Abstract
Multiple studies have hypothesized parity is associated with pancreatic cancer risk but obtained conflicting results. We conducted a meta-analysis (including a dose-response approach) of current available epidemiologic studies to investigate the association between parity and risk of pancreatic cancer. Ten cohort studies and ten case-control studies including 8205 cases were eligible for inclusion. The combined RR (relative risk) of pancreatic cancer for the parous vs. nulliparous was 0.91 (95% CI, confidence interval = 0.85–0.97, I2 = 39.0%, Ph = 0.01). We observed an inverse association between giving birth to two children pancreatic cancer risk with RR of 0.86 (95% CI = 0.80–0.93, I2 = 8.7%, Ph = 0.36). And no evidence supported there was non-linear (P = 0.33) or linear relationship (P = 0.14) between number of parity and risk of pancreatic cancer. Findings from this meta-analysis indicate that giving birth to two children has the lowest pancreatic cancer risk, mechanism of this protective effect needs further investigation.
Similar content being viewed by others
Introduction
Pancreatic cancer remains an aggressive malignancy that caused the eighth leading cancer-related mortality worldwide1. Currently, the only possibility for cure is surgery and only 20% patients have such chance due to late detection and diagnosis2. The extremely low 5-year survival rate (<5%) highlighted the urgency to find out the etiology of pancreatic cancer. However, in the past few decades, smoking has been confirmed as the greatest risk factor for pancreatic cancer and accounts for approximately 25% of cases3,4. The other suspected propensities such as alcohol consuming, BMI, physical activities, chronic pancreatitis and dietary factors yield disaccord results and need to be further validated5. Notwithstanding the recent genome-wide association studies identified several genetic susceptibility loci of pancreatic cancer6,7, only explaining ~4% of the cases8.
The differences in sex distribution9 which could not entirely be explained by cigarette smoking and the fact that steroid hormone receptors exist in normal and neoplastic human pancreatic tissue10,11,12 plus the findings that anti-estrogenic agents inhibit the growth of pancreatic cancer in both animal and human models13 prompted investigators to hypothesize that the reproductive factors may contribute to the etiology of pancreatic cancer. Up to now, numerous studies14,15,16,17 have focused on the roles of reproductive factors such as parity, age at first birth, age of menarche, age of menopause played in the development of pancreatic cancer, but obtained inconsistent findings. Of these factors the parity was the most extensively investigated and yielded conflicting results. The association ranged from protective effects18,19 to substantial increased risk with the increasing number of birth20.
The efforts of making a conclusion across these studies hampered by small sample size rendering limited power to detect the association and inconsistent referent groups making non comparability between studies. Therefore, we conducted a meta-analysis (including a dose-response approach) of current available epidemiologic studies to precisely evaluate the association between parity and risk of pancreatic cancer. And to extensively control the misclassification, we divided the number of parity into three groups and combined the corresponding data in each group separately.
Results
Study characteristics
Using the search strategy described in method paragraph we identified 107 articles, of which 80 articles were excluded after review of the title or abstract. 27 full-texts were reviewed and one article was excluded due to insufficient data21. Other two studies22,23 were drived out due to employ the measure of standard incidence rate ratios (SIRs) and standard mortality ratios (SMRs) to estimate the risk. In addition, two studies24,25 were removed for overlapping population with another longer duration follow-up report26 and larger sample size27. Two studies28,29 were removed for focusing on the number of pregnancy rather than the number of parity. Finally, 10 cohort studies16,17,18,19,20,26,30,31,32,33 and 10 case-control studies14,15,27,34,35,36,37,38,39,40 were eligible for this meta-analysis yielding a combined number of cases of 8205 (Figure 1). Characteristics of the 20 included studies are shown in Table 1. Among these studies, seven were conducted in USA15,18,30,32,33,35,40, two in Canada20,39, seven in Europe16,17,26,27,34,36,38, one in Japan31 and two in China19,37, one in Egypt14. The average of following- up duration of cohort studies was 18.65 years, ranged from 7.1 to 38 years. Cohort size ranged from 37459 to 1292462 and the number of cases varied from 52 to 1959. Almost all studies provided relative risk estimates adjusted for age (n = 19), most studies for smoking (n = 14), BMI (n = 8) and few controlled for history of diabetes (n = 5) (Table 1).
