Abstract
After the accident at the Fukushima Daiichi Nuclear Power Plant, the thyroid ultrasound screening program for children aged 0–18 at the time of the accident was started from October 2011. The prevalence of thyroid carcinomas in that population has appeared to be very high (84 cases per 296,253). To clarify the pathogenesis, we investigated the presence of driver mutations in these tumours. 61 classic papillary thyroid carcinomas (PTCs), two follicular variant PTCs, four cribriform-morular variant PTCs and one poorly-differentiated thyroid carcinoma were analysed. We detected BRAFV600E in 43 cases (63.2%), RET/PTC1 in six (8.8%), RET/PTC3 in one (1.5%) and ETV6/NTRK3 in four (5.9%). Among classic and follicular variant PTCs, BRAFV600E was significantly associated with the smaller size. The genetic pattern was completely different from post-Chernobyl PTCs, suggesting non-radiogenic etiology of these cancers. This is the first study demonstrating the oncogene profile in the thyroid cancers discovered by large mass screening, which probably reflects genetic status of all sporadic and latent tumours in the young Japanese population. It is assumed that BRAFV600E may not confer growth advantage on paediatric PTCs and many of these cases grow slowly, suggesting that additional factors may be important for tumour progression in paediatric PTCs.
Similar content being viewed by others
Introduction
After the accident at the Fukushima Daiichi Nuclear Power Plant due to the Great East Japan Earthquake occurred on March 11th, 2011, there have been great concerns regarding a possible health impact by radioactive materials released into the environment. Fukushima prefecture, therefore, started the Fukushima Health Management Survey for long-term health management1,2. This survey includes the thyroid ultrasound screening program for all children aged 0–18 years old at the time of the accident. After the Chernobyl accident, internal exposure to radioactive iodine induced a massive increase in childhood thyroid cancers in Belarus, Ukraine and Russia3,4,5,6. This increase started to appear 4–5 years after the accident. Therefore, the first round of the screening program, so-called the baseline survey, was started in October, 2011 to grasp the general ultrasound findings in children and adolescents, because such a screening program for a huge number of young individuals using advanced ultrasound technologies has never been done. After the first round of the screening, the prevalence of thyroid cancers in Fukushima appeared to be quite high: 84 per 296,253 children as of October 2014 (http://www.fmu.ac.jp/radiationhealth/results/media/17-2_Thyroid_Ultrasound_Examination_I-S.pdf). Most of them were papillary thyroid carcinomas (PTCs). Logically, this increase has been thought to be due to screening effect with advances in diagnostic instruments in recent years, because the estimated thyroid doses of radioiodine exposure in Fukushima were far lower than those in Chernobyl7,8,9 and the period from the date of the accident until the onset is too short. Presumably, a real morbidity rate may be comparable throughout Japan10,11 and many of the PTC cases could be silent or very slowly progressing until middle or older age.
PTCs have particular genetic alterations such as RET/PTC rearrangements and point mutations in the BRAF and RAS family genes resulting in activation of the mitogen-activated protein kinase (MAPK) pathway12,13. There are more than 15 different types of RET/PTC chimeric genes that differ according to the 5’ partner gene involved in the rearrangement. RET/PTC1 and RET/PTC3 are the most common types, accounting for more than 90% of all the rearrangements. These oncogenes rarely overlap in a same tumour, providing strong genetic evidence for the requirement of constitutive active MAPK signaling for the development of PTC. In adult sporadic PTCs, the BRAFV600E mutation is the most prevalent genetic alteration ranging approximately 30–70%14,15,16,17,18. On the other hand, the RET/PTC rearrangements have been reported to be dominant in childhood sporadic PTCs19,20. Regarding radiation-induced thyroid carcinomas, post-Chernobyl PTCs also had higher prevalence of the RET/PTC rearrangements. Especially, in cases with short latency (developed less than 7–10 years after the accident), they were found in 64–86% of the tumours and RET/PTC3 was the most frequent type of the rearrangement in this group5. Consequently, the pattern of genetic alterations in PTCs depends on patient age and etiology of the tumours.
