Abstract
Recently, infertility treatment-related psychological effects are receiving increased attention. However, whether sexual satisfaction is reduced amongst infertile couples remains to be elucidated. In this study, sexual satisfaction of Japanese infertile couples was assessed using a validated questionnaire designed to assess the male and female partner individually and the couple as a whole for the first time. This study randomly included 170 infertile couples seen at the outpatient clinic and 170 couples that had recently achieved spontaneous pregnancy. All couples were given the Japanese version of the Golombok-Rust Inventory of Sexual Satisfaction (GRISS). In couples aged 35 years or older, the male partners showed significantly worse sexual satisfaction scores than the female partners. Sexual satisfaction also deteriorated with therapeutic interventions, with mental factors affected more than physical factors. Therapeutic interventions such as timed sexual intercourse and assisted reproductive technology were considered emotionally stressful for infertile couples, with sexual satisfaction accordingly lower in this group than in couples achieving spontaneous pregnancy. GRISS successfully evaluated lower sexual satisfaction associated with infertility and hence is a useful tool for identifying couples whose sexual satisfaction could be enhanced by counselling or other stress-reduction modalities.
Similar content being viewed by others
Introduction
Sexual satisfaction is an integral part of life and human wellbeing. Therapeutic interventions to improve the chance of conceiving such as timed sexual intercourse and assisted reproductive technology are considered emotionally stressful for infertile couples1. Psychiatric morbidity has previously shown a significant association with the number of treatment cycles2. Furthermore, stressed couples were found to be less fertile, while infertile couples gave higher scores on depression and anxiety scales3,4. Psychological stress has been associated with lower pregnancy rates and a lower success rate of in vitro fertilization and embryo transfer5. However, whether sexual satisfaction is less amongst infertile couples than amongst couples who achieved a recent spontaneous pregnancy remains to be elucidated.
This study aimed to elucidate the sexual satisfaction characteristics of Japanese infertile couples for the first time using a validated self-administered structured questionnaire, the Japanese version of the Golombok-Rust Inventory of Sexual Satisfaction (GRISS)6. This assessment tool was designed to assess the sexual satisfaction of male and female partners individually and of the couple as a whole.
Results
In total, 93 of the 170 infertile couples (response rate, 54.7%) and 92 of the 170 pregnant couples (response rate, 54.1%) completed and returned the study questionnaire. Table 1 summarises the clinical characteristics of the study subjects. Because couples in the infertile group were significantly older for both men and women, had longer relationships and longer-lasting marriages than those in the pregnancy group, the two groups were compared according to age group.
Deterioration of the overall score
The overall GRISS score showed a moderate tendency to deteriorate with age (correlation coefficient (r) = 0.447 in men, 0.391 in women) (Figure 1). It also deteriorated with the length of relationship (r = 0.450 in men, 0.395 in women) and the length of marriage (r = 0.514 in men, 0.461 in women).
Proportion of low sexual satisfaction (overall score ≥ 5)
The sexual satisfaction of male partners was significantly lower than that of female partners in those aged 30 years or older. There was marked deterioration in overall scores for men aged 35 years or older and the difference between men and women also tended to increase with age (18.2% vs. 8.8% in 30- to 34-year-old pregnant couples; 19.2% vs. 11.5% in 30- to 34-year-old infertile couples; 65.5% vs. 12.5% in 35- to 39-year-old pregnant couples; 75.5% vs. 16.7% in 35- to 39-year-old infertile couples; 55.6% vs. 22.2% in 40- to 45-year-old pregnant couples; and 80.8% vs. 23.1% in 40- to 45-year-old infertile couples) (Figure 2). Thus, the infertile group had significantly worse overall scores in men aged 35 years or older than the group who achieved pregnancy (73.5% vs. 65.5%, P < 0.05 in 35- to 39-year-old men; 80.8% vs. 55.6%, P < 0.01 in 40- to 45-year-old men) (Figure 2).
Proportion of low sexual satisfaction (overall score ≥ 5).
The sexual satisfaction of male partners was significantly lower than that of female partners in those aged 30 years or older. There was marked deterioration in the overall score for sexual satisfaction in men aged 35 years or older and the differences in overall score between men and women also tended to increase with age. Men aged 35 years or older in the infertile group had significantly worse overall sexual satisfaction scores than men in the pregnancy group. P values were calculated using the Mann-Whitney U-test; differences with a P value < 0.05 were considered significant. Y-axis: Percentage of subjects in each group with an overall score of 5 or higher.
