Abstract
To discern if physical function test are better mortality predictors than muscle mass in elderly hospitalized patients, we analyzed the prognostic value of muscle mass malnutrition and compared it with physical muscle function tests, including the six-minute walking test (6MWT) and hand grip strength. We included the ankle brachial index (ABI) to assess arterial disease, related to muscle atrophy due to hypoperfusion. We also analyzed the relationship of ABI with malnutrition, physical function tests and survival. We studied 310 hospitalized patients older than 60 years. To assess nutritional status, we determined BMI, triceps skinfold and mid-arm muscle area; we performed a subjective nutritional assessment; and evaluated the degree of inflammatory stress. We assessed physical function by hand grip strength and 6MWT. We evaluated arterial disease by ABI. Forty-one patients died during hospitalization; 269 were discharged and followed for a mean 808 days, reaching a mortality of 49%. Muscle malnutrition was frequent and was related to mortality, but the best predictors were physical function tests: inability to perform the 6MWT and low handgrip strength. Function tests were closely related to each other and correlated with nutritional data. Reduced ABI was related to impaired nutritional status, physical function tests and mortality.
Similar content being viewed by others
Introduction
Malnutrition is frequent among elderly hospitalized patients and is related to prognosis. In this regard, muscle and serum protein levels are more relevant than fat stores1,2. Muscle protein may be assessed as a mass amount by mid-arm anthropometry, for example, or by physical function assessment including stair climbing ability, handgrip strength or distance covered in a walking test. Regarding prognosis, poor performance in physical function tests is related to mortality in the same way as loss of muscle mass is2,3,4,5,6,7.
Sarcopenia is the age-related loss of muscle mass and function8,9. There are three main conditions which lead to sarcopenia: first, starvation or semi-starvation, with a negative balance of calories and protein; second, an inflammatory disease with associated active protein degradation (sarcopenic cachexia); and third, muscle atrophy secondary to neuromuscular impairment, reduced mobility or chronic hypoxia induced by arteriosclerosis. All these conditions are closely related to ageing.
As function tests may assess muscle quality, their relationship with prognosis would be better than that of muscle mass. Our objective is to compare, in elderly hospitalized patients, the prognostic value of muscle mass estimated by mid-arm anthropometrics and subjective assessment with muscle function estimated by the ability to climb stairs, handgrip strength and the 6 minute walking test (6MWT). In addition, as the relationship between arteriosclerosis and sarcopenia has not been extensively studied, we included the ankle brachial index (ABI), a noninvasive test, to evaluate possible muscle atrophy related to arteriosclerotic low blood flow and its possible relationship with muscle malnutrition, loss of physical function and prognosis10,11,12.
Methods
In an observational study, we included 310 consecutively admitted patients older than 60 years, hospitalized in the Internal Medicine Department of the Hospital Universitario de Canarias; 159 men and 151 women aged 61–99 years.
Comorbidity
Diseases were categorized and recorded according to diagnoses at medical reports. They included previous cardiovascular diseases: coronary disease, 67 (21.6%), stroke, 59 (19%) and peripheral arterial disease, 73 (23.5%), as well as cardiovascular risk factors: hypertension, 87 (21.1%), hyperlipidemia, 145 (46.82%), obesity (BMI > 30 kg/m2), 87 (28.1%), diabetes mellitus, 142 (45.8%) and smoking, 92 (29.7%).
Other diseases were: congestive heart failure, 134 (43%); COPD, 66 (21.3%); cancer, 39 (12.6%); alcohol abuse, 36 (11.6%); liver cirrhosis, 14 (4.5%); renal failure, 144 patients (46.5%); and dementia in 39 (12.5%). The most frequent infections at admission were pneumonia, detected in 95 (30.6%) and urinary tract infection in 44 cases (14.2%); sepsis, was present in 134 cases (43.2%). Charlson's comorbidity index (without age) was also calculated13.