In the present study, we investigated the presence of various known genetic alterations in 68 operated cases discovered in Fukushima. First, we aimed to assess whether their genetic pattern is similar to that of post-Chernobyl PTCs, even though these Fukushima cases are very unlikely to be radiation-induced. Second, we also attempted to gain insight into the carcinogenic mechanisms of the thyroid cancers found by the large mass screening program in the young population in Fukushima.
Results
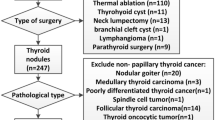
The profile of the genetic alterations
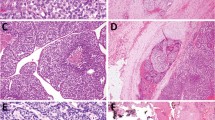
We obtained tissue samples from 68 patients operated at Fukushima Medical University, consisting of 61 classical PTCs, two follicular variant PTCs, four cribriform-morular variant PTCs and one poorly differentiated thyroid carcinoma (PDTC). We first screened them for BRAF (exon 15), HRAS, KRAS and NRAS (codons 12, 13 and 61) and RET/PTC1 and RET/PTC3. In samples without above-mentioned frequent known genetic alterations, we next investigated the presence of AKAP9/BRAF and ETV6(exons 4 and 5)/NTRK3 rearrangements. The mutation in the TERT promoter (C250T and C228T) was checked in all samples. The clinicopathological features and genotyping results are summarized in Table 1 and 2, respectively. We found these known oncogenes in 54 out of 68 (79.4%) samples. The BRAFV600E mutation was highly prevalent and found in 43 out of 68 (63.2%). Note that four cases showed the weak signal of a mutant allele: the intensity of A signal in the sequence chromatogram was less than 20% compared to that of T signal (Table 1). In these tumours, the BRAFV600E mutation may not be clonal. None of samples had the RAS mutation nor the TERT promoter mutation. Regarding the fusion genes, six RET/PTC1, one RET/PTC3 and four ETV6(ex.4)/NTRK3 were detected. AKAP9/BRAF and ETV6(ex.5)/NTRK3 were not found. In one PDTC, we did not find any of the above genetic alterations. The four cases with cribriform-morular variant PTCs are highly suspected to be familial adenomatous polyposis; the analyses of the APC gene/genetic counseling are being conducted and their results will be published elsewhere.
Clinicopathological correlations
We compared clinicopathological parameters between the BRAFV600E mutation-positive PTC cases and the BRAFV600E-negative PTCs including the fusion gene-positive and mutation-negative cases, excluding cribriform-morular PTCs. As shown in Table 3, the BRAFV600E mutation was significantly associated with smaller tumour size (12.2 ± 6.8 mm in the BRAFV600E-positive PTCs vs. 18.3 ± 9.5 mm in the BRAFV600E-negative PTCs) but not with the TNM parameters and extrathyroidal extension in univariate analysis. On multivariate analysis adjusted for age and sex, tumour size in BRAFV600E-positive cases was still significantly smaller than that in the negative cases (Table 3) and also an association with older patients’ age was detected after adjustment for sex (Table 3).
Discussion
In the present study, we have demonstrated that high prevalence of the BRAFV600E mutation and low frequency of chromosomal rearrangements such as RET/PTC in young PTC cases were found by the screening program. There are not so many publications about the BRAF mutation in paediatric thyroid carcinomas. In the early period (2004–2005) after the discovery of the BRAF mutation in thyroid cancers, its prevalence in paediatric PTCs was reported to be 0–20%21,22,23,24. However, two very recent papers published in 2014 demonstrated much higher prevalence (63 and 36.8%, respectively), especially in tumours with classic papillary subtype (71.4 and 63.6%, respectively)25,26. We cannot explain this discrepancy although all of these studies analysed a limited number of cases. One possibility is that this increase may be due to improved sensitivity of detection methods: PCR-restriction fragment length polymorphism (RFLP) and pyrosequencing were used in the recent studies. As the histological classification of most of our Fukushima cases was classic papillary subtype, our data are consistent with the recent studies. The prevalence of the BRAFV600E mutation depends on population and iodine intake27. In East Asian countries such as South Korea and Japan where iodine intake is very high, PTCs usually show very high rate of the BRAFV600E mutation. Our cases in Fukushima demonstrated a similar rate. In terms of the BRAF mutation in radiation-induced paediatric thyroid carcinomas including post-Chernobyl PTCs, its prevalence was reported to be low (0–17%)5,21,28. Furthermore, point mutations have been shown to display negative dose-response relationship in thyroid cancers in Chernobyl29 and in A-bomb survivors30. These observations are suggestive of non-radiogenic etiology of the thyroid cancers in Fukushima.
