A retrospective study was designed and implemented in a tertiary comprehensive hospital in Shanghai, PR China. The study population was composed of all consecutive patients who required treatment of infantile hemangiomas from January 2014 through May 2014. To be included in the study sample, patients must meet the following inclusion criteria: compound hemangiomas with imminent undesirable functional or cosmetic outcomes if left untreated. The exclusion criteria was that the patients have contraindication of ß-blockers, including bronchial asthma, heart failure, sinus bradycardia, hypoglycaemia, hypotension, heart block and known allergy to ß-blockers. Patients with ulcerated or mucosal IHs were also excluded from the study population. Consent to treatment and documentation of the disease response were received from all parents whose infants participated in the present study. The retrospective study followed the tenets of the Declaration of Helsinki for research involving human subjects, informed consent was obtained from all participants and the study was critically reviewed and approved by the institutional review board of Shanghai Ninth People’s Hospital. The methods were carried out in accordance with the approved guidelines of SCIENTIFIC REPORTS.
Evaluations before and during treatment
Before treatment, all patients underwent a thorough history taking and physical examination, including clinical examination, ultrasound investigation, echocardiography, blood pressure and blood glucose measurements. The patients were scheduled to revisit at 1, 3, 6, 9 months after the initiation of treatment for scoring of IHs, physical examination (including blood pressure, heart rate and blood glucose measurements), measuring of body weight for dosage adjustment and recording of adverse effects, until the end of treatment.
Dosage and duration
All patients were treated with oral propranolol and topical timolol, a combination of oral and topical nonselective ß-blockers. The dosage of propranolol (Propranolol Hydrochloride Tablet, Changzhou Kangpu Pharmaceutical Co., Ltd, Jiangsu Province, China) was 2 mg/kg/day divided 2 times daily, meanwhile timolol maleate 0.5% gel (School of Pharmacy, Shanghai Jiao Tong University, China) was applied evenly on the surface of tumours 3 times daily (the dosage was depending on the IH’s surface area). This dosage was maintained during the entire period of the study. The objective of treatment was to inhibit further growth and induce complete regression of the lesions. Treatment was continued until the objective goals were obtained or no further improvement could be achieved. Then the medication of oral propranolol was tapered by decreasing to one half dose for 2 weeks followed by one quarter dose for 2 weeks and then discontinued. The treatment of topical timolol was ceased when there was no improvement of the superficial component of IH.
Hemangioma score system
Until now, no standardized or validated method exists for outcomes measurement of hemangiomas. Because the goal of treatment is reducing functional and cosmetic impairment, the semi-quantitative hemangioma score system may be sufficient to meet these goals (Table 1)11. Two senior oral and maxillofacial surgeons independently evaluated all patients by determining their hemangioma score at each follow-up visit. For the patient with more than 1 cutaneous IHs, the mean value of each hemangioma score was employed. The mean of the two independent measurements was used for data analysis. At each clinical follow-up visit, the hemangiomas were given a score from 0 to 15 to evaluate the activity and severity. The score system consists of 5 components: color, surface consistency, firmness, depth by ultrasound and organ involvement. Because an organ involvement has the largest medical relevance, this component is the one with the strongest score. The purpose of the score was to monitor and compare the hemangioma from visit to visit individually and from patient to patient. Reducing in hemangioma score was graded as none (0%), minimal (<25%), fair (≥25% and <50%), moderate (≥50% and <75%), near complete (≥75% and <100%) or complete (100%) resolution.
Statistical analysis
Patient demographics, hemangioma characteristics, indications for treatment were presented as descriptive statistics. The change in the hemangioma score values of the IHs was evaluated using paired t test, comparing the different follow-up visits. All statistical tests were 2-tailed and α was set at 0.05. Intra-observer reliability was evaluated using the intra-class correlation coefficient (ICC) by standard statistical software packages (SPSS, version17.0, Chicago). A ICC value <0.40 was considered poor agreement, 0.40–0.60 was fair agreement, 0.61–0.80 was good agreement and >0.80 was excellent agreement.
Results
Patients’ demographic data and were summarized in Table 2. There were 89 children in the study, ranging in age from 1 month to 1.5 years. The mean age was 4.96 ± 4.15 months and the median age was 3 months. Three children had previously been treated with laser and failed to achieve significant improvement. The range of ICCs was between 0.91 and 0.98, demonstrating excellent reliability within raters.