Impact of therapeutic interventions on sexual satisfaction
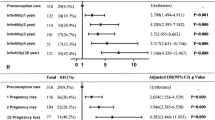
Couples who started therapeutic interventions such as timed sexual intercourse, intrauterine insemination (IUI) and in vitro fertilization and embryo transfer (IVF-ET) showed significantly worse overall scores (P < 0.0001 in men, P = 0.0004 in women) and the interventions significantly affected infrequency (P < 0.0001), non-sensuality (P = 0.0023 in men, P < 0.0001 in women), non-communication (P = 0.02), male dissatisfaction (P = 0.026) and male avoidance (P = 0.048). On the other hand, physical factors, such as impotence, premature ejaculation, vaginismus and anorgasmia were not significantly affected in either group (Figure 3).
Impact of therapeutic interventions on sexual satisfaction.
Couples who started therapeutic interventions such as timed sexual intercourse, intrauterine insemination (IUI), in vitro fertilization and embryo transfer (IVF-ET) showed significantly worse overall scores (P < 0.0001 in men, P = 0.0004 in women). In addition, the interventions significantly affected infrequency (P < 0.0001), non-sensuality (P = 0.0023 in men, P < 0.0001 in women), non-communication (P = 0.02), male dissatisfaction (P = 0.026) and male avoidance (P = 0.048). P values were calculated using the Mann-Whitney U-test and differences with a P value < 0.05 were considered significant.
Subscales showing the strongest correlation with deterioration of overall score
To clarify which subscales were most closely associated with low sexual satisfaction, we assessed the correlation between deterioration of the overall score and each subscale. In male partners, impotence (r = 0.778) showed the strongest correlation with deterioration of the overall score, while in female partners, it was non-sensuality (r = 0.722). In men and women, the subscales of infrequency (r = 0.710 in men, 0.629 in women) and non-communication (r = 0.661 in men, 0.656 in women) showed the strongest correlation. Furthermore, male avoidance (r = 0.627) and vaginismus (r = 0.625) were strongly correlated with deterioration of the overall score in men, whereas vaginismus (r = 0.607) and anorgasmia (r = 0.605) were strongly correlated with deterioration of the overall score in women. In addition, premature ejaculation (r = 0.509), male non-sensuality (r = 0.501) and female non-sensuality (r = 0.501) were moderately correlated with deterioration of the overall score in men, whereas impotence (r = 0.551) was moderately correlated with deterioration of the overall score in women.
Discussion
To our knowledge, this is the first study to assess sexual satisfaction characteristics of Japanese infertile couples using a validated, self-administered, structured questionnaire. The GRISS scores successfully associated reduced sexual satisfaction with infertility in the cohort assessed by questionnaire. In both infertile and pregnant couples, the overall score of sexual satisfaction showed a moderate tendency to deteriorate with age, length of relationship and length of marriage. Such a trend is generally associated with the increasing involvement of women in the workforce and consequent trend toward planned pregnancy, which has contributed to couples postponing reproductive attempts into their 30s and 40s7. Moreover, older couples statistically take a longer period to achieve pregnancy than younger couples8, further contributing to a vicious circle.
In couples aged 35 years and older, which is the main age group of couples seen for infertility treatment, male partners showed significantly worse sexual satisfaction scores than their female partners and these differences between men and women also tended to increase with age. These findings contrast to those of previous reports that infertile wives perceived their fertility problem as highly more stressful than their husbands9 and that infertility is more stressful for women than for men10. However, this study did find that mental factors were more affected than physical factors with therapeutic interventions and deterioration of the overall score in female partners showed the strongest correlation with infrequency, non-sensuality and non-communication, whereas in male partners the strongest correlation was with impotence. The present results thus indicated that sexual satisfaction is worse in male partners compared to female partners when the couples were assessed as a whole and with mental and physical factors taken into consideration.
The deterioration in sexual satisfaction of male partners could also be explained by traditional social patterns whereby Japanese male partners tend not to express feelings openly11,12, or by the use of more invasive and stressful assisted reproductive technologies such as intracytoplasmic sperm injection (ICSI) from the start of treatment if the male partner is diagnosed as subfertile13. On the other hand, Pal and Santoro14 implicated the age of male partners as a contributing factor, stating that “despite the decline in semen parameters and sexual performance with aging, this does not appear to have a major effect on the eventual fertility of the aging couple.”