In the post-Chernobyl paediatric PTCs, the RET/PTC rearrangements were usually detected in more than 50%. RET/PTC3 was the most common type in tumours with short latency (4–8 years after the exposure), whereas tumours developed after longer period of time had RET/PTC1 predominantly. In addition, RET/PTC3 had a strong correlation with solid variant subtype, while RET/PTC1 usually found in classic papillary subtype5. Ricarte-Filho et al.31 reported the results of analysis of driver mutations in post-Chernobyl radiation-exposed PTCs that showed a similar age range to our series (radiation-exposed, median: 17.8 years old, range: 13.4–23.0; Fukushima, median: 18.0 years old, range: 9–22). In this report, the prevalence of the RET/PTC rearrangements in the radiation-exposed cases was 57.7%. The detected rate of the RET/PTC rearrangements in our series was only 10.3%, all of which were RET/PTC1 except one RET/PTC3, also suggesting that the mode of carcinogenesis in the Fukushima cases is different from post-Chernobyl PTCs.
The prevalence of the RET/PTC rearrangements in sporadic paediatric PTCs was reported to be also high (30–67%)5,19. In the above paper by Ricarte-Filho et al.31, sporadic PTCs, most of which were teenagers (median: 16.6 years old, range 5.8–19.8), were also analysed and the prevalence of the RET/PTC rearrangements was 25.9%. As far as we are aware, there are only two studies that analysed Japanese cases and they demonstrated 30% (9–14 years old) and 41.9% (<20 years old)32,33. However, note that the cohort in the present study is completely different from those in the above previous studies because the data in this work were obtained due to mass screening of basically healthy individuals without any symptom. Even though the incidence in Fukushima has been much higher than that reported previously, it is quite unlikely that this is due to radiation exposure because of their shorter latency and higher age distribution34,35. Moreover, the patterns of the genetic alterations in our cases were completely different from radiation-induced PTCs. Assuming that most of these cases would be silent until middle or older age, we could speculate that paediatric PTCs with the BRAFV600E mutation may be not so progressive compared to those with the rearrangements. Consistent with this hypothesis, our data in the present study has demonstrated that tumours with the BRAFV600E mutation were significantly smaller than BRAFV600E-negative cases including RET/PTC or ETV6/NTRK3. It is supposed that we detected these tumours earlier in life because of the extremely sensitive ultrasound screening procedure.
ETV6/NTRK3 has been recently found in both radiation-associated paediatric PTCs and sporadic paediatric PTCs with comparable frequencies (2 of 26 in exposed and 2 of 27 in sporadic)31, although the number of analysed cases was limited. It has been reported that this rearrangement was significantly more common in post-Chernobyl PTCs (mean age: 22.7 ± 5.1 years; 9 of 62, 14.5%) than in sporadic PTCs (mean age: 45.6 ± 17.7 years; 3 of 151, 2%); however, the age was not matched in this study29. Thus, the association between ETV6/NTRK3 and radiation exposure is not clear and this fusion gene may just be associated with young age.
TERT promoter mutations (C250T and C228T) have also been discovered recently in thyroid cancers36,37. These mutations are highly associated with older age and worse prognosis38,39. Some papers have also reported that these mutations are correlated with the presence of the BRAFV600E mutation36,38,39,40. Here we demonstrate that these mutations were completely absent in this age group even though many of them carried the BRAFV600E mutation.
