Abstract
The aim of this study was to investigate the contribution of chromosomal anomalies and the frequency of particular types of aberrations in general couples preparing for pregnancy and make recommendations for pregnancy on the basis of the medical literature. A total of 6,198 general couples were included in the present study. The karyotypes were generated from the peripheral blood lymphocyte cultures and the cytogenetic analysis was performed using G-banding. In 12,396 cases, chromosomal anomalies were detected in 59 cases (0.48%, 59/12,396). Among of them, the frequency of translocation was 0.35% (n = 43). Sex chromosomal anomalies accounted for 0.07% (n = 9), including Klinefelter syndrome (KS) (n = 4), Turner syndrome (TS) (n = 4) and XYY syndrome (n = 1). The others, including inversions (n = 6) and deletion (n = 1), accounted for 0.06%. Our study indicates that clinically important chromosomal defects are present at a remarkable frequency in the general couples in eastern China, suggesting pre-pregnancy cytogenetic analysis should be routinely performed among general couples in this area so that informed decision can be made, which will help to improve the quality of the pregnancy.
Similar content being viewed by others
Introduction
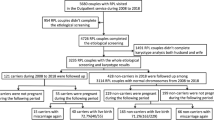
Generally, the couples planning for their first pregnancy have no information related to reproductive problems. The reproducing disorders are the relatively common problem that affects couples worldwide. It is estimated that approximately one in six couples experiences difficulties in reproducing1. It was reported that the frequency of chromosomal aberrations is approximately 8% in cases suffering reproductive failure such as infertility and pregnancy losses2, while it is 0.6% in general population3, the majority of whom wouldn't do cytogenetic analysis before encountering reproductive problems. In Zhenjiang City in eastern China, the cradle of the Chinese Wu culture and the region of the fastest-growing economy in China, the local government sponsors every couple for cytogenetic karyotype analysis before pregnancy if they would like to. The couples can chose one of the following three government-assigned institutes to do cytogenetic analysis: Zhenjiang Family Planning Guidance Institute, Zhenjiang Jingkou District Family Planning Guidance Station and Department of Reproductive &Genetics, the Fourth Affiliated Hospital of Jiangsu University. Here, we report the contribution of chromosomal anomalies and the frequency of particular types of aberrations in general couples preparing for pregnancy, some suggestions are also made on the basis of the present study combining the medical literatures.
Results
A total of 6,198 couples (i.e. 12,396 cases) were evaluated during 1990–2010. Chromosome anomalies were found in 59 cases (0.48%, 59/12,396) (Table 1). Sex chromosome disorders were found in nine cases (15.3%, 9/59), including eight aneuploidy cases and one isochromosome of Xq (Table 2). Translocations were detected in 43 cases (72.9%, 43/59), including 33 balanced translocations and 10 robertsonian translocations. The other structural chromosomal anomalies, including inversions and deletion, were seen in seven cases (11.9%, 7/59) (Table 3). Totally, the incidence of the sex chromosome disorders and the structural chromosomal abnormalities were 0.08% (9/12,396) and 0.4% (50/12,396), respectively.
Discussion
The present study investigated the incidence of chromosomal abnormalities in 6,198 couples i.e. 12,396 cases. Overall, 0.48% of the cases were found to have chromosomal aberration. Chromosomal disorder is closely related to reproductive abnormalities according to previous literatures2,3,4,5,6. Chromosomal abnormalities, such as trisomy, reciprocal translocation, Robertsonian translocation, chromosomal inversion and chromosomal deletion, could be the main factors related to the bad reproductive ending event7. The goal of pre-pregnancy cytogenetic tests is to uncover potential genetic defects in the prospective parents, thus helping them make informed decision about the planned pregnancy. For example, balanced reciprocal translocations carriers should undergo prenatal diagnosis to rule out for any monosomies and trisomies in their offspring.
Klinefelter syndrome (KS) is one of the common causes of human male infertility. This study detected four cases of KS in 6,198 couples and the rate is about one in 1,500(4/6,198) in the male. The patients with KS carry an additional X chromosome, which results in male hypogonadism, androgen deficiency and impaired spermatogenesis. Treatment consists of testosterone replacement therapy to correct the androgen deficiency and to provide patients with appropriate virilization. This therapy also has positive effects on mood and self-esteem and has been shown to protect against osteoporosis, although it will not reverse infertility8. Nowadays, however, patients with KS, including the non-mosaic type, should no longer be considered irrevocably infertile, because a biological paternity can be obtained by Testicular Sperm Extraction and Intra-Cytoplasmic sperm injection (TESE-ICSI). TESE will be followed by cryopreservation of extracted sperms before introducing androgen treatment in adolescent and will be used latter for ICSI when the KS patient would like to seek children9,10. But in some cases, chromosomal errors might be transmitted to the offspring of males with this syndrome. The genetic implications of the fertilisation procedures, including pre-transfer or prenatal genetic assessment, should be explained to patients and their spouse11.
