Abstract
Tissue scaffolds provide a framework for living tissue regeneration. However, traditional tissue scaffolds are exogenous, composed of metals, ceramics, polymers and animal tissues and have a defined biocompatibility and application. This study presents a new method for obtaining a tissue scaffold from blood albumin, the major protein in mammalian blood. Human, bovine and porcine albumin was polymerised into albumin polymers by microbial transglutaminase and was then cast by freeze-drying-based moulding to form albumin tissue scaffolds. Scanning electron microscopy and material testing analyses revealed that the albumin tissue scaffold possesses an extremely porous structure, moderate mechanical strength and resilience. Using a culture of human mesenchymal stem cells (MSCs) as a model, we showed that MSCs can be seeded and grown in the albumin tissue scaffold. Furthermore, the albumin tissue scaffold can support the long-term osteogenic differentiation of MSCs. These results show that the albumin tissue scaffold exhibits favourable material properties and good compatibility with cells. We propose that this novel tissue scaffold can satisfy essential needs in tissue engineering as a general-purpose substrate. The use of this scaffold could lead to the development of new methods of artificial fabrication of autogenic tissue substitutes.
Similar content being viewed by others
Introduction
New translational research in tissue engineering has irreversibly and permanently reshaped the landscape of modern medicine. Researchers have developed novel artificial tissues and have used them to replace human tissues, including skin, blood vessels, bone, cartilage, urethras and the trachea1,2. Research has also focused on translating technologies into tissue engineering applications, such as electrospinning, self-assembling peptides, optical trapping and bioprinting. These technologies can manipulate polymers, peptides, cells and even individual molecules into ordered macroscopic objects for artificial tissue fabrication3,4,5,6,7,8. The cellularisation of decellularised animal organs, such as the heart, lung, liver, kidney and pancreas, represents another method of fabricating wholly transplantable organs9,10,11,12. The synergy of these powerful methods will enable the production of complex artificial grafts. The ultimate goal of tissue engineering is to creating normal tissue-like grafts. Advanced artificial grafts are designed to be functionally similar to and structurally indistinguishable from normal tissue. By fostering safety, biocompatibility and functionality, innovations in cell and tissue engineering can address the increasing demand for tissue replacement. Thus, this topic is very closely associated with the future health, wellbeing and quality of life of all humans.
The raw materials used in tissue engineering cover a broad range of natural and synthetic sources, including metals, ceramics, synthetic polymers and natural polymers. Each material has its own unique merits and promising applications in translational medicine. Although there are many new artificial materials that have been proposed for many potential medical applications, autologous tissues and autogenic materials are still the sources of choice in current medical practices because autologous materials are free of biocompatibility and immunocompatibility concerns. Autologous transplantations have been widely used in clinical applications, particularly for bone-, cartilage-, cosmetic surgery- and reconstruction-related uses. In addition, autologous tissues may be harvested and frozen and they are compatible with long-term storage. For example, the autologous transplantation of frozen ovarian tissue has recently been applied to preserve the reproductive ability of female cancer patients13. However, the difficulties of donor-site availability and donor-site morbidity often limit the general use of autografts. Allografts from a human tissue bank offer an alternative source when autografts or isografts are not available to patients. However, allografts harvested from cadavers are erratic in function, raising concerns regarding their common use.
Porous tissue scaffolds consist of many pores that are capable of supporting cell attachment, growth and differentiation. Tissue scaffolds are conducive to ongoing cellular activities that generate three-dimensional (3D) artificial tissue. An anatomically correct tissue scaffold fabricated for a patient may be used as a tissue substitute for damaged tissue replacement and new tissue regeneration. The implanted tissue scaffold should undergo tissue remodelling. The term “biologic scaffold construct” refers to a tissue scaffold with or without the incorporation of a cell homing factor, a tissue morphogenesis factor, or other tissue-forming factors, creating a robust implant. This type of composite is capable of direct, specific tissue formation in vivo. For example, an absorbable collagen sponge (ACS) infused with recombinant human bone morphogenetic protein-2 (rhBMP-2) is a potent construct that induces ectopic bone formation in living animals. This construct has been clinically used as a bone substitute in orthopaedic applications. Another construct, consisting of poly-ε-caprolactone and hydroxyapatite (PCL-HA) infused with transforming growth factor β-3 (TGFβ-3) and collagen type I, has been shown to fully regenerate the cartilage of rabbit humeral joints14. These proof-of-concept results demonstrate that the biologic scaffold construct is a powerful approach for directing new tissue formation, establishing its role in current tissue engineering research15,16.