In conclusion, the genetic profile of the Fukushima thyroid cancers was completely different from post-Chernobyl radiation-induced PTCs, suggesting non-radiogenic etiology of these cancers. However, note that since similar high-resolution ultrasound apparatus was not available after the Chernobyl accident, it might be difficult to strictly compare the results of the two populations. Simultaneously, we for the first time demonstrate the distribution of the oncogenes in the young thyroid cancer cases discovered by large mass screening. This probably reflects genetic status of all sporadic and latent thyroid carcinomas in the young Japanese population. The prevalence of the BRAFV600E mutation was comparable to Japanese adult cases, implying that the carcinogenic mechanisms may be similar between paediatric and adult PTCs. However, it is assumed that the BRAFV600E mutation may not confer growth advantage on paediatric PTCs and many of these tumours do not grow rapidly, suggesting that additional factors may be necessary to enhance tumour growth. Thus, it is beneficial to identify such a key factor to improve the management of paediatric PTC patients.
Methods
The thyroid ultrasound screening program under the Fukushima Health Management Survey is being conducted by Fukushima Medical University. This program covers all residents in the Fukushima prefecture aged from zero to 18 years old at the time of the accident. During first three years, the baseline survey has been conducted. We also included three cases in the same age range incidentally discovered through other medical examinations in the same region.
We analysed 68 thyroid cancer cases operated between February 2013 and September 2014 (mean age: 17.3 years old; mean tumour size: 14.7 mm; 22 males and 46 females) at Fukushima Medical University. Fresh tumour tissue samples were obtained during surgical operations, snap-frozen in liquid nitrogen and stored at −80 °C. DNA and total RNA were extracted at the same time using ISOGEN reagent (Nippon Gene) according to the manufacturer’s protocol. Mutations of BRAF (exon 15), HRAS, KRAS and NRAS (codons 12, 13 and 61) and TERT promoter (C250T and C228T) were examined by direct DNA sequencing. PCR enzymes and primer sequences used for PCR amplifications and sequencing are listed in Supplemental Table S1. PCR products were then treated with ExoSAP-IT PCR clean-up reagent (GE Healthcare) and sequencing was performed with Big Dye Terminator sequencing kit version 3.1 (Applied Biosystems) on an ABI3730 automated sequencer (Applied Biosystems). For RET/PTC, AKAP9/BRAF and ETV6/NTRK3 detection, total RNA was reverse transcribed using High Capacity RNA-to-cDNA kit (Applied Biosystems). Subsequent PCR amplifications were done using PCR enzymes and primers listed in Supplemental Table S1. We included 3–5 negative controls (w/o template) per 96 samples in every PCR to ensure contamination-free amplifications.
Statistical analysis was performed using the SPSS software version 21.0.0.0 (IBM). Mann-Whitney or Fisher’s exact test were used for continuous variables or group analyses, respectively. For multivariate analyses, linear or logistic regression models were used. The p value less than 0.05 was regarded as indicating statistical significance.
This study was approved by the ethics committees of Fukushima Medical University and Nagasaki University. Written informed consent was obtained from each patient. All experiments were carried out in accordance with the approved study plan and relevant guidelines.
Additional Information
How to cite this article: Mitsutake, N. et al. BRAFV600E mutation is highly prevalent in thyroid carcinomas in the young population in Fukushima: a different oncogenic profile from Chernobyl. Sci. Rep. 5, 16976; doi: 10.1038/srep16976 (2015).
References
Yasumura, S. et al. Study protocol for the Fukushima Health Management Survey. J. Epidemiol. 22, 375–383 (2012).
Yamashita, S. & Tenth Warren, K. Sinclair keynote address-the Fukushima nuclear power plant accident and comprehensive health risk management. Health Phys. 106, 166–180 (2014).
Kazakov, V. S., Demidchik, E. P. & Astakhova, L. N. Thyroid cancer after Chernobyl. Nature 359, 21 (1992).
Cardis, E. et al. Cancer consequences of the Chernobyl accident: 20 years on. J. Radiol. Prot. 26, 127–140 (2006).
Nikiforov, Y. E. Radiation-induced thyroid cancer: what we have learned from chernobyl. Endocr. Pathol. 17, 307–317 (2006).
Saenko, V. et al. The Chernobyl accident and its consequences. Clin. Oncol. (R. Coll. Radiol.) 23, 234–243 (2011).
Tokonami, S. et al. Thyroid doses for evacuees from the Fukushima nuclear accident. Sci. Rep. 2, 507 (2012).
