Abstract
Prostate cancer (PCa) is the most common solid neoplasm diagnosed in developed countries. Nerve-sparing radical prostatectomy (NS-RP) has been widely accepted as the best choice treatment for localised PCa. However, erectile dysfunction (ED) and urinary incontinence are commonly observed after NS-RP. Using meta-analysis, we examined if phosphodiesterase type 5 inhibitors (PDE5-Is) could improve the symptoms of ED in patients undergoing NS-RP. This review contained seven randomised placebo-controlled trials with a total of 2,655 male patients. Patients in PDE5-Is group showed significant improvement in the International Index of Erectile Function-Erectile Function domain score (IIEF-EF), Global Assessment Questionnaire (GAQ), Sexual Encounter Profile question 2 (SEP-2) and SEP-3. Although the incidence of treatment-emergent adverse events (TEAEs) were high in both groups (56.44% vs. 40.63%), the safety profile were acceptable, with low incidence of discontinuation rate due to adverse events. Therefore, PDE5-Is are recommended for the treatment of post-NS-RP ED. Patients should be informed of possible adverse events.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most common solid neoplasm diagnosed in developed countries. In 2014, the epidemiological data from United States revealed a high incidence of PCa in men. PCa alone will account for approximately 27% (233,000) of the newly diagnosed cancers1. For patients with clinically localised PCa, radical prostatectomy (RP), particularly nerve-sparing radical prostatectomy (NS-RP), is the best choice treatment, with a life expectancy of ≥10 years2. However, despite the advancement in NS-RP, erectile dysfunction (ED) and urinary incontinence are still commonly encountered in these patients3.
Intracorporeal injections of alprostadil and vacuum pump therapy have been widely accepted by clinicians for treating post-NS-RP ED4,5. However, these therapies are ineffective and often present complications. Phosphodiesterase type 5 inhibitors (PDE5-Is) are the first line therapy for ED in general population6. Although less effective than in the general population, PDE5-Is appears to be effective in the patients with post-NS-RP ED7,8. Recently, several studies were conducted to identify whether PDE5-Is could be of benefit to patients suffering from post-NS-RP ED. In the present work, we performed a meta-analysis of the reported data from clinical trials to determine if post-NS-RP ED could be ameliorated with the help of PDE5-Is.
Results
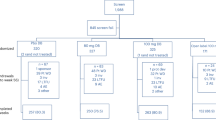
Initially, 67 articles were identified from the databases and 4 additional reports were collected manually. After the elimination of the duplicates, 57 records remained, of which 39 were excluded after reading the title and abstract and 10 were excluded after reading the full-text. Finally, data from the 7 RCTs9,10,11,12,13,14,15 were subjected to meta-analysis. Figure 1 shows the flow chart of the evidence acquisition. Overall, 2,655 male patients with a history of NS-RP were randomly selected to receive PDE5-Is (N = 1770) or placebo (N = 885). All patients underwent NS-RP for PCa before randomization and PDE5-Is were administered to those patients who developed ED after NS-RP. Among the seven RCTs, patients in three9,11,12 were treated with vardenafil and patients in two10,15 were randomly selected to receive tadalafil. Sildenafil and avanafil were used in Padma-Nathan's13 and Mulhall's study14, respectively. Table 1 shows the main characteristics of the studies. The Cochrane risk of bias tool was used to analyse all trials. Although ‘unclear risk of biases’ were allocated to the allocation concealment in all studies, ‘high risk of biases’ were allocated to the incomplete outcome data in two studies and the selective reporting was considered as ‘high risk of bias’ in two studies, the overall quality of the included studies were high. Figure 2 shows the authors' judgments on each of the risk of bias domain for each study.
Efficacy Assessments
IIEF
Nearly all of the studies reported IIEF-Erectile Function domain (IIEF-EF). However, only three studies9,10,15 reported data in mean ± SD and data from these three trials were extracted for meta-analysis. Of these three trials, one9 used vardenafil and the remaining two studies10,15 administered tadalafil. Our pooled analysis of IIEF-EF showed that erectile function of patients in PDE5-Is group improved significantly when compared with that of the patients in the placebo group (Figure 3: MD = 4.35; 95% CI, 3.42–5.29; P < 0.00001).
GAQ
Data corresponding to the responses to the Global Assessment Question in three studies9,10,14, which enrolled a total 1041 patients, was extracted. Vardenafil, tadalafil and avanafil were used in Brock's9, Montorsi's10 and Mulhall's study14, respectively. Pooled analysis revealed that when compared to the placebo group, significantly higher proportion of patients in PDE5-Is group responded positively to the treatment. The overall RR was 3.50 (95% CI, 2.31–5.31; P < 0.00001, Figure 4).
