Abstract
Neurocognition is a key factor in the development and maintenance of Substance Use Disorders (SUD). However, there are still several aspects that need to be studied in this area. In this study, we elucidate the influence of age of onset of substance use (OSU) on the clinical course and neuropsychological performance of substance use disorder (SUD) patients, as well as to explore the influence of years of education, duration of drug use and premorbid intelligence quotient (IQ) on the cognitive results obtained. An exhaustive neuropsychological battery was used to assess different cognitive domains in 80 male polyconsumers, 41 with earlier OSU (16 years or before: OSU ≤ 16) and 39 with later OSU (17 years or later: OSU ≥ 17). The patients were under treatment with at least 4 months of abstinence confirmed by urinalysis. The OSU ≤ 16 group presented a worse clinical state, as well as a lower premorbid IQ and worse performance in processing speed, visual perception and planning skills. The duration of drug use may account for the differences in planning and processing speed. In this work we discuss the premorbid or acquired nature of the cognitive deficits found.
Similar content being viewed by others
Introduction
The United Nations Office on Drugs and Crime considers substance use as a public health issue that has severe consequences on individuals and communities1. Despite the improvements in prevention and treatment of Substance Use Disorders (SUD), the world levels of consumption are significantly high2. This may be partly due to the fact that several genetic and environmental factors intervene in the onset and maintenance of SUD3, which in turn causes a wide array of clinical symptomatology4 and response to intervention5. Thus, it is necessary to study new ways to improve our knowledge of the ethiopathogenesis of SUD, its typologies and the relevant associated variables both its prevention and rehabilitation.
In this line, neuropsychology has made valuable contributions in recent years. Some studies, scarce but promising, indicate that incorporating cognitive rehabilitation in the treatment of addiction optimizes the results of traditional interventions6,7. This is consistent with current models of development and maintenance of SUD where the role of biological and neurocognitive factors stands, in addition to environmental factors3.
Thus, it has been shown that SUD patients show alterations in cognitive functions such as inhibitory or executive control8,9, working memory10 or visuospatial skills11, even before consumption onset. In addition, several studies support that cognitive impairment due to consumption is related to both duration and severity of addiction, there being dose-dependent relationships12, although more studies are needed to establish a reliable relationship between cognitive impairment and the severity of SUD. Likewise, it has been shown that the greater the cognitive impairment, poorer are the treatment outcomes13,14. Specifically, deficits in inhibitory control and cognitive flexibility may affect the ability of patients to focus attention and direct their behavior to new and alternative goals which are incompatible with substance use-related behaviors15.
In the study of the relationship between cognitive functions and the development and characteristics of SUD, special attention has been paid to modulating factors such as the type of substance used16, the pattern of consumption or duration of drug use17. While some studies have also highlighted the relevance of the age of onset of substance use (OSU), new studies are needed to provide more robust data about their relationship, particularly in cases of polyconsumption or considering specific ages of OSU. However, in samples of alcoholic patients, an earlier OSU has been linked to increased intensity of personality traits linked to consumption, such as high Novelty Seeking or low Harm Avoidance6,18, worse clinical course4 and greater structural and functional brain alterations19. In polyconsumers, early OSU has also been associated with greater cognitive impairment20. Furthermore, consumption in adolescence implies greater cognitive impairment compared to adulthood21,22, due to the different critical periods for brain maturation23. Thus, the study of typologies of addicts based on their cognitive performance and their clinical implications considering the age of OSU is a research area of undoubted clinical interest.
In several studies with cannabis consumers, neuropsychological differences have been observed depending on whether consumption begins at age 16 or earlier, or at age 17 or later. Individuals with an earlier OSU perform lower in tasks of visual exploration24, processing speed and cognitive flexibility25; have lower verbal intelligence quotient (VIQ)26 and show less cerebral and gray matter volume27. The cut-off age used in these studies was based on three characteristics of brain ontogeny: (a) between 12 and 15 years the network involved in visual scanning reaches its peak development28; (b) compared with the serotonergic system, the dopaminergic and endocannabinoid systems, which are key in prefrontal functioning, mature earlier29, being almost defined by the end of puberty30; (c) by age 15 there is one last peak in cortical changes31. However, the only study that used this cutoff age with mostly cocaine and alcohol consumers did not replicate earlier findings32.
