Abstract
We assessed the incidence of diabetic ketoacidosis (DKA) in children aged <15 years with newly diagnosed type 1 diabetes mellitus (T1DM) in the Auckland Region (New Zealand) in 1999–2013, in a retrospective review of a complete regional cohort. DKA and its severity were classified according to ISPAD 2014 guidelines. Of 730 children presenting with new-onset T1DM over the 15-year time period, 195 cases had DKA of any severity (27%). There was no change in the incidence of DKA or the proportion of children with severe DKA at presentation. The incidence of DKA among children aged <2.0 years (n = 40) was 53% compared to 25% for those aged 2–14 years (n = 690; p = 0.005). In children aged 2–14 years, increasing age at diagnosis was associated with greater likelihood of DKA at presentation (p = 0.025), with the odds of DKA increasing 1.06 times with each year increase in age. Non-Europeans were more likely to present in DKA than New Zealand Europeans (OR 1.52; p = 0.048). Despite a consistent secular trend of increasing incidence of T1DM, there was no reduction in the incidence of DKA in new-onset T1DM in the Auckland Region over time. Thus, it is important to explore ways to reduce DKA risk.
Similar content being viewed by others
Introduction
The most serious complication in newly diagnosed cases with type 1 diabetes mellitus (T1DM) is diabetic ketoacidosis (DKA), the leading cause of death in children with T1DM1. DKA is preceded by a variable period of symptomatic diabetes characterised by weight loss, polyuria and polydipsia. Early insulin replacement prevents DKA, thus the presence and severity of DKA is largely a consequence of delay in diagnosis and initiation of insulin therapy2.
Children with DKA often require prolonged hospitalisation or intensive care. Neuroimaging reveals that a high proportion of patients with DKA at T1DM-onset have evidence of some brain swelling3. Although severe swelling is uncommon, it is associated with 20–30% mortality4,5. Further, DKA is associated with acute reductions of brain volumes, followed by long-term impairment of IQ and short-term memory3,6,7.
Reported risk factors for DKA at presentation include young age, minority ethnicity, poor access to medical care, absence of first-degree relatives with T1DM and lack of medical insurance8. Recent meta-analyses suggest that a higher background incidence of T1DM is associated with a lower risk of DKA in children with newly diagnosed T1DM2,8,9. Although there has been a progressive worldwide increase in the incidence of T1DM10,11, there is conflicting evidence on the associated effects on DKA rates. While some longitudinal studies found this increase to be associated with reduced incidence of DKA12,13, others have not14,15,16.
New Zealand has a social security system that provides medical care free of charge. As a result, income is not a direct impediment for take-up of medical care and the associated costs of T1DM to patients’ families are minimal. We have previously shown that the incidence of T1DM has increased over the last three decades in Auckland, in line with worldwide trends11. Auckland is New Zealand’s major urban centre and its population is ethnically heterogeneous17. Previous cross-sectional data from this urban regional service suggest that the frequency of DKA fell from 63% in 1988-89 to 42% in 1995-9618. However, there have been significant changes in medical services over this extended interval that may have contributed to this improvement.
In the present study, we aimed to determine: i) whether the incidence of DKA at T1DM-onset in children under 15 years in the Auckland Region has changed over the last 15 years (1999–2013); ii) whether the risk of DKA was associated with specific factors, such as age, sex, socioeconomic status and ethnicity.
Methods
Ethics approval
Ethics approval to conduct this study was granted by the Auckland District Health Board Research Review Committee (study number A + 5475, NTX/12/EXP/076). All procedures followed were in accordance with the ethical standards of the responsible committees. Written or verbal informed consent was not required, as this study involved an audit of routine clinical practice.
Participants
Data were collected on all children aged <15 years diagnosed with T1DM and residing within the Auckland Region between 1 January 1999 and 31 December 2013 from the Starship Children’s Hospital Diabetes Database (Starbase). Additional information was obtained from hospital records as required. The Paediatric Diabetes and Endocrinology Service at Starship Children’s Hospital provides specialist care for a total population of approximately 1.5 million, with case ascertainment levels over 95%19.
T1DM was diagnosed based on clinical features. All patients had elevated blood glucose at presentation (a random measurement of >11.1 mmol/l and/or fasting blood glucose >7.1 mmol/l) and presented with classical symptoms. In addition, all patients met at least one of the following criteria: a) DKA; b) presence of pre-T1DM associated antibodies (glutamic acid decarboxylase, islet antigen 2, islet cell, or insulin autoantibodies); or c) on-going requirement for insulin therapy. Subjects with type 2 diabetes, monogenic or other forms of diabetes (e.g. associated with cystic fibrosis) were excluded from this study.