SEP2 and SEP3
Data from two9,10 and three studies9,10,15 reported in mean ± SD could be extracted to perform a forest plot for SEP2 and SEP3, respectively. Two classes of PDE5-Is (vardenafil and tadalafil) were included in these trials. Forest plot shown in Figure 5 indicated that the use of PDE5-Is was associated with a significantly greater change in SEP2 than when placebo was used. The overall MD was 21.49 (95% CI, 16.36–26.63; P < 0.00001, Figure 5). Similarly, forest plot in Figure 6 also revealed a significant greater change in SEP3 in the PDE5-Is group than in the placebo group. The overall MD for SEP3 was 17.01 (95% CI, 8.46–25.56; P < 0.0001, Figure 6).
Safety Assessments
TEAEs and Discontinuation rate
Overall, the incidence of TEAEs in PDE5-Is and placebo groups were 56.44% and 40.63%, respectively. The most frequently reported adverse events were headache, flushing, dyspepsia and rhinitis, all of which were mild. The Forest plot showed that TEAEs in PDE5-Is group were significantly more than that in the placebo group. As shown in Figure 7, the overall RR was 1.42 (95% CI, 1.21–1.65; P < 0.0001). Discontinuation rate was reported in nearly all included studies. The overall discontinuation date in PDE5-Is and placebo groups were 5.29% and 2.84%, respectively. Although both groups had a low discontinuation rate related to adverse events, the pooled analysis showed that the reported discontinuation was significantly more in PDE5-Is group than in the placebo group. The overall RR for discontinuation rate was 1.87 (95% CI, 1.16–2.99; P = 0.01, Figure 8).
Discussion
Radical prostatectomy is commonly used to treat localised PCa. The incidence of ED and urinary incontinence in patients undergoing NS-RP is high. Intracorporeal alprostadil injections and vacuum-pump therapy have been suggested for the rehabilitation of patients with post-RP ED. However, these therapies are of poor efficacy and present complications.
In mammals, more than 10 phosphodiesterase (PDE) families have been identified. PDE5, which limits the action of nitric oxide-cyclic guanosine monophosphate (cGMP) pathway by degrading cGMP, is the predominant phosphodiesterase expressed in male corpus cavernosum16. PDE5-Is enhances erectile function by preventing the degradation of cGMP17. Accordingly, PDE5-Is such as tadalafil, sildenafil, vardenafil, have been successfully used to treat male ED. To date, a large number of studies have been conducted to assess the efficacy and safety of using PDE5-Is to treat ED in general populations. A meta-analysis by Yuan18 showed that PDE5-Is are well tolerated and are more effective than placebo for treating ED in general populations. However, the effectiveness and safety of using PDE5-Is in PCa patients after NS-RP remain unclear.
In this meta-analysis, we evaluated the erectile function by assessing the IIEF-EF domain, GAQ, SEP2 and SEP3. Our systematic review of the published data from seven RCTs indicated that compared with placebo, the use of PDE5-Is yielded better results for all of the indicators examined. To assess the safety of using PDE5-Is, we evaluated both the TEAEs and the discontinuation rate. Although the incidences of TEAEs in both groups were high (56.44% vs. 40.63%), the main adverse events were mild in nature. The high incidence in both groups might be explained by the subjective symptoms or the sequela by surgery itself. Despite the high incidence of TEAEs, the discontinuation rate due to AEs was low (5.29% vs. 2.84%). Overall, the safety of using PDE5-Is for ED following NS-RP was acceptable and the treatment was considered well tolerated.
All trials included in this meta-analysis were described as double-blind, randomised controlled trials. We defined the intervention as PDE5-Is alone vs. placebo for clearly describing the efficacy and safety parameters. Thus, the study conducted by Pavlovich19 was excluded since a placebo group could not be found. The quality of the trials was assessed using the ‘Jadad score’ system and the Cochrane risk bias tool. Although nearly all trials included in this meta-analysis lacked a clear description of the allocation concealment, the methods were designed well and could be considered as of high quality. Thus, the data from the trials included in our analysis were reliable.
In this meta-analysis, we excluded one trial20 because it doesn't meet the inclusion criteria ‘reported least one of the following outcome measures: IIEF-EF, GAQ, SEP-2, SEP-3, TEAEs and discontinuation rate’. Although the patients in five studies10,11,12,13,15 had no history of ED, the preoperative erectile function of patients in other9,14 studies were unclear. Therefore, the efficacy of PDE5-Is for the treatment of ED associated with NS-RP appeared to be speculative. This might influence the results of a study investigating the effectiveness of using PDE5-Is to treat ED in patients undergoing NS-RP as well as in general populations (a history of ED before NS-RP). All PCa patients underwent NSRP before randomization. Patients in five studies10,12,13,14,15 underwent a bilateral NS-RP and patients in two other studies9,11 underwent unilateral or bilateral NS-RP. However, whether or not the efficacy and safety of using PDE5-Is to treat ED reported following unilateral and bilateral NS-RPs are similar is not clear.