Our work has three aims. The first is to study the differences in the clinical course of polyconsuming men diagnosed with SUD, depending on whether they initiated substance use at age 16 or earlier (OSU ≤ 16) or at age 17 or later (OSU ≥ 17). The second is to assess the differences in their neuropsychological performance. Unlike previous works where only one type of cognitive function has been studied, in the current work we have administered a comprehensive battery of neuropsychological tests sensitive to the characteristics of SUD patients. Our third goal is to explore, regardless of the groups, if the age of patients, age of OSU, years of education, duration of drug use and the premorbid intelligence quotient (IQ) modulate their neurocognitive performance.
Results
Differences in sociodemographic and clinical data
With respect to sociodemographic variables, the OSU ≤ 16 and OSU ≥ 17 groups provided no significant differences in any of them: age, years of education, marital and economic status. The overall sample was aged 20 to 55 (36.45 ± 8.20) and most of the patients had completed the Spanish compulsory education (from 6 to 16 years, grades 1 to 10). The analyses of the clinical variables did indicate significant differences between groups, being more frequent in the OSU ≤ 16 group to have relatives with SUD (p = 0.044). See Table 1.
Regarding SUD data, the OSU ≤ 16 group had a higher rate of patients in residential rather than in ambulatory treatment (p = 0.003) and with a higher rate of polyconsumption (p = 0.008). They also had lower age of OSU (p = 0.0001), greater duration of drug use (p = 0.001) and higher rates of relapse (p = 0.039). The groups did not differ in the type of substance used or in the months of abstinence (see Table 2). In the total sample, the substances most frequently used were cocaine (95%), alcohol (77.5%) and cannabis (48.8%).
In the total sample, an additional analysis was carried out considering the treatment regimen (residential or ambulatory), to assess whether this was an indicator of clinical severity related to the recruitment of patients in both regimes and not related to the age of OSU. No significant differences between groups were found regarding age (t(39) = 1.899; p = 0.065), years of education (U = 549.50; p = 0.102) or scores in the Block Design subtest (t(39) = 1.19; p = 0.544). Instead, significant differences were found in duration of drug use (t(39) = 0.826; p = 0.030) and in the Vocabulary subtest scores (t(39) = −0.764; p = 0.016).
Differences in neuropsychological functioning
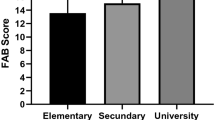
Considering age and years of education as covariates, significant differences between groups were found in the Vocabulary (p = 0.007) and Block Design (p = 0.019) subtests, where the OSU ≤ 16 group had a worse performance in both. This group also took longer (p = 0.003) to complete the Trail Making Test part A (TMT-A). Regarding the Judgment of Line Orientation Test (JLOT), the OSU ≤ 16 group performed worse in all the parameters measured: number of correct answers (p = 0.024) and reaction time (p = 0.038) (see Table 3).
In addition, in the Tower of Hanoi test the OSU ≤ 16 group required more number of movements (p = 0.045), committed more errors (p = 0.262) and showed a higher reaction time (p = 0.009) (see Table 4). No differences between groups were found in the other neuropsychological tasks: Digits Forward, Digits Backwards, Rey Auditory Verbal Learning Test (RAVLT), Trail Making Test part-B (TMT-B), Wisconsin Card Sorting Test (WCST) and Iowa Gambling Test (IGT).
Influence on neuropsychological functioning of age of onset of substance use, age, years of education, duration of drug use, premorbid verbal and performance IQ
First, comparing cognitive performance taking age, years of education, duration of drug use and score in Vocabulary and Block Design as covariates eliminated intergroup differences observed previously (see Table 3 and Table 4).
Second, considering the total sample, the regression analysis indicated that the model was significant in only three neuropsychological tasks: TMT-A, JLOT and Tower of Hanoi (see Table 5). In these three cognitive domains, the significant variables were Block Design, duration of drug use and age of OSU, explaining more than 17% of the variance. Block Design explained 34% of the variance of the number of correct answers in the JLOT (p = 0.0001) and, together with age of OSU, 17% of the variance of reaction time (p = 0.0001). Block Design and duration of drug use accounted for 29% of the variance in the TMT-A. Finally, duration of drug use explained 20% of the variance in reaction time in the Tower of Hanoi (p = 0.0001).
Discussion
This study examines, for the first time, the possible existence of clinical and neurocognitive differences in polydrug addicts depending on whether their substance use began at age 16 or earlier, or at age 17 or later. In addition, we also assess the effect of age of onset, age, years of education, duration of drug use and premorbid IQ on cognitive performance for the total sample.