Researchers have widely acknowledged the applications of tissue-derived autogenic cells from adults, including induced pluripotent stem (iPS) cells, hematopoietic stem cells (HSCs) and mesenchymal stem cells (MSCs). However, consensus on how to generate and use self-derived biomaterials from adults is lacking. The potential of albumin in tissue engineering and regenerative medicine remains to be explored17,18,19. The human body rapidly replenishes plasma proteins and tens of litres of adult plasma can be harvested from one person per year through routine plasmapheresis. Normal diet and exercise, with careful monitoring of haemoglobin, immunoglobulin and total serum protein levels and erythrocyte volume, are required20. In addition, the human serum albumin can be polymerised by cross-linkage. The polymerised human has been known to bind both hepatocyte and hepatitis B virus and may play a role in the pathology of hepatitis21,22. Albumin accounts for half of the total protein in the plasma and has a concentration of approximately 3%. Albumin can also be easily isolated from plasma by precipitation with a high purity, yield and homogeneity23. Because albumin appears to be an attractive source of autogenic biomaterials for autologous tissue engineering, this study investigated the processing method needed to convert albumin into an available biomaterial and also tested the cell compatibility of this new biomaterial.
Results
The cross-linking of individual albumins into polymeric albumins is required to generate a solid object. We used an enzyme-based method to polymerise albumin, which is based on the enzymatic activity of a microbial transglutaminase (EC 2.3.2.13; Streptomyces mobaraensis). This enzyme effectively catalyses new covalent bond formation between peptide residues, extensively bridging the side chains of glutamines and lysines. This enzymatic polymerisation was conducted in an aqueous solution buffered at a mild pH (8.0) in the presence of a reducing agent. As shown in Figure 1, bovine serum albumin was polymerised into albumin polymers when more than 200 μg/ml microbial transglutaminase was added to the reaction. As a result, the albumin polymers could not be resolved by SDS polyacrylamide gel electrophoresis (SDS-PAGE) and accumulated at the top of the gel after protein electrophoresis (see the arrow in Figure 1). The protein structure of mammalian serum albumin is highly conserved. Therefore, human and porcine serum albumins were polymerised by microbial transglutaminase during the same reaction. Albumin solutions were solidified after polymerisation and a urea-containing buffer was applied to isolate the albumin polymers from the reaction.
Transglutaminase-cross-linked peptides and the polymerisation of bovine serum albumin.
Various amounts of microbial transglutaminase were mixed with bovine serum albumin. The reactions were conducted at 37°C. After 1 h of incubation, samples were collected, treated with reducing sample buffer (including 0.1 M DTT as a reducing agent) and analysed using SDS-PAGE. The concentration of bovine serum albumin was 5% in all reactions and the final concentrations of microbial transglutaminase were 0, 25, 50, 100, 200, 300, 400 and 500 μg/ml (lanes 1 to 8, respectively). Lane M: molecular weight standards. The arrow on the left of the figure indicates the band corresponding to the albumin polymer.
Albumin polymers may serve as the starting material for preparing albumin-based biomaterials, such as albumin membranes, sheets, rods and hydrogels and in this study, the albumin polymer was formed into a tissue scaffold by freeze-drying-based moulding. Albumin polymer at a 2% concentration was freeze-dried and subsequently treated with formaldehyde vapour. The formaldehyde treatment introduced covalent bond bridges within the polymer, thus permanently fixing its shape and size. The photographs in Figure 2A and Supplementary Figure S1 show the appearance of the prepared albumin tissue scaffolds derived from human, bovine and porcine serum albumins. The scanning electron microscopy (SEM) and Cryo-SEM images in Figure 2B, 2C and 2D show the structural features of a bovine albumin tissue scaffold. The porous structures had circular and elliptical geometries, with diameters of approximately 10 to 200 μm. Their pore sizes were generally much larger than animal cells, which typically have diameters of approximately 10 to 50 μm. The pore geometries were evenly distributed throughout the entire scaffold, as the transverse section showed that the inside of the scaffold had the same pore geometries as the surface. A 10-μm section stained with eosin Y was used to measure the pore diameter, resulting in an average value of 89 ± 35 μm (Figure 3 and Supplementary Table 1).
Appearance and SEM images of the prepared albumin tissue scaffolds.
(A) The photographs show the tissue scaffolds generated from bovine serum albumin. Cylindrical tissue scaffolds, with a 0.1-ml volume, were prepared using a 96-well tissue culture plate as the casting mould. A rectangular tissue scaffold of 3.5 ml in volume was prepared using an 8-well tissue culture multidish as the casting mould. Representative SEM images of the surface (B) and inside (C) of a bovine albumin tissue scaffold. Both the surface and the inside images were acquired from the same sample. (D) Representative Cryo-SEM images of the inside of a bovine albumin tissue scaffold.
Pore diameter measurements of the albumin tissue scaffold.
A bovine albumin tissue scaffold was embedded in glycol methacrylate resin, followed by sectioning into 10-μm sections. After staining with eosin Y, a sample image was acquired by fluorescence microscopy (A). Distribution of the observed pore diameters (B).
The albumin tissue scaffolds had a sponge-like appearance. A dry albumin tissue scaffold can absorb a substantial amount of water. The water binding of the bovine albumin tissue scaffold was determined to be 43.4 ± 1.5, which is the ratio of the wet weight to the dry weight. Therefore, water accounted for approximately 97% of the weight of the wet albumin tissue scaffold. The wet albumin tissue scaffold exhibited resilience. As shown in Figure 4A, cyclic compression testing demonstrated the complete recovery of the bovine albumin tissue scaffold from a compressive strain of 0.8. The results revealed full elastic hysteresis loops for the wet materials in these compression cycles. The water absorbed by the albumin tissue scaffolds could be removed by mechanical force. For example, pressure could be applied with the fingertips to achieve a semi-dry status, but immersing the scaffold in water completely restored its original shape and size. In contrast, a dried albumin tissue scaffold is brittle and lacks resilience. A tensile test indicated that this material presents moderate toughness. The ultimate tensile strength, failure strain and linear modulus of the bovine albumin tissue scaffold were determined to be 20.7 ± 5.9, 0.21 ± 0.05 and 102 ± 26 kPa, respectively (Figure 4B and Supplementary Figure S2). These physical and mechanical results are similar to those of a collagen-based tissue scaffold24,25. In general, we found that the appearance, water binding, resilience and mechanical strength of the albumin-based tissue scaffolds were very similar to those of collagen-based tissue scaffolds.
Cyclic compression testing and tensile strength of the albumin tissue scaffold.
(A) A cylinder-shaped bovine albumin tissue scaffold (0.3-ml volume) was cast using a 96-well plate as the mould. A cyclic compression test was performed in a water tank under ambient conditions (25°C). The rates of compression and decompression were both 20 mm/min. (B) dog bone-shaped bovine albumin tissue scaffold (1-ml volume) was cast using a plexiglass mould. Tensile testing was performed at ambient temperature (25°C) under wet conditions. The rate of tensile strain was 25 mm/min.
MSCs from adults are self-derived agents that have the potential to be used in clinics to treat various human diseases. The results of recent clinical trials have demonstrated that the systemic injection of autologous MSCs is a safe treatment, thus supporting the further development of related clinical therapies26,27. In the present study, we seeded and cultured human MSCs to test the cell compatibility of the albumin tissue scaffold (see Supplementary Figure S3 for an immunocytochemical staining). Figure 5 shows that human MSCs were viable in the albumin tissue scaffold and that cell activity was substantially increased after 3 days. We further explored the ability of the albumin tissue scaffold to support the long-term culture and differentiation of human MSCs. After seeding the cells, the cultures were maintained in osteogenic induction medium to induce osteogenic differentiation of the MSCs28. As shown in Figure 6, the activity of ALP, which is a specific early marker of osteogenic differentiation, was increased 3- to 9-fold from 3 to 9 days post-induction. In contrast, ALP activity in non-induced cultures did not increase significantly. As shown in Figure 7A, the calcium content in the cultures accumulated proportionally to the period of in vitro culturing after 14 or 28 days. Little or no calcium accumulation was found in the non-induced cultures. Dye staining of the cell-scaffold construct clearly showed the extensive deposition of calcium phosphate throughout the entire scaffold (Figure 7B and 7C). These results demonstrate that the albumin tissue scaffold can support human cell attachment, growth and differentiation.
Culture and growth of human MSCs in the albumin tissue scaffold.
An bovine albumin tissue scaffold with a volume of 0.1 ml was seeded with 1 × 105 human MSCs. The cultures were maintained in 1 ml of culture medium in a 5-ml tissue culture tube for 1, 2 and 3 days. Cell viability was determined using a fluorescent dye (PrestoBlue, Invitrogen). *P < 0.05 compared with the value on day 0.
Upregulation of the ALP activity of human MSCs in the albumin tissue scaffold.
A bovine albumin tissue scaffold with a volume of 0.1 ml was seeded with 1 × 105 human MSCs. The cultures were maintained in 1 ml of basal or induction medium in a 5-ml tissue culture tube for 0, 3, 6, 9, 12 and 15 days. ALP activity and DNA content were measured. *P < 0.05 compared with the corresponding non-induced value.
Accumulation of calcium phosphate deposits from human MSCs in the albumin tissue scaffold.
An albumin tissue scaffold with a volume of 0.1 ml was seeded with 1 × 105 human MSCs. The cultures were maintained in 1 ml of basal (−) or induction (+) medium in a 5-ml tissue culture tube for 0, 14 and 28 days. Samples were fixed in acetone and for calcium quantification and DNA content measurements (A). Samples also were fixed in paraformaldehyde and stained with alizarin red S dye (B and C). Photography of the surface of the stained osteogenic constructs (B). Photography of the inside of the stained osteogenic constructs (C). *P < 0.05 compared with the value on day 0.
Discussion
This study presents a completely new processing method in which liquid albumin solution is first converted into an albumin polymer and is then converted into a solid-state tissue scaffold by freeze-drying-based moulding. The yield of the present method was approximately 75% with respect to volume. Thus, for a single 500-ml tube of human blood, the overall yield for a human albumin tissue scaffold would be approximately 105 ml. The availability of this material is adequate for many tissue engineering applications. The presented preliminary evaluations of the biocompatibility and differentiation of this novel biomaterial strongly support the albumin tissue scaffold as a useful substrate. Albumin is routinely used as an additive in tissue culture medium, but few, if any, specific cell responses are associated with this protein. In addition, albumin is the major protein in animal blood. Plasma albumin binds fatty acids, steroids, nutrients and metabolites in the circulation and distributes these small molecules throughout the body. Plasma albumin also plays a role in maintaining the pH, osmotic stress and reducing power of mammalian blood29,30. These biochemical and physiological characteristics indicate that albumin is a relatively inactive substance. Therefore, we hypothesised that an albumin-based tissue scaffold would be a useful substrate because it can play a structural-support role in cell and tissue engineering. Importantly, this unique characteristic of albumin can dramatically reduce the complexity of developing cell-scaffold-based medical products by avoiding complicated cell-scaffold interactions. The data reported based on the present assessments and previous research support this proposal, indicating that albumin is a suitable proteinous starting material for tissue engineering applications.
Assays for physical and mechanical properties have revealed that as prepared, albumin tissue scaffolds yield results very similar to those of collagen-based tissue scaffolds. Both albumin tissue scaffolds and collagen tissue scaffolds have excellent resilience and an extremely high water-binding capacity (>1:40). Both materials exhibit similar tensile strengths and extremely high porosities (>97%). Because they are peptide-based biomaterials, albumin and collagen tissue scaffolds have good cell-binding characteristics, supporting cell growth. Collagen tissue scaffolds, which are also known as collagen sponges, have been extensively investigated in this regard. However, the common problem associated with collagen-based matrices is their rapid degradation, as collagen is decomposed and dissolved by cell activity, causing an unstable architecture during the in vitro tissue culture process. As a result, collagen-based 3D matrices are not commonly used in long-term cell culture maintenance and differentiation, such as the 4- to 5-week time period required for the osteogenic differentiation of MSCs31. In the current study, we found that even after 28 days of MSC culture, the appearance of the albumin tissue scaffold had not changed in dimension or shape. This observation may suggest that the albumin tissue scaffold is difficult to degrade by MSCs in vitro. The degradation of cross-linked albumins may be very different from other biopolymer based materials like collagen and fibrin. Collagen is degraded by collagenase, fibrin is degraded by plasmin, but specific protease that responsible for degradation of serum albumin or polymerized albumin is lacking. Further investigating the degradation properties involved can help clarify this.
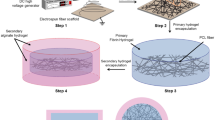
The possibility of a prepared autogenic biomaterial has created certain opportunities in tissue engineering (Figure 8). A plain albumin tissue scaffold may be prepared from any individual and developed as a new type of tissue filler. This scaffold can be used alone for implantation. Alternatively, a scaffold infused with potent tissue-regenerative factors, such as rhBMP-2, may be used to direct new tissue formation in vivo. It may also be possible to generate a tissue substitute in a living bioreactor using a suitable biologic-scaffold construct32. Finally, the combination of an albumin tissue scaffold and stem cells, such as MSCs, as illustrated by this study, can form a living cell-scaffold construct. Such a construct can be used for cell transplantation or culture and can also order the seeded cells into differentiated functional effector cells. The last approach can theoretically create many artificial tissues in a test tube. By unleashing the power of the plasticity of human stem cells, different autogenic tissue substitutes can be artificially constructed on the platform provided by the albumin tissue scaffold. The advantages of the human autogenic construct can address practical difficulties regarding autograft availability and morbidity. Hopefully, these novel autogenic tissues and grafts created in the laboratory can mitigate the increased demand for human tissues. It is also hoped that this new biomaterial will present particular advantages in the future of medicine.
Potential application of the albumin tissue scaffold in tissue engineering.
There are three possible methods of preparing artificial tissue substitutes. Blood and tissue are first harvested from an individual (for example, an adult, as depicted here), followed by developing an albumin tissue scaffold and seeding it with stem cells in the laboratory. An albumin tissue scaffold may be used alone, as a plain construct (method 1, red colour), or it may be combined with potent biologics to form a composite biologic-scaffold construct (method 2, green colour). Autogenic cells or stem cells can also be seeded in an autogenic albumin tissue scaffold to form a living cell-scaffold construct and artificial tissue (method 3, blue colour).
In the present study, we reported a method for synthesising an albumin-based tissue scaffold and characterised its cell compatibility. The 3D porous tissue scaffold can be prepared from human, bovine and porcine albumin using transglutaminase cross-links and freeze-drying-based moulding processes. The prepared albumin tissue scaffold has a sponge-like appearance and properties. The scaffold binds a large amount of water, possesses resilience under wet conditions and has moderate mechanical strength. Surface electron microscopy analysis revealed a large pore size that can accommodate many living cells inside. We propose that the albumin tissue scaffold could be a good substrate for tissue culture and tissue engineering that can support human MSC attachment, growth and differentiation. Importantly, the scaffold is an autogenic biomaterial that is available in plentiful quantities. Biofabrication from a combination of autogenic cells and autogenic biomaterials is a promising approach that may facilitate medical innovations.
Methods
Preparation of the albumin tissue scaffold
Albumin solutions at 10% w/v were prepared from the lyophilised powders of human, bovine and porcine albumin (≥98%, suitable for cell culture) by dissolving the powders in a buffer of 50 mM bicine, pH 8.3 and 125 mM NaCl. Microbial transglutaminase (specific activity of 20 U/mg) at a concentration of 1 mg/ml was prepared in a buffer of 20 mM 2-(N-morpholino)ethanesulfonic acid (MES), pH 6.2. A 2 M stock solution of dithiothreitol (DTT) was prepared in water. Equal volumes of 10% albumin solution and 1 mg/ml microbial transglutaminase were combined and DTT was added to a final concentration of 12.5 mM in the reaction. After incubation of the reaction at 37°C for 16 h, four volumes of washing buffer (6 M urea and 0.1 M sodium acetate, pH 5.0) were added and the content was homogenised by a motor-driven tissue grinder. The homogenate was centrifuged at 2330 × g for 5 min to recover the albumin polymers. The homogenisation step was repeated twice. The albumin polymers were washed with 0.1% lactic acid 3 times, transferred to a casting mould, frozen at −80°C for 1 h and transferred to a freeze dryer for 24 h. The dried materials were treated with formaldehyde vapour in a sealed container for 2 h. The prepared albumin tissue scaffolds were then stored in a dry box.
Physical and mechanical characterisations
The albumin tissue scaffold was coated with gold by an SPI Module Sputter Coater (SPI Supplies, PA, USA), mounted on a specimen stub and imaged using a JSM-5610LV scanning electron microscope (JEOL, Tokyo, Japan). After acquiring surface images, the scaffold was cut in half to examine the inner structure. For cryo-SEM, the tissue scaffold was rinsed in pure water. Hydrated sample was loaded on stub, frozen by liquid nitrogen, transferred to a sample preparation chamber and then sublimed at −80°C for 30 min (PP2000TR Cryo-preparation System; Quorum Technologies, East Sussex, UK). After coating with platium, the sample was imaged at −160°C using a cryo scanning electron microscope (Quanta 200 SEM; FEI, OR, USA). A cylindrical tissue scaffold was prepared for cyclic compressive testing. Testing was performed at ambient temperature in a water tank using a Model 4467 Universal Testing System (Instron, MA, USA) and a 50 N load cell was installed. A dog bone-shaped scaffold was prepared for tensile testing33. Glycol methacrylate embedding using Technovit 8100 resin (Heraeus Kulzer, Hanau, Germany) was performed according to the manufacturer's recommendations. Sections were stained with eosin Y and images were acquired by fluorescence microscopy. For image analysis, each image was first rendered binary form and ellipse fitting using computer software (ImageJ, National Institutes of Health, MA, USA) was then performed.
Human MSC culture and osteogenic differentiation
The cylindrical albumin tissue scaffold, with a 0.1-ml volume (approximately 5 mm in diameter and 3 mm in height), was prepared for tissue culture. The tissue scaffold was treated with 0.1 M ethanolamine at pH 9.5 for 1 h to block residual formaldehyde, followed by sequential washing with 70% alcohol, sterile water and culture medium. Human MSCs (Cat. No. PT-2501; Cambrex BioScience/Lonza Walkersville, MD, USA) were seeded at a density of 1 × 105 cells per scaffold. The cells were injected into a compressed, semi-dry tissue scaffold. The cultures were maintained in 5-ml gas-permeable culture tubes containing 1 ml of MSC growth medium (DMEM supplemented with 10% FBS and 1X Pen-Strep). The osteogenic differentiation basal medium was the same as the MSC growth medium in this study. The osteogenic induction medium was the MSC growth medium supplemented with 0.1 μM dexamethasone, 10 mM β-glycerophosphate and 50 μg/ml L-ascorbic acid 2-phosphate sesquimagnesium salt. The tissue culture tubes were statically incubated in a humidified 95% air, 5% CO2 incubator at 37°C. The tissue culture media was routinely changed every 3 or 4 days.
Cell viability and differentiation
An assay for human MSC cell growth in the albumin tissue scaffold was performed using PrestoBlue Cell Viability Reagent (Invitrogen, CA, USA) according to the manufacturer's recommendations. The measurement of alkaline phosphatase (ALP) activity was performed using a SensoLyte pNPP Alkaline Phosphatase Assay Kit (AnaSpec, CA, USA). The amount of p-nitrophenol developed in reaction was calculated using a molar extinction coefficient of 17800 M−1cm−1. One unit of phosphatase activity is defined as hydrolyse 1 μmol of pNPP per minute at 30°C. For the determination of calcium content, the cell-scaffold samples were fixed in acetone. After air drying, 40 μl of proteinase K solution (0.5 mg/ml proteinase K in 500 mM NaCl, 10 mM Tris Cl, pH 7.2, 1.5 mM MgCl2, 10 mM EDTA and 2% sodium dodecyl sulphate [SDS]) was added. The samples were kept at 60°C for 4 h. Acetic acid was added to the proteinase K digest to 10% and heated at 85°C for 10 min. The calcium concentrations in the samples were quantified by a QuantiChrom Calcium Assay Kit (BioAssay Systems, CA, USA). The DNA content in the protease K digest was quantified by a Quant-iT PicoGreen dsDNA Assay Kit (Invitrogen, CA, USA). For the staining of calcium phosphate deposits, the samples were fixed in 4% paraformaldehyde/phosphate-buffered saline (PBS) solution at room temperature for 1 h, washed with water and stained with alizarin red S dye (0.5% alizarin red S in 0.1% ammonium hydroxide). The stained samples were destained with 0.1% ammonium hydroxide, washed with acetone and air dried. The results are presented as the mean and standard deviation. Statistical analyses were performed using analysis of variance (ANOVA) and a P-value less than 0.05 was considered to be significant.
References
Sievert, K. D. The next step in urethral reconstruction. Lancet 377, 1130–1131 (2011).
Jungebluth, P. et al. Tracheobronchial transplantation with a stem-cell-seeded bioartificial nanocomposite: a proof-of-concept study. Lancet 378, 1997–2004 (2011).
Li, W. J., Laurencin, C. T., Caterson, E. J., Tuan, R. S. & Ko, F. K. Electrospun nanofibrous structure: a novel scaffold for tissue engineering. J Biomed Mater Res 60, 613–621 (2002).
Silva, G. A. et al. Selective differentiation of neural progenitor cells by high-epitope density nanofibers. Science 303, 1352–1355 (2004).
Zhang, S., Marini, D. M., Hwang, W. & Santoso, S. Design of nanostructured biological materials through self-assembly of peptides and proteins. Curr Opin Chem Biol 6, 865–871 (2002).
Ellis-Behnke, R. G. et al. Nano neuro knitting: peptide nanofiber scaffold for brain repair and axon regeneration with functional return of vision. Proc Natl Acad Sci U S A 103, 5054–5059 (2006).
Saleh, A. A. & Dionne, J. A. Toward efficient optical trapping of sub-10-nm particles with coaxial plasmonic apertures. Nano Lett 12, 5581–5586 (2012).
Marga, F. et al. Toward engineering functional organ modules by additive manufacturing. Biofabrication 4, 022001 (2012).
Ott, H. C. et al. Perfusion-decellularized matrix: using nature's platform to engineer a bioartificial heart. Nat Med 14, 213–221 (2008).
Ott, H. C. et al. Regeneration and orthotopic transplantation of a bioartificial lung. Nat Med 16, 927–933 (2010).
Uygun, B. E. et al. Organ reengineering through development of a transplantable recellularized liver graft using decellularized liver matrix. Nat Med 16, 814–820 (2010).
Orlando, G. et al. Production and implantation of renal extracellular matrix scaffolds from porcine kidneys as a platform for renal bioengineering investigations. Ann Surg 256, 363–370 (2012).
von Wolff, M. et al. Cryopreservation and autotransplantation of human ovarian tissue prior to cytotoxic therapy--a technique in its infancy but already successful in fertility preservation. Eur J Cancer 45, 1547–1553 (2009).
Lee, C. H. et al. Regeneration of the articular surface of the rabbit synovial joint by cell homing: a proof of concept study. Lancet 376, 440–448 (2010).
Smith, I. O. & Ma, P. X. Cell and biomolecule delivery for regenerative medicine. Science and Technology of Advanced Materials 11, 014102 (2010).
Pramanik, S., Pingguan-Murphy, B. & Osman, N. A. A. Progress of key strategies in development of electrospun scaffolds: bone tissue. Science and Technology of Advanced Materials 13, 043002 (2012).
Gallego, L. et al. Repair of rat mandibular bone defects by alveolar osteoblasts in a novel plasma-derived albumin scaffold. Tissue Eng Part A 16, 1179–1187 (2010).
Gallego, L., Junquera, L., Meana, A., García, E. & García, V. Three-dimensional culture of mandibular human osteoblasts on a novel albumin scaffold: growth, proliferation and differentiation potential in vitro. Int J Oral Maxillofac Implants 25, 699–705 (2010).
Gallego, L., Junquera, L., Meana, A., Alvarez-Viejo, M. & Fresno, M. Ectopic bone formation from mandibular osteoblasts cultured in a novel human serum-derived albumin scaffold. J Biomater Appl 25, 367–81 (2010).
Schulzki, T. et al. A prospective multicentre study on the safety of long-term intensive plasmapheresis in donors (SIPLA). Vox Sang 91, 162–173 (2006).
Thung, S. N., Wang, D. F., Fasy, T. M., Hood, A. & Gerber, M. A. Hepatitis B surface antigen binds to human serum albumin cross-linked by transglutaminase. Hepatology 9, 726–730 (1989).
Pontisso, P., Petit, M. A., Bankowski, M. J. & Peeples, M. E. Human liver plasma membranes contain receptors for the hepatitis B virus pre-S1 region and, via polymerized human serum albumin, for the pre-S2 region. J Virol 63, 1981–1988 (1989).
Hao, Y. A simple method for the preparation of human serum albumin. Vox Sang 36, 313–320 (1979).
Roeder, B. A., Kokini, K., Sturgis, J. E., Robinson, J. P. & Voytik-Harbin, S. L. Tensile mechanical properties of three-dimensional type I collagen extracellular matrices with varied microstructure. J Biomech Eng 124, 214–222 (2002).
Chvapil, M. Collagen sponge: theory and practice of medical applications. J Biomed Mater Res 11, 721–741 (1977).
Trounson, A., Thakar, R. G., Lomax, G. & Gibbons, D. Clinical trials for stem cell therapies. BMC Med 9, 52 (2011).
Ankrum, J. & Karp, J. M. Mesenchymal stem cell therapy: Two steps forward, one step back. Trends Mol Med 16, 203–209 (2010).
Karageorgiou, V. & Kaplan, D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26, 5474–5491 (2005).
Oettl, K. & Stauber, R. E. Physiological and pathological changes in the redox state of human serum albumin critically influence its binding properties. Br J Pharmacol 151, 580–590 (2007).
Sugio, S., Kashima, A., Mochizuki, S., Noda, M. & Kobayashi, K. Crystal structure of human serum albumin at 2.5 A resolution. Protein Eng 12, 439–446 (1999).
Donzelli, E. et al. Mesenchymal stem cells cultured on a collagen scaffold: In vitro osteogenic differentiation. Arch Oral Biol 52, 64–73 (2007).
Warnke, P. H. In-vivo tissue engineering of biological joint replacements. Lancet 376, 394–396 (2010).
Alston, S. M., Solen, K. A., Broderick, A. H., Sukavaneshvar, S. & Mohammad, S. F. New method to prepare autologous fibrin glue on demand. Transl Res 149, 187–195 (2007).
Author information
Authors and Affiliations
Contributions
I.L. wrote the main manuscript text and prepared Figures 1–4 and 8. P.L. and W.Y. prepared Figures 5–7. J.S. contributed to the data interpretation. W.N. prepared Figures 2D. H.S. supervised and coordinated all of the research, which was approved by all co-authors. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary info
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Li, PS., -Liang Lee, I., Yu, WL. et al. A Novel Albumin-Based Tissue Scaffold for Autogenic Tissue Engineering Applications. Sci Rep 4, 5600 (2014). https://doi.org/10.1038/srep05600
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05600
This article is cited by
-
Sulfonate-terminated carbosilane dendron-coated nanotubes: a greener point of view in protein sample preparation
Analytical and Bioanalytical Chemistry (2017)
-
pH and redox sensitive albumin hydrogel: A self-derived biomaterial
Scientific Reports (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.