Abstract
Single-nucleotide polymorphisms (SNP) of the gene belonging to the BCL2 family are thought to play a role in chemotherapy resistance. This study investigated the association of BCL2-938C>A(rs2279115) and BAX-248G>A(rs4645878) promoter region SNPs and the clinical responses and outcomes of 235 non-small cell lung cancer (NSCLC) patients treated with platinum-based chemotherapy. The data suggested that BAX-248GA and GA+AA genotype was associated with poor response [odds ratio (OR) 1.943, p = 0.039; OR 1.867, p = 0.038, respectively] to chemotherapy and BCL2-938CA, CA+AA and BAX-248GA, AA and GA+AA were associated with poor progression-free survival (PFS) [hazard ratio (HR) 1.514, p = 0.004; HR 1.456, p = 0.009; HR 1.449, p = 0.013; HR 2.006, p = 0.010; HR 1.506, p = 0.003, respectively] and BCL2-938CA, AA and CA+AA and BAX-248GA, AA and GA+AA were associated with poor overall survival (OS) (HR 2.006, p < 0.001; HR 2.322, p < 0.001; HR 2.096, p < 0.001; HR 1.632, p = 0.001; HR 2.014, p = 0.010; HR 1.506, p < 0.001, respectively). Furthermore, combination of these two polymorphisms showed patients with 2–4 variant alleles of these two genes associated with poor PFS and OS (HR 1.637, p = 0.001; HR 2.365, p < 0.001). The data from the current study provide evidence that BCL2-938C>A and BAX-248G>A polymorphisms may be useful in predicting clinical outcomes of patients with advanced inoperable NSCLC to platinum-based chemotherapy.
Similar content being viewed by others
Introduction
Lung cancer is a major cause of cancer-related mortality worldwide1. Histologically, lung cancer is usually classified as small cell or non-small cell lung cancer (NSCLC) and the latter represents up to 85% of all lung cancer cases and frequently is diagnosed at the later stages of disease, preventing curative surgery. Platinum-based chemotherapy is the first line standard treatment for NSCLC patients with advanced disease2; however, such treatment is often associated with poor response due to drug resistance. Chemotherapy resistance of NSCLC to platinum-based treatments is complex, but single-nucleotide polymorphisms (SNP) in apoptosis genes, particularly the BCL2 family, may play a critical role3.
Platinum-based chemotherapeutic agents bind to and cause crosslinking of genomic DNA, especially in fast growing tumor cells and trigger tumor cells to undergo apoptosis4. Apoptosis is a process of programmed cell death that occurs under both physiological and pathological conditions. Apoptosis regulates homeostasis in the human body. The balance of anti-apoptotic and pro-apoptotic proteins determines cell fate and regulates the response to apoptotic signals5,6,7. Deficiency in apoptosis alters intracellular homeostasis and may lead to carcinogenesis and promote tumor progression8. Two well-characterized regulators of apoptosis are the anti-apoptotic B-cell lymphoma 2 (BCL2) and the pro-apoptotic B-cell lymphoma 2-associated X protein (BAX ). BCL2 promotes cell survival by inhibiting apoptosis, whereas BAX promotes apoptosis9,10. Thus, aberrant expression of Bcl-2 and/or BAX is thought to play a role in cancer development. Additionally, SNPs in these genes have been reported to be associated with various human cancers such as head and neck squamous cell carcinoma11, endometrial cancer12, prostate cancer13, breast cancer14, acute lymphoblastic leukemia15 and glioma16. Furthermore, high BCL2 expression has been associated with chemoresistance and overexpression in cell lines has been observed to inhibit apoptosis17,18. Crosstalk occurs between chemotherapy-induced DNA damage and mitochondrial-induced apoptosis19. Previous studies have indicated that BCL2 and BAX SNPs are associated with survival in various types of cancer20,21,22,23,24,25,26. Most studies of BCL2 and BAX SNPs have focused on the promoter regions of these two genes, BCL2-938C>A (rs2279115) and BAX-248G>A(rs4645878), because they have been reported to be associated with altered expression of BCL2 and BAX14,25,27. The BCL2-938C>A A allele was associated with an increase in BCL-2 expression[14,27]. The BAX-248G>A A allele was associated with a decrease in BAX expression25. Hence, in this study, we hypothesized that BCL2 and BAX polymorphisms, located in the untranslated promoter regions, could be associated with treatment responses and clinical outcomes in advanced NSCLC treated with platinum-based chemotherapy. To assess our hypothesis, we analyzed the responses and treatment outcomes of 235 patients with advanced NSCLC treated with platinum-based therapy and the association of treatment response and outcomes with BCL2 -938C>A) (rs2279115) and BAX -248G>A (rs4645878) SNP status.