The groups did not differ in any sociodemographic parameter studied or in the main substance of consumption. Moreover, they did not differ in the variables that affect cognition, such as duration of abstinence33,34, rates of caffeine and nicotine intake35 or use of psychotropic drugs36 and therefore we discarded their effects on the results of neuropsychological performance.
The OSU ≤ 16 group presented a more severe clinical pattern, characterized by the presence of more family history of SUD, higher relapse rate, the need for a more intensive treatment regimen to achieve abstinence, greater duration of drug use and consumption of more substances. Only Pope et al.26 studied the family history of substance abuse in cannabis consumers, obtaining no differences between the OSU ≤ 16 and OSU ≥ 17 groups. However, our results on the age of OSU are revealing and link with the observation that, for alcoholic patients, younger ages of first use have been associated with worse clinical course of SUD4.
We observed several differences in neuropsychological functioning between groups. Controlling the effect of age and years of education, the OSU ≤ 16 group presented lower premorbid IQ in both the verbal component (VIQ), measured using the Vocabulary subtest and in the performance component (PIQ), measured through the Block Design subtest. These cognitive differences have not been found in cannabis addicts with brief periods of abstinence24. In contrast, consumers with age of OSU ≤ 16 and longer periods of abstinence, more similar to our sample, show lower VIQ26. This suggests that when patients begin consumption at age 17 or later, with the maintenance of abstinence the speed of recovery in global cognitive ability is higher than in those who began consumption at age 16 or earlier.
Two hypotheses might explain the lower IQ of the OSU ≤ 16 group: the existence of a worse cognition prior to consumption or a higher effect of overall neurotoxicity associated to the age of OSU. In the case of lower VIQ, some results seem to be more indicative of the hypothesis of lower cognitive ability prior to consumption: (a) participants in this group had a higher rate of family history of SUD, a characteristic related to the presence of cognitive impairment in their descendants even if the latter have not consumed29; (b) the estimate is made from the Vocabulary subtest, where performance is more preserved after neurological damage, thus making it the most widely accepted as a measure of premorbid cognitive functioning35. In contrast, the origin of the low PIQ raises more questions. In this case, other evidence supports the hypothesis of a greater brain damage arising from SUD: (a) although the Block Design subtest is commonly used as a measure of premorbid PIQ, its performance is sensitive to attacks to the central nervous system37; (b) since this task is related to perceptual organization35, whose neurological substrate shows a critical maturation period prior to age 1638, consumption at age 16 or earlier could promote aberrant synaptic reorganizations that would chronically alter its functionality. However, it is noteworthy that, contrary to this second hypothesis, visuospatial deficits have been found in patients with a family history of SUD11 as well as lower PIQ associated with development of SUD in adulthood39, which would support the hypothesis of a worse premorbid PIQ. Unfortunately, the design of our study does not allow us to clarify these issues at the moment.
In addition, the OSU ≤ 16 group showed lower speed of processing and slower visuoperceptual skills, as well as higher deficits in planning. However, no differences were observed in tasks of attention, verbal memory, working memory, cognitive flexibility or abstract reasoning, nor were there alterations in the processes of risk decision-making. Moreover, when premorbid IQ and duration of drug use were controlled in the analyses, all cognitive differences between groups disappeared. The linear regression analyses with the total sample allowed us to elucidate these results.
At lower PIQ scores, the patients performed worse in the task of visual perception and showed slower processing speed. Therefore, we cannot confirm that consumption at age 16 or earlier is related to higher deficits in these skills since the lower premorbid IQ interferes with their performance.
However, it should be highlighted that the age of OSU also modulated the visuoperceptual performance of the participants: when it was lower, they needed more time to respond to the stimuli in this task. This would support the idea that drug consumption at age 16 or earlier may alter the optimal neurodevelopment and its consequence would imply specific visuoperceptual deficits. Since in our area of study no previous work had considered this cognitive function24,25,26,32, more data are needed to sustain this hypothesis.
Nevertheless, our results indicate that the variable with greater explanatory power regarding planning abilities and processing speed is the duration of drug use. This is consistent with evidence that repeated use of substances is associated with morphological brain changes in both gray and white matter. In polydrug patients, as consumption becomes chronic, it has been observed greater volume reduction in the prefrontal cortex40, associated with planning skills41. In cocaine users, increased abnormalities in the corpus callosum also correlate with greater impulsivity and lack of planning42,43. Therefore, differences in duration of drug use could underlie some results that, unlike ours, have observed different executive functioning and processing speed between the OSU ≤ 16 and OSU ≥ 17 groups25.