Study parameters
Demographic and anthropometric data were collected at diagnosis. Height was measured to the nearest 0.1 cm using a Harpenden stadiometer (Holtain, Crosswell, UK). Weight was measured to the nearest 0.1 kg, with the participant in light clothing, by electronic scales. Body mass index standard deviation scores (BMI SDS) were calculated based on British 1990 growth reference data20.
Ethnicity was recorded by self-report using a prioritised system, such that if multiple ethnicities were selected, the patient was assigned to a single ethnicity, following a hierarchical classification of Maori, Pacific Islander, Other and then New Zealand European17. “Other” included Indian, South-East Asian, African and Middle Eastern ethnicities. Socioeconomic status was determined using the New Zealand Index of Deprivation 2006 (NZDep2006), a geo-coded deprivation score derived from current residential address21.
Bicarbonate and pH were measured from predominantly venous samples. HbA1c was measured by high-performance liquid chromatography analysis (Bio-Rad Laboratories, CA, USA). DKA occurrence was assessed by blood gases using pH and bicarbonate. DKA severity was categorized according to ISPAD 2014 guidelines22, as mild (venous pH < 7.3 or bicarbonate <15 mmol/l), moderate (pH < 7.2 or bicarbonate <10 mmol/l), or severe (pH < 7.1 or bicarbonate <5 mmol/l). Autoantibodies to glutamic acid decarboxylase and tyrosine phosphatase-like protein were measured using ELISA kits (RSR Ltd, Cardiff, UK).
Statistical analysis
Baseline data were assessed using one-way ANOVA or non-parametric Kruskal-Wallis, while sex ratio and ethnic composition data were compared with chi-square tests. The yearly incidence of DKA was assessed as the percentage of all patients newly diagnosed with T1DM who met the criteria for DKA at presentation. Possible changes in incidence and in biochemical blood parameters over the 15-year period were analysed using Poisson regression.
Among subjects who had DKA at diagnosis, ordinary logistic regressions were carried out to assess whether any independent factors (socioeconomic status, sex, ethnicity and age at diagnosis) were associated with increasing DKA severity. Binary logistic regressions were used to assess whether any of the independent factors were associated with the likelihood of DKA at the time of diagnosis of T1DM throughout the study period.
Linear regression models were used to examine possible associations between the independent factors listed above with glucose, bicarbonate, pH and HbA1c measurements at diagnosis. In order to assess whether changes differed among age groups, data were also analysed separately for children <2 years and those aged 2-14 years. Possible seasonal variations in DKA incidence were assessed using binary logistic regressions (as described above) and chi-square tests; note that Southern Hemisphere seasons were defined on meteorological criteria23. Statistical analyses were carried out using SAS version 9.3 (SAS Institute Inc. Cary NC, USA) and Minitab version 16 (Pennsylvania State University, State College, PA, USA). All statistical tests were two-tailed and maintained at a 5% significance level.
Results
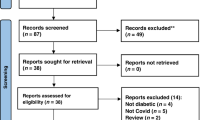
A total of 955 subjects were diagnosed with diabetes over the study period. 104 were either aged ≥15 years or did not reside in the Auckland Region, 90 were cases of type 2 diabetes and 31 were classified as “other” (e.g. monogenic of cystic fibrosis-related diabetes). Thus, over the 15-year period, 730 children aged <15 years were diagnosed with new-onset T1DM. Of these, 195 (27% of cases) had DKA at diagnosis, of whom 92 were classified as mild (47%), 52 as moderate (27%) and 51 as severe (26%). Note that the age at diagnosis among those in DKA increased by approximately 0.22 years per year, from 7.2 years in 1999–2000 to 9.6 years in 2012–2013 (p = 0.002). However, this was a likely reflection of an overall increase in the average age at T1DM diagnosis, which also rose over the study period (p = 0.037, as previously reported11).
The yearly proportion of patients in DKA varied from 19% to 37% (Fig. 1A), but there was no overall change in the incidence of DKA (p = 0.81). When the cohort was assessed as a whole, DKA was not associated with age at diagnosis (p = 0.94), sex (p = 0.09), ethnicity (p = 0.10), or socioeconomic status (p = 0.59). There was also no seasonal variation in DKA incidence (data not shown).