Material and Methods
Study Population, Response Assessment, Toxicity Evaluation and Survival Calculation
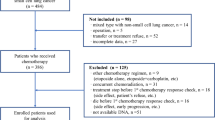
In this study, we enrolled a total of 235 inoperable NSCLC (stage III/IV) patients treated with at least two cycles of first line platinum-based chemotherapy between July 2007 and July 2012 from Daping Hospital, The Third Military Medical University (Chongqing, China). The study was approved by the ethics committee of the Daping Hospital and also carried out according to the protocols approved by the ethics committee. Only patients who understood the purpose of the study and signed the informed consent were included in the study. All patients had routine blood, hepatic and renal function tests and an electrocardiogram. Patients had not received previous chemotherapy or radiotherapy and also had no other malignancies in the 5 years preceding this study. Patients were assessed for their Eastern Cooperative Oncology Group performance status (ECOG PS) and all participants were graded as level 0 ~ 2 before chemotherapy. Patients were treated with 75 mg/m2 cisplatin on day 1 plus 135 mg/m2 Taxol, 75 mg/m2 docetaxel, or 1000 mg/m2 gemcitabine on day 1 and day 8. The therapy cycles were repeated every 3–4 weeks.
Standard Response Evaluation Criteria in Solid Tumors (RECIST 1.0) were used to evaluate the treatment response and the response was assessed by comparison of the baseline MRI or CT images with the follow-up images after every two cycles of chemotherapy. Patients were categorized as responders (complete response and partial response; CR or PR) or nonresponders (stable disease and progressive disease; SD or PD).
Chemotherapy-related toxicities were recorded for each treatment cycle, including leukocytopenia, anemia, thrombocytopenia, nausea, vomiting, diarrhea, neuropathy, weakness, hypersensitivity reaction and renal toxic effects. Grade 3/4 toxicity (defined by the National Cancer Institute common toxicity criteria version 3.0) was assessed twice a week during chemotherapy.Progression-free survival (PFS) was calculated from the start of treatment to documentation of the first date of disease progression (death was considered a progression event in patients who died before disease progression). Overall survival (OS) was calculated from the start of treatment to death. Patients without documented death or objective progression at the time of the final analysis were censored at the time of their last objective tumor assessment or at the date they were last known to be alive. The survival data in this study were censored on July 23, 2014. Ten (4.3%) cases were censored.
Genotyping
A 5 mL whole-blood sample was obtained from each patient before chemotherapy. Genotyping of BCL2-938C>A SNPs and BAX-248G>A was conducted by using the PCR-restriction fragment length polymorphism (PCR-RFLP) method. Each PCR amplification was performed in a 25 μl reaction mixture containing 12.5 pmol of each primer, 2 μl genomic DNA, 0.5 U of TaqMan SNP Genotyping Assay Mix (40x), 0.30 mM of dNTPs, 1.5 mM total MgCl2 and 5 μl of PCR buffer (5×).
The primers used to detect the BCL2-938C>A polymorphism were 5′-CTGCCTTCATTTATCCAGCA-3′ and 5′-GGCGGCAGATGAATTACAA-3′11. The PCR conditions consisted of an initial 96 °C for 5 min, 35 cycles at 96 °C for 45 s, 56 °C for 40 s and 72 °C for 30 s and a final extension at 72 °C for 10 min. The PCR products were then digested by BccI (New England BioLabs, Beverly, MA) overnight at 37 °C. The wild-type allele (CC) produced two bands of 189 and 111 bp; wild-type/variant allele (CA) produced three bands of 111, 189 and 300 bp and the variant allele (AA) produced a single 300 bp band.
The primers for the BAX-248G>A polymorphism were 5′-CGGGGTTATCTCTTGGGC-3′ and 5′-GTGAGAGCCCCGCTGAAC-3′'28. The PCR conditions consisted of an initial denaturation at 95 °C for 5 min, followed by 40 cycles of 30 s at 94 °C, 30 s at 56 °C and 45 s at 72 °C and a final extension at 72 °C for 5 min. The PCR products were then digested by Aci I (Aci I, which recognizes CCGC, New England BioLabs) at 37 °C for 15 min. Homozygous GG alleles (wild-type) were visualized as three major bands of 352, 256 and 96 base pair (bp) with the highest intensity for the 256-bp band under the UV light. In the heterozygous condition (AG alleles) the 256bp and 96 bp products are fainter, while the 352bp band is more intense. In contrast, the homozygous AA alleles (homozygous carrier of this SNP) showed only one 352-bp band.
Statistical Analyses
Statistical analyses were performed using SPSS (IBM SPSS Statistics 19, SPSS, Chicago, IL, USA). Differences in response to treatment or grade 3/4 toxicities were analyzed between groups with different genotypes of these SNPs (variants vs. the wild-type) by calculation of p values using the Pearson χ2 test or the Fisher exact test. Multivariate logistic regression analyses were used to assess associations between the selected SNPs and chemotherapy response or toxicity by estimating odds ratios (ORs) and 95% confidence intervals (CIs). Survival curves for PFS and OS were determined using the Kaplan-Meier method and the Log-rank test was used to generate p values. Multivariate Cox proportional hazards models (Forward Stepwise: Likelihood Ratio) were used to estimate adjusted hazard ratios (HR) with 95% confidence intervals. Multivariable regressions analysis was adjusted for age, gender, ECOG stage, histology, disease stage, smoking status, weight loss and chemotherapy regimens. Two-sided p-values of less than 0.05 were considered statistically significant. In order to adjust the p-value due to multiple comparisons, the Bonferroni-Holm method was used to calculate the p-value for the results of any SNP.