Statistical analysis showed that the combined therapy achieved responses in 100% of this case series (89/89). The initial hemangioma score before treatment was 8.67(7.55–9.79) and the score at the end of the treatment was 2.07(0.91–3.23), which indicated that the involution of the hemangiomas was statistically significant (p ≤ 0.001). There was a rapid response to treatment and an immediate statistically significant improvement during the initial 1-month follow-up visit (p ≤ 0.001). During the following clinical evaluation visits, a significant continuous involution of the hemangiomas score was documented until the end of the treatment. When up to 9 months, the improvement compared to the 6-month value was not obvious (p = 0.06) (Fig. 1). Relevant difference exists when distributed according to the patient’s age at the beginning of the combined treatment (Fig. 2). There was a marginally significant improvement observed in children with IH in whom the treatment was started after 12 months of age (p = 0.03).
Hemangioma scores of hemangiomas distributed to different ages (months at the beginning of therapy) before, during and at the end of propranolol treatment.
Data were expressed as means (95% confidence intervals). *indicated p < 0.05 when compared to the previous hemangioma score, **indicated p < 0.001 when compared to the previous hemangioma score.
Of 89 patients, the resolution of hemangioma was complete in 19 children (21.3%), near-complete in 41 children (46.1%), moderate in 18 children (20.2%), fair in 7 children (7.9%), minimal in 4 children (4.5%).
During the following outpatient clinic evaluation visits, few minor side effects were noted: cold extremities (n = 3; 3.4% of all patients), agitation during the night (n = 2; 2.2%) and diarrhoea (n = 2; 2.2%). None of these side effects resulted in a discontinuation of the combined treatment.
The average treatment duration was 6.48 (5.77–7.19) months. After the end of treatment, a rebound growth of the hemangiomas was noted in 1 patient (1.1%). This rebound resulted in a second combined therapy regimen.
Figures 3 and 4 showed patients with compound infantile hemangiomas before and after combined therapy.
Discussion
Infantile hemangiomas (IH) are the most common benign vascular tumors of infancy. The various risk factors include female gender, prematurity, low birth weight, multiple pregnancies, advanced maternal age and in vitro fertilization1. Over 60% IH affect the head and neck region. Morphologically, hemangiomas are classified into superficial, deep and compound types. Oral propranolol has become the standard treatment for high-risk and deep IH, whereas topical timolol is commonly used for superficial lesions to minimize systemic side effects. In this study, we introduced a combined therapy consisting of oral propranolol and topical timolol, which is targeting at both superficial and deep components of compound IHs.
In this study, the overall response rate was 100% (89/89), which indicated that the combined therapy could inhibit the growth and promote regression of compound IHs. Different modalities have been reported for treatment of IHs, include laser surgery, cryosurgery and pharmacotherapy (namely, corticosteroids, vincristine, α-interferon, cyclophosphamide and propranolol). Their response rates for compound IHs were between 67%–100%4,5,6,7,12,13. Previous case series and observational studies have shown that after the initiation of therapy, a visible change in color and considerable softening of the lesion occurs within 1 month, followed by the growth halt or progressive involution11,14,15,16. Our results are consistent with these findings (Fig. 1). The first noticeable effects of the combined therapy were the continuing fading of the color as well as softening of the lesions. The clinically based changes in lesions’ color and firmness have been objectively proven by the statistically significant changes at lesions’ score (P < 0.001). This is related to the β2 inhibitory effect of ß-blockers that decreases the release of the vasodilator transmitters such as nitric oxide. The resulting vasoconstriction of the feeding capillaries is responsible for the early changes in hemangiomas17. At 6 months of treatment, the average score was 2.3(1.0–3.6) (p < 0.001 compared to the pre-treatment value) and 16 children (18%) demonstrated complete resolution. The intermediate effects of ß-blocker is due to down regulation of both vascular endothelial growth factors (VEGF) and basic fibroblast growth factors (bFGF) expression in proliferative IH, resulting in inhibition of pro-angiogenic cascade and angiogenesis. The long term effect of ß-blocker is due to apoptosis resulting in regression of hemangiomas17. This may be the reason for its use in the post proliferative phase.
