Abstract
Uncertainty exists about the role of diabetes in the development of surgery-related pressure ulcers. Therefore, we conducted a meta-analysis to explore the association between pre-existing diabetes mellitus and pressure ulcers among patients after surgery. Summary odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using random effects models. Thirteen eligible studies of 2367 patients in total and 12053 controls were included in the final analysis. Compared with patients without diabetes, the pooled odds ratio (OR) of the incidence of pressure ulcers in diabetic patients was 1.74 [95% confidence interval (CI) = 1.40–2.15, I2 = 51.1%]. Estimates by type of surgery suggested similar results in cardiac surgery [OR = 2.00, 95% CI = 1.42–2.82, I2 = 0%], in general surgery [OR = 1.75, 95% CI = 1.42–2.15, I2 = 0%] and in major lower limb amputations [OR = 1.65, 95% CI = 1.01–2.68, I2 = 0%] for diabetic patients versus non-diabetic controls. We did not find an increased incidence of pressure ulcers in diabetic patients undergoing hip surgery compared with non-diabetic controls [OR = 1.46, 95% CI = 0.62–3.47, I2 = 93.1%]. The excess risk of pressure ulcers associated with pre-existing diabetes was significantly higher in patients undergoing surgery, specifically in patients receiving cardiac surgery. Further studies should be conducted to examine these associations in other types of surgery.
Similar content being viewed by others
Introduction
Pressure ulcers have become a common problem faced by global health care institutions and seriously threaten the life and health of the patient, leading to large economic pressures and societal health burdens. Therefore, accurately identifying patients who are at risk of developing pressure ulcers is the key to prevention. Patients undergoing surgical procedures are a high-risk group for pressure ulcers; reported incidence rates of perioperative pressure ulcers have ranged from 3.4% to 66%2,3,4,5,6,7,8,9,10,11,12,13,14.
Surgical risk factors leading the development of pressure ulcers include the number of surgeries, total time in the operating room, surgical site and the use of extracorporeal circulation, among other factors2,3,9,10,14. One possible reason may be that the patient is immobile for long periods during surgical procedures and is unable to relieve the pressure on bony prominences. Consequently, tissue ischemia results because of capillary blood flow occlusion from prolonged unrelieved pressure. In addition to the aforementioned surgical risk factors, diabetes mellitus is also a characteristic thought to be commonly associated with perioperative pressure ulcers2,3,4,5,6,7,8,9,10,11,12,13.
To date, several studies have focused on the association between diabetes mellitus and surgery-related pressure ulcers; however, these published reports have varied by incidence, type of surgery and risk factors, among other reasons. A previous meta-analysis conducted by Liu et al.15 examined the association and calculated the total efficacy rate but did not include all eligible publications. In addition, the conclusions were not stratified by different types of surgery. Furthermore, many new relevant cohort and case-control studies have now been published, especially three recently published studies1,2,4 that each involved large samples of more than two thousand participants. Thus, we undertook an updated and extended analysis that incorporated additional previous and more recent data to further assess diabetes as a risk factor for pressure ulcers in patients undergoing different types of surgery.
Methods
Search strategy
A comprehensive literature search was performed using the PubMed (1946-October 2014) and EMBASE (1947-October 2014) electronic databases by two independent investigators (ZQK and XJZ). The following search strategy, adapted for PubMed and EMBASE, was used for the searches without restrictions: (“operative” OR “operation” OR “surgery” OR “surgical” OR “surg*”) AND (“diabetes” OR “diabetic” OR “Diabetes Mellitus” OR “diabet*”) AND (“pressure ulcer” OR “bedsore*” OR “pressure sore*” OR “bed sore*” OR “decubitus ulcer*” OR “bed-sore*”). Furthermore, we conducted a manual search by checking the cited reference lists of the original reports to locate additional relevant studies. Unpublished reports were not considered.