Results
Patient characteristics
Patients’ characteristics and genotypic data are shown in Table 1. In brief, all patients were Chinese with 180 (76.6%) males and 55 (23.4%) females and a median age of 58 years old (range between 29 and 84 years old). Histologically, 133 of these 235 patients were adenocarcinoma, while 78 were squamous cell carcinoma and 24 were other types of NSCLC; 43 (18.3%) patients had clinical stage IIIA disease, 38 (16.2%) stage IIIB and 154 (65.5%) stage IV disease. Furthermore, 124 (52.8%) patients had ECOG PS 0 and 111 (47.2%) patients had ECOG PS ≥ 1 and 91 (38.7%) never smoked tobacco and 76 (32.3%) patients had weight loss before chemotherapy. BCL2-938C>G, 88 (37.4%) patients were CC genotype, 104 (44.3%) were CG genotype and 43 (18.3%) were GG genotype. BAX-248G>A, 129 (54.9%) patients were GG genotype, 87 (37.0%) were GA genotype and 19 (8.1%) were AA genotype. A significant association was found with histology (p = 0.005) between the BCL2–938C>A genotype and clinicopathologic factors (Table 2).
For chemotherapy, 180 (76.6%) patients received TP regimens (Taxol/docetaxel plus cisplatin), 32 (13.6%) had GP regimens (gemcitabine plus cisplatin) and 23 (9.80%) had other platinum combinations (vinorelbine plus cisplatin or pemetrexed plus cisplatin). The median number of chemotherapy cycles was four (range between 2 and 8).
Association of Genotypes with Treatment Response and Toxicity
The overall response rate of patients to platinum-based chemotherapy was 35.7% with the following responses to the first-line treatments: one patient had CR (0.4% of evaluable patients), 83 PR (35.32%), 75 SD (31.9%) and 76 PD (32.3%). A numerically increased rate of response was observed in patients with the BAX-248GG vs. the GA or GA+AA phenotype but the differences did not reach statistical significance after multiplicity adjustment (42.6% vs. 27.6%, p = 0.024; 42.6% vs. 27.4%, p = 0.015). No statistically significant association was observed between BCL2-938C>A and responses to chemotherapy (Table 3). After adjusting for age, gender, ECOG PS, histology, tumor stage, smoking status, chemotherapy regimens, weight loss, BCL2-938C>A and BAX-248G>A, the logistic regression model analysis showed that the following parameters were able to predict the treatment response: ECOG PS (adjusted OR 2.112, 95% CI 1.156–3.857, p = 0.015), tumor stage (adjusted OR 2.887, 95% CI 1.510–5.518, p = 0.001), smoking status (adjusted OR 2.446, 95% CI 1.140–5.247, p = 0.022) and BAX-248G>A (GG vs. GA, adjusted OR 1.943, 95% CI 1.035–3.648, p = 0.039; GG vs. GA+AA, adjusted OR 1.867, 95% CI 1.035–3.369, p = 0.038).
The incidence of grade 3/4 toxicity was 57.5%. In particular, 90 patients (38.3%) had grade 3/4 hematologic toxicity, 44 patients (18.7%) had grade 3/4 gastrointestinal toxicity, 27 patients (11.49%) had both and 127 patients (54.04%) had neither hematologic toxicity nor gastrointestinal toxicity. Our SNP data showed that there was no significant association between risk of grade 3/4 hematologic toxicity or gastrointestinal toxicity and BCL2-938C>A (adjusted OR 1.006, 95% CI 0.680 ~ 1.490, p = 0.975; adjusted OR 0.927, 95% CI 0.572 ~ 1.500, p = 0.756) or BAX-248G>A (adjusted OR 0.726, 95% CI 0.464 ~ 1.490, p = 0.160; adjusted OR 0.976, 95% CI 0.576 ~ 1.655, p = 0.929) polymorphisms (Logistic regression model analysis). However, chemotherapeutic regimens (TP vs. GP, adjusted OR 2.566, 95% CI 1.154 ~ 5.706, p = 0.021) and age (adjusted OR 1.802, 95% CI 1.030 ~ 3.152, p = 0.039) were associated with the risk of hematologic toxicity (Logistic regression model analysis).
Association of Genotypes with PFS and OS of these patients after chemotherapy
The median follow-up time was 22 months (range between 1.8 and 70.4 months) and 214 (91.06%) patients died during the follow-up. The one-year survival rate was 60% and the 2-year survival rate was 25%. The median PFS was 7.0 months (95% CI, 6.058–7.942). The median OS was 15.0 months (95% CI, 12.981–17.019).