Providing couples with counselling may contribute to enhanced sexual satisfaction and hence result in better fertility. Indeed, Merari et al.15 suggested a link between anxiety–depression dynamics involving the hypothalamic–pituitary–adrenal axis (HPA) and failure to conceive and proposed that psychological interventions aimed at reducing anxiety might increase the likelihood of conception. However, the directionality between HPA dysregulation and preconception stress or risk of infertility is still unclear16. Likewise, Tarlatzis et al.17 indicated that psychological counselling and supportive psychotherapy have been very effective in reducing high levels of anxiety in couples undergoing different reproductive treatments. Moreover, there is a wealth of information available regarding effective stress-reduction modalities such as yoga, meditation and mindfulness that demonstrably alleviated stress in studies of other health outcomes18,19,20. Another concern is that the response rate in this study was not high (54.7% or 54.1%). However, we must bear in mind that such studies can underestimate infertility treatment-related psychological effects because infertile couples suffering from severely deteriorated sexual relationships might not be totally cooperative towards questionnaires such as GRISS. Further investigation is therefore required to clarify a possible causal relationship between infertility treatment-related psychological effects and sexual dysfunction or dissatisfaction. In conclusion, our present use of GRISS successfully evaluated sexual satisfaction deteriorating with infertility and hence is a useful tool for identifying couples whose sexual satisfaction might be enhanced by counselling or other stress-reduction modalities.
Methods
Subjects
Infertile couples (n = 170) and couples with a recent spontaneous pregnancy (control; n = 170) consecutively seen at the outpatient clinics of Tokyo Women's Medical University were randomly included in the study. All enrolled couples were given a self-administered structured questionnaire (GRISS) to be returned either by post or at their next outpatient visit. This study was approved by the Institutional review board of Tokyo Women's Medical University and carried out in accordance with the Ethical Guidelines for Clinical Studies established by Japan Ministry of Health, Labour and Welfare. Written informed consent was obtained from all subjects before commencing the study.
Assessment measures
The GRISS questionnaire was designed in 1983 to assess the existence and severity of sexual problems of heterosexual couples or individuals in a heterosexual relationship6. A Japanese version of GRISS is in the process of development, linguistic validation and the first stage of the recommended procedure for cultural adaptation21. After conceptual analysis, forward translation, backward translation and comparison of the backward translation with the English version, a pilot study was conducted21.
Although there are many questionnaires validated and used in clinical studies on sexual satisfaction, we selected a questionnaire that 1) assesses male and female individual factors and the factors between the partners in a couple, 2) evaluates mental and physical factors, 3) does not include items on drug use or homosexuality, 4) includes only multiple-choice, but free-response, items, so that it is quick and easy to answer and 5) does not particularly define the reference period as past 7 days or 4 weeks. There are two versions of GRISS, one for women and one for men. Each version consists of 28 short items with a 5-point response format.
GRISS provides the overall scores and subscale scores of infrequency, non-communication, dissatisfaction, avoidance, non-sensuality, impotence [men], premature ejaculation [men], anorgasmia [women] and vaginismus [women]. All scores are converted to a scale (1 to 9), in which a higher score indicates greater sexual dysfunction. The construction has allowed for non-problematic variation between scale points 1 and 4.
Statistical analysis
Spearman's rank correlation coefficient was used to analyse bivariate association in this study and the Mann-Whitney U test was used to analyse group comparisons. Differences with a P value < 0.05 were considered statistically significant. Analyses were performed using SPSS version 13.0.
References
Kopitzke, E. J., Berg, B. J., Wilson, J. F. & Owens, D. Physical and emotional stress associated with components of the infertility investigation: perspectives of professionals. Fertil Steril. 55, 1137–1143 (1991).
Guerra, D., Llobera, A., Veiga, A. & Barri, P. N. Psychiatric morbidity in couples attending a fertility service. Hum Reprod. 13, 1733–1736 (1998).
Newton, C. R., Sherrard, W. & Glavac, I. The Fertility Problem Inventory: measuring perceived infertility-related stress. Fertil Steril. 72, 54–62 (1999).
Wischmann, T., Stammer, H., Scherg, H., Gerhard, I. & Verres, R. Psychosocial characteristics of infertile couples: a study by the ‘Heidelberg Fertility Consultation Service’. Hum Reprod. 16, 1753–1761 (2001).
Thiering, P., Beaurepaire, J., Jones, M., Saunders, D. & Tennant, C. Mood as predictor of treatment outcome after in vitro fertilization/embryo transfer technology (IVF/ET). J Psychosom Res. 37, 481–491 (1993).