In the current study, TS was detected in four cases, one of which is a isochromosome 46,X, i(Xq), with the rate of one in1500(4/6,198)in the female that is higher than one in 3000 to one in 2500 in live-born girls reported in the literature12. We only dealt with the cases of TS that remained unrecognized till the adulthood in this study, which make it not sure whether the incidence of TS in our studied region is really higher than previous reports. Although individuals with TS are infertile, there is increasing interest in fertility for women with TS by using assisted reproductive technologies. Heterologous fertility assistance using the donor oocytes is an established technique for TS. However, medical risks such as hypertensive disorders, fetal growth restriction, abortion, etc. during pregnancy are supposed to be highly increased. It is essential that further research should be performed to improve maternal and fetal outcomes for women with TS. Homologous fertility preservation has been performed in younger girls over 30 cases prior to ovarian atresia, but none in women with TS13.
Most XYY syndromes can have baby, but the same chromosome errors might occur in the offspring, which suggested that the prenatal diagnosis should be performed after pregnancy.
Reciprocal translocations, typically an exchange of two terminal segments from different chromosomes, will lead to recurrent miscarriages leading to bad obstetric history; for others, there may be a risk of offspring with mental and physical disability due to segregation of the translocation chromosomes at meiosis resulting in sperm or eggs with chromosome imbalance14,15.
Conventional karyotyping can be used for analyzing fetal chromosomes including distinguishing the balanced carriers or the fetus with imbalanced translocations through amniocentesis, chorion villus sampling (CVS) or periumbilical cord blood sampling (PUBS) after their natural pregnancy15. The advents of in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI) have enabled people to increase the pregnancy chance of the chromosome balanced translocations carriers. Preimplantation genetic diagnosis (PGD) has been very successful in assisting couples to achieve a viable unaffected pregnancy and has certainly reduced the time taken to achieve a pregnancy. PGD is used for reciprocal translocation carriers to minimize the risk of having an affected child or the distress of pregnancy termination and to reduce the risk of miscarriage due to abnormal segregation of the translocation16,17.
Robertsonian translocation is a special kind of balanced translocation, involving only the acrocentric chromosomes, specifically chromosomes 13, 14, 15, 21 and 22. They are formed when the long arms of two acrocentric chromosomes are translocated, ultimately forming a single chromosome. The clinical significance of the robertsonian translocation is the increased risk of infertility, spontaneous abortion and unbalanced chromosomal offspring18,19,20. In the current study, we found three cases of robertsonian translocation involving chromosome 21, accounting for 30% (3/10) of the sex chromosome disorders. The potential live-born unbalanced outcome of this robertsonian translocation is translocation trisomy 21, resulting in Down syndrome.
Reproductive risks of Robertsonian translocations are dependent on the chromosomes involved21,22. For couples with robertsonian translocations, the prenatal diagnosis should be suggested after their natural pregnancy to avoid the serious fetal malformation like trisomies. Like reciprocal translocation, robertsonian translocation couples need assisted conception for subfertility. Therefore, PGD should be performed after careful risk assessment and genetic counselling20,21.
The government policy that recommends and offers free pre-pregnancy cytogenetic diagnosis to all willing couples has enabled us to uncover diverse and rather frequent chromosomal abnormalities “hidden” in the couples planning for pregnancy. Obviously, this policy not only achieved a remarkable success but also raised many interesting questions: How many of these chromosomal syndromes would be probably detected by this way? How many people would benefit from the management after the sponsored cytogenetic analysis? How about the cost/benefit of this policy? We will attempt to address these questions in our future studies.
Methods
Study population
A retrospective study was conducted in the couples planning for pregnancy during the period of 1990 to 2010 in Zhenjiang City, eastern China. We carefully screened our study subjects, ensuring that the couples enlisted had no prior pregnancy and had no information or evidence whatsoever, based on medical examination or heath history, suggestive of fertility problems. A total of 6,198 couples, namely 12,396 individuals, were included. The average age of females is 23 ± 4 and the males is 26 ± 3; in our region, the average maternal age in last decade is about 26 ± 6, according to the government statistics calculating by Zhenjiang Family Planning Guidance institute. Informed consent was obtained from all subjects in the present study.
Chromosomal analysis
Karyotypes were generated from the peripheral blood lymphocyte cultures and the metaphase chromosome preparations were made according to standard cytogenetic protocols. Cytogenetic analysis was performed by G-banding and C-banding was also performed where necessary. Routine evaluation of each case involved 30 random metaphase spreads. Four metaphase spreads were photographed for karyotyping. When mosaicism was suspected, the analysis would be extended to 50 metaphase spreads. Karyotypes were described according to the International System for Human Cytogenetic Nomenclature (2005) (ISCN2005). Some cases would be recalled to re-examination if there were failure of cell cultures or poor quality karyotypes. The methods were carried out in accordance with the approved guidelines of the Association for Practical and Professional Ethics of Jiangsu University. All experiments in the present study were approved by the committee on Practical and Professional Ethics of Jiangsu University.
References
O'Flynn O'Brien, K. L., Varghese, A. C. & Agarwal, A. The genetic causes of male factor infertility: a review. Fertil. Steril. 93, 1–12 (2010).