Study selection
The titles or abstracts of all of the identified studies were screened by two independent reviewers (ZQK and XJZ). The full text was retrieved for further assessment when the reviewers could not evaluate a study’s topic from its title or abstract. Discrepancies were resolved by discussion. The inclusion criteria for screening the studies were as follows: (1) original human studies published in English; (2) original epidemiologic studies (i.e., RCT, cohort or case-control); (3) pre-existing diabetes mellitus was the exposure; (4) the outcome was the development of pressure ulcers; (5) the study investigated the association between pressure ulcer and pre-existing diabetes mellitus among perioperative patients; and (6) risk estimates (odds ratio or relative risk) were published along with their 95% confidence intervals (CI) or enough data were provided to calculate these estimates. Studies were excluded if they (1) were letters, comments, correspondences, review articles or case reports; (2) were based on small sample size (<30 patients); (3) provided insufficient data; or (4) did not examine relevant outcomes. If multiple studies were found to share an identical population, we only included the most recent publication.
Data extraction and quality assessment
Two reviewers (ZQK and XJZ) independently extracted the data from the eligible studies using piloted and standardized data extraction forms. The form included the first author’s name, publication year, type of publication, study geographic location, study design, inclusion period, operation methods, sample size, mean/median age, diabetes type, treatment regimen, use of multivariate logistic model analysis, follow-up period, adjustment factors and ORs with corresponding 95% CIs. Discrepancies were resolved by discussion.
The eligible studies were assessed by two independent reviewers (ZQK and XJZ) using the Newcastle-Ottawa Scale (NOS)16. The quality of each study was evaluated using 3 major categories: selection, comparability and exposure/outcomes. A full NOS score was 9 stars; an awarded score of 5 stars or more was defined as a high-quality research in our study according to standards of previous meta-analysis17.
Statistical analysis
The meta-analysis was performed using STATA statistical software (version 12.0, Stata Corporation, College Station, TX, USA). We retrieved or calculated the OR estimates with a 95% CI from the baseline form. Summary ORs and 95% CIs were performed using a random effects model due to the potential heterogeneity among the studies in the meta-analysis (e.g., methods of surgery, study designs, follow-up time, etc.). Inter-study heterogeneity was explored and quantified using the I2 test; an I2 > 50% indicated significant heterogeneity18. Reasons for heterogeneity were detected through sensitivity analyses. Publication bias was assessed visually by inspecting funnel plots and by using Egger’s or Begg’s regression test whereby a P-value < 0.10 was considered to be significant19.
We performed subgroup analyses to reveal potential associations among the different types of operations (e.g., hip surgery, major lower limb amputations, cardiac surgery and general surgery).
Results
Search results and study characteristics
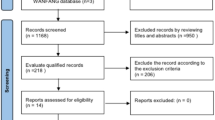
A total of 863 studies were identified from the PubMed and EMBASE electronic databases; of these, 64 studies were considered to have potential value for further review. We retrieved the full texts for detailed evaluation and identified two relevant individual studies through a manual reference search. By excluding unrelated studies based on the inclusion criteria, 17 total studies were identified. Lastly, we excluded 4 studies with insufficient data when we could not acquire the necessary information by contacting the authors directly. Finally, thirteen eligible studies were included in our meta-analysis. The screening process was summarized in a flow diagram (Fig. 1).
Table 1 outlines the characteristics of the 13 included studies, totaling 2367 patients and 12053 controls including 1422 incident perioperative pressure ulcer events during the follow-up periods. All of the selected studies were observational, including eight prospective cohort studies and three retrospective case-control studies. Seven studies were from the US, two from the UK and one each was from Sweden, Italy, Spain and Belgium. Logistic regression analysis was the most common approach, used in nine of the eligible studies. The remaining four studies were performed using univariate analysis. The data collection period was from 1995 to 2009 (five studies did not report the data collection period). All of the eligible studies were considered to be of high quality, ranging from five to eight points according to the Newcastle-Ottawa Scale (Table 1).
Results of meta-analysis
We conducted a primary meta-analysis using all thirteen studies included in the final analysis. The pooled summary OR of pressure ulcer incidence in diabetic patients was 1.74 [95% CI = 1.40–2.15, I2 = 51.1%] compared with individuals without diabetes (Fig. 2).
We conducted subgroup analyses according to the surgical method in order to further explore the associations between diabetes and the risk of perioperative pressure ulcers (Fig. 3). The subgroup analysis of four studies examining cardiac surgery suggested a significant association [OR = 2.00, 95% CI = 1.42–2.82, I2 = 0%]. Similar results were also found in the general surgery subgroup [OR = 1.75, 95% CI = 1.42–2.15, I2 = 0%] and in the major lower limb amputation subgroup [OR = 1.65, 95% CI = 1.01–2.68, I2 = 0%]. We did not observe an increased incidence of pressure ulcers between diabetic patients undergoing hip surgery compared with non-diabetic controls [OR = 1.46, 95% CI = 0.62–3.47, I2 = 93.1%].
