Abstract
Mean platelet volume (MPV) has not yet been well-established in urinary tract infection (UTI). The purpose of this study was to evaluate the role of MPV as an acute phase reactant in children with UTI. Data from 118 young children (<2 years) with UTI between 2012 and 2013 were grouped as acute pyelonephritis (APN) and lower UTI according to the dimercaptosuccinic acid (DMSA) scan abnormalities. MPV, platelet distribution width (PDW) platelet count and other infection markers (white blood cell [WBC] count, erythrocyte sedimentation rate [ESR] and C-reactive protein [CRP]) were measured. WBC (P = 0.001), ESR (P = 0.005), CRP (P < 0.001) and MPV levels (P = 0.011) were significantly higher in the APN group than those in the lower UTI group. MPV positively correlated with PDW, CRP and negatively with platelet count. Multiple logistic regression analyses showed that CRP and MPV were independent predictive factors for APN patients. However, the area under the Receiver Operating Characteristic (ROC) curve analysis for MPV was lower than CRP. Our results suggest that MPV can be an inflammatory marker in UTI, but the predictive value of MPV was not superior to CRP in the diagnosis of APN.
Similar content being viewed by others
Introduction
Urinary tract infection (UTI) is one of the common bacterial infections in children and may lead to serious morbidity and mortality1,2. UTI associated with high grade vesicoureteral reflux (VUR) can lead to renal scarring and chronic renal failure3. Clinical symptoms and some inflammatory markers have been used for the differentiation of upper from lower UTI4,5. Laboratory findings of UTI usually show leukocytosis, neutrophilia and increased erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) levels4,5.
Dimercaptosuccinic acid (DMSA) scan is used in distinguishing acute pyelonephritis (APN) from lower UTI, but it can expose the patients to radiation6,7. Platelets play an important role in the pathogenesis of various infectious or inflammatory disorders8,9. Platelet counts and mean platelet volume (MPV) have been studied as inflammatory markers in relation to the disease activity10. MPV may be increased in mild inflammation due to the emergence of the large platelets in the peripheral circulation and conversely, may be decreased in severe inflammation because of the consumption of large platelets in the inflammatory area11,12. MPV has also been studied as an inflammatory marker in various infectious disorders, not only as a negative marker with rotavirus gastroenteritis, but also as a positive marker with hepatitis B, acute appendicitis and sepsis12,13,14,15.
In this study, we compared MPV in children with APN and with low UTI to determine whether it could be used as an inflammatory marker in distinguishing APN with lower UTI.
Results
Clinical characteristics and laboratory findings of the patients were presented in Table 1. There were no significant differences regarding the age at presentation and gender between the APN and lower UTI groups. WBC counts were significantly higher in the APN group than those in the lower UTI group (P = 0.001). ESR (P = 0.005) and CRP levels (P < 0.001) were also significantly higher in the APN group than those in the lower UTI group. The incidence of VUR was more frequent in the APN group (P = 0.004), but abnormal USG findings did not differ between the two groups. There were significant differences between the APN and lower UTI group in terms of MPV levels (P = 0.011), while platelet count (P = 0.742) and PDW (P = 0.451) did not differ between the two groups.
Moreover, MPV positively correlated with PDW (R = 0.338, P < 0.001), CRP levels (R = 0.199, P = 0.031) and negatively with platelet count (R = −0.025, P = 0.006) (Fig. 1). Multiple logistic regression analyses showed that CRP (odds ratio [OR]: 1.026, 95% CI : 1.013–1.040, P < 0.001) and MPV levels (OR: 2.393, 95% CI: 1.019–5.620, P = 0.045] were independent predictive factors for positive DMSA defects in UTI patients (Table 2). However, MPV levels were not different according to gender (male 7.4 ± 0.6 vs. female 7.5 ± 0.5 fL in the APN group [P = 0.878] and male 7.2 ± 0.5 vs. female 7.2 ± 0.6 fL in the lower UTI group [P = 0.927]) and those were not correlated with age (R = −0.092, P = 0.478 in the APN group and R = −0.217, P = 0.107 in the lower UTI group) or the duration of fever (R = −0.036, P = 0.701).