Rust, J. & Golombok, S. The Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Br J Clin Psychol. 24, 63–64 (1985).
Klein, J. & Sauer, M. V. Assessing fertility in women of advanced reproductive age. Am J Obstet Gynecol. 185, 758–770 (2001).
Berkowitz, G., Skowron, M. L. & Lapinski, R. Delayed childbearing and outcome of pregnancy. N Engl J Med. 322, 659–664 (1990).
Abbey, A., Andrews, F. M. & Halrnan, J. Gender's role in responses to infertility. Psychol Women Q. 15, 295–316 (1991).
Freeman, E. W., Boxer, A. S., Rickels, K., Tureck, R. & Mastroianni, L., Jr Psychological evaluation and support in a program of in vitro fertilization and embryo transfer. Fertil Steril. 43, 48–53 (1985).
Ogrodniczuk, J. & Oliffe, J. The strong, silent type: Is masculinity bad for men's mental health? CrossCurrents: J Addict Ment Health. 13, 8–10 (2010).
Ingersoll-Dayton, B., Campbell, R. & Mattson, J. Forms of communication: A cross-cultural comparison of older married couples in the USA and Japan. J Cross-Cult Gerontol. 13, 63–80 (1998).
Rockliff, H. E., Lightman, S. L., Rhidian, E., Buchanan, H., Gordon, U. & Vedhara, K. A systematic review of psychosocial factors associated with emotional adjustment in in vitro fertilization patients. Human Reprod Update. (2014) Epub ahead of print.
Pal, L. & Santoro, N. Age-related decline in fertility. Endocrinol Metab Clin N Am. 32, 669–688 (2003).
Merari, D., Feldberg, D., Elizur, A., Goldman, J. & Modan, B. Psychological and hormonal changes in the course of in vitro fertilization. J Assist Reprod Genet. 9, 161–169 (1992).
Lynch, C. D., Sundaram, R., Maisog, J. M., Sweeney, A. M. & Buck Louis, G. M. Preconception stress increases the risk of infertility: results from a couple-based prospective cohort study-the LIFE study. Human Reprod. 29, 1067–1075 (2014).
Tarlatzis, I. et al. Psychosocial impacts of infertility on Greek couples. Hum Reprod. 8, 396–401 (1993).
Balaji, P. A., Varne, S. R. & Ali, S. S. Psychological effects of yogic practices and transcendental meditation in health and disease. N Am J Med Sci. 4, 442–448 (2012).
Yadav, R. K., Magan, D., Mehta, N., Sharma, R. & Pahapatra, S. C. Efficacy of short-term yoga-based lifestyle intervention in reducing stress and inflammation: preliminary results. J Altern Complement. 18, 662–667 (2012).
Carmody, J. & Baer, R. A. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. 31, 23–33 (2008).
Shimizu, S. et al. Linguistic validation of Golombok-Rust Inventory of Sexual Satisfaction (GRISS) for assessing Couples' Sexuality. J Fertil Implant. 28, 453–456 (2011). Japanese.
Acknowledgements
We greatly appreciate Professor Suzan Golombok of London University (incumbent: Centre for Family Research in the University of Cambridge) for invaluable advice and providing the GRISS, Associate Professor Raoul Breugelmans of the Department of International Medical Communications of Tokyo Medical University for editing the manuscript and Ms. Yukiko Tashiro and Ms. Hiroe Sakanaka for data collection.
Author information
Authors and Affiliations
Contributions
M.S., T.H. and S.I. contributed to the experimental design, data acquisition, data analysis and interpretation and to drafting of the article. N.K., H.O., H.M. and Y.Y. assisted with experimental design as well as data analysis and interpretation. All authors examined the data and approved the final manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images in this article are included in the article's Creative Commons license, unless indicated otherwise in the image credit; if the image is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the image. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Shoji, M., Hamatani, T., Ishikawa, S. et al. Sexual Satisfaction of infertile couples assessed using the Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Sci Rep 4, 5203 (2014). https://doi.org/10.1038/srep05203
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05203
This article is cited by
-
Impact of assisted reproduction treatment on sexual function of patients diagnosed with infertility
Archives of Gynecology and Obstetrics (2022)
-
The Inferto-Sex Syndrome (ISS): sexual dysfunction in fertility care setting and assisted reproduction
Journal of Endocrinological Investigation (2021)
-
Impact of Infertility on the Sexuality of Couples: an Overview
Current Sexual Health Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.