Four different PDE5-Is, vardenafil, tadalafil, avanafil and sildenafil, were used in the trials. However, due to the lack of sufficient data, the relative efficacies of these drugs could not be assessed. The treatment strategy in four9,10,11,14 of the included trials was ‘on-demand’ (taking medication before sexual intercourse), two12,15 used both ‘on-demand’ and ‘once daily’ strategies, whereas the strategy in one trial was ‘once daily’. Whether these strategies influenced the safety and efficacy is not known. The treatment period in the trials included in this analysis varied from 12 weeks to 9 months. However, an effective treatment period could not be assessed. It is likely that the 12-week treatment is too short to achieve optimal results.
In summary, our results showed that PDE5-Is significantly improved the erectile function in patients with post-NS-RP ED. Although adverse events commonly occurred in patients, the low discontinuation rate revealed that the safety profile was acceptable. Therefore, PDE5-Is are recommended for the treatment of post-NS-RP ED. Patients should be informed of the possible adverse events.
Methods
Design and search strategy
All randomised controlled trials (RCTs) related to the use of PDE5-Is to treat post-NS-RP ED were identified for this meta-analysis. Literature search was performed in March 2014 and no language and geographic region restriction were applied. The PubMed, EMBASE and Cochrane Central Register of Controlled trials databases were searched. Additional articles and abstracts were manually retrieved after scrutinizing the reference list. The search terms included ‘Phosphodiesterase type 5 inhibitors/PDE5-Is’, ‘erectile dysfunction/ED’ and ‘nerve-sparing radical prostatectomy/NS-RP’. The literature search was performed by Li J and Shi Q.
Study selection and data extraction
All studies were independently evaluated by two reviewers (Li J and Shi Q). The inclusion criteria were, (1) all male patients had undergone an NS-RP for PCa, (2) the patients had ED after NS-RP, (3) the patients were treated with PDE5-Is without any other medication, (4) the treatment intervention was PDE5-Is alone versus placebo and (5) the trials reported least one of the following outcome measures: IIEF-EF, Global Assessment Questionnaire (GAQ), Sexual Encounter Profile question 2 (SEP-2), SEP-3, treatment-emergent adverse events (TEAEs) and discontinuation rate. Animal experiments, quasi-RCTs and Non-RCTs were excluded. Patients diagnosed with co-morbidities, particularly diabetes were also excluded.
Data from the included studies were extracted by two reviewers and cross-checked. Any disagreements were reconciled by discussion or by a third person. The following information was collected from the reports of original trials: first author, study design, number of participants, treatment strategy and duration, surgery mode and outcome measures. The primary outcomes were IIEF-EF and GAQ and the secondary outcomes included SEP-2, SEP-3, TEAEs and discontinuation rate.
Quality assessment and statistical analysis
As described previously21,22, both the Jadad scoring system and the Cochrane risk bias tool were used to assess the quality of all included trials. Briefly, Jadad scores of 0–5 points were allocated to each trial and seven different quality parameters were used to assess each bias. Trial with a score of 3 points or more in Jadad scoring system was considered as a high-quality trial. For Cochrane risk bias tool, low, unclear, or high risk of bias for each item was used to describe the bias. All included trials were assessed independently by two reviewers (Li J and Shi Q).
Statistical analysis was performed using the Review Manager, version 5.1.0 (Cochrane Collaboration, Oxford, UK). The statistical heterogeneity between studies was assessed using the Mantel–Haenszel chi-square test and the I2 statistic. Heterogeneity was acceptable if the I2 value was less than 50% and the P value was more than 0.10. In the absence of an evidence for heterogeneity, a fixed-effect model was applied for calculations. Otherwise, a random-effect model was used. The Risk Ratio (RR) and the Mean Difference (MD) were used to evaluate the dichotomous data and continuous data, respectively. All results were reported with 95% confidence intervals (CIs) and a P value less than 0.05 was considered statistically significant. For reporting the standard error of the mean (SEM), we calculated the standard deviation (SD) by multiplying SEM by the square root of N (N is the number of subjects).
References
Siegel, R., Ma, J., Zou, Z. & Jemal, A. Cancer Statistics, 2014. CA Cancer J Clin 64, 9–29 (2014).
Briganti, A. et al. Management of erectile dysfunction after radical prostatectomy in 2007. World J Urol 25, 143–148 (2007).
Penson, D. F. et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the Prostate Cancer Outcomes Study. J Urol 179, S40–44 (2008).
Montorsi, F. et al. Recovery of spontaneous erectile function after nerve-sparing radical retropubic prostatectomy with and without early intracavernous injection of alprostadil: results of a prospective, randomized trial. J Urol 158, 1408–1410 (1997).