Test of heterogeneity and sensitivity analyses
There was significant heterogeneity among the eligible studies [P = 0.014, I2 = 51.1%]. In order to detect the possible reasons for heterogeneity, we used the leave-one-out sensitivity analysis technique. When removing the study by Ekstrom et al.1, the estimate using all of the other studies was clearly altered [OR = 1.63, 95% CI = 1.25–2.14] (Fig. 4).
Publication bias
The funnel plot showed slight asymmetry (Fig. 5) and possible publication bias existed among the 13 included studies (Begg’s test, P for bias = 0.228; Egger’s test, P for bias = 0.009).
Discussion
Our updated meta-analysis suggested that diabetes mellitus may lead to a higher risk of perioperative pressure ulcers. In subgroup analyses, similar results were found in cardiac surgery, general surgery and major lower limb amputations.
Among the diabetic patients undergoing cardiac surgery, we found that the risk of pressure ulcers was twice that for the non-diabetic controls. Compared with other types of surgery, restricted movement from cardiac assistive devices (e.g., intra-aortic balloon pumps, left ventricular assist devices, etc.) and heart failure were considered to be contributing factors for the pressure ulcers in patients undergoing cardiac surgery8.
For lower limb amputations, diabetes mellitus has been widely considered to be a risk factor20 compared with amputees without diabetes; the presence of diabetes often indicated a worse prognosis and a higher incidence of pressure sores6,21. Peripheral neuropathy in diabetic patients might assist the development of pressure ulcers due to injuries to protective pain sensations and interferences with micro-vascular circulation9.
No significant association was observed in the hip surgery subgroup. The subgroup analysis of the 5966 hip surgery cases4 indicated that patients with diabetes had a higher incidence and risk of pressure ulcers than the non-diabetic group. However, the other included study of 2133 patients1 did not indicate a clear difference in the incidence of pressure ulcers between diabetics and non-diabetics. The most likely explanations could be that 76% of the participants in Ekstrom’s study1 had ASA class (American Society of Anesthesiologists’ classification) 3–5, indicating entirely reduced physical activity and health. This finding may have led to the inconsistent results from the two studies.
Compared with the prior meta-analysis of the six studies conducted by Peng Liu et al.15, we included thirteen studies and performed more subgroup analyses to explore the potential confounders that influenced the findings. We conducted more powerful and detailed analyses to obtain our results. First, we included more studies in the analysis, especially three recently published studies that each had large sample sizes exceeding two thousand participants. Second, we conducted more comprehensive subgroup analyses. Despite the similar results found among cardiac surgery and general surgery patients, we also found a consistency effect among patients with major lower limb amputations.
Several limitations in our meta-analysis should be noted. First, we only searched for studies published in English that were included in PubMed and EMBASE; thus, some relevant studies published in other languages and in additional databases may not be identified in our research. Moreover, caution should be warranted when interpreting the overall study estimates because there was significant heterogeneity. Furthermore, we did not register our meta-analysis at inception. We suggest that future systematic reviews should be prospectively registered to improve transparency in the review process and prevent selective publication bias.
In summary, the excess risk of pressure ulcers associated with diabetes is significantly higher in participants undergoing surgery, specifically in patients receiving cardiac surgery. Further studies should be conducted to assess the association in other types of surgery.
Additional Information
How to cite this article: Kang, Z.-Q. and Zhai, X.-J. The Association between Pre-existing Diabetes Mellitus and Pressure Ulcers in Patients Following Surgery: A Meta-analysis. Sci. Rep. 5, 13007; doi: 10.1038/srep13007 (2015).
References
Ekstrom, W. et al. Health related quality of life, reoperation rate and function in patients with diabetes mellitus and hip fracture - A 2 year follow-up study. Injury 44, 769–775 (2013).
Tschannen, D., Bates, O., Talsma, A. & Guo, Y. Patient-specific and surgical characteristics in the development of pressure ulcers. American journal of critical care : an official publication, American Association of Critical-Care Nurses 21, 116–125, doi: 10.4037/ajcc2012716 (2012).