Ideally, propranolol should be initiated immediately once the decision is made. In this study, there was significant improvement observed in children younger than 12-month (p < 0.001, compared with the pre-treatment value), while minimal reduction was observed in children older than 12-month (p = 0.03, compare with the pre-treatment value) (Fig. 2). In 59 cases less than 6-month at the beginning of treatment in the present study, a considerable shortening of the natural course of IHs (55/59) had been achieved for those lesions at proliferative phase. This finding was in accordance with previous studies: A recent systematic review (including 1264 children in 41 studies) showed that oral propranolol was initiated at a mean age of 6.6 months (range from 3 days to 10 years)18. Other researchers did not observe any improvement in children with IH in whom the propranolol was started after 9 months of age16. Previously published studies also indicated that early treatment with oral propranolol, particularly when started during the proliferative phase, has been shown to be associated with better long-term outcomes19,20,21. Although no large prospective studies confirm that early start of propranolol therapy results in better outcomes, it is always better to start the treatment as early as possible during rapid proliferation of the tumor.
The duration of therapy depends on the extent of involvement and the sensitivity to the treatment. A systematic review of 1264 children in 41 studies found that the propranolol was administered for an average duration of 6.4 months (range 1 weeks to 15 months)18. In a recent study on propranolol treatment for complicated IH, the authors have used the drug for a mean duration of 10.7 months22. In this study, the mean duration of treatment was 6.48 (5.77–7.19) months, which indicated that the combined therapy may shorten the treatment duration. However, one child (2-month old) had relapse after cessation of 6-month combined therapy. This is consistent to the previous studies which suggested that the optimal propranolol treatment must at least cover the entire proliferative phase of compound IHs4,11,22. As for larger and deeper IHs, due to their protracted late proliferative phase, the treatment could extending to the age of 12 months23.
The reported side effects of ß-blocker include hypotension, bradycardia, hypoglycaemia, pulmonary symptoms, sleep disturbances, somnolence, cold extremities and gastro-intestinal (GI) complaints. These adverse reactions are reversible, dose-dependent and not serious24. In a systematic review18 of 39 studies in 1189 children, 371 cases (31.2%) had adverse reactions. The most common adverse event was sleep changes in 136 cases (11.4%), followed by acrocyanosis in 61 children (5.1%). There were 41 reports (3.4%) of GI problem like diarrhoea and gastroesophageal reflux. Respiratory adverse events were seen in 35 patients (2.9%). Hypotension and bradycardia were seen in 39 (3.3%) and 8 cases (0.7%), respectively. Hypoglycaemia was reported only in 4 cases (0.3%). In this study, seven children (7.8%) developed side effects: three children (3.4%) with cold extremities, two children (2.2%) with agitation during the night and 2 children (2.2%) with diarrhoea. The incidences of total and subcategory side effects were lower than the data mentioned above, which indicated that the combined therapy could be a safe choice for compound IHs. No patient had serious side effects leading to discontinuation of the combined therapy. Oral propranolol was administered strictly after feeding and parents are advised to avoid long periods of fasting, this might be the reasons that hypoglycaemia didn’t occur in our series.
Currently there is no universally accepted protocol for initiation, dosage and monitoring of topical timolol treatment. As timolol is 4–10 times as potent as propranolol25, the overall dose of concomitant use of oral propranolol and topical timolol should be taken into consideration. In the recent consensus conference report on propranolol treatment for hemangioma, a target dose of 1–3 mg/kg has been recommended24 and the average treatment dose of propranolol was 2.1 mg/kg/day24. In this study, the dosage of propranolol was 2 mg/kg/day, while the dosage of timolol maleate 0.5% gel (5 mg/mL) was 8.33 mg per day (50 ml gel for 1 month, dosage for a moderate IH). In general, the percutaneous systemic absorption of most topical drugs occupies only a small percentage of total drug amounts. Using a revised and probably still overly cautious estimate of the systemic bioavailability of 5%–10% topical timolol gel-forming solution would yield equivalent oral propranolol doses of only 0.2 to 1.0 mg, or 0.05 to 0.25 mg/kg for a 4-kg infant (0.03–0.17 mg/kg for a 6-kg infant, i.e., a 3-month-old in the 50th percentile for weight)26. These estimates suggest far less need for caution and systemic side effects of topical timolol are unlikely to occur. However, until larger clinical trials are completed and the safety is fully established, the combined therapy should be used with caution, especially in preterm infants, IH with large body surface areas.