Raina, R. et al. Early use of vacuum constriction device following radical prostatectomy facilitates early sexual activity and potentially earlier return of erectile function. Int J Impot Res 18, 77–81 (2006).
Wespes, E. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. (2013) Available at: http://www.uroweb.org/gls/pdf/14_Male%20Sexual%20Dysfunction_LR.pdf (Date of access: 01/02/2014).
Salonia, A. et al. Prevention and management of postprostatectomy sexual dysfunctions. Part1: choosing the right patient at the right time for the right surgery. Eur Urol 62, 261–272 (2012).
Salonia, A. et al. Prevention and management of postprostatectomy sexual dysfunctions. Part2: recovery and preservation of erectile function, sexual desire and orgasmic function. Eur Urol 62, 273–286 (2012).
Brock, G. et al. Safety and efficacy of vardenafil for the treatment of men with erectile dysfunction after radical retropubic prostatectomy. J Urol 170, 1278–1283 (2003).
Montorsi, F. et al. Tadalafil in the treatment of erectile dysfunction following bilateral nerve sparing radical retropubic prostatectomy: a randomized, double-blind, placebo controlled trial. J Urol 172, 1036–1041 (2004).
Nehra, A., Grantmyre, J., Nadel, A., Thibonnier, M. & Brock, G. Vardenafil improved patient satisfaction with erectile hardness, orgasmic function and sexual experience in men with erectile dysfunction following nerve sparing radical prostatectomy. J Urol 173, 2067–2071 (2005).
Montorsi, F. et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol 54, 923–931 (2008).
Padma-Nathan, H. et al. Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res 20, 479–486 (2008).
Mulhall, J. P. et al. A phase 3, placebo controlled study of the safety and efficacy for the treatment of erectile dysfunction after nerve sparing radical prostatectomy. J Urol 189, 2229–2236 (2013).
Montorsi, F. et al. Effects of tadalafil treatment on erectile function recovery following bilateral nerve-sparing radical prostatectomy: a randomised placebo-controlled study (REACTT). Eur Urol 65, 587–596 (2014).
Corbin, J. D. Mechanisms of action of PDE5 inhibition in erectile dysfunction. Int J Impot Res 16 Suppl 1S4–7 (2004).
Rosen, R. C. & Kostis, J. B. Overview of phosphodiesterase 5 inhibition in erectile dysfunction. Am J Cardiol 92, 9M–18M (2003).
Yuan, J. et al. Comparative effectiveness and safety of oral phosphodiesterase type 5 inhibitors for erectile dysfunction: a systematic review and network meta-analysis. Eur Urol 63, 902–912 (2013).
Pavlovich, C. P. et al. Nightly vs on-demand sildenafil for penile rehabilitation after minimally invasive nerve-sparing radical prostatectomy: results of a randomized double-blind trial with placebo. BJU Int 112, 844–851 (2013).
McMullough, A. R. Levine, L. A. & Padma-Nathan, H. Return of nocturnal erections and erectile function after bilateral nerve-sparing radical prostatectomy in men treated nightly with sildenafil citrate: subanalysis of a longitudinal randomized double-blind placebo-controlled trial. J Sex Med 5, 476–484 (2008).
Li, J. et al. Efficacy and safety of muscarinic antagonists as add-on therapy for male lower urinary tract symptoms. Sci Rep 4, 3948 (2014).
Higgins, J. & Green, S. Cochrane Handbook For Systematic Review Of Intervention 5.1.0 (The Nordic Cochrane Centre, Copenhagen, 2011).
Acknowledgements
This work was collectively supported by grant (National Natural Science Foundation of China (No.30901484 and No.81270841)). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
H.P., W.Q., D.Q., Y.J. and L.X. contributed to the conception and design of the study and the critical revision of the article. L.J. and S.Q. searched and selected the studies, analyzed the data, prepared figures 1–8 and drafted the article. P.C. and B.Y. participated in the acquisition of data and statistical analysis. T.Y. and Y.H. participated in the interpretation of data. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Li, J., Shi, Q., Pu, C. et al. Phosphodiesterase type 5 inhibitors for the treatment of post-nerve sparing radical prostatectomy erectile dysfunction in men. Sci Rep 4, 5801 (2014). https://doi.org/10.1038/srep05801
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05801
This article is cited by
-
Is there a relationship between phosphodiesterase type 5 inhibitors and biochemical recurrence after radical prostatectomy: a systematic review and meta-analysis
International Urology and Nephrology (2018)
-
Comparisons of regular and on-demand regimen of PED5-Is in the treatment of ED after nerve-sparing radical prostatectomy for Prostate Cancer
Scientific Reports (2016)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.