In univariate analysis, patients with BCL2-938AA, CA or CA+AA genotype had significantly shorter median PFS compared with those with −938CC genotype [9 m vs. 5 m, p = 0.035 (the difference did not reach statistical significance after multiplicity adjustment); 9 m vs. 6 m, p = 0.004; 9 m vs. 6 m, p = 0.003; Log-rank test; respectively; Fig. 1a,c. tif]. The median PFS of patients with the BAX-248GG genotype was significantly longer than those with the -248GA, AA or GA+AA genotype [8 m vs. 6 m, p = 0.018; 8 m vs. 5 m, p = 0.010; 8 m vs. 6 m, p = 0.004 (significance remained after the Bonferroni–Holm method); Log-rank test; respectively; Fig. 1e,g. tif]. The multivariate analysis showed that age (HR 0.638, 95% CI 0.480–0.846, p = 0.002), ECOG PS (HR 1.906, 95% CI 1.432–2.537, p < 0.001), BCL2–938C>A (CC vs. CA, HR 1.570, 95% CI 1.152–2.140, p = 0.004; CC vs. CA+AA, HR 1.456,95% CI 1.099–1.929, p = 0.009) and BAX–248G>A (GG vs. GA, HR 1.449, 95% CI 1.080–1.945, p = 0.013; GG vs. AA, HR 2.006, 95% CI 1.184–3.399, p = 0.010; GG vs. GA+AA, HR 1.506, 95% CI 1.145–1.980, p = 0.003) were all significant prognostic indictors for PFS (Table 4).
Furthermore, in the univariate model (Table 4), the BCL2-938C>A polymorphism was significantly associated with OS, i.e., patients carrying the CC genotype had a longer median OS than patients carrying the CA, AA or CA+AA genotype (19 m vs. 12 m, p < 0.001; 19 m vs. 11 m, p < 0.001; 19 m vs. 12 m, p < 0.001; Log-rank test; respectively; Fig. 1b,d. tif). The median survival time of patients with BAX-248GG genotypes was significantly longer than those with the -248GA, AA or GA+AA genotype (17 m vs. 12 m, p = 0.001; 17 m vs. 12 m, p = 0.005; 17 m vs. 12 m, p < 0.001; Log-rank test; respectively; Fig. 1f,h. tif). The multivariate analysis showed that ECOG PS (HR 2.430, 95% CI 1.823–3.238, p < 0.001), BCL2-938C>A (CC vs. CA, HR 2.006, 95% CI 1.462–2.752, p < 0.001; CC vs. AA, HR 2.322, 95% CI 1.558–3.461, p < 0.001; CC vs. CA+AA, HR 2.096, 95% CI 1.555–2.824; p < 0.001) and BAX-248G>A (GG vs. GA, HR 1.632, 95% CI 1.210–2.199, p = 0.001; GG vs. AA, HR 2.014, 95% CI 1.188–3.425, p = 0.010; GG vs. GA+AA, HR 1.705, 95% CI 1.283–2.266, p < 0.001) were all independent predictors for OS of these NSCLC patients.
After that, we combined these two BCL2-938C>A and BAX-248G>A polymorphisms for association with PFS and OS of patients. Our data showed that the -938A and -248A were classified as adverse alleles based on association with higher risk of progression and death presented in Table 4 and as the number of adverse allele increased, the median PFS and OS decreased. Patients with more than 2 adverse alleles had shorter median PFS (5 m vs. 8 m, p = 0.001) and OS (12 m vs. 18 m, p < 0.001) compared to those with 0–1 adverse alleles (Table 4, Fig. 2. tif). The multivariate analysis showed that patients with 2–4 adverse alleles had an increased risk of disease progression (HR 1.637, 95% CI 1.240 ~ 2.161, p = 0.001) and death (HR 2.365, 95% CI 1.760–3.178, p < 0.001). These significances remained after the Bonferroni-Holm method analysis.
Discussion
Cisplatin resistance occurs through a variety of mechanisms, such as changes in cellular uptake and efflux of the drug, increased expression of detoxification enzymes, increased DNA repair or inhibition of apoptosis29. In this study, we investigated whether the occurrence of SNPs, located in the promoter regions of two apoptosis-related genes are associated with responses and/or outcomes in patients with advanced NSCLC that are treated with cisplatin-based chemotherapy. A numerically increased rate of response was observed in patients with the BAX-248GG vs. the GA or GA+AA phenotype but the difference did not reach statistical significance after multiplicity adjustment. We found no significant association between the BCL2-938C>A polymorphism and chemotherapy response. There was no statistical association between BCL2-938C/A or BAX-248G>A polymorphism and grade 3/4 hematologic or gastrointestinal toxicity in these patients. Furthermore, patients with the BCL2-938C>A variant genotype (A allele) or BAX-248G>A variant genotype (A allele) associated with poor PFS and OS. The combined BCL2-938C>A and BAX-248G>A were also associated with PFS and OS of the patients. The multivariate analysis showed that ECOG PS, BCL2-938C>A and BAX-248G>A were all independent predictors for OS of these NSCLC patients. To the best of our knowledge, this is the first study of this kind to demonstrate an association between the BAX-248G>A or the combination of BCL2-938C>A and BAX-248G>A with outcome of advanced NSCLC patients to cisplatin-based chemotherapy.