Overall, older age at diagnosis was associated with higher HbA1c (β = 0.296; p < 0.0001) but lower glucose concentrations (β = −0.258; p = 0.018). Non-Europeans had higher HbA1c values (12.7 vs. 11.6%; p = 0.001) and higher glucose concentrations (28.8 vs. 25.9 mmol/l; p = 0.003) than New Zealand Europeans.
Children with DKA displayed similar age at diagnosis, sex ratio, ethnic composition and socioeconomic status to those who were not in DKA (Table 1), but lower BMI by a mean of 0.33 SDS (Table 1). As expected, children in DKA had lower pH and bicarbonate and higher glucose and HbA1c levels than patients who were not in DKA (Table 1).
DKA severity
The proportion of children in severe DKA did not change over the study period (p = 0.48), despite marked variation from year to year (Fig. 1B). The severity of DKA at T1DM diagnosis was unaffected by age or socioeconomic status (Table 2). However, non-Europeans were more likely to have milder DKA at diagnosis than New Zealand Europeans (odds ratio (OR) 1.93; p = 0.032) and there was a possible trend for boys to have milder DKA than girls (OR 1.70; p = 0.056) (Table 2).
Age bands
40 children were aged less than 2 years at diagnosis of T1DM. The incidence of DKA in this age group was 53% (21/40) compared to 25% (174/690) for children aged 2–14 years (p = 0.005). Among those with DKA, 38% of children aged less than 2 years had severe DKA in comparison to 25% of older children (p = 0.34). In this youngest group, HbA1c levels were considerably higher in non-Europeans than in New Zealand Europeans (12.1 vs 8.7%; p = 0.014). In addition, lower socioeconomic status was associated with higher glucose concentrations (p = 0.022).
Among children aged 2 to 14 years (n = 690), increasing age at diagnosis was associated with greater likelihood of being in DKA at presentation (β = 0.058; p = 0.025; Fig. 2), with the odds of DKA increasing 1.06 times with each year increase in age (95% confidence interval 1.01–1.12). As a result, older age was associated with lower pH (β = −0.005; p = 0.0005) and higher HbA1c levels (β = 0.230; p < 0.0001). In this age group, non-Europeans were more likely to be in DKA at presentation than New Zealand Europeans (OR 1.52; p = 0.048), but were more likely to have mild DKA (OR 2.07; p = 0.026). Non-Europeans also had higher HbA1c levels (12.8 vs 11.7%; p = 0.002) and higher glucose concentrations (28.9 vs 25.7 mmol/l; p = 0.002).
Girls aged 2–14 years had lower bicarbonate concentrations (19.0 vs 20.2 mmol/l, respectively; p = 0.027) and higher HbA1c levels (12.6 vs 11.9%, respectively; p = 0.015) than boys. In addition, girls were less likely to have mild DKA than boys (OR 0.46; p = 0.011).
Discussion
In this complete regional population of children newly diagnosed with T1DM, an average of 27% were in DKA at presentation over a 15-year period, but with considerable variation in the annual incidence. The age at diagnosis of DKA increased progressively, reflecting the increased average age at presentation with T1DM. Furthermore, consistent with previous studies24,25,26, the risk of DKA was considerably higher in children aged less than 2 years.
The literature suggests that a higher overall rate of T1DM is associated with a lower risk of DKA at presentation with new-onset T1DM8. For example, a Finnish study observed a relative reduction in the incidence of DKA over a 20-year period, particularly among children < 5 years of age12. In contrast and consistent with the present study, a large prevalence study of > 14,000 children from 106 centres in Germany and Austria observed no change in DKA incidence or severity over a similar period (1995-2007)14. Further, recent nationwide study of 1299 children aged < 15 years with T1DM in France found a continuing high rate of DKA (43.9%)27. Similarly, the SEARCH for Diabetes in Youth Study found that the incidence of DKA (in 5615 cases of T1DM from 0 to 19 years of age) was high and stable from 2002 to 2010 in 5 American centers15.