Düzcan, F., Atmaca, M., Cetin, G. O. & Bagci, H. Cytogenetic studies in patients with reproductive failure. Acta Obstet. Gynecol. Scand. 82, 53–6 (2003).
Berger, R. et al. Cytogenetic studies on 519 consecutive de novo acute nonlymphocytic leukemias. Cancer Genet. Cytogenet. 29, 9–21 (1987).
Tunç, E., Demirhan, O., Demir, C. & Tastemir, D. Cytogenetic study of recurrent miscarriages and their parents. Genetika 43, 545–52 (2007).
Chang, E. M. et al. Preimplantation genetic diagnosis for couples with a Robertsonian translocation: practical information for genetic counseling. J. Assist. Reprod. Genet. 29, 67–75 (2012).
Dutta, U. R., Rajitha, P., Pidugu, V. K. & Dalal, A. B. Cytogenetic abnormalities in 1162 couples with recurrent miscarriages in southern region of India: report and review. J. Assist. Reprod. Genet. 28, 145–9 (2011).
Qin, J. et al. Analysis of the chromosomal abnormality in 5774 patients with clinical reproductive abnormality and 32 new karyotypes. Yi Chuan 31, 142–6 (2009).
Lanfranco, F., Kamischke, A., Zitzmann, M. & Nieschlag, E. Klinefelter's syndrome. Lancet 364, 273–83 (2004).
Sabbaghian, M., Modarresi, T., Hosseinifar, H., Hosseini, J. & Farrahi, F. Comparison of sperm retrieval and intracytoplasmic sperm injection outcome in patients with and without klinefelter syndrome. Urology 83, 107–10 (2014).
Oates Robert, D. Sperm retrieval in adolescents with Klinefelter syndrome. Fertil. Steril. 100, 943–4 (2013)
Smyth, C. M. & Bremner, W. J. Klinefelter syndrome. Arch. Intern. Med. 158, 1309–14 (1998).
Sybert, V. P. & McCauley, E. Turner's syndrome. N. Engl. J. Med. 351, 1227–38 (2004).
Hewitt, J. K., Jayasinghe, Y., Amor, D. J. & Gillam, L. H. Fertility in Turner syndrome. Clin. Endocrinol (Oxf) 79, 606–14 (2013).
Shah, K., Sivapalan, G., Gibbons, N., Tempest, H. & Griffin, D. K. The genetic basis of infertility. Reproduction 126, 13–25 (2003).
Gardner, R. J. M., Sutherland, G. R. & Shaffer, L. G. Chromosome Abnormalities and Genetic Counseling. [Gardner R. J. M., Sutherland G. R., & Shaffer L. G. (ed.)] [173–174] (Oxford, New York, 2012).
Paul, N. S. et al. Benefits and drawbacks of preimplantation genetic diagnosis (PGD) for reciprocal translocations: lessons from a prospective cohort study. Eur. J. Hum. Genet. 21, 1035–1041 (2013).
Ogilvie, C. M., Braude, P. R. & Scriven, P. N. Preimplantation genetic diagnosis-an overview. J. Histochem. Cytochem. 53, 255–260 (2005).
Ferfouri, F. et al. The chromosomal risk in sperm from heterozygous Robertsonian translocation carriers is related to the sperm count and the translication type. Fertil. Steril. 96, 1337–43 (2011).
Shamash, J. et al. Preimplantation genetic haplotyping a new application for diagnosis of translocation carrier's embryos-preliminary observations of two robertsonian translocation carrier families. J. Assist. Reprod. Genet. 28, 77–83 (2011).
Rius, M. et al. Detection of unbalanced chromosome segregations in preimplantation genetic diagnosis of translocations by short comparative genomic hybridization. Fertil. Steril. 96, 134–42 (2011).
Scriven, P. N., Flinter, F. A., Braude, F. R. & Ogilvie, C. M. Robertsonian translocations: reproductive risks and indications for preimplantation genetic diagnosis. Hum. Reprod. 16, 2267–73 (2001).
Kolgeci, S. et al. Reproductive risk of the silent carrier of Robertsonian translocation. Med. Arch. (Sarajevo, Bosnia Herzegovina) 67, 56–9 (2013).
Acknowledgements
The authors thank Zhenjiang Family Planning Guidance Institute and Jingkou District family planning guidance Station for the assistance with samples collecting. This work was supported by Jiangsu Research Project for the Key Talent of Maternal and Child Health under Grant No. FRC201214.
Author information
Authors and Affiliations
Contributions
Y.Y., H.W. and Y.T. designed, carried out the experiments, analyzed the data and prepared the draft of manuscript. M.G. and S.X. participated the experiments. X.X. and X.C. conceived the idea, supervised all research and revised the manuscript. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Yang, Y., Wang, H., Gao, M. et al. Pre-pregnancy cytogenetic analysis of general couples in eastern China. Sci Rep 4, 7224 (2014). https://doi.org/10.1038/srep07224
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep07224
This article is cited by
-
Cytogenetic analysis of 2959 couples with spontaneous abortion and detailed analysis of rare karyotypes
Journal of Genetics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.