We also analyzed the diagnostic properties of the various inflammatory markers, using ROC curves (Fig. 2). Area under the curves (AUC) values from ROC curve analysis for WBC, ESR, CRP and MPV were 0.670 (P = 0.001, 95% CI: 0.573–0.768), 0.626 (P = 0.018, 95% CI: 0.526–0.727), 0.764 (P < 0.001, 95% CI: 0.678–0.850) and 0.641 (P = 0.008, 95% CI: 0.541–0.742), respectively (Table 3). The AUC values for CRP were higher than those of other inflammatory markers such as WBC, ESR and MPV levels. The AUC values for MPV were lower than those of CRP, but higher than those of ESR.
The sensitivity, specificity, positive and negative predictive values, positive and negative likelihood ratios of the MPV were determined with different cut-off values, which were compared with a previous study (Table 4). MPV, the cut-off value of 7.4 fL and with AUC of 0.641, detected APN patients among those with UTI. The sensitivities and specificities for MPV were found to be 45.2% and 82.1%, respectively.
We found that MPV levels were significantly increased one day after antibiotic therapy (P = 0.031) and were similar 2–5 days after antibiotic therapy and were significantly decreased >6 days after antibiotic therapy (P = 0.046) compared with initial levels (Table 5).
Discussion
The early diagnosis of APN may be difficult during infancy, but differentiation of APN from lower UTI is important due to renal parenchymal damage, which can cause renal scarring that may lead to renal hypertension and chronic renal failure2,3. To differentiate APN from lower UTI, DMSA scan can be used, but it can expose the patients to radiation and require sedation in young infants and children16,17,18.
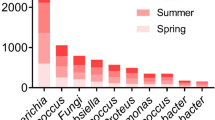
There have been a few reports which have evaluated the relationship between MPV and infectious disorders12,13,14,15. Some studies suggested that MPV increased as a positive acute phase reactant13,14, while others reported that it decreased as a negative acute phase reactant12. MPV as a positive acute phase reactant has much been studied in patients with sepsis. Aydemir et al. reported that MPV was significantly increased for the first 3 days of patients with Gram-positive sepsis, for 4 days in Gram-negative septic patients and for all 5 days in fungal septic patients (P < 0.001)15. Guida et al. also showed that sepsis was frequently associated with thrombocytopenia and an elevation in MPV in very low birth weight infants19. Icli et al. also demonstrated that MPV levels were higher in patients with infective endocarditis and decreased significantly after treatment20. Increased MPV may indicate an increased proportion of young platelets in the peripheral circulation and is suggestive of increased platelet production or increased platelet destruction21. Currently, however, there is no study how fast MPV is elevated in response to infection, requiring future studies.
Conversely, Albayrak et al. reported significantly lower MPV in adults who sustained acute appendicitis than in controls14. The reason for the reduced MPV in acute appendicitis is unclear, but the reduced MPV could be due to the consumption or sequestration of the large activated platelets in intestinal vasculature22. In addition to sepsis and various infections, MPV also has a positive correlation with many different diseases such as diabetes, myocardial infarction and young children with infections and varying degrees of the cut-off value (8.0–10.35 fL), sensitivity (53–98%) and specificity (35–87%)23,24,25,26,27.
Regarding the role of MPV in UTI, Catal et al. reported an increase in MPV in children with APN compared to normal children28. However, they did not analyze MPV levels between APN and lower UTI according to the DMSA scan abnormalities and used the bag urine in some patients as a collection method in the diagnosis of UTI, which might lead to contamination. Tekin et al. showed that the sensitivity and specificity of the MPV using a cut-off value of 8.2 fL was 81.4% and 86.3%, respectively, in predicting APN which were higher than those of the WBC, CRP and ESR levels29.
In the present study, we found increased levels of MPV in children with APN than those with lower UTI, suggesting MPV acted as a positive acute phase reactant in UTI. We also showed that MPV levels had a positive correlation with CRP levels, which further supports previous findings28,29. However, the sensitivity and specificity of the MPV using a cut-off value of 7.4 fL was 45.2% and 82.1%, respectively, in predicting APN and the sensitivity of MPV in predicting APN was lower than that of Tekin et al.’s study29. One of the differences between Tekin et al.’s study and ours is the age of the patient groups29. Tekin et al.’s study included the patients with a broad range of age from 2 months to 12 years while we did young infants with less than 2 years of age29. Therefore, MPV may be an adjunctive inflammatory marker rather than an absolute biomarker for APN in UTI, considering the predictive value of MPV was not superior to CRP in the diagnosis of APN. In addition, platelet count and PDW did not differ between children with APN and those with lower UTI in our study.