The interpretation of our results is subject to limitations. Most of the sample consisted of polydrug users, making it impossible to separate the differential effect of each type of substance on neurocognition16. Although this is a frequent limitation with this type of patients44, in our study its effect is relatively controlled since the groups did not differ in the main substances used. Future studies should considered the main substance associated with the diagnosis of dependence, since it is possible that it plays a role in the explanatory model of performance in visual perception, planning and processing speed, together with the age of OSU, duration of drug use and PIQ. In addition, it would be interesting to incorporate designs that contribute to clarify the etiology and clinical course of cognitive deficits observed in the OSU ≤ 16 group and its relation to clinical severity.
Although our results should be interpreted with caution, they may have clinical implications. SUD patients may benefit from cognitive rehabilitation6,7, because cognitive deficits and clinical course are related12. Therefore, neuropsychological assessment and rehabilitation in SUD treatment programs, especially in patients with OSU ≤ 16, could improve adherence and response to interventions. This is relevant because our results confirm that the duration of drug use is related to cognitive impairment on executive performance and processing speed, which could increase the difficulty of rehabilitation15. Finally, it would be interesting to develop longitudinal studies assessing the presence of cognitive disorders in the OSU ≤ 16 group prior to consumption and, therefore, help to consider this age group as a target population in primary prevention programs.
In conclusion, the cut-off age considered in our study allows us to differentiate typologies of polydrug addicts in relation to their clinical severity and cognitive functioning, so that taking them into consideration could contribute to improve SUD prevention and treatment programs. The OSU ≤ 16 group presents a more severe clinical pattern: higher rates of family history of SUD, greater number of relapses, a consumption pattern characterized by the use of more substances and the need for interment to achieve similar abstinence. They also show lower IQ scores, higher visuoperceptual and planning deficits and slower processing speed. The lower VIQ could be a premorbid characteristic and the lower PIQ and visuoperceptual skills could be either the result of consumption on the neurodevelopment as characteristics prior to the SUD. Further work is required to shed light on this issue. The difficulties in planning and greater slowdown in information processing may be related to the duration of drug use, which make it highly relevant both for the study of neuropsychological characteristics in the field of addictions as well as for tertiary prevention programs.
Methods
Participants
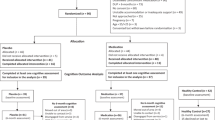
In a cross-sectional study design, we enrolled 80 patients linked to different healthcare resources for SUD treatment. All were male, given the high prevalence of this gender in admissions to treatment for SUD45 and to avoiding bias on the results due to sex differences46. Informed consent was obtained from all participants, who were not compensated for their collaboration in the study.
The inclusion criteria were: current or past diagnosis of SUD, ongoing treatment, confirmed by a diagnostic interview according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revised (DSM-IV-TR)47 criteria, established by their treating clinician or a trained clinical researcher; with abstinence for at least 4 months at the time of the study (excluding caffeine or nicotine consumption), confirmed by urinalysis. The exclusion criteria were: female gender; age below 18 and above 55; presence of mental retardation or pervasive developmental disorder, history of traumatic brain injury or neurological injury, or cognitive or physical impairment that would preclude the correct application of the selected tests; and presence of a comorbid axis I mental disorder confirmed by a diagnostic interview according to DSM-IV-TR criteria.
The patients were added consecutively according to the centers’ referral, without taking into account the OSU variable. After collecting the information, the sample was classified into two groups depending on whether substance use had begun at age 16 or earlier (OSU ≤ 16; n = 41) or at age 17 or later (OSU ≥ 17; n = 39). The age cut-off was based on neurodevelopmental characteristics, similarly to what had been done in previous studies with cannabis consumers28,29,30,31.
Experimental protocol of this study was approved by the University of Barcelona’ ethic committee and the methods were carried out in accordance with the ethical principles of the declaration of Helsinki.
Clinical measures
Information was collected on sociodemographic (age, marital status, educational and economic status) and clinical (presence of organic pathology, psychiatric and substance use family history, suicidal attempts, past treatment for SUD, consumption pattern, type of drugs used, age of onset substance use, duration of drug use, typology of treatment regimen, medication, abstinence periods and relapses) variables, using a structured interview. This information was confirmed with the medical history of the centers database and with the patients treating psychiatrist. Furthermore, daily consumption of cigarettes and caffeine beverages was recorded. The Fagerström test of nicotine dependence48 was administered to smokers. All participants were administered the Clinical Global Impression questionnaire (CGI)49, as a subjective measure of the clinical severity.