Bulfone, G., Marzoli, I., Quattrin, R., Fabbro, C. & Palese, A. A longitudinal study of the incidence of pressure sores and the associated risks and strategies adopted in Italian operating theatres. Journal of perioperative practice 22, 50–56 (2012).
Norris, R. & Parker, M. Diabetes mellitus and hip fracture: a study of 5966 cases. Injury 42, 1313–1316, doi: 10.1016/j.injury.2011.03.021 (2011).
Slowikowski, G. C. & Funk, M. Factors associated with pressure ulcers in patients in a surgical intensive care unit. Journal of wound, ostomy and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society/WOCN 37, 619–626, doi: 10.1097/WON.0b013e3181f90a34 (2010).
Aragon-Sanchez, J. et al. In-hospital complications and mortality following major lower extremity amputations in a series of predominantly diabetic patients. International Journal of Lower Extremity Wounds 9, 16–23 (2010).
Frankel, H., Sperry, J. & Kaplan, L. Risk factors for pressure ulcer development in a best practice surgical intensive care unit. The American surgeon 73, 1215–1217 (2007).
Pokorny, M. E., Koldjeski, D. & Swanson, M. Skin care intervention for patients having cardiac surgery. American journal of critical care : an official publication, American Association of Critical-Care Nurses 12, 535–544 (2003).
Spittle, M., Collins, R. J. & Connor, H. The incidence of pressure sores following lower limb amputations. Practical Diabetes International 18, 57–61 (2001).
Schultz, A., Bien, M., Dumond, K., Brown, K. & Myers, A. Etiology and incidence of pressure ulcers in surgical patients. AORN journal 70, 434, 437–440, 443–439 (1999).
Stordeur, S., Laurent, S. & D’Hoore, W. The importance of repeated risk assessment for pressure sores in cardiovascular surgery. Journal of Cardiovascular Surgery 39, 343–349 (1998).
Lewicki, L. J., Mion, L., Splane, K. G., Samstag, D. & Secic, M. Patient risk factors for pressure ulcers during cardiac surgery. AORN journal 65, 933–942 (1997).
Papantonio, C. T., Wallop, J. M. & Kolodner, K. B. Sacral ulcers following cardiac surgery: incidence and risks. Advances in wound care : the journal for prevention and healing 7, 24–36 (1994).
Schoonhoven, L., Defloor, T. & Grypdonck, M. Incidence of pressure ulcers due to surgery. Journal of Clinical Nursing 11, 479–487 (2002).
Liu, P., He, W. & Chen, H. L. Diabetes mellitus as a risk factor for surgery-related pressure ulcers: a meta-analysis. Journal of wound, ostomy and continence nursing : official publication of The Wound, Ostomy and Continence Nurses Society/WOCN 39, 495–499, doi: 10.1097/WON.0b013e318265222a (2012).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25, 603–605, doi: 10.1007/s10654-010-9491-z (2010).
Millett, G. A., Flores, S. A., Marks, G., Reed, J. B. & Herbst, J. H. Circumcision status and risk of HIV and sexually transmitted infections among men who have sex with men: a meta-analysis. JAMA : the journal of the American Medical Association 300, 1674–1684, doi: 10.1001/jama.300.14.1674 (2008).
Higgins, J., Thompson, S., Deeks, J. & Altman, D. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Egger, M., Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Boulton, A., Vileikyte, L., Ragnarson-Tennvall, G. & Apelqvist, J. The global burden of diabetic foot disease. Lancet 366, 1719–1724 (2005).
Schofield, C. et al. Mortality and hospitalization in patients after amputation: a comparison between patients with and without diabetes. Diabetes Care 29, 2252–2256, doi: 10.2337/dc06-0926 (2006).
Author information
Authors and Affiliations
Contributions
X.J.Z. and Z.Q.K. designed the experiments; X.J.Z. and Z.Q.K. collected the data; Z.Q.K. wrote the main manuscript text; and all authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Kang, ZQ., Zhai, XJ. The Association between Pre-existing Diabetes Mellitus and Pressure Ulcers in Patients Following Surgery: A Meta-analysis. Sci Rep 5, 13007 (2015). https://doi.org/10.1038/srep13007
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep13007
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.