Nutritional assessment
We inquired about anorexia and weight loss in the year preceding admission. Dietary changes were classified as reduced intake and only liquid consumption. BMI was calculated at admission as weight/height2. We measured mid-arm circumference (MAC) and triceps skinfold (TSF) using a Holtain lipocaliper and calculated mid-arm muscle area (MAMA). Anthropometric parameters were compared within sex and age categories for the adult population of the Western Canary Islands14.
Subjective nutritional assessment included examination of the muscle mass of the upper and lower limbs and of the temporal muscle, defining two degrees of atrophy (severe, moderate) and absence of atrophy. We assigned 2, 1 and 0 points to each category, respectively. Bichat's pad and subcutaneous fat atrophy were scored in the same way. Thus, a subjective nutritional score was obtained for each patient based on the sum of the assigned points. As previously reported, a score of 0 to 2 was considered normal, 3–4 points indicated mild malnutrition and higher than 4 points indicated severe malnutrition15.
Clinical stress was classified as one of three categories: high when the patient presented hyper-metabolic hyper-catabolic disease such as severe sepsis or septic shock, severe pancreatitis or “delirium tremens”; moderate in the case of non-complicated inflammatory problems such as pneumonia, urinary tract infection, heart failure or arthritis and low in the absence of these conditions16. Samples for blood analysis were taken at 08.00 in the morning after admission. We determined nutritional data including cholesterol, triglyceride, B12 and folate levels; we also included acute phase reactants such as serum albumin, alpha1antitrypsin and C Reactive Protein (CRP).
Physical function assessment
In the first two days after admission, dominant arm hand grip strength was determined using a Collin's dynamometer, selecting the best of three measurements17. We assessed mobility as the self-reported ability to climb stairs and to walk without aid at discharge. The 6MWT employed was that standardized by the ATS18. It was performed when patients were cooperative before discharge. In 135 patients it was not possible to perform the test due to limited physical conditions; in this case it was computed as a result of 0 meters.
Ankle Brachial Index (ABI)
Doppler ultrasound (HADECO ES-100 Kawasaki, Japan) was used to measure bilateral systolic blood pressure (SBP) of the brachial, tibial and dorsal pedal arteries. ABI was calculated as the quotient between the highest SBP of pedal or tibial arteries in each lower limb and the highest SBP of the upper limbs. The lowest ABI of the two legs was used. We considered an ABI value between 0.9 and 1.3 as normal10,11,12,19.
Statistical analysis (SPSS15.0)
Variables were analyzed by Chi-2, Student t test and Pearson r correlation. Stepwise logistic regression was performed to analyze which parameters yielded independent predictive value on hospital survival. After discharge, patients were followed by telephone to know the status (alive or dead) and the survival time. Kaplan-Meier curves and log rank test were performed to assess differences in long-term survival and Cox regression analysis to discern which parameters had independent prognostic value.
Methods were carried out in accordance with approved guidelines. The study was approved by the Hospital Universitario de Canarias Research and Ethics Board; informed consent was obtained from all patients or its relatives in the case of confusion or dementia.
Results
Of the 310 patients included, 41 (13.2%) died during hospitalization. Of the 269 discharged patients, Kaplan- Meyer survival curves showed a mortality rate of 49% after a mean follow-up of 808 ± 40 days (including deceased patients).
Table 1 shows the prognostic value of previous vascular events, ABI, nutritional status, physical function capacity, acute phase reaction and diseases.
We did not find significant sex or age differences in mortality during hospitalization. However, patients older than 80 years showed worse subjective nutritional score, impaired hand grip strength, less distance covered in the 6MWT and lower survival after discharge.
Arterial disease
Sixty-seven (21.6%) patients were previously diagnosed with coronary disease; 59 (19%) with stroke and 73 (23.5%) with peripheral arterial disease. In these cases we found no relationship with mortality during hospitalization or after discharge.
ABI was determined in 300 patients. Values were over 1.3 in 31 (10.3%), between 1.3 and 0.9 in 156 (52%) and below 0.9 in 113 (37.7%): between 0.9 and 0.5 in 77 (25.6%) and below 0.5 in 36 (12%) patients. As shown in Table 1, patients with an ABI value under 0.5 showed increased mortality both in hospital and after discharge. Patients with stroke or peripheral arterial disease showed lower ABI (p = 0.001 in both cases).