Over the past 20 years in the greater Auckland region, there has been an apparent improvement and then stabilisation of DKA incidence from 64% in 1988–9, to 42% in 1995–6 and 27% in the present study, with a concomitant reduction in severity of DKA18. This is less than the rate of 38% reported in Western Sydney (Australia) in 1998 to 201028. Further, previous data from 11 European centres9 suggest that the current risk of DKA in Auckland is broadly consistent with its incidence of T1DM. The reasons for the lack of further reduction in the risk of DKA over the last 15 years are unclear. The inverse relationship between rate of T1DM and risk of DKA at onset between countries has been attributed to improved awareness of T1DM amongst families and medical professionals as the condition becomes more common. However, the historical improvement in risk of DKA in Auckland may have been partly related to other factors, such as the development of a specialist Paediatric Diabetes Service for the region, as well as technological advances (e.g. the widespread availability of glucose meters). The lack of further change in risk of DKA in the Auckland region since these changes were introduced suggests that factors beyond ‘awareness’ are important contributors to risk of DKA.
The risk factors for DKA at presentation identified in previous studies include younger age, minority race/ethnicity, lower income, lack of private health insurance and lack of family history of T1DM2,15. The present study is broadly consistent with this background. The youngest presenting patients (aged < 2 years) constituted a relatively small group (5.5% overall), but had a nearly 2-fold greater rate of DKA compared to children aged 2 to 14 years. The most likely reason for the high rate of DKA in toddlers is that it is simply more difficult to recognize polyuria or polydipsia in very young children, who for example, may be still in nappies. Interestingly, amongst the much larger group of children older than 2 year of age (approximately 95% of the cohort), there was a significant overall increase in risk of DKA with greater age, despite the lower average risk compared to toddlers. In contrast with the known increase in risk of secondary DKA in adolescents, the rate of DKA in the present cohort was maximal around 11 years of age. Speculatively, this may reflect greater day to day involvement in toileting and provision of water for younger children by their parents and thus earlier detection of symptoms, balanced by greater self-awareness and earlier reporting of symptoms amongst children older than 11 years.
Non-Europeans aged 2 to 14 years were more likely to be in DKA than New Zealand Europeans. The reasons are unclear, since socioeconomic status did not appear to be a factor, most likely as a result of the universal access to health care in New Zealand. We have previously shown that the secular trend to increased T1DM in Auckland was similar in New Zealand Europeans and Non-Europeans11. Thus, this cannot explain the increased risk of DKA at diagnosis of T1DM. Potentially, it may relate to awareness of T1DM amongst ethnic minorities or cultural-related factors (such as engagement with medical practitioners).
A limitation of the present study is that we were unable to analyse the presence or not of first-degree relatives with T1DM. Previous studies have found a greatly reduced incidence of DKA in children with a first-degree relative with T1DM2,29, supporting the benefits of increased awareness in the prevention of DKA at diabetes diagnosis. In addition, it was not possible to identify any pre-admission visits to primary care prior to T1DM diagnosis.
Nonetheless, our findings, viewed in the context of the lower rate of DKA presentation with greater incidence of T1DM demonstrated in meta-analyses, suggest that increasing community awareness is likely to be central to further reduce the incidence of DKA at presentation8. Unfortunately, there is contradictory evidence for public education campaigns to improve awareness of the symptoms of T1DM. The ‘Parma campaign’ delivered posters, promoting the link between enuresis, polyuria and diabetes to schools, parents and paediatric practices and was associated with a reduction in DKA incidence at diagnosis from 78% to 12.5% over two years30. However, subsequent studies have had mixed results31,32,33.
In conclusion, there has been no reduction in the risk of DKA in children with newly diagnosed T1DM over a 15-year period in the greater Auckland region of New Zealand, despite publically supported health care and a secular trend of increased incidence of T1DM11. This suggests that direct action to improve community and medical awareness of T1DM is needed to further reduce the rate of DKA at the time of diagnosis.
Additional Information
How to cite this article: Jefferies, C. et al. 15-year incidence of diabetic ketoacidosis at onset of type 1 diabetes in children from a regional setting (Auckland, New Zealand). Sci. Rep. 5, 10358; doi: 10.1038/srep10358 (2015).
References
Edge, J. A., Ford-Adams, M. E. & Dunger, D. B. Causes of death in children with insulin dependent diabetes 1990–96. Arch. Dis. Child 81, 318–323, doi:10.1136/adc.81.4.318 (1999).
Usher-Smith, J. A., Thompson, M. J., Sharp, S. J. & Walter, F. M. Factors associated with the presence of diabetic ketoacidosis at diagnosis of diabetes in children and young adults: a systematic review. BMJ 343, d4092, doi:10.1136/bmj.d4092 (2011).
Cameron, F. J. et al. Neurological consequences of diabetic ketoacidosis at initial presentation of type 1 diabetes in a prospective cohort study of children. Diabetes Care 37, 1554–1562, doi:10.2337/dc13-1904 (2014).