Parous vs. Nulliparous
Eleven studies including 38 reports reported the results using nulliparous (number of parity = 0) as reference. The summary multivariable-adjusted RR (95% CI) of pancreatic cancer associated with parity for parous versus nulliparous was 0.91 (95%CI = 0.85–0.97) (Table 2, Figure 2), indicating inverse association between parity and pancreatic cancer risk. Moderate between-study heterogeneity was observed among studies (P = 0.01, I2 = 39.0%). The 38 report-specific RRs of parous versus nulliparous ranged from a low of 0.89 (95% CI = 0.84–0.95) after omission of report by Teras et al18 to a high of 0.92 (95% CI = 0.86–0.98) after omission of report by Steven et al16. The power for the sample size of meta-analysis to detect an RR of 0.91 is more than 95%.
Different number of parity
The results of effects of different number of parity on pancreatic cancer risk were presented in Table 3. To explore the effects of different number of parity, we divided the number of parity into three groups and included the studies using number of parity of 0 or 1 as reference. 11 studies were assigned to the first group (number of parity = 2) and the summary multivariable-adjusted RR (95%CI) of pancreatic cancer associated with give birth to two children versus number of parity of 0 or 1 was 0.86 (95% CI = 0.80–0.93) with I2 = 8.7% (Ph = 0.36) (Figure 3). The second group (>2 and <5) contained 16 studies including 28 reports and our analysis of these reports yielded the combined risk estimate of 0.98 (95%CI = 0.89–1.09) with I2 = 53.7% (Ph < 0.01). 9 studies including 11 reports in the third group (≥5) yielded the combined risk estimate of 0.95 (95% CI = 0.75–1.20) with I2 = 66.3% (Ph < 0.01). The sensitivity analysis revealed that the pooled RRs for the second and third groups were similar before and after elimination of individual report. Considering the first group, the 11 report-specific RRs ranged from a low of 0.82 (95% CI = 0.76–0.89) after omission of report by Teras et al18 to a high of 0.92 (95% CI = 0.84–1.01) after omission of report by Steven et al16.
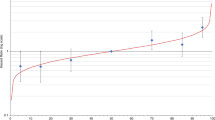
Dose response meta-analysis
The dose-response analysis on the number of parity and risk of pancreatic cancer involved 19 studies, we did not find a curve linear association between number of parity and risk of pancreatic cancer (P = 0.33 for non-linearity, I2 = 25%, Ph = 0.05).
The combined relative risk of pancreatic cancer for per live birth was 0.98 (95% CI = 0.95 to 1.01; P = 0.14 for linear trend) with I2 = 66.2% (Ph < 0.01), indicating no linear relationship between number of parity and risk of pancreatic cancer (Figure 4).
Meta-regression
We conducted a meta-regression to comprehensively explore the source of heterogeneity of parous versus nulliparous. Six factors such as study design, location, whether adjusted for smoking, BMI and diabetes, number of cases were included in the meta-regression model. In this model, the Adj R-squared was 100.00% and Prob > F was 0.0024, which indicated that the model was significant. After 100 times permutation, only study location appeared to be significant (adjusted P < 0.01) to explain the between-study heterogeneity.
Subgroup analyses
In the subgroup analysis of parous versus nulliparous, significant protective effects of parous on pancreatic cancer were observed in cohort studies (RR = 0.89, 95% CI = 0.84–0.95, I2 = 28.7%, Ph = 0.10), number of cases of more than 100 (RR = 0.89, 95% CI = 0.82–0.99, I2 = 60.2%, Ph = 0.01) and European population (RR = 0.82, 95% CI = 0.76–0.89, I2 = 16.3%, Ph = 0.27). In the subgroup analysis of effects of different number of parity on pancreatic cancer, the effects still turned out to be null in each stratum in both second and third groups. However, significant protective effects were observed in the subgroups of cohort studies (RR = 0.87, 95% CI = 0.77–0.99, I2 = 45.3%, Ph = 0.10), number of cases of more than 100 (RR = 0.87, 95% CI = 0.78–0.97, I2 = 44.9%, Ph = 0.11) and European population (RR = 0.84, 95% CI = 0.76–0.93, I2 = 14.5%, Ph = 0.33) of giving birth to two children (Table 3).