Nutritional status
According to the subjective nutritional assessment, 112 (36.1%) were normal, 64 (20.6%) had moderate malnutrition and 134 (43.2%) had severe malnutrition. Body mass index (BMI) was determined in 286 patients; 14 (4.9%) patients were under 20 kg/m2 (low weight); 89 (31.1%) between 20 and 25 kg/m2 (normal); 105 (36.7%) between 25 and 30 kg/m2 (overweight); and 78 (27.3%) with a BMI above 30 Kg/m2 were obese. With respect to mid-arm anthropometrics, MAC was under the 10th percentile of the health reference population in 111 (35.9%); MAMA was under the 10th percentile in 147 (47.6%); and TSF was under the 10th percentile in 16 (5.2%) patients. Regarding serum lipids levels, 7 patients (2.3%) showed serum cholesterol levels over 250 mg/dl, 44 (14.2%) between 200 and 250 mg/dl and 29 (9.5%) below 100 mg/dl; and 98 patients (32%) showed serum triglyceride over 150 mg/dl. Low serum vitamin B12 levels (<170 pg/ml) were observed only in 8 (2.7%) and low serum folate levels (<3 ng/ml) in 57 (19.1%) patients.
As shown in Table 1, patients with better nutritional status showed better short and long term prognosis. It is noteworthy that patients with a BMI over 25 kg/m2 showed better long term survival. Moreover, obese patients with a BMI over 30 kg/m2 showed better long term prognosis when compared with those with normal weight (BMI 20–25 kg/m2) (p = 0.022) and those with low weight (BMI < 20 kg/m2) (p = 0.009). Overweight patients (BMI 25–30 kg/m2) also had better long term survival than those with a normal BMI (20–25 kg/m2) and those with low BMI (<20 kg/m2). Obese and overweight patients showed less weight loss, better subjective nutritional score, higher MAMA, handgrip strength and serum albumin levels.
Physical function assessment
The study of physical function capacity showed low handgrip strength in many patients: 140 (45%) of the men and women had handgrip strength under 10 and 5 lbs, respectively. Similarly poor results were obtained with the walking test: 135 (43.5%) patients were unable to perform the test and 60 (19.4%) walked less than 150 m; only 115 (37.1%) walked between 150 and 750 m in six minutes. Similarly, 140 (45.2%) patients did not climb stairs and of the 269 discharged, 61 (22.7%) did not walk at all and 86 (32%) were unable to walk without aid at discharge. A good physical function capacity was related to improved survival. Thus, patients with better results for handgrip strength, ability to walk at discharge or to climb stairs and distance covered at 6MWT, showed better short and long term prognosis.
Handgrip strength and ability to walk were closely related to each other and both to nutritional status, especially to muscle and serum protein data (Tables 2 and 3). Arterial disease, assessed as an ABI value less than 0.5, was also related to worse nutritional status, impaired handgrip strength, reduced ability to walk (Tables 2 and 3) and to worse short and long term prognosis (Table 1).
Acute phase reaction
Eighty patients (28.1%) showed serum albumin under 3 g/dl with an in- hospital mortality rate of 23.3%; low serum albumin levels were also related with increased mortality after discharge. C reactive protein higher than 90 mg/dl was observed in 58 (19%) cases, with a hospital mortality rate of 24.1%. Alpha1antitrypsin levels over 250 mg/dl did not show any relationship with in-hospital mortality, only after discharge. Moreover, the 50 (16.1%) patients with diseases involving severe inflammatory stress showed increased short term mortality (28%) and long term mortality, as shown in Table 1.
At table 3 we show how serum albumin levels correlated with the nutritional status and the muscle physical function tests and inversely with the Charlson comorbiditiy index.
Diseases
Sepsis and urinary tract infection were related with higher in-hospital mortality, but not after discharge. Cancer, dementia, renal failure and a Charlson index of more than five points were related to higher mortality, both during hospitalization and after discharge (Table 1).