Neuropsychological assessment
Cognitive functioning was assessed by a comprehensive battery of cognitive measures, extensively validated and routinely used35. The administration of the tests was distributed into two separate sessions of two hours each, always in a fixed order alternating verbal and manipulative tests. All participants completed the battery. The Vocabulary and Block Design subtests of the Wechsler Adult Intelligence Third Edition Scale Revised (WAIS-III)50 were administered to assess the premorbid VIQ and PIQ, respectively35. Attention span was measured with the Digit Span Subtest of the WAIS-III. The TMT-A51 was administered as a measure of processing speed. We assessed visuospatial perception with the JLOT52, in there computerized version of Estévez-González (2001). Declarative, immediate and delayed memory variables were assessed with the RAVLT53. Finally, we measured the performance in different components of executive functions: the TMT-B51 and the Digits Backwards Subtest of the WAIS-III for the working memory; the Tower of Hanoi54, in there four disk computerized version of González-Vilches (2000) for the planning and problem solving; the WCST55, in there computerized version of Estévez-González (2001), for the cognitive flexibility, reasoning and problem solving; and the IGT56, in there computerized version of Kilgard (1997), for the decision making with risk.
Statistical analysis
Differences between groups in the sociodemographic and clinical variables were explored with the Mann-Whitney U test (U) or with the Chi Square test for categorical variables. If the quantitative data fulfilled the necessary conditions, the Student’s t-test (t) was used; when the conditions were not met, the nonparametric Mann-Whitney U test (U) was used instead.
Differences in neuropsychological performance were assessed using analysis of covariance (ANCOVA), multiple analysis of covariance (MANCOVA) or with repeated measures MANCOVA (RM MANCOVA), depending on the task. The Bonferroni test was applied in all analyses to reduce the occurrence of a type 1 error. The effect size was calculated with the partial Eta squared (ηp2) index, assuming a value of 0.01 as low, of 0.04 as moderate and of 0.1 as high57. Age and years of education were considered as covariates, given their known effects on cognitive performance58,59 and because they presented high standard deviations in both groups.
The two groups differed in duration of drug use and in the scores obtained in the Vocabulary and Block Design subtests of the Wechsler Adult Intelligence Scale-Revised Third Edition (WAIS-III). These subtests are considered measures of premorbid IQ35,60. Moreover, the effects of duration of drug use on neuropsychological performance are well known35,44. Thus, we explored their possible influence on the neuropsychological results, together with age and years of schooling. This was done in two steps. Firstly, the analyses of covariance were repeated for all the cognitive tasks considering the five covariates. Secondly, a confirmatory analysis was performed using a stepwise regression analysis, in order to study their influence on those neuropsychological tasks in which a loss of significance was observed when compared to the first analysis. We consider the total sample, considering the neuropsychological measures as dependent variables and introducing as independent variables the age of OSU, age, years of schooling and duration of consumption and the scores in the Vocabulary and Block Design subtests. Data were analyzed using the Statistical Package for the Social Sciences (SPSS; version 15.0), considering bilateral statistical significance with an established type 1 error at 5% (p < 0.05).
Additional Information
How to cite this article: Capella, M. M. et al. Neuropsychological Performance in Polyconsumer Men Under Treatment. Influence of Age of Onset of Substance Use. Sci. Rep. 5, 12038; doi: 10.1038/srep12038 (2015).
References
United Nations Office on Drugs and Crime. World Drug Report. Vienna: UNODC; 2014. Available at: http://www.unodc.org/unodc/secured/wdr/wdr2013/World_Drug_Report_2013.pdf (Accessed on January 7, 2015).
Palmer, R. H. et al. Developmental epidemiology of drug use and abuse in adolescence and young adulthood: Evidence of generalized risk. Drug Alc. Dep. 102, 78–87; 10.1016/j.drugalcdep.2009.01.012 (2009).
Kreek, M. J. et al. Opiate addiction and cocaine addiction: Underlying molecular neurobiology and genetics. J. Clin. Invest. 122, 3387–3393; 10.1172/jci60390 (2012).
Kendler, K. S., Ohlsson, H., Sundquist, K. & Sundquist, J. A latent class analysis of drug abuse in a national Swedish sample. Psychol. Med. 43, 2169–2178; 10.1017/S0033291713000081 (2013).
Kampman, K. M. et al. A double-blind, placebo-controlled pilot trial of quetiapine for the treatment of Type A and Type B alcoholism. J. Clin. Psychopharmacol. 27, 344–351; 10.1097/jcp.0b013e3180ca86e5 (2007).