Dunger, D. B. et al. ESPE/LWPES consensus statement on diabetic ketoacidosis in children and adolescents. Arch. Dis. Child 89, 188–194, doi:10.1136/adc.2003.044875 (2004).
Glaser, N. et al. Risk factors for cerebral edema in children with diabetic ketoacidosis. The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics. N. Engl. J. Med. 344, 264–269, doi:10.1056/nejm200101253440404 (2001).
Ghetti, S., Lee, J. K., Sims, C. E., Demaster, D. M. & Glaser, N. S. Diabetic ketoacidosis and memory dysfunction in children with type 1 diabetes. J. Pediatr 156, 109–114, doi:10.1016/j.jpeds.2009.07.054 (2010).
Nadebaum, C., Scratch, S. E., Northam, E. A. & Cameron, F. J. Clinical utility of mental state screening as a predictor of intellectual outcomes 6 months after diagnosis of type 1 diabetes. Pediatr Diabetes 13, 632–637, doi:10.1111/j.1399-5448.2012.00870.x (2012).
Usher-Smith, J. A., Thompson, M., Ercole, A. & Walter, F. M. Variation between countries in the frequency of diabetic ketoacidosis at first presentation of type 1 diabetes in children: a systematic review. Diabetologia 55, 2878–2894, doi:10.1007/s00125-012-2690-2 (2012).
Levy-Marchal, C., Patterson, C. C. & Green, A. Geographical variation of presentation at diagnosis of type I diabetes in children: the EURODIAB study. Diabetologia 44 Suppl 3, B75–B80, doi:10.1007/PL00002958 (2001).
The Diamond Project Group. Incidence and trends of childhood Type 1 diabetes worldwide 1990–1999. Diabet Med. 23, 857–866, doi:10.1111/j.1464-5491.2006.01925.x (2006).
Derraik, J. G. et al. Increasing incidence and age at diagnosis among children with type 1 diabetes mellitus over a 20-year period in Auckland (New Zealand). PLoS ONE 7, e32640, doi:10.1371/journal.pone.0032640 (2012).
Hekkala, A., Knip, M. & Veijola, R. Ketoacidosis at diagnosis of type 1 diabetes in children in northern Finland: temporal changes over 20 years. Diabetes Care 30, 861–866, doi:10.2337/dc06-2281 (2007).
de Vries, L. et al. Decrease in frequency of ketoacidosis at diabetes onset over the past two decades - perspectives of a paediatric tertiary care centre. Diabet Med. 29, e170–e175, doi:10.1111/j.1464-5491.2012.03679.x (2012).
Neu, A. et al. Ketoacidosis at diabetes onset is still frequent in children and adolescents: a multicenter analysis of 14,664 patients from 106 institutions. Diabetes Care 32, 1647–1648, doi:10.2337/dc09-0553 (2009).
Dabelea, D. et al. Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for Diabetes in Youth Study. Pediatrics 133, e938–e945, doi:10.1542/peds.2013-2795 (2014).
Schober, E., Rami, B. & Waldhoer, T. Diabetic ketoacidosis at diagnosis in Austrian children in 1989-2008: a population-based analysis. Diabetologia 53, 1057–1061, doi:10.1007/s00125-010-1704-1 (2010).
Carter, P. J. et al. Ethnicity and social deprivation independently influence metabolic control in children with type 1 diabetes. Diabetologia 51, 1835–1842, doi:s10.1007/s00125-008-1106-9 (2008).
Jackson, W. et al. The changing presentation of children with newly diagnosed type 1 diabetes mellitus. Pediatr Diabetes 2, 154-159, doi:10.1034/j.1399-5448.2001.20403.x (2001).
Campbell-Stokes, P. L. & Taylor, B. J. Prospective incidence study of diabetes mellitus in New Zealand children aged 0 to 14 years. Diabetologia 48, 643–648, doi:10.1007/s00125-005-1697-3 (2005).
Delderfield, M. SDS Individual Calculator for British 1990 Growth Reference Data v 1.1, < http://www.phsim.man.ac.uk/SDSCalculator/> (2005).
Salmond, C., Crampton, P. & Atkinson, J. NZDep2006 Index of Deprivation. (Department of Public Health, University of Otago, Wellington, 2007).
Wolfsdorf, J. I. et al. Diabetic ketoacidosis and hyperglycemic hyperosmolar state. Pediatric Diabetes 15, 154–179, doi:10.1111/pedi.12165 (2014).