BCL2 is localized to chromosome 18q21.330, coding a protein with three exons and two gene promoters (P1 and P2). These two promoters have different functions in regulation of BCL2 expression, i.e., the P2 promoter is localized to the translation initiation site and functions as a negative regulatory element of the P1 promoter31,32. Park et al.33 identified BCL2-938C>A(rs2279115) in P2 and Nückel et al.27 found that the -938C allele of BCL2-938C>A displayed a significant increase in BCL2 promoter activity. Concomitantly, expression of BCL2 protein in B-lymphocytes from chronic lymphocytic leukemia patients carrying the -938 AA genotype was significantly increased compared with CC genotypes. This has been confirmed by other studies of prostate cancer34, renal cancer24, oropharyngeal squamous cell carcinoma35 and breast cancer36, although Zhang et al.14 have an opposite result showing that the −938A allele contributed to decreased expression of the BCL2 protein in breast cancer cell lines. Furthermore, previous studies showed that the BCL2-938 A variant was associated with a decreased risk of head and neck squamous cell carcinoma11 and prostate cancer13, but increased risk of breast cancer14 and glioma16. The –938 AA genotype was independently associated with worse PFS and OS of prostate cancer34, chronic lymphocytic leukemia27, glioblastoma multiforme21 and NSCLC20, whereas it associated with a better prognosis of lymph node-negative invasive breast cancer36, oropharyngeal squamous cell carcinoma35, renal cancer24, ovarian cancer37 and limited-disease small cell lung cancer38. In our current study, we found that the BCL2-938 A variant was associated with poor PFS and OS of patients with advanced NSCLC after chemotherapy, which supports previous data reported by Katsuhiro Masago and colleagues of 168 advanced NSCLC patients who received platinum-based chemotherapy20. Expression of the anti-apoptotic BCL2 protein should contribute to resistance to cisplatin-induced tumor cell apoptosis and thus lead to a poor response and outcome. Indeed, BCL2 overexpression has been shown to be a marker of chemotherapy resistance in both SCLC and NSCLC39,40. However, Fontanini et al.41 reported that survival probability was higher in patients with BCL2-expressing, resected NSCLC because of the less aggressive behavior of NSCLC with BCL2 overexpression. A meta-analysis of 28 studies revealed that BCL2 overexpression had a positive influence on survival of NSCLC42. However, further study is needed to clarify this discrepancy.
BAX is localized to chromosome 19q13.3, coding a protein with six exons and a promoter43. The BAX promoter binds to different transcription factors or proteins, such as p53 response elements, the TATA box, canonical E-boxes and the NF-κB binding site to regulate BAX expression44. BAX was extensively studied in different types of cancer such as pancreatic cancer45, colon cancer46,47, esophageal cancer48, lung cancer49,50, squamous cell carcinoma of the head and neck11, prostate carcinoma51, ovarian carcinoma52 and breast cancer53. Recently, BAX-248G>A (rs4645878) was reported to be associated with reduced expression of BAX protein and altered susceptibility to chronic lymphocytic leukemia25,26, although a meta-analysis of seven independent studies with 1772 cases and 1708 controls revealed that neither allele frequency nor genotype of BAX-248G>A associated with risk of human cancer using different genetic models54. Several studies reported that patients with BAX low expression had a significantly longer median survival in NSCLC50, esophageal squamous cell carcinoma48 and colon cancer47. Moreover, Paola Perego et al.55 showed that p53 mutations developed cisplatin resistance in ovarian cancer as a consequence of the loss of p53 transactivation of BAX expression. Our current SNP data further confirm the role of BAX in the regulation of cisplatin resistance and shorter PFS and OS of patients with advanced NSCLC.
Indeed, previous studies showed that BAX was able to heterodimerize with BCL2 and Mcl-1 and that overexpression of BCL2 and Mcl-1 proteins compromised the proapoptotic capacity of BAX56,57. Therefore, we determined to assess whether BCL2 and BAX interact synergistically to contribute to cisplatin resistance and alter the PFS and OS of patients with advanced NSCLC. We found that as the number of variant alleles increased, the median PFS and OS were decreased accordingly. Patients with more than 2 variant alleles had a much shorter median PFS and OS compared to those carrying 0–1 variant alleles.