Publication bias
The result of Egger's test indicated no evidence of substantial publication bias for parous versus nulliparous (P = 0.52) and in the first group (P = 0.54), second group (P = 0.68) and third group (P = 0.70). And the of Begg's funnel plot of parous versus nulliparous was presented in Figure 5.
Discussion
We systematically reviewed ten cohorts and ten case-control studies including 8205 cases on the association between number of parity and pancreatic cancer risk. The factor became interesting candidate exposure related to pancreatic cancer because the difference of gender distribution and several biologic researches suggested that estrogen had protective effect against pancreatic cancer41,42,43 and pancreatic cancer might be in case another hormone-dependent cancer10,11,12. The current meta-analysis indicated that parous was inversely associated with pancreatic cancer risk compared with nulliparous. Giving birth to two children has the lowest risk of pancreatic cancer. We did not observe a non-linear or linear relationship between number of parity and pancreatic cancer. To the best of our knowledge, it is the first meta-analysis deeply mined the effects of different number of parity on pancreatic cancer risk.
The meta-regression analysis revealed that the study location might be the major source of between-study heterogeneity. We further carried out subgroup analysis by study design, study location and number of cases. And the between-study heterogeneity was largely removed when stratified according to study location, which further indicated that it mainly contributed to the heterogeneity. In the subgroup analysis of parous versus nulliparous, significant protective effects of parous on pancreatic cancer were identified in cohort studies, number of cases of more than 100 and European population. Similar with the subgroup analysis of parous, the subgroup analysis of different number of parity revealed that giving birth to two children was inversely associated with pancreatic cancer risk in those previously mentioned subgroups. The sample size of cohort studies was larger than the case-control studies and most studies conducted in Europe also have larger sample size than the studies conducted in North-America. So the detection of significant inverse associations might be due to dramatically increased statistic power of the combined large sample size. And the underlie mechanisms of the geographic variation of the effects of parity on pancreatic cancer risk is largely unknown and needs further validation and exploration.
Our meta-analysis indicated parous women had lower risk of pancreatic cancer compared with nulliparous women. Parous women are likely to have had longer periods of exposure to high levels of circulating estrogens. And animal studies reported that the estrogen had the inhibitory effect on the growth of preneoplastic pancreatic lesions or transplanted pancreatic carcinoma in rats11,12, indicating that estrogen may have effect against pancreatic cancer. However, the discrepancy between giving birth to two children and more than two is not fully understood, several potential biologic mechanisms might have been proposed. First, there was a progressive increase in insulin resistance during pregnancy44 and insulin resistance was suggested to be independently associated with pancreatic cancer risk45. Another explanation may be obesity which is known as a risk factor for pancreatic cancer46 and pregnant women are more tend to be obese. So the harmful effects of insulin resistance and obesity may counteract the protective effect of estrogen against pancreatic cancer.
Our current meta-analysis has several strengths. First, we included ten cohorts and ten case-control studies which enabled us significant statistical power to detect potential association. Second, to control misclassification, we combined different number of parity separately rather than used the highest versus the lowest number. Third, we applied the model adjusting for most established risk factors therefore largely controlled the confounders. In addition, no publication biases were detected, which suggested the entire pooled result may be unbiased.
Despite these advantages, some limitations of the current study should be acknowledged. First we did not have access to the primary data from the studies included in this meta-analysis, so could not perform additional adjustments for potential important covariates. Second, there is a relatively wide range of values for cutoff of highest level of number of parity so we could not accurately assign an exposure value to open-ended category, which might impact our current analysis.
