Abstract
The study was to explore whether auricular acupressure (AA) can relieve anxiety during the period from trans-vaginal oocyte retrieval to the embryo transfer in IVF treatment and whether AA can improve the outcomes of IVF. 305 infertile patients with tubal blockage who were referred for IVF were included. The women were randomized into a control group with 102 cases, a Sham-AA group with 102 cases and an AA group with 101 cases. The anxiety levels were rated with Spielberger's State Trait Anxiety Inventory and the Amsterdam Preoperative Anxiety and Information Scale. Data of clinical pregnancy rate (CPR), implantation rate (IR) and live birth rate (LBR) were obtained. The levels of neuropeptide Y (NPY) and transforming growth factor alpha (TGF-alpha) in the follicular fluids were detected with ELISA. After treatment, in AA group, the levels of state anxiety, preoperative anxiety and need-for-information were significantly lower, whereas CPR, IR, LBR and NPY levels in the follicular fluids were markedly higher than Sham-AA group and control group. We concluded that AA could help to reduce anxiety levels associated with IVF and improves the outcomes of IVF partly through increasing the levels of NPY in the follicular fluids.
Similar content being viewed by others
Introduction
Auricular acupressure (AA), a micro-acupuncture technique similar to reflexology, is effective in reducing state anxiety in both healthy volunteers and the adult patients awaiting their surgery1,2. It was also effective in improving functions of the endocrine system3,4,5,6,7. AA was first described in French and Chinese medicine and rapid progress has been made on the theory and practice of AA since Paul Nogier, a French practitioner