Hosoda, M. et al. Estimation of internal exposure of the thyroid to (131)I on the basis of (134)Cs accumulated in the body among evacuees of the Fukushima Daiichi Nuclear Power Station accident. Environ. Int. 61, 73–76 (2013).
Nagataki, S. & Takamura, N. A review of the Fukushima nuclear reactor accident: radiation effects on the thyroid and strategies for prevention. Curr. Opin. Endocrinol. Diabetes Obes. 21, 384–393 (2014).
Hayashida, N. et al. Thyroid ultrasound findings in children from three Japanese prefectures: Aomori, Yamanashi and Nagasaki. PLoS One 8, e83220 (2013).
Hayashida, N. et al. Thyroid ultrasound findings in a follow-up survey of children from three Japanese prefectures: Aomori, Yamanashi and Nagasaki. Sci. Rep. 5, 9046 (2015).
Kondo, T., Ezzat, S. & Asa, S. L. Pathogenetic mechanisms in thyroid follicular-cell neoplasia. Nat. Rev. Cancer 6, 292–306 (2006).
Xing, M. Molecular pathogenesis and mechanisms of thyroid cancer. Nat. Rev. Cancer 13, 184–199 (2013).
Xing, M. BRAF mutation in thyroid cancer. Endocr. Relat. Cancer 12, 245–262 (2005).
Fukushima, T. et al. BRAF mutations in papillary carcinomas of the thyroid. Oncogene 22, 6455–6457 (2003).
Kurtulmus, N. et al. BRAF(V600E) mutation in Turkish patients with papillary thyroid cancer: strong correlation with indicators of tumor aggressiveness. Endocrine 42, 404–410 (2012).
Kim, S. J. et al. BRAF V600E mutation is associated with tumor aggressiveness in papillary thyroid cancer. World J. Surg. 36, 310–317 (2012).
Yang, L. B. et al. The Clinicopathological Features of BRAF Mutated Papillary Thyroid Cancers in Chinese Patients. Int. J. Endocrinol. 2015, 642046 (2015).
Yamashita, S. & Saenko, V. Mechanisms of Disease: molecular genetics of childhood thyroid cancers. Nat. Clin. Pract. Endocrinol. Metab. 3, 422–429 (2007).
Fenton, C. L. et al. The ret/PTC mutations are common in sporadic papillary thyroid carcinoma of children and young adults. J. Clin. Endocrinol. Metab. 85, 1170–1175 (2000).
Kumagai, A. et al. Low frequency of BRAFT1796A mutations in childhood thyroid carcinomas. J. Clin. Endocrinol. Metab. 89, 4280–4284 (2004).
Penko, K. et al. BRAF mutations are uncommon in papillary thyroid cancer of young patients. Thyroid 15, 320–325 (2005).
Rosenbaum, E. et al. Mutational activation of BRAF is not a major event in sporadic childhood papillary thyroid carcinoma. Mod. Pathol. 18, 898–902 (2005).
Powell, N. et al. Frequency of BRAF T1796A mutation in papillary thyroid carcinoma relates to age of patient at diagnosis and not to radiation exposure. J. Pathol. 205, 558–564 (2005).
Henke, L. E. et al. BRAF V600E mutational status in pediatric thyroid cancer. Pediatr. Blood Cancer 61, 1168–1172 (2014).
Givens, D. J., Buchmann, L. O., Agarwal, A. M., Grimmer, J. F. & Hunt, J. P. BRAF V600E does not predict aggressive features of pediatric papillary thyroid carcinoma. Laryngoscope 124, E389–393 (2014).
Guan, H. et al. Association of high iodine intake with the T1799A BRAF mutation in papillary thyroid cancer. J. Clin. Endocrinol. Metab. 94, 1612–1617 (2009).
Lima, J. et al. BRAF mutations are not a major event in post-Chernobyl childhood thyroid carcinomas. J. Clin. Endocrinol. Metab. 89, 4267–4271 (2004).
Leeman-Neill, R. J. et al. ETV6-NTRK3 is a common chromosomal rearrangement in radiation-associated thyroid cancer. Cancer 120, 799–807 (2014).