Multivariate analysis
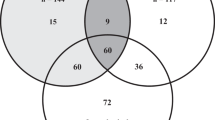
At table 3 we can observe by correlation analysis how nutritional status (subjective nutritional score, global and muscle component), muscle physical function tests (hand grip and walking test), acute phase reaction (serum albumin), ankle brachial index and comorbidity Charlson index, are all variables that significantly correlated among them. So, as nutritional status becomes impaired and physical function declines serum albumin decreases. An ABI lower than 0.5 is related to an impaired nutritional status and physical function tests, decreased serum albumin and increased Charlson index.
To determine which variables had independent short term prognostic value for in-hospital mortality, we included in a logistic regression analysis, age ≥ 80 years, subjective nutritional score >4, serum albumin under 3 g/dl, clinically assessed high degree of stress, inability to perform the 6MWT, handgrip strength below the 50th percentile, ABI less than 0.5, sepsis, cancer and Charlson index over 5 points. The following variables showed independent prognostic value: inability to perform the 6MWT, handgrip strength below the 50th percentile, sepsis, cancer, serum albumin under 3 mg/dl, high degree of inflammatory stress and Charlson index over 5 points (Table 4).
Similarly, to determine which variables had independent prognostic value for post-discharge mortality, we performed a survival analysis with covariates (Cox regression) including the same list of variables (except for sepsis). Those with independent prognostic value were: subjective nutritional score greater than 4 points, inability to perform the 6MWT, cancer, Charlson index over 5 points and ABI less than 0.5 (Table 4).
Discussion
We found a high mortality rate, 13.2% in hospital and 49% after discharge, which is related to aging, comorbidity and malnutrition. Elderly hospitalized patients frequently suffer from malnutrition and sarcopenia, which may be induced by negative caloric protein balance, active proteolysis and muscle atrophy by neuromuscular disorders, inactivity or low blood flow. All these factors were present in our study. We observed anorexia related to weight loss. Besides high comorbidity, with a mean Charlson index of 5, more than half our patients had hyper catabolic diseases, such as infections and sepsis with a high inflammatory component, in which active protein degradation may result in sarcopenic cachexia with low serum albumin levels. Furthermore, around half our patients were unable to perform the 6MWT or could not walk without aid at discharge and such incapacity can lead to more muscle atrophy due to inactivity. Also, patients with peripheral arterial disease and low ABI may suffer muscle atrophy by hypoperfusion; 12% of our patients showed ABI values below 0.5, a very low ABI, which is related with decreased muscle mass, handgrip strength and shorter distance covered in the 6MWT (Table 2).
Malnutrition and obesity paradox
The high prevalence of malnutrition (nearly 40%) was not reflected by BMI results. Only 14 patients (5%) had a BMI under 20 kg/m2, the habitual cut-off point for malnutrition. Moreover, among patients with a BMI between 20 and 25 kg/m2, considered normal, there was a high proportion with malnutrition: 50.6% according to MAMA values. So, in elderly hospitalized patients, a BMI below 20 kg/m2 as a criterion of malnutrition lacks sensitivity and a BMI between 20 and 25 kg/m2 is no guarantee of a normal nutritional status1,2. Moreover, patients with a BMI between 20 and 25 kg/m2 had worse long term survival that those with overweight or obesity. This is known as the obesity paradox and is explained by better nutritional status regarding muscle in overweight and obese patients, pointing to the greater importance of muscle loss compared with fat1,2.
Loss of physical function and prognosis
Physical function capacities depend on nutritional status. So muscle malnutrition may be estimated by muscle function. Moreover, as shown in Table 1, abilities related to muscle function, such as the ability to climb stairs or to walk without aid at discharge, handgrip strength and the distance covered during 6MWT are better predictors of short- and long-term mortality than muscle mass. In our study, all these abilities were related to each other and to nutritional status. Thus, when nutritional status is impaired, physical abilities decline.