Our current study is just the first of this kind for proof-of-principle. Although we showed that the BCL2-938C>A and BAX-248G>A SNPs significantly associated with platinum-based chemotherapy response, PFS and OS of patients with advanced NSCLC, we did not show the association of these SNPs with chemotherapy-related toxicities. However, the mechanism by which BCL2 SNPs may influence the clinical outcomes of patients with advanced NSCLC to platinum-based chemotherapy is unclear. This raises the question of whether a patient with such polymorphisms would have better survival than those without these polymorphisms in the absence of treatment. Do the polymorphisms actually affect the effectiveness of the regimen, or do they simply afford a better prognosis to patients? Hence, further work is necessary; for example, a larger sample size and a prospective study would be able to confirm our current data. Variation of BCL2 and BAX expression associates with an altered sensitivity and clinical outcome of NSCLC patients to chemotherapy.
Additional Information
How to cite this article: Peng, Y. et al. Polymorphisms of BCL2 and BAX Genes Associate with Outcomes in Advanced Non-small cell lung cancer Patients treated with platinum-based Chemotherapy. Sci. Rep. 5, 17766; doi: 10.1038/srep17766 (2015).
References
Jemal, A. et al. Global cancer statistics. CA: a cancer journal for clinicians 61, 69–90, doi: 10.3322/caac.20107 (2011).
Schiller, J. H. et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. The New England journal of medicine 346, 92–98, doi: 10.1056/NEJMoa011954 (2002).
Lindner, A. U. et al. Systems analysis of BCL2 protein family interactions establishes a model to predict responses to chemotherapy. Cancer research 73, 519–528, doi: 10.1158/0008-5472.CAN-12-2269 (2013).
Gonzalez, V. M., Fuertes, M. A., Alonso, C. & Perez, J. M. Is cisplatin-induced cell death always produced by apoptosis? Molecular pharmacology 59, 657–663 (2001).
Adams, J. M. & Cory, S. The Bcl-2 protein family: arbiters of cell survival. Science 281, 1322–1326 (1998).
Kroemer, G. Mitochondrial implication in apoptosis. Towards an endosymbiont hypothesis of apoptosis evolution. Cell death and differentiation 4, 443–456, doi: 10.1038/sj.cdd.4400266 (1997).
Oltvai, Z. N., Milliman, C. L. & Korsmeyer, S. J. Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell 74, 609–619 (1993).
Tang, D. G. & Porter, A. T. Target to apoptosis: a hopeful weapon for prostate cancer. The Prostate 32, 284–293 (1997).
Bukholm, I. K. & Nesland, J. M. Protein expression of p53, p21 (WAF1/CIP1), bcl-2, Bax, cyclin D1 and pRb in human colon carcinomas. Virchows Archiv: an international journal of pathology 436, 224–228 (2000).
Linjawi, A., Kontogiannea, M., Halwani, F., Edwardes, M. & Meterissian, S. Prognostic significance of p53, bcl-2 and Bax expression in early breast cancer. Journal of the American College of Surgeons 198, 83–90, doi: 10.1016/j.jamcollsurg.2003.08.008 (2004).
Chen, K. et al. Single-nucleotide polymorphisms at the TP53-binding or responsive promoter regions of BAX and BCL2 genes and risk of squamous cell carcinoma of the head and neck. Carcinogenesis 28, 2008–2012, doi: 10.1093/carcin/bgm172 (2007).
Dorjgochoo, T. et al. Association of genetic markers in the BCL-2 family of apoptosis-related genes with endometrial cancer risk in a Chinese population. PloS one 8, e60915, doi: 10.1371/journal.pone.0060915 (2013).
Hirata, H. et al. Bcl2 -938C/A polymorphism carries increased risk of biochemical recurrence after radical prostatectomy. The Journal of urology 181, 1907–1912, doi: 10.1016/j.juro.2008.11.093 (2009).
Zhang, N. et al. BCL-2 (-938C > A) polymorphism is associated with breast cancer susceptibility. BMC medical genetics 12, 48, doi: 10.1186/1471-2350-12-48 (2011).
Kunkele, A. et al. The BCL2-938 C > A promoter polymorphism is associated with risk group classification in children with acute lymphoblastic leukemia. BMC cancer 13, 452, doi: 10.1186/1471-2407-13-452 (2013).
Li, W., Qian, C., Wang, L., Teng, H. & Zhang, L. Association of BCL2-938C>A genetic polymorphism with glioma risk in Chinese Han population. Tumour biology: the journal of the International Society for Oncodevelopmental Biology and Medicine 35, 2259–2264, doi: 10.1007/s13277-013-1299-5 (2014).
Rodriguez-Nieto, S. & Zhivotovsky, B. Role of alterations in the apoptotic machinery in sensitivity of cancer cells to treatment. Current pharmaceutical design 12, 4411–4425 (2006).
Kaufmann, S. H. & Vaux, D. L. Alterations in the apoptotic machinery and their potential role in anticancer drug resistance. Oncogene 22, 7414–7430, doi: 10.1038/sj.onc.1206945 (2003).
Galluzzi, L. et al. Independent transcriptional reprogramming and apoptosis induction by cisplatin. Cell cycle 11, 3472–3480, doi: 10.4161/cc.21789 (2012).