IHs are the most common benign vascular tumors in children. They are a cause of parental discomfort and anxiety and need to be carefully assessed from the treatment point of view. In this study, oral propranolol combined with topical timolol treatment was proven to be very effective and safe for compound IHs, this may offer a better first line treatment. However, future prospective trials involving a larger number of patients and a longer follow-up period should be addressed to determine whether this combined therapy fulfils its therapeutic promise. Anticipatory guidance and appropriate monitoring protocol are important for the safe use of the combined therapy.
Conclusion
This retrospective study revealed that oral propranolol combined with topical timolol treatment is very effective and safe for compound IHs, which can be used as a first line treatment. Future prospective trials involving a larger number of patients and a longer follow-up period should be addressed to determine whether this combined therapy fulfils its therapeutic promise.
Additional Information
How to cite this article: Jing Ge. et al. Oral propranolol combined with topical timolol for compound infantile hemangiomas: a retrospective study. Sci. Rep. 6, 19765; doi: 10.1038/srep19765 (2016).
References
Kilcline, C. & Frieden, I. J. Infantile hemangiomas: how common are they? A systematic review of the medical literature. Pediatric dermatology 25, 168–173, 10.1111/j.1525-1470.2008.00626.x (2008).
Kanada, K. N., Merin, M. R., Munden, A. & Friedlander, S. F. A prospective study of cutaneous findings in newborns in the United States: correlation with race, ethnicity and gestational status using updated classification and nomenclature. The Journal of pediatrics 161, 240–245, 10.1016/j.jpeds.2012.02.052 (2012).
Hoornweg, M. J., Smeulders, M. J., Ubbink, D. T. & van der Horst, C. M. The prevalence and risk factors of infantile haemangiomas: a case-control study in the Dutch population. Paediatric and perinatal epidemiology 26, 156–162, 10.1111/j.1365-3016.2011.01214.x (2012).
Talaat, A. A., Elbasiouny, M. S., Elgendy, D. S. & Elwakil, T. F. Propranolol treatment of infantile hemangioma: clinical and radiologic evaluations. Journal of pediatric surgery 47, 707–714, 10.1016/j.jpedsurg.2011.10.058 (2012).
Kwon, S. H. et al. Effect of early long-pulse pulsed dye laser treatment in infantile hemangiomas. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.] 40, 405–411, 10.1111/dsu.12451 (2014).
Rizzo, C. et al. Outcomes of childhood hemangiomas treated with the pulsed-dye laser with dynamic cooling: a retrospective chart analysis. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.] 35, 1947–1954, 10.1111/j.1524-4725.2009.01356.x (2009).
Couto, J. A. & Greene, A. K. Management of problematic infantile hemangioma using intralesional triamcinolone: efficacy and safety in 100 infants. Journal of plastic, reconstructive & aesthetic surgery : JPRAS 67, 1469–1474, 10.1016/j.bjps.2014.07.009 (2014).
Izadpanah, A., Izadpanah, A., Kanevsky, J., Belzile, E. & Schwarz, K. Propranolol versus corticosteroids in the treatment of infantile hemangioma: a systematic review and meta-analysis. Plastic and reconstructive surgery 131, 601–613, 10.1097/PRS.0b013e31827c6fab (2013).
Ovadia, S. A., Landy, D. C., Cohen, E. R., Yang, E. Y. & Thaller, S. R. Local administration of beta-blockers for infantile hemangiomas: a systematic review and meta-analysis. Annals of plastic surgery 74, 256–262, 10.1097/sap.0000000000000390 (2015).
Chambers, C. B., Katowitz, W. R., Katowitz, J. A. & Binenbaum, G. A controlled study of topical 0.25% timolol maleate gel for the treatment of cutaneous infantile capillary hemangiomas. Ophthalmic plastic and reconstructive surgery 28, 103–106, 10.1097/IOP.0b013e31823bfffb (2012).
Schneider, M., Cremer, H. J. & Ruef, P. A retrospective analysis of systemic propranolol for the treatment of complicated infantile haemangiomas. Acta paediatrica (Oslo, Norway : 1992) 103, 977–983, 10.1111/apa.12691 (2014).
Bagazgoitia, L. et al. Propranolol for infantile hemangiomas. Pediatric dermatology 28, 108–114, 10.1111/j.1525-1470.2011.01345.x (2011).
Leaute-Labreze, C. et al. A randomized, controlled trial of oral propranolol in infantile hemangioma. The New England journal of medicine 372, 735–746, 10.1056/NEJMoa1404710 (2015).