The poor general physical condition of our elderly, pluripathologic and malnourished patients conditioned their impaired ability to climb stairs and to perform the six minute walking test, as found in 45% and 44% of our patients, respectively. Moreover, as in other studies, incapacity to perform the 6MWT was a main marker of poor prognosis6,20,21 and the probability of early mortality has been related to gait speed22.
Handgrip strength is a very simple and inexpensive way to assess muscle capacity. Table 2 and 3 shows the close relationship between impaired 6MWT, handgrip strength and nutrition. Many studies have stressed the value of handgrip on prognosis1,2,3,4,5,23 even, as Ling CH et al reported (2013), in very old subjects24. Mid-life muscle strength predicted longevity in a 44-year prospective study25. Handgrip also predicts the recovery of walking capacity after hip fracture surgery26. Besides diseases, represented by sepsis, cancer and Charlson comorbidity index, nutritional status and physical functional tests were independent predictors of mortality in our study, which highlights the importance of performing such functional tests. In this way, Vetrano DL et al (2014) recently report that sarcopenia is a prevalent condition among older adults admitted to acute care wards and it is associated with increased short- and long-term mortality in hospitalized older adults27.
Vascular disease, a low ABI, is related to malnutrition and prognosis
In our sample, there was a high prevalence (48%) of vascular disease. As consequence, diminished ABI (<0.9) was found in 38%, a figure very much higher than that observed in asymptomatic elderly people, about 2–5%11,28 but more similar to the 29% reported by Pasqualini et al (2012) or the 36% reported by Antonopoulos et al (2005), both studies in patients over 50 years admitted to an internal medicine department10,29.
Patients with a severely decreased ABI - below 0.5 - showed impaired nutritional status with lower MAMA, subjective nutritional score, hand grip strength, distance covered on the walking test, decreased serum albumin, perhaps as expression of acute response and increased mortality. Besides vascular events, age-related arterial disease reduces the blood flow and oxygenation of limb muscles, leading to atrophy and sarcopenia. There are few studies on ABI and malnutrition. Ochi M et al (2010) reported a relationship between carotid atherosclerosis and arterial stiffness with diminished mid-thigh muscle mass30. Sampaio RA et al (2014) reported a relationship between arterial stiffness and a low skeletal muscle mass. Moreover, patients with low skeletal mass showed poorer physical performance (handgrip strength and walking speed)31. The relation of arteriosclerosis with malnutrition and sarcopenia adds a new dimension to the study of malnutrition in the elderly. In elderly pluripathologic patients, a decreased ABI may not only be a sign of peripheral arterial disease but also an indicator of malnutrition and impaired physical function.
Multivariate assessment
In recent years, we have witnessed a progressive increase in age and comorbidity of patients admitted to general hospital wards and a parallel increase in the prevalence of malnutrition and loss of physical function. Malnutrition-sarcopenia syndrome, has been defined by the following five criteria: recent history of reduced appetite and poor food intake; unintentional weight loss; low muscle mass; decreased gait speed; and reduced hand grip strength32. All these criteria were highly prevalent among our patients.
We found a close relationship between functional abilities and nutritional status, especially muscle mass. Patients with better hand grip and ability to walk and climb stairs showed better nutritional status. In contrast, patients with less muscle mass showed impaired function. Moreover, multivariate analysis showed that physical function capacities, such as handgrip and walking test ability and ABI as an indicator of vascular disease, had prognostic value for mortality, independently of nutrition and disease (table 4). It has been proposed that ABI should be measured in all elderly patients admitted to general medical care11. On the other hand, a battery of tests has been proposed to assess physical function, frailty and sarcopenia5. Because of its relationship with nutritional status, physical function and mortality, ABI should be included in this battery of tests in addition to physical function tests for elderly patients admitted to general medical care departments.