Hamatani, K. et al. RET/PTC rearrangements preferentially occurred in papillary thyroid cancer among atomic bomb survivors exposed to high radiation dose. Cancer Res. 68, 7176–7182 (2008).
Ricarte-Filho, J. C. et al. Identification of kinase fusion oncogenes in post-Chernobyl radiation-induced thyroid cancers. J. Clin. Invest. 123, 4935–4944 (2013).
Motomura, T. et al. ret rearrangements in Japanese pediatric and adult papillary thyroid cancers. Thyroid 8, 485–489 (1998).
Nakazawa, T. et al. RET gene rearrangements (RET/PTC1 and RET/PTC3) in papillary thyroid carcinomas from an iodine-rich country (Japan). Cancer 104, 943–951 (2005).
Tronko, M. D. et al. Age distribution of childhood thyroid cancer patients in Ukraine after Chernobyl and in Fukushima after the TEPCO-Fukushima Daiichi NPP accident. Thyroid 24, 1547–1548 (2014).
Yamashita, S. & Suzuki, S. Risk of thyroid cancer after the Fukushima nuclear power plant accident. Respir Investig 51, 128–133 (2013).
Liu, X. et al. Highly prevalent TERT promoter mutations in aggressive thyroid cancers. Endocr. Relat. Cancer 20, 603–610 (2013).
Landa, I. et al. Frequent somatic TERT promoter mutations in thyroid cancer: higher prevalence in advanced forms of the disease. J. Clin. Endocrinol. Metab. 98, E1562–1566 (2013).
Melo, M. et al. TERT promoter mutations are a major indicator of poor outcome in differentiated thyroid carcinomas. J. Clin. Endocrinol. Metab. 99, E754–765 (2014).
Xing, M. et al. BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence. J. Clin. Oncol. 32, 2718–2726 (2014).
Liu, X. et al. TERT promoter mutations and their association with BRAF V600E mutation and aggressive clinicopathological characteristics of thyroid cancer. J. Clin. Endocrinol. Metab. 99, E1130–1136 (2014).
Acknowledgements
This work was supported in part by JSPS KAKENHI, grant number: 25461989 (TF), 25257508 (SY), 26293222 (SY), 26293142 (NM). This study was also supported in part by Cooperative Research Grant of Atomic Bomb Disease Institute, Nagasaki University (TF). We thank members of Departments of Thyroid and Endocrinology and Organregulatory Surgery, Fukushima Medical University, the Thyroid Examination Unit of the Radiation Medical Centre for the Fukushima Health Management Survey and the Consensus Meeting of Pathological Diagnosis of Fukushima Thyroid Cancers, who participate the thyroid ultrasound screening program.
Author information
Authors and Affiliations
Contributions
N.M., T.F., S.S. and S.Y. planned the study. T.F. and S.S. collected samples and clinical data. M.M. and T.R. performed genetic analysis. N.M., V.S., S.U., M.I. and K.S. analyzed data. V.S. did statistical analysis. N.M. wrote the manuscript. All authors approved the final version of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Mitsutake, N., Fukushima, T., Matsuse, M. et al. BRAFV600E mutation is highly prevalent in thyroid carcinomas in the young population in Fukushima: a different oncogenic profile from Chernobyl. Sci Rep 5, 16976 (2015). https://doi.org/10.1038/srep16976
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep16976
This article is cited by
-
No increase in translocated chromosomal aberrations, an indicator of ionizing radiation exposure, in childhood thyroid cancer in Fukushima Prefecture
Scientific Reports (2023)
-
Increased trend of thyroid cancer in childhood over the last 30 years in EU countries: a call for the pediatric surgeon
European Journal of Pediatrics (2022)
-
Molecular Pathology of Non-familial Follicular Epithelial–Derived Thyroid Cancer in Adults: From RAS/BRAF-like Tumor Designations to Molecular Risk Stratification
Endocrine Pathology (2021)
-
Consequences of atmospheric contamination by radioiodine: the Chernobyl and Fukushima accidents
Endocrine (2021)
-
Poorly differentiated thyroid carcinoma of childhood and adolescence: a distinct entity characterized by DICER1 mutations
Modern Pathology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.