In conclusion, the current meta-analysis indicates that parous is inversely associated with pancreatic cancer risk compared with nulliparous and giving birth to two children has the lowest pancreatic cancer risk. The exact mechanism of this protective effect needs further investigation.
Methods
Literature search and eligibility criteria
We searched the Pubmed and Embase databases from inception to November 2013 targeting the studies investigating the relationship between parity and the risk of pancreatic cancer. To undertake a comprehensive literature search, we used the combined terms: the MeSH heading and keywords relating to pancreatic neoplasms, the MeSH heading “reproductive history” and the keywords regarding to the exposure (reproductive factors, parity, birth), without language restriction. Reference lists of eligible studies and relevant review articles were also scanned to identify further pertinent studies. Studies were considered eligible if they met the following criteria: (a) the design of the study is prospective cohort study or case-control study; (b) investigate the relationship of parity and pancreatic cancer risk; (c) provide or allow the calculation of odds ratio (OR), relative risk (RR), or hazard ratio (HR) estimates with 95% CI. We excluded non-human, case reports, comparative studies not using an analytical epidemiologic design, or studies not reporting analyses of primary data (e.g., letters, editorials, narrative reviews) and not providing sufficient data. When multiple studies pertained to the same or partially overlapping populations, we used the result with the longest follow-up time or the largest sample size.
Data extraction
For each eligible study, two investigators (BBZ and LZ) independently carried out the eligibility evaluation, data abstraction and quality assessment and disagreements were resolved by consensus. The following data were extracted from eligible study: the first author, publication year, geographic region, demographics of participants, sample size (number of case and total participants), duration of follow-up or study period, covariates adjusted in the multivariable analysis, parity number categories, the corresponding OR or RR (with their 95% CI) and person-years for each category. For the RR, we chose the one represented the greatest degree control of potential confounders. The individual authors were contacted with E-mail if the data of interest were not shown in the publications.
Statistical analysis
Because the absolute risk of pancreatic cancer is low in human, the ORs and HRs were considered equivalent to RRs and we simply used RRs representing all of the three measures. To control confounding factors in the greatest extent, we extracted the maximally adjusted RRs (95%CI).
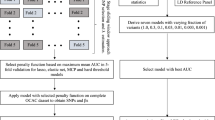
First of all, we evaluated the overall effect of parous compared with nulliparous, if the study considered nulliparous as reference, we summed up all the parous categories (number of parity >0) as ever parity in each study together and treated these different categories as different reports. For those studies considering number of parity of 0 or 1 as reference, we further assessed the effects of different number of parity. We first divided the number of parity into three groups (2, >2 and <5, ≥5) based on the pre-analysis of the data structure across these eligible articles and then combined the corresponding data in each group separately. We pooled the RRs for the overall effects of parous and respective effects of different groups in a random effects model described by DerSimonian and Laird47 which takes into account both within- and between-study variability. Then we explored the possible non-linear or linear relationship between number of parity and risk of pancreatic cancer using a random-effects dose-response meta-analysis according to the method described by Greenland and coworkers48,49. This method requires that the distribution of cases and person-years/number of cases and controls and the RR with 95%CI for at least three quantitative exposure categories. For each study, the median or mean level of exposure category was assigned to each corresponding RR. When the median or mean exposure level per category was not presented in the study, we assigned the midpoint of the upper and lower boundaries in each category as value of exposure. If the highest category was open-ended, we assumed that it had the same amplitude as the closest category. Furthermore, a potential cure linear relationship between parity and pancreatic cancer risk was assessed using restricted cubic splines with 3 knots at fixed percentiles (10%, 50% and 90%) of the distribution50. A P value for curve linearity or non-linearity was calculated by testing the null hypothesis that the coefficient of the second spline is equal to zero.