As shown in table 3 our results disentangle a complex network of interrelated factors afecting nutritional status, sarcopenia, physical function, frailty, vascular disease and mortality in the elderly. Dietary measures alone may be insufficient to reverse or avoid sarcopenia. They must be combined with adequate activity and aerobic exercise to improve muscle oxygenation, muscle mass and physical function capacities33. Moreover, adequate physical activity may improve cardiovascular health34. Muscle loss related to vascular disease and low ABI, which were highly prevalent in our elderly patients, indicate the importance of muscle trophic preservation not only with adequate food intake, but avoiding inactivity and promoting exercise to maintain appropriate blood supply and nervous stimuli. Thus, not only survival could be improved but also autonomy and quality of life, which are dependent on muscle mass and physical function.
References
Martín-Ponce, E. et al. Factors involved in the paradox of reverse epidemiology. Clin. Nutr. 29, 501–506 (2010).
Casas-Vara, A. et al. The obesity paradox in elderly patients with heart failure: analysis of nutritional status. Nutrition 28, 616–622 (2012).
Vecchiarino, P., Bohannon, R. W., Ferullo, J. & Maljanian, R. Short-term outcomes and their predictors for patients hospitalized with community-acquired pneumonia. Heart & Lung. 33, 301–307 (2004).
Norman, K., Stobäus, N., Gonzalez, M. C., Schulzke, J. D. & Pirlich, M. Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr 30, 135–42 (2011).
De Buyser, S. L. et al. Physical function measurements predict mortality in ambulatory older men. Eur J Clin Invest 43, 379–386 (2013).
Taekema, D. G., Gussekloo, J., Westendorp, R. G., de Craen, A. J. & Maier, A. B. Predicting survival in oldest old people. Am. J. Med. 125, 1188–1194 (2012).
Studenski, S. et al. Gait Speed and Survival in Older Adults. JAMA 305, 50–58 (2011).
Roubenoff, R. Sarcopenia: a major modifiable cause of frailty in the elderly. J. Nutr. Health. Aging 4, 140–142 (2000).
Vanitallie, T. B. Frailty in the elderly: contributions of sarcopenia and visceral protein depletion. Metabolism 52, 22–26 (2003).
Pasqualini, L. et al. Prognostic value of low and high ankle-brachial index in hospitalized medical patients. Eur. J. Intern. Med. 23, 240–244 (2012).
Taylor-Piliae, R. E. et al. Ankle brachial index screening in asymptomatic older adults. Am. Heart. J. 161, 979–985 (2011).
Sheng, C. S. et al. Four-limb blood pressure as predictors of mortality in elderly Chinese. Hypertension. 61, 1155–1160 (2013).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic. Dis. 40, 373–383 (1987).
González-Hermoso, F., Porta, R. & Herrero, A. Resultados del estudio antropométrico de la población canaria adulta. Nutr. Hosp. 5, 238–247 (1990).
Tormo, A. et al. Short-term prognostic value of subjective nutritional assessment in general medical patients. J. Nutr. Med. 4, 287–295 (1994).
Kalantar-Zadeh, K., Kopple, J. D., Humphreys, M. H. & Block, G. Comparing outcome predictability of markers of malnutrition-inflammation complex syndrome in haemodialysis patients. Nephrol. Dial. Transplant. 19, 1507–1519 (2004).
Chau, N. et al. Comparison between estimates of hand volume and hand strengths with sex and age with and without anthropometric data in healthy working people. Eur. J. Epidemiol. 13, 309–316 (1997).
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am. J. Respir. Crit. Care. Med. 166, 111–117 (2002).
Ghannam, M., Rodriguez, Y., Ehrmann, D. & Grossman, P. M. Ankle-brachial index as a clinical tool. Am. J. Med. 125, 1171–1172 (2012).
Mutikainen, S. et al. Walking ability and all-cause mortality in older women. Int. J. Sports. Med. 32, 216–222 (2011).
De Feo, S. et al. The inability to perform a 6 minute walking test after cardio-thoracic surgery is a marker of clinical severity and poor outcome. Data from the ISYDE-2008 Italian survey. Int. J. Cardiol. 151, 115–116 (2011).
Stanaway, F. F. et al. How fast does the Grim Reaper walk? Receiver operating characteristics curve analysis in healthy men aged 70 and over. B.M.J. 343, d7679 (2011).