Masago, K. et al. Effect of the BCL2 gene polymorphism on survival in advanced-stage non-small cell lung cancer patients who received chemotherapy. Oncology 84, 214–218, doi: 10.1159/000342854 (2013).
El Hindy, N. et al. Association of the CC genotype of the regulatory BCL2 promoter polymorphism (-938C>A) with better 2-year survival in patients with glioblastoma multiforme. Journal of neurosurgery 114, 1631–1639, doi: 10.3171/2010.12.JNS10478 (2011).
Moon, J. H. et al. BCL2 gene polymorphism could predict the treatment outcomes in acute myeloid leukemia patients. Leukemia research 34, 166–172, doi: 10.1016/j.leukres.2009.05.009 (2010).
Zenz, T. et al. BCL2-938C>A polymorphism and disease progression in chronic lymphocytic leukemia. Leukemia & lymphoma 50, 1837–1842, doi: 10.3109/10428190903207530 (2009).
Hirata, H. et al. The bcl2 -938CC genotype has poor prognosis and lower survival in renal cancer. The Journal of urology 182, 721–727, doi: 10.1016/j.juro.2009.03.081 (2009).
Starczynski, J. et al. Common polymorphism G(-248)A in the promoter region of the bax gene results in significantly shorter survival in patients with chronic lymphocytic Leukemia once treatment is initiated. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 23, 1514–1521, doi: 10.1200/JCO.2005.02.192 (2005).
Saxena, A., Moshynska, O., Sankaran, K., Viswanathan, S. & Sheridan, D. P. Association of a novel single nucleotide polymorphism, G(-248)A, in the 5’-UTR of BAX gene in chronic lymphocytic leukemia with disease progression and treatment resistance. Cancer letters 187, 199–205 (2002).
Nuckel, H. et al. Association of a novel regulatory polymorphism (-938C>A) in the BCL2 gene promoter with disease progression and survival in chronic lymphocytic leukemia. Blood 109, 290–297, doi: 10.1182/blood-2006-03-007567 (2007).
Ocana, M. G. et al. Bax gene G(-248)A promoter polymorphism is associated with increased lifespan of the neutrophils of patients with osteomyelitis. Genetics in medicine: official journal of the American College of Medical Genetics 9, 249–255, doi: 10.1097GIM.0b013e318039b23d (2007).
Stordal, B. & Davey, M. Understanding cisplatin resistance using cellular models. IUBMB life 59, 696–699, doi: 10.1080/15216540701636287 (2007).
Tsujimoto, Y., Gorham, J., Cossman, J., Jaffe, E. & Croce, C. M. The t(14;18) chromosome translocations involved in B-cell neoplasms result from mistakes in VDJ joining. Science 229, 1390–1393 (1985).
Seto, M. et al. Alternative promoters and exons, somatic mutation and deregulation of the Bcl-2-Ig fusion gene in lymphoma. The EMBO journal 7, 123–131 (1988).
Young, R. L. & Korsmeyer, S. J. A negative regulatory element in the bcl-2 5’-untranslated region inhibits expression from an upstream promoter. Molecular and cellular biology 13, 3686–3697 (1993).
Park, B. L. et al. Identification of variants in cyclin D1 (CCND1) and B-Cell CLL/lymphoma 2 (BCL2). Journal of human genetics 49, 449–454, doi: 10.1007/s10038-004-0173-0 (2004).
Bachmann, H. S. et al. Regulatory BCL2 promoter polymorphism (-938C>A) is associated with adverse outcome in patients with prostate carcinoma. International journal of cancer. Journal international du cancer 129, 2390–2399, doi: 10.1002/ijc.25904 (2011).
Lehnerdt, G. F. et al. The regulatory BCL2 promoter polymorphism (-938C>A) is associated with relapse and survival of patients with oropharyngeal squamous cell carcinoma. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 20, 1094–1099, doi: 10.1093/annonc/mdn763 (2009).
Bachmann, H. S. et al. The AA genotype of the regulatory BCL2 promoter polymorphism (938C>A) is associated with a favorable outcome in lymph node negative invasive breast cancer patients. Clinical cancer research: an official journal of the American Association for Cancer Research 13, 5790–5797, doi: 10.1158/1078-0432.CCR-06-2673 (2007).
Heubner, M. et al. Association of the AA genotype of the BCL2 (-938C>A) promoter polymorphism with better survival in ovarian cancer. The International journal of biological markers 24, 223–229 (2009).
Knoefel, L. F. et al. Polymorphisms in the apoptotic pathway gene BCL-2 and survival in small cell lung cancer. Journal of thoracic oncology: official publication of the International Association for the Study of Lung Cancer 6, 183–189, doi: 10.1097/JTO.0b013e3181f8a20e (2011).
Sartorius, U. A. & Krammer, P. H. Upregulation of Bcl-2 is involved in the mediation of chemotherapy resistance in human small cell lung cancer cell lines. International journal of cancer. Journal international du cancer 97, 584–592 (2002).