Catal et al. speculated that the rise in MPV in APN can be caused by an increased production of larger and/or younger platelets as a reaction to infection-related platelet destruction and increased levels of β-thromboglobulin in bacterial infections might activate and release of platelets30. However, we would like to add another pathomechanism. Although not studied in UTI, there have been some reports on the effect of thrombopoietin (TPO) on MPV levels and Senaran et al. reported that there was a positive correlation between TPO levels and MPV values (P < 0.05) in patients with coronary artery disease31. TPO is thought to be the primary physiological regulator of megakaryopoiesis and injection of recombinant TPO protein selectively induced thrombocytosis in vivo32. Also, cytokines such as interleukin (IL)-6, erythropoietin, stem cell factor and granulocyte–macrophage–CSF are known to play a role in megakaryopoiesis33,34. Because an inflammatory cytokine, IL-6, increased in APN and is associated with renal scarring35, there is a possibility that MPV might be increased due to increased TPO production induced by IL-6 in APN.
Our study has some limitations: the number of patients was not many; the values of normal young children have not been established yet. Although MPV levels did not correlate with the duration of fever in our study, there is the possibility that the time might have an important impact on the MPV levels. We used EDTA as an anticoagulant and analyzed MPV levels within 1 hour, but those levels might be affected by the use of anticoagulants36.
In conclusion, we found that MPV acted as a positive acute phase reactant in children with UTI and MPV levels were significantly elevated in children with APN on DMSA scan. However, the predictive value of MPV was low in the diagnosis of APN. Nevertheless, our results may contribute to our understanding of MPV as an inflammatory marker in UTI.
Further studies are necessary to evaluate the relationship among MPV levels, TPO and IL-6 levels in UTI to elucidate the kinetics of megakaryopoiesis in response to various stimuli in the future, although we did not measure these parameters.
Methods
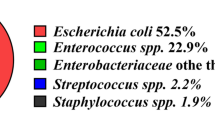
We retrospectively analyzed the data from 118 children (86 boys and 32 girls, aged 2–24 months; mean age of 4.8 ± 3.4 months) with febrile UTI admitted to Severance Children’s Hospital from January 2012 to December 2013. Fever was defined as a body temperature ≥38 °C37. All patients were diagnosed with UTI who had culture growing >50,000 colonies of one single bacterial species on a urine sample obtained by catheterization38. We included only patients who had received blood sampling before administration of antibiotics, because the concomitant antibiotic therapy can affect the MPV levels. We also analyzed the data according to the age and gender to elucidate whether MPV levels are affected by these parameters.
Clinical data such as age, sex and duration of fever were recorded. Before initiation of antibiotic treatment, blood was sampled for laboratory investigations, including white blood cell count, platelets, MPV, ESR and CRP. Peripheral venous blood samples were collected by antecubital venipuncture into Vacutainer tubes (Becton Dickinson™, Rutherford, NJ) containing tripotassium EDTA. Complete blood count (CBC) studies were done within one hour after the blood samples were drawn to minimize changes in platelet size. We also followed a standardized protocol. CBC analysis was performed using Advia 2120i automated analyzer (Siemens Healthcare Diagnostics, Deerfield, IL, USA). CRP levels were measured by the latex-enhanced turbidimetric assay method using a Hitachi 7600 P module (Hitachi, Japan). ESR levels were measured by the TEST 1 (Alifax, Padova, Italy). Strict quality control procedures were adopted.
Radiologic studies such as renal ultrasonography (USG), DMSA scan and voiding cystourethrogram (VCUG) were performed in all patients. After the patients were admitted with UTI, DMSA scan was performed within the first 5 days. They were divided into groups with APN and lower UTI according to the positive (focal or multifocal perfusion defects) or negative DMSA scan abnormalities.