We quantified the extent of heterogeneity using Q-test51 and I2 score52. We conducted a meta-regression analysis and subgroup analyses to explore source of heterogeneity and subgroup analyses were performed, if feasible, according to study design, geographic region and number of cases. Sensitivity analysis was also performed to assess the influence of each individual report on overall estimates by sequential removal of individual studies. Funnel plots and the Egger's test53 were applied to examine the publication bias. All statistical analyses were carried out by Stata (version 10.0). The power of our meta-analysis was calculated using PowerV3.0 (http://www.mds.qmw.ac.uk/statgen/dcurtis/software.html).
References
Siegel, R., Ward, E., Brawley, O. & Jemal, A. Cancer statistics, 2011. CA. Cancer J. Clin. 61, 212–236 (2011).
Ahrendt, S. A. & Pitt, H. A. Surgical management of pancreatic cancer. Oncology (Williston Park, NY) 16, 725–734 (2002).
Zou, L. et al. Non-linear dose-response relationship between cigarette smoking and pancreatic cancerrisk: evidence from a meta-analysis of 42 observational studies. Eur. J. Cancer 50, 193–203 (2014).
Raimondi, S., Maisonneuve, P. & Lowenfels, A. B. Epidemiology of pancreatic cancer: an overview. Nature Reviews Gastroenterology and Hepatology 6, 699–708 (2009).
Lowenfels, A. B. & Maisonneuve, P. Epidemiology and risk factors for pancreatic cancer. Best Practice & Research Clinical Gastroenterology 20, 197–209 (2006).
Wu, C. et al. Genome-wide association study identifies five loci associated with susceptibility to pancreatic cancer in Chinese populations. Nat. Genet. 44, 62–66 (2011).
Huang, L. et al. Identification of common variants in BRCA2 and MAP2K4 for susceptibility to sporadic pancreatic cancer. Carcinogenesis 34, 1001–1005 (2013).
Wray, N. R., Yang, J., Goddard, M. E. & Visscher, P. M. The genetic interpretation of area under the ROC curve in genomic profiling. PLoS Genet. 6, e1000864 (2010).
Parkin, D. M., Bray, F., Ferlay, J. & Pisani, P. Global cancer statistics, 2002. CA. Cancer J. Clin. 55, 74–108 (2005).
Greenway, B., Iqbal, M. J., Johnson, P. J. & Williams, R. Oestrogen receptor proteins in malignant and fetal pancreas. Br. Med. J. (Clin. Res. Ed). 283, 751–753 (1981).
Sandberg, A. A., Kirdani, R. Y., Varkarakis, M. J. & Murphy, G. P. Estrogen receptor protein of pancreas. Steroids 22, 259–271 (1973).
Sandberg, A. A. & Rosenthal, H. E. Steroid receptors in exocrine glands: the pancreas and prostate. J. Steroid Biochem. 11, 293–299 (1979).
Longnecker, D. S. Hormones and pancreatic cancer. Int. J. Pancreatol. 9, 81–86 (1991).
Lo, A.-C. et al. Lifestyle, occupational and reproductive factors in relation to pancreatic cancer risk. Pancreas 35, 120–129 (2007).
Zhang, Y., Coogan, P. F., Palmer, J. R., Strom, B. L. & Rosenberg, L. A case–control study of reproductive factors, female hormone use and risk of pancreatic cancer. Cancer Causes Control 21, 473–478 (2010).
Stevens, R. J. et al. Reproductive history and pancreatic cancer incidence and mortality in a cohort of postmenopausal women. Cancer Epidemiol Biomarkers & Prev 18, 1457–1460 (2009).
Duell, E. J. et al. Menstrual and reproductive factors in women, genetic variation in CYP17A1 and pancreatic cancer risk in the European prospective investigation into cancer and nutrition (EPIC) cohort. Int. J. Cancer 132, 2164–75 (2012).
Teras, L. R., Patel, A. V., Rodriguez, C., Thun, M. J. & Calle, E. E. Parity, other reproductive factors and risk of pancreatic cancer mortality in a large cohort of US women (United States). Cancer Causes Control 16, 1035–1040 (2005).
Chang, C.-C., Chiu, H.-F. & Yang, C.-Y. Parity, age at first birth and risk of death from pancreatic cancer: Evidence from a cohort in Taiwan. Pancreas 39, 567–571 (2010).