Pedrero, E. J. et al. Diferencias de personalidad entre adictos al alcohol y controles emparejados: Relación con sintomatología frontal y subtipos de adictos. Psicothema 23, 100–106 (2011).
Bates, M. E., Buckman, J. F. & Nguyen, T. T. A role for cognitive rehabilitation in increasing the effectiveness of treatment for alcohol use disorders. Neuropsychol. Rev. 23, 27–47; 10.1007/s11065-013-9228-3 (2013).
McGue, M., Iacono, W. G., Legrand, L. N., Malone, S. & Elkins, I. Origins and consequences of age at first drink. Associations with Substance-Use Disorders, disinhibitory behavior and psychopathology and P3 Amplitude. Alcohol Clin. Exp. Res 25, 1156–1165; 10.1111/j.1530-0277.2001.tb02330.x (2001).
Squeglia, L. M., Jacobus, J., Nguyen-Louie, T. T. & Tapert, S. F. Inhibition during early adolescence predicts alcohol and marijuana use by late adolescence. Neuropsychology 28, 782–790; 10.1037/neu0000083 (2014).
Weiland, B. J. et al. Resiliency in adolescents at high risk for substance abuse: flexible adaptation via subthalamic nucleus and linkage to drinking and drug use in early adulthood. Alc. Clin. Exp. Res. 36, 1355–1364; 10.1111/j.1530-0277.2012.01741.x (2012).
Thoma, R. J. et al. Adolescent substance abuse: the effects of alcohol and marijuana on neuropsychological performance. Alc. Clin. Exp. Res. 35, 39–46; 10.1111/j.1530-0277.2010.01320.x (2011).
Passetti, F., Clark, L., Mehta, M. A., Joyce, E. & King, M. Neuropsychological predictors of clinical outcome in opiate addiction. Drug Alc. Dep. 94, 82–91; 10.1016/j.drugalcdep.2007.10.008 (2008).
Fals‐Stewart, W. & Schafer, J. The relationship between length of stay in drug‐free therapeutic communities and neurocognitive functioning. J. Clin. Psychol. 48, 539–543 (1992).
Streeter, C. C. et al. Performance on the Stroop predicts treatment compliance in cocaine-dependent individuals. Neuropsychopharmacology 33, 827–836; 10.1038/sj.npp.1301465 (2008).
Mohamed, S., Bondi, M. W., Kasckow, J. W., Golshan, S. & Jeste, D. V. Neurocognitive functioning in dually diagnosed middle aged and elderly patients with alcoholism and schizophrenia. Int. J. Geriat. Psychiatry 21, 711–718; 10.1002/gps.1528 (2006).
Schweinsburg, A. D., Schweinsburg, B. C., Nagel, B. J., Eyler, L. T. & Tapert, S. F. Neural correlates of verbal learning in adolescent alcohol and marijuana users. Addiction 106, 564–573; 10.1111/j.1360-0443.2010.03197.x (2011).
Madoz-Gúrpide, A., Blasco-Fontecilla, H., Baca-García, E. & Ochoa-Mangado, E. Executive dysfunction in chronic cocaine users: an exploratory study. Drug Alc. Dep. 117, 55–58; 10.1016/j.drugalcdep.2010.11.030 (2011).
Cloninger, C. R. Neurogenetic adaptive mechanisms in alcoholism. Science 236, 410–416; 10.1126/science.2882604 (1987).
Elofson, J., Gongvatana, W. & Carey, K. B. Alcohol use and cerebral white matter compromise in adolescence. Addic. Behav. 38, 2295–2305; 10.1016/j.addbeh.2013.03.001 (2013).
Muñoz, J. J. & Graña, J. L. Las funciones ejecutivas en subtipos de drogodependientes en tratamiento. Psicopatología Clínica, Legal y Forense 11, 29–50 (2011).
Johnson, B. A., Cloninger, C. R., Roache, J. D., Bordnick, P. S. & Ruiz, P. Age of onset as a discriminator between alcoholic subtypes in a treatment‐seeking outpatient population. Am. J. Addic. 9, 17–27; 10.1080/10550490050172191 (2000).
Castellanos-Ryan, N., O’Leary-Barrett, M. & Conrod, P. J. Substance-use in childhood and adolescence: A brief overview of developmental processes and their clinical implications. J. Can. Acad. Child Adolesc. Psychiatry 22, 41–46 (2013).