Statistical analyses were performed, using the SPSS for Windows version 18.0 (SPSS Inc., Chicago, Illinois, USA) and MedCalc version 15.8 (MedCalc Software, Belgium). The independent and paired t-test was used for continuous variables and expressed as mean ± standard deviation. Chi-square test was used to analyze categorical variables. Correlation analysis was also carried out to determine the relationship between two variables by Spearman correlation. Multiple logistic regression analysis was used to find independent predictive factors for DMSA scan abnormalities, indicating APN. To establish the predictive value of the parameters for diagnosing APN, receiver operating characteristic (ROC) curves were plotted for WBC, ESR, CRP and MPV. All differences were considered significant at a value of p < 0.05.
Ethics statement
The Institutional Review Board and Research Ethics Committee of Yonsei University Severance Hospital approved this study. We were given exemption from getting informed consents by the IRB because the present study is a retrospective study and personal identifiers were completely removed and the data were analyzed anonymously. Our study was conducted according to the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional Information
How to cite this article: Lee, I. R. et al. Mean platelet volume in young children with urinary tract infection. Sci. Rep. 5, 18072; doi: 10.1038/srep18072 (2015).
References
Masson, P., Matheson, S., Webster, A. C. & Craig, J. C. Meta-analyses in prevention and treatment of urinary tract infections. Infect Dis Clin North Am 23, 355–385 (2009).
Montini, G., Tullus, K. & Hewitt, I. Febrile urinary tract infections in children. N Engl J Med 365, 239–250 (2011).
Fillion, M. L., Watt, C. L. & Gupta, I. R. Vesicoureteric reflux and reflux nephropathy: from mouse models to childhood disease. Pediatr Nephrol 29, 757–766 (2014).
Jaye, D. L. & Waites, K. B. Clinical applications of C-reactive protein in pediatrics. Pediatr Infect Dis J 16, 735–746 (1997).
de Man, P. Bacterial attachment, inflammation and renal scarring in urinary tract infection. Wien Med Wochenschr 141, 537–540 (1991).
Rushton, H. G. The evaluation of acute pyelonephritis and renal scarring with technetium 99m-dimercaptosuccinic acid renal scintigraphy: evolving concepts and future directions. Pediatr Nephrol 11, 108–120 (1997).
Benador, D. et al. Cortical scintigraphy in the evaluation of renal parenchymal changes in children with pyelonephritis. J Pediatr 124, 17–20 (1994).
Hamzeh-Cognasse, H. et al. Platelets and infections - complex interactions with bacteria. Front Immunol 6, 82 (2015).
Nording, H. M., Seizer, P. & Langer, H. F. Platelets in inflammation and atherogenesis. Front Immunol 6, 98 (2015).
Giles, C. The platelet count and mean platelet volume. Br J Haematol 48, 31–37 (1981).
Gasparyan, A. Y., Sandoo, A., Stavropoulos-Kalinoglou, A. & Kitas, G. D. Mean platelet volume in patients with rheumatoid arthritis: the effect of anti-TNF-alpha therapy. Rheumatol Int 30, 1125–1129 (2010).
Tanju, C., Ekrem, G., Berksoy Emel, A. & Nur, A. Mean platelet volume as a negative marker of inflammation in children with rotavirus gastroenteritis. Iran J Pediatr 24, 617–622 (2014).
Turhan, O., Coban, E., Inan, D. & Yalcin, A. N. Increased mean platelet volume in chronic hepatitis B patients with inactive disease. Med Sci Monit 16, Cr202– 205 (2010).
Albayrak, Y. et al. Mean platelet volume: a new predictor in confirming acute appendicitis diagnosis. Clin Appl Thromb Hemost 17, 362–366 (2011).
Aydemir, H. et al. Platelet and mean platelet volume kinetics in adult patients with sepsis. Platelets 26, 331–335 (2015).
Stokland, E. et al. Renal damage one year after first urinary tract infection: role of dimercaptosuccinic acid scintigraphy. J Pediatr 129, 815–820 (1996).
Goldraich, N. P. & Goldraich, I. H. Update on dimercaptosuccinic acid renal scanning in children with urinary tract infection. Pediatr Nephrol 9, 221–226 (1995).
Lin, K. Y. et al. Acute pyelonephritis and sequelae of renal scar in pediatric first febrile urinary tract infection. Pediatr Nephrol 18, 362–365 (2003).