Silvera, S. A. N., Miller, A. B. & Rohan, T. E. Hormonal and reproductive factors and pancreatic cancer risk: a prospective cohort study. Pancreas 30, 369–374 (2005).
La Vecchia, C., Negri, E., Franceschi, S. & Parazzini, F. Long-term impact of reproductive factors on cancer risk. Int. J. Cancer 53, 215–219 (1993).
Persson, I., Yuen, J., Bergkvist, L. & Schairer, C. Cancer incidence and mortality in women receiving estrogen and estrogen-progestin replacement therapy—long-term follow-up of a Swedish cohort. Int. J. Cancer 67, 327–332 (1996).
Adami, H. O., Persson, I., Hoover, R., Schairer, C. & Bergkvist, L. Risk of cancer in women receiving hormone replacement therapy. Int. J. Cancer 44, 833–839 (1989).
Kvåle, G., Heuch, I. & NILSSEN, S. Parity in relation to mortality and cancer incidence: a prospective study of Norwegian women. Int. J. Epidemiol. 23, 691–699 (1994).
Fernandez, E., La Vecchia, C., D'Avanzo, B. & Negri, E. Menstrual and reproductive factors and pancreatic cancer risk in women. Int. J. Cancer 62, 11–14 (1995).
Heuch, I., Jacobsen, B., Albrektsen, G. & Kvåle, G. Reproductive factors and pancreatic cancer risk: a Norwegian cohort study. Br. J. Cancer 98, 189–193 (2007).
Lucenteforte, E. et al. Reproductive and hormonal factors and pancreatic cancer risk in women. Pancreas 40, 460–463 (2011).
Hanley, A. J., Johnson, K. C., Villeneuve, P. J. & Mao, Y. Physical activity, anthropometric factors and risk of pancreatic cancer: results from the Canadian enhanced cancer surveillance system. Int. J. Cancer 94, 140–147 (2001).
Duell, E. J. et al. Menstrual and reproductive factors and pancreatic cancer in the SEARCH program of the IARC. Cancer Causes Control 20, 1757–1762 (2009).
Skinner, H. G. et al. Parity, reproductive factors and the risk of pancreatic cancer in women. Cancer Epidemiol Biomarkers & Prev 12, 433–438 (2003).
Lin, Y. et al. Association of menstrual and reproductive factors with pancreatic cancer risk in women: findings of the Japan Collaborative Cohort Study for Evaluation of Cancer Risk. J. Gastroenterol. 41, 878–883 (2006).
Prizment, A. E., Anderson, K. E., Hong, C.-P. & Folsom, A. R. Pancreatic cancer incidence in relation to female reproductive factors: Iowa Women's Health Study. JOP 8, 16–27 (2007).
Lee, E. et al. Reproductive Factors, Exogenous Hormones and Pancreatic Cancer Risk in the CTS. Am. J. Epidemiol. 178, 1403–1413, 10.1093/aje/kwt154 (2013).
De Mesquita, H. B., Maisonneuve, P., Moerman, C. & Walker, A. Anthropometric and reproductive variables and exocrine carcinoma of the pancreas: A population-based case-control study in The Netherlands. Int. J. Cancer 52, 24–29 (1992).
Cantor, K. P., Lynch, C. F. & Johnson, D. Reproductive factors and risk of brain, colon and other malignancies in Iowa (United States). Cancer Causes Control 4, 505–511 (1993).
Kalapothaki, V. et al. Tobacco, ethanol, coffee, pancreatitis, diabetes mellitus and cholelithiasis as risk factors for pancreatic carcinoma. Cancer Causes Control 4, 375–382 (1993).
Ji, B. T. et al. Anthropometric and reproductive factors and the risk of pancreatic cancer: A case-control study in Shanghai, China. Int. J. Cancer 66, 432–437 (1996).
Karlson, B. M., Wuu, J., Hsieh, C. c., Lambe, M. & Ekbom, A. Parity and the risk of pancreatic cancer: A nested case-control study. Int. J. Cancer 77, 224–227 (1998).