Crews, F., He, J. & Hodge, C. Adolescent cortical development: A critical period of vulnerability for addiction. Pharmacol. Biochem. Behav. 86, 189–199; 10.1016/j.pbb.2006.12.001 (2007).
Ehrenreich, H. et al. Specific attentional dysfunction in adults following early start of cannabis use. Psychopharmacology 142, 295–301; 10.1007/s002130050892 (1999).
Jockers-Scherübl, M. C. et al. Cannabis induces different cognitive changes in schizophrenic patients and in healthy controls. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 31, 1054–1063; 10.1016/j.pnpbp.2007.03.006 (2007).
Pope, Jr. H. G. et al. Early-onset cannabis use and cognitive deficits: what is the nature of the association? Drug Alc. Dep. 69, 303–310; 10.1016/s0376-8716(02)00334-4 (2003).
Wilson, W. et al. morphological changes and early marijuana use: a magnetic resonance and positron emission tomography study. J. Addict. Dis. 19, 1–22; 10.1300/j069v19n01_01 (2006).
Kunert, H. J., Derichs, G. & Irle, E. Entwicklung von Aufmerksamkeitsfunktionen im Kindesalter: Ergebnisse einer vorläufigen Normierung der computergestützten Testbatterie zur Aufmerksamkeitsprüfung (TAP) an 9- bis 12jährigen Kindern. Zeitschrift Neuropsychol. 7, 92–113 (1996).
Sundram, S. Cannabis and neurodevelopment: implications for psychiatric disorders. Hum. Psychopharmacol. Clin. Exp. 21, 245–254; 10.1002/hup.762 (2006).
Lambe, E. K., Krimer, L. S. & Goldman-Rakic, P. S. Differential postnatal development of catecholamine and serotonin inputs to identified neurons in prefrontal cortex of rhesus monkey. J. Neurosci. 20, 8780–8787 (2000).
Shaw, P. et al. Intellectual ability and cortical development in children and adolescents. Nature 440, 676–679; 10.1038/nature04513 (2006).
Benaiges, I., Serra‐Grabulosa, J. M., Prat, G. & Adan, A. Executive functioning in individuals with schizophrenia and/or cocaine dependence. Hum. Psychopharmacol Clin Exp 28, 29–39; 10.1002/hup.2279 (2013).
West, R. & Gossop, M. Overview: a comparison of withdrawal symptoms from different drug classes. Addiction 89, 148314–89; 10.1111/j.1360-0443.1994.tb03747.x (1994).
Kosten, T. R. & O’ Connor, P. G. Management of drug and alcohol withdrawal. New England J. Med. 348, 1786–1795; 10.1056/nejmra020617 (2003).
Lezak, M. D., Howieson, D. B. & Loring, D. W. Neuropsychological assessment. 4th ed. (Oxford, Oxford University Press, 2004).
Barker, M. J., Greenwood, K. M., Jackson, M. & Crowe, S. F. Cognitive effects of long-term benzodiazepine use. CNS Drugs 18, 37–48; 10.1002/hup.453 (2004).
Nelson, H. E. in The assessment of psychoses: a practical handbook (eds. Barnes, T. R. E. & Nelson, H. E. ) 85–104. London: Chapman and Hall (1994).
Luria, A. R. El cerebro en acción. (Barcelona, Martínez Roca, 1986).
Pechtel, P., Woodman, A. & Lyons-Ruth, K. Early maternal withdrawal and nonverbal childhood IQ as precursors for substance use disorder in young adulthood: Results of a 20-year prospective study. Inter. J. Cognitive Therapy 5, 316–329; 10.1521/ijct.2012.5.3.316 (2012).
Liu, X., Matochik, J. A., Cadet, J. L. & London, E. D. Smaller volume of prefrontal lobe in polysubstance abusers: a magnetic resonance imaging study. Neuropsychopharmacology 18, 243–252; 10.1016/s0893-133x(97)00143-7 (1998).
Fincham, J. M., Carter, C. S., van Veen, V., Stenger, V. A. & Anderson, J. R. Neural mechanisms of planning: a computational analysis using event-related fMRI. Proc. Ntl. Acad. Sc.i USA 99, 3346–3351; 10.1073/pnas.052703399 (2002).
Moeller, F. G. et al. Reduced anterior corpus callosum white matter integrity is related to increased impulsivity and reduced discriminability in cocaine-dependent subjects: diffusion tensor imaging. Neuropsychopharmacology 30, 610–617; 10.1038/sj.npp.1300617 (2004).