Guida, J. D. et al. Platelet count and sepsis in very low birth weight neonates: is there an organism-specific response? Pediatrics 111, 1411–1415 (2003).
Icli, A. et al. Mean platelet volume is increased in infective endocarditis and decreases after treatment. Med Princ Pract 22, 270–273 (2013).
Becchi, C. et al. Mean platelet volume trend in sepsis: is it a useful parameter? Minerva Anestesiol 72, 749–756 (2006).
Danese, S., Motte Cd Cde, L. & Fiocchi, C. Platelets in inflammatory bowel disease: clinical, pathogenic and therapeutic implications. Am J Gastroenterol 99, 938–945 (2004).
Catal, F. et al. Mean platelet volume (MPV) may simply predict the severity of sepsis in preterm infants. Clin Lab 60, 1193–1200 (2014).
Guclu, E., Durmaz, Y. & Karabay, O. Effect of severe sepsis on platelet count and their indices. Afr Health Sci 13, 333–338 (2013).
Unubol, M., Ayhan, M. & Guney, E. The relationship between mean platelet volume with microalbuminuria and glycemic control in patients with type II diabetes mellitus. Platelets 23, 475–480 (2012).
Dehghani, M. R., Taghipour-Sani, L., Rezaei, Y. & Rostami, R. Diagnostic importance of admission platelet volume indices in patients with acute chest pain suggesting acute coronary syndrome. Indian Heart J 66, 622–628 (2014).
Gao, Y. et al. The impact of various platelet indices as prognostic markers of septic shock. PLoS One 9, e103761 (2014).
Catal, F. et al. Platelet parameters in children with upper urinary tract infection: is there a specific response? Ren Fail 30, 377–381 (2008).
Tekin, M. et al. Is the mean platelet volume a predictive marker for the diagnosis of acute pyelonephritis in children? Clin Exp Nephrol 19, 688–693 (2015).
Douglas, J. T., Lowe, G. D., Forbes, C. D. & Prentice, C. R. Beta-thromboglobulin and platelet counts - effect of malignancy, infection, age and obesity. Thromb Res 25, 459–464 (1982).
Senaran, H. et al. Thrombopoietin and mean platelet volume in coronary artery disease. Clin Cardiol 24, 405–408 (2001).
Kaushansky, K. et al. Promotion of megakaryocyte progenitor expansion and differentiation by the c-Mpl ligand thrombopoietin. Nature 369, 568–571 (1994).
Sheu, J. N. et al. Serum and urine levels of interleukin-6 and interleukin-8 in children with acute pyelonephritis. Cytokine 36, 276–282 (2006).
Sheu, J. N. et al. Relationship between serum and urine interleukin-6 elevations and renal scarring in children with acute pyelonephritis. Scand J Urol Nephrol 43, 133–137 (2009).
Tramma, D., Hatzistylianou, M., Gerasimou, G. & Lafazanis, V. Interleukin-6 and interleukin-8 levels in the urine of children with renal scarring. Pediatr Nephrol 27, 1525–1530 (2012).
McShine, R. L., Sibinga, S. & Brozovic, B. Differences between the effects of EDTA and citrate anticoagulants on platelet count and mean platelet volume. Clin Lab Haematol 12, 277–285 (1990).
Mori, R., Lakhanpaul, M. & Verrier-Jones, K. Diagnosis and management of urinary tract infection in children: summary of NICE guidance. BMJ 335, 395–397 (2007).
Roberts, K. B. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128, 595–610 (2011).
Author information
Authors and Affiliations
Contributions
I.R.L., J.I.S., S.J.P., J.Y.O. and J.H.K. designed study, coordinated data acquisition, analyzed and interpreted the data, drafted and revised the manuscript. All authors read and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lee, I., Shin, J., Park, S. et al. Mean platelet volume in young children with urinary tract infection. Sci Rep 5, 18072 (2015). https://doi.org/10.1038/srep18072
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep18072
This article is cited by
-
Recombinant human thrombopoietin therapy for primary immune thrombocytopenia in pregnancy: a retrospective comparative cohort study
BMC Pregnancy and Childbirth (2023)
-
Association between multimorbidity and mean platelet volume in diabetic patients with acute myocardial infarction
Acta Diabetologica (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.