Han, J. Y. et al. Death receptor 5 and Bcl-2 protein expression as predictors of tumor response to gemcitabine and cisplatin in patients with advanced non-small-cell lung cancer. Medical oncology 20, 355–362, doi: 10.1385/MO:20:4:355 (2003).
Fontanini, G. et al. Bcl2 and p53 regulate vascular endothelial growth factor (VEGF)-mediated angiogenesis in non-small cell lung carcinoma. European journal of cancer 34, 718–723 (1998).
Martin, B. et al. Role of Bcl-2 as a prognostic factor for survival in lung cancer: a systematic review of the literature with meta-analysis. British journal of cancer 89, 55–64, doi: 10.1038/sj.bjc.6601095 (2003).
Chou, D. et al. The BAX gene maps to the glioma candidate region at 19q13.3, but is not altered in human gliomas. Cancer genetics and cytogenetics 88, 136–140 (1996).
Saxena, A., McMeekin, J. D. & Thomson, D. J. Expression of Bcl-x, Bcl-2, Bax and Bak in endarterectomy and atherectomy specimens. The Journal of pathology 196, 335–342, doi: 10.1002/path.1040 (2002).
Pirocanac, E. C. et al. Bax-induction gene therapy of pancreatic cancer. The Journal of surgical research 106, 346–351 (2002).
Miquel, C. et al. Role of bax mutations in apoptosis in colorectal cancers with microsatellite instability. American journal of clinical pathology 123, 562–570, doi: 10.1309/JQ2X-3RV3-L8F9-TGYW (2005).
Sturm, I. et al. Analysis of the p53/BAX pathway in colorectal cancer: low BAX is a negative prognostic factor in patients with resected liver metastases. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 17, 1364–1374 (1999).
Kang, S. Y. et al. Low expression of Bax predicts poor prognosis in patients with locally advanced esophageal cancer treated with definitive chemoradiotherapy. Clinical cancer research: an official journal of the American Association for Cancer Research 13, 4146–4153, doi: 10.1158/1078-0432.CCR-06-3063 (2007).
Porebska, I. et al. Apoptotic markers p53, Bcl-2 and Bax in primary lung cancer. In vivo 20, 599–604 (2006).
Jeong, S. H. et al. Low expression of Bax predicts poor prognosis in resected non-small cell lung cancer patients with non-squamous histology. Japanese journal of clinical oncology 38, 661–669, doi: 10.1093/jjco/hyn089 (2008).
Anvari, K. et al. Expression of Bcl-2 and Bax in advanced or metastatic prostate carcinoma. Urology journal 9, 381–388 (2012).
Yigit, S. et al. The clinicopathological significance of Bax and Bcl-2 protein expression with tumor infiltrating lymphocytes in ovarian carcinoma. Neoplasma 59, 475–485, doi: 10.4149/neo_2012_061 (2012).
Lopes-Costa, P. V., dos Santos, A. R. & da Silva, B. B. The effect of raloxifene on Bax protein expression in breast carcinomas of postmenopausal women. Diagnostic cytopathology 40, 570–574, doi: 10.1002/dc.21580 (2012).
Sahu, S. K. & Choudhuri, T. Lack of association between Bax promoter (-248G>A) single nucleotide polymorphism and susceptibility towards cancer: evidence from a meta-analysis. PloS one 8, e77534, doi: 10.1371/journal.pone.0077534 (2013).
Perego, P. et al. Association between cisplatin resistance and mutation of p53 gene and reduced bax expression in ovarian carcinoma cell systems. Cancer research 56, 556–562 (1996).
Zha, H., Aime-Sempe, C., Sato, T. & Reed, J. C. Proapoptotic protein Bax heterodimerizes with Bcl-2 and homodimerizes with Bax via a novel domain (BH3) distinct from BH1 and BH2. The Journal of biological chemistry 271, 7440–7444 (1996).
Bodrug, S. E. et al. Biochemical and functional comparisons of Mcl-1 and Bcl-2 proteins: evidence for a novel mechanism of regulating Bcl-2 family protein function. Cell death and differentiation 2, 173–182 (1995).
Acknowledgements
This study was supported by a grant from the National Natural Science Foundation of China (NO. 81171904).
Author information
Authors and Affiliations
Contributions
Y.P. and L.W. contributed to the design of the study, genetic analysis, collection and analysis of data and writing of the main manuscript. Y.Q., M.L. and J.S. made constructive proposals to the arrangement of the work. S.Z. carried out statistical analysis and revised the manuscript. T.R. prepared all figures. C.L. and Q.L. searched the related papers. Z.Y., G.W. and D.W. designed this study and revised the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Peng, Y., Wang, L., Qing, Y. et al. Polymorphisms of BCL2 and BAX Genes Associate with Outcomes in Advanced Non-small cell lung cancer Patients treated with platinum-based Chemotherapy. Sci Rep 5, 17766 (2015). https://doi.org/10.1038/srep17766
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep17766
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.