Lim, K. O. et al. Brain macrostructural and microstructural abnormalities in cocaine dependence. Drug Alc. Dep. 92, 164–172; 10.1016/j.drugalcdep.2007.07.019 (2008).
Fernández-Serrano, M. J., Pérez-García, M., Río-Valle, J. S. & Verdejo-García, A. Neuropsychological consequences of alcohol and drug abuse on different components of executive functions. J. Psychopharmacol. 24, 1317–1332; 10.1177/0269881109349841 (2010).
Observatorio Español Droga Toxicomanías. Estadísticas 2013: Alcohol, tabaco y drogas ilegales en España. Available at: http://www.pnsd.msc.es/Categoria2/observa/pdf/2_Informe_2013.pdf (Accessed on January 3, 2015).
Nolen-Hoeksema, S. Gender differences in risk factors and consequences for alcohol use and problems. Clin. Psychol. Rev. 24, 981–1010; 10.1016/j.cpr.2004.08.003 (2004).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. text rev. (Washington D. C., American Psychiatric Association, 2000).
Heaterton, T. F., Kozlowski, L. T, Frecker, R. C. & Fagerström, K. O. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance questionnaire. Brit. J. Addic. 86, 1119–1127; 10.1111/j.1360-0443.1991.tb01879.x (1991).
Guy, W. Early Clinical Drug Evaluation (ECDEU) assessment manual. (Rockville, National Institute of Mental Health, 1976).
Wechsler, D. WAIS-III: Escala de Inteligencia Wechsler para Adultos-III. Adaptación española (2nd ed.). (Madrid, TEA Ediciones, 2001).
Reitan, R. The relation of Trail Making Test to organic brain damage. J. Consulting Psychol. 19, 393–394; 10.1037/h0044509 (1995).
Benton, A. L., Hamsher, K., Varney, N. R. & Spreen, O. Contributions to neuropsychological assessment. (New York, Oxford University Press, 1983).
Schmidt, M. Rey auditory Verbal Learning Test: A Handbook. (Lutz F. L., Psychological Assessment Resources, 2011).
Lucas, É. Récréations Mathématiques (III). (Paris, Gauthier-Villars, 1893).
Grant, D. A. & Berg, E. A behavioral analysis of degree of reinforcement and ease of shifting to new responses in a Weigl-type card-sorting problem. J. Exp. Psychol. 38, 404–411; 10.1037/h0059831 (1948).
Bechara, A., Damasio, A. R., Damasio, H. & Anderson, S. W. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 50, 7–15; 10.1016/0010-0277(94)90018-3 (1994).
Huberty, C. J. A history of effect sizes indices. Educa. Psychol. Meas. 62, 227–40; 10.1177/0013164402062002002 (2002).
Voineskos, A. A. et al. Age-related decline in white matter tract integrity and cognitive performance: A DTI tractography and structural equation modeling study. Neurobiol. Aging 33, 21–34; 10.1016/j.neurobiolaging.2010.02.009 (2012).
Salthouse, T. A. Within-cohort age-related differences in cognitive functioning. Psychol. Sci. 24, 123–130; 10.1177/0956797612450893 (2013).
Vanderploeg, R. D. & Schinka, J. A. Predicting WAIS-R IQ premorbid ability: Combining subtest performance and demographic variable predictors. Arch. Clin. Neuropsychol. 10, 225–239; 10.1093/arclin/10.3.225 (1995).
Acknowledgements
This work was supported by grants from the Spanish Ministry of Science and Innovation (PSI2009-12300), the Spanish Ministry of Economy and Competitiveness (PSI2012-32669). We thank the Man Project Foundation in Catalonia, ATRA Association and Mental Health and Addictions Division of the Mataró Hospital for providing the patients in the sample. We are grateful to Silvia López-Vera and Julia Elena Marquez-Arrico who assisted in collecting data.
Author information
Authors and Affiliations
Contributions
A.A. conceived the original idea for the study, sought funding, wrote the protocol and managed the day to day running of the study. M.M.C. and I.B. collected the sample data. M.M.C. carried out all the data analyses. The manuscript was written by M.M.C. and A.A. with input from I.B. All authors have approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Capella, M., Benaiges, I. & Adan, A. Neuropsychological Performance in Polyconsumer Men Under Treatment. Influence of Age of Onset of Substance Use. Sci Rep 5, 12038 (2015). https://doi.org/10.1038/srep12038
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep12038
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.