Hogeling, M., Adams, S. & Wargon, O. A randomized controlled trial of propranolol for infantile hemangiomas. Pediatrics 128, e259–266, 10.1542/peds.2010-0029 (2011).
Schiestl, C. et al. Efficacy and safety of propranolol as first-line treatment for infantile hemangiomas. European journal of pediatrics 170, 493–501, 10.1007/s00431-010-1324-2 (2011).
Holmes, W. J., Mishra, A., Gorst, C. & Liew, S. H. Propranolol as first-line treatment for rapidly proliferating infantile haemangiomas. Journal of plastic, reconstructive & aesthetic surgery : JPRAS 64, 445–451, 10.1016/j.bjps.2010.07.009 (2011).
Storch, C. H. & Hoeger, P. H. Propranolol for infantile haemangiomas: insights into the molecular mechanisms of action. The British journal of dermatology 163, 269–274, 10.1111/j.1365-2133.2010.09848.x (2010).
Marqueling, A. L., Oza, V., Frieden, I. J. & Puttgen, K. B. Propranolol and infantile hemangiomas four years later: a systematic review. Pediatric dermatology 30, 182–191, 10.1111/pde.12089 (2013).
McGee, P., Miller, S., Black, C. & Hoey, S. Propranolol for infantile haemangioma: a review of current dosing regime in a regional paediatric hospital. The Ulster medical journal 82, 16–20 (2013).
Schupp, C. J., Kleber, J. B., Gunther, P. & Holland-Cunz, S. Propranolol therapy in 55 infants with infantile hemangioma: dosage, duration, adverse effects and outcome. Pediatric dermatology 28, 640–644, 10.1111/j.1525-1470.2011.01569.x (2011).
Sondhi, V. & Patnaik, S. K. Propranolol for infantile hemangioma (PINCH): an open-label trial to assess the efficacy of propranolol for treating infantile hemangiomas and for determining the decline in heart rate to predict response to propranolol. Journal of pediatric hematology/oncology 35, 493–499, 10.1097/MPH.0b013e3182a11658 (2013).
Hermans, D. J., Bauland, C. G., Zweegers, J., van Beynum, I. M. & van der Vleuten, C. J. Propranolol in a case series of 174 patients with complicated infantile haemangioma: indications, safety and future directions. The British journal of dermatology 168, 837–843, 10.1111/bjd.12189 (2013).
Chang, L. C. et al. Growth characteristics of infantile hemangiomas: implications for management. Pediatrics 122, 360–367, 10.1542/peds.2007-2767 (2008).
Drolet, B. A. et al. Initiation and use of propranolol for infantile hemangioma: report of a consensus conference. Pediatrics 131, 128–140, 10.1542/peds.2012-1691 (2013).
McMahon, P., Oza, V. & Frieden, I. J. Topical timolol for infantile hemangiomas: putting a note of caution in “cautiously optimistic”. Pediatric dermatology 29, 127–130, 10.1111/j.1525-1470.2011.01685.x (2012).
Berk, D. R., Lehman, P. A., Franz, T. J., Blunt, J. R. & Bayliss, S. J. On topical timolol gel-forming solution for infantile hemangiomas. Pediatric dermatology 30, 160–161, 10.1111/pde.12060 (2013).
Acknowledgements
This study was partially supported by the National Natural Science Foundation of China (81271163, 81470755 and 81570992) and the Fund for Interdisciplinary Projects of Medicine and Engineering by Shanghai Jiao Tong University.
Author information
Authors and Affiliations
Contributions
J.G. participated in the study design, acquisition of data, analysis and interpretation of data, drafting and revising the manuscript for important intellectual content. J.Z. conceptualized and designed the study, reviewed and revised the manuscript and approved the final manuscript as submitted. L.Z. participated in the study design and the data collection instruments, critically reviewed revising the manuscript for important intellectual content. W.Y. conceptualized and designed the study of timolol maleate for the study treatment, participated in the adverse events monitoring, critically reviewed and revised the manuscript for important intellectual content. H.Z. participated in the data collection instruments, critically reviewed revising the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Ge, J., Zheng, J., Zhang, L. et al. Oral propranolol combined with topical timolol for compound infantile hemangiomas: a retrospective study. Sci Rep 6, 19765 (2016). https://doi.org/10.1038/srep19765
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep19765
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.