Trenberth, K. E. What are the seasons? Bull Am. Meteorol. Soc. 64, 1276–1282, (1983).
Lokulo-Sodipe, K., Moon, R. J., Edge, J. A. & Davies, J. H. Identifying targets to reduce the incidence of diabetic ketoacidosis at diagnosis of type 1 diabetes in the UK. Arch. Dis. Child. 99, 438–442, doi:10.1136/archdischild-2013-304818 (2014).
Oyarzabal Irigoyen, M. et al. Ketoacidosis at onset of type 1 diabetes mellitus in pediatric age in Spain and review of the literature. Pediatr Endocrinol Rev. 9, 669–671, (2012).
de Vries, L. et al. Factors associated with diabetic ketoacidosis at onset of Type 1 diabetes in children and adolescents. Diabet Med. 30, 1360–1366, doi:10.1111/dme.12252 (2013).
Choleau, C. et al. Ketoacidosis at diagnosis of type 1 diabetes in French children and adolescents. Diabetes Metab. 40, 137–142, doi:10.1016/j.diabet.2013.11.001 (2014).
Claessen, F. M., Donaghue, K. & Craig, M. Consistently high incidence of diabetic ketoacidosis in children with newly diagnosed type 1 diabetes. Med. J. Aust. 197, 216, doi:10.5694/mja12.10686 (2012).
Marigliano, M. et al. Diabetic ketoacidosis at diagnosis: role of family history and class II HLA genotypes. Eur. J. Endocrinol. 168, 107–111, doi:10.1530/EJE-12-0541 (2013).
Vanelli, M. et al. Effectiveness of a prevention program for diabetic ketoacidosis in children. An 8-year study in schools and private practices. Diabetes Care 22, 7–9, doi:10.2337/diacare.22.1.7 (1999).
Lansdown, A. J. et al. Prevalence of ketoacidosis at diagnosis of childhood onset Type 1 diabetes in Wales from 1991 to 2009 and effect of a publicity campaign. Diabet Med. 29, 1506–1509, doi:10.1111/j.1464-5491.2012.03638.x (2012).
Fritsch, M. et al. Diabetic ketoacidosis at diagnosis in Austrian children: a population-based analysis, 1989-2011. J. Pediatr 163, 1484–1488.e1, doi:10.1016/j.jpeds.2013.06.033 (2013).
King, B. R. et al. A diabetes awareness campaign prevents diabetic ketoacidosis in children at their initial presentation with type 1 diabetes. Pediatr Diabetes 13, 647–651, doi:10.1111/j.1399-5448.2012.00896.x (2012).
Acknowledgements
The Starbase Diabetes Database was designed by Mr C. Hira. We are very grateful for the diligent recording off all new cases of diabetes within our service by the paediatric diabetes nurse specialists, in particular Grace Harris and Rosalie Hornung. The authors have no support or funding to report.
Author information
Authors and Affiliations
Contributions
S.W.C., W.S.C., P.L.H., C.J., A.J.G. and J.G.B.D. conceived and designed the study. S.C., J.B., C.J. and B.B.A. collected and compiled the data. J.G.B.D. analysed the data. C.J., S.W.C., A.J.G., W.S.C. and J.G.B.D. wrote the manuscript, with input from P.L.H.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Jefferies, C., Cutfield, S., Derraik, J. et al. 15-year incidence of diabetic ketoacidosis at onset of type 1 diabetes in children from a regional setting (Auckland, New Zealand). Sci Rep 5, 10358 (2015). https://doi.org/10.1038/srep10358
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep10358
This article is cited by
-
Clinical characteristics of 683 children and adolescents, aged 0–18 years, newly diagnosed with type 1 diabetes mellitus in Henan Province: a single-center study
BMC Pediatrics (2023)
-
Clinical, hormonal, and biochemical characteristics of 70 chinese children with moderate to severe type 1 diabetic ketoacidosis
BMC Endocrine Disorders (2022)
-
Management of severe inaugural diabetic ketoacidosis in paediatric intensive care: retrospective comparison of two protocols
European Journal of Pediatrics (2022)
-
The relationship between hyperchloremia and acute kidney injury in pediatric diabetic ketoacidosis and its impact on clinical outcomes
Pediatric Nephrology (2022)
-
Management of Diabetic Ketoacidosis in Children and Adolescents with Type 1 Diabetes Mellitus
Pediatric Drugs (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.