Suárez-Santamaría, M. et al. Prognostic value of inflammatory markers (notably cytokines and procalcitonin), nutritional assessment and organ function in patients with sepsis. Eur. Cytokine Netw. 21, 19–26 (2010).
Ling, C. H. et al. Handgrip strength and mortality in the oldest old population: the Leiden 85-plus study. C.M.A.J. 182, 429–435 (2010).
Rantanen, T. et al. Midlife muscle strength and human longevity up to age 100 years: a 44-year prospective study among a decedent cohort. Age (Dordr) 34, 563–570 (2012).
Savino, E. et al. Handgrip strength predicts persistent walking recovery after hip fracture surgery. Am. J. Med. 126, 1068–1075 (2013).
Vetrano, D. L. et al. Association of Sarcopenia With Short- and Long-term Mortality in Older Adults Admitted to Acute Care Wards: Results From the CRIME Study. J. Gerontol. A. Biol. Sci. Med. Sci. 69, 1154–1161 (2014).
Naqvi, A. Z., Davis, R. B. & Mukamal, K. J. Nutrient intake and peripheral artery disease in adults: Key considerations in cross-sectional studies. Clin. Nutr. 33, 443–447 (2014).
Antonopoulos, S. et al. High prevalence of subclinical peripheral artery disease in Greek hospitalized patients. Eur. J. Intern. Med. 16, 187–191 (2005).
Ochi, M. et al. Arterial stiffness is associated with low thigh muscle mass in middle-aged to elderly men. Atherosclerosis 212, 327–332 (2010).
Sampaio, R. A. et al. Arterial stiffness is associated with low skeletal muscle mass in Japanese community-dwelling older adults. Geriatr. Gerontol. Int. 14 (Suppl. 1), 109–114 (2014).
Vandewoude, M. F., Alish, C. J., Sauer, A. C. & Hegazi, R. A. Malnutrition-sarcopenia syndrome: is this the future of nutrition screening and assessment for older adults? J. Aging Res. 2012, 651570 (2012).
Umanskaya, A. et al. Genetically enhancing mitochondrial antioxidant activity improves muscle function in aging. Proc Natl Acad Sci USA 111, 15250–15255 (2014).
Santulli, G., Ciccarelli, M., Trimarco, B. & Iaccarino, G. Physical activity ameliorates cardiovascular health in elderly subjects: the functional role of the β adrenergic system. Front Physiol. 209, 1–7 (2013).
Author information
Authors and Affiliations
Contributions
E.M.P. and I.H.B. collected, analyzed and interpreted the data and followed up the patients, R.H.L. helped to collect and analyze the data; F.S. participated in the design of the study, in the analysis and interpretation of the data and wrote the manuscript; A.M.R. helped in the conception of the study and in the analysis and interpretation of the results; E.G.R. collaborated in the conception and interpretation of the results and revised the manuscript. All the authors have substantially contributed to this paper: conception and design of the study, acquisition of data, analysis and interpretation of the data. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Martín-Ponce, E., Hernández-Betancor, I., González-Reimers, E. et al. Prognostic value of physical function tests: hand grip strength and six-minute walking test in elderly hospitalized patients. Sci Rep 4, 7530 (2014). https://doi.org/10.1038/srep07530
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07530
This article is cited by
-
Effect of comprehensive geriatric assessment for frail elderly patients operated for colorectal cancer—the colorectal cancer frailty study: study protocol for a randomized, controlled, multicentre trial
Trials (2022)
-
Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) diet in relation to age-associated poor muscle strength; a cross-sectional study from the Kurdish cohort study
Scientific Reports (2022)
-
Cross-sectional analysis of myosteatosis and physical function in pretreatment head and neck cancer patients
Supportive Care in Cancer (2022)
-
Case–control study of the correlation between the five times sit to stand and 6-min walk distance in patients with pancreatic cancer
Supportive Care in Cancer (2022)
-
Treat-to-target in axial spondyloarthritis — what about physical function and activity?
Nature Reviews Rheumatology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.