Kreiger, N., Lacroix, J. & Sloan, M. Hormonal factors and pancreatic cancer in women. Ann. Epidemiol. 11, 563–567 (2001).
Duell, E. J. & Holly, E. A. Reproductive and menstrual risk factors for pancreatic cancer: a population-based study of San Francisco Bay Area women. Am. J. Epidemiol. 161, 741–747, 10.1093/aje/kwi104 (2005).
Sumi, C., Longnecker, D. S., Roebuck, B. D. & Brinck-Johnsen, T. Inhibitory effects of estrogen and castration on the early stage of pancreatic carcinogenesis in Fischer rats treated with azaserine. Cancer Res. 49, 2332–2336 (1989).
Bourhis, J., Lacaine, F., Augusti, M. & Huguier, M. Protective effect of oestrogen in pancreatic cancer. The Lancet 330, 977 (1987).
Sumi, C., Brinck-Johnsen, T. & Longnecker, D. S. Inhibition of a transplantable pancreatic carcinoma by castration and estradiol administration in rats. Cancer Res. 49, 6687–6692 (1989).
Stanley, K., Fraser, R. & Bruce, C. Physiological changes in insulin resistance in human pregnancy: longitudinal study with the hyperinsulinaemic euglycaemic clamp technique. Br. J. Obstet. Gynaecol. 105, 756–759 (1998).
Wolpin, B. M. et al. Hyperglycemia, insulin resistance, impaired pancreatic beta-cell function and risk of pancreatic cancer. J. Natl. Cancer Inst. 105, 1027–1035, 10.1093/jnci/djt123 (2013).
Michaud, D. S. et al. Physical activity, obesity, height and the risk of pancreatic cancer. JAMA 286, 921–929 (2001).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 7, 177–188 (1986).
Greenland, S. & Longnecker, M. P. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am. J. Epidemiol. 135, 1301–1309 (1992).
Orsini, N., Bellocco, R. & Greenland, S. Generalized least squares for trend estimation of summarized dose-response data. Stata Journal 6, 40 (2006).
Harre, F. E., Lee, K. L. & Pollock, B. G. Regression models in clinical studies: determining relationships between predictors and response. J. Natl. Cancer Inst. 80, 1198–1202 (1988).
Higgins, J. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558 (2002).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557 (2003).
Egger, M., Smith, G. D., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 (1997).
Acknowledgements
This work is supported by Outstanding Young Scientists of Organization Department 2012, National HighTech Research and Development Program of China 2014AA020609 and Specialized Research Fund for the Doctoral Program of Higher Education 20130142110017 for Xiaoping Miao and the National Natural Science Foundation of China (NSFC-81001275, 81171878, 81222038).
Author information
Authors and Affiliations
Contributions
Conceived and designed the study strategy: X.P.M.; Acquisition of data: statistical analysis and interpretation of data B.B.Z., L.Z., W.C.; Drafting or revision of the manuscript: B.B.Z., J.H.; Reference collection and data management: N.S., J.Y.L., X.Q.C.; Wrote the manuscript: B.B.Z.; Prepared the tables and figures: C.L., Y.S., R.Z.; Study supervision: X.P.M.; All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Zhu, B., Zou, L., Han, J. et al. Parity and pancreatic cancer risk: evidence from a meta-analysis of twenty epidemiologic studies. Sci Rep 4, 5313 (2014). https://doi.org/10.1038/srep05313
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05313
This article is cited by
-
Which Aspects of Elderly Living Conditions are Important to Predict Mortality? The Complex Role of Family Ties at Home and in Institutions
Social Indicators Research (2019)
-
Long-term trends in pancreatic cancer mortality in Spain (1952–2012)
BMC Cancer (2018)
-
Environmental risk factors for pancreatic cancer: an update
Archives of Toxicology (2016)
-
Physical activity and risk of pancreatic cancer: a systematic review and meta-analysis
European Journal of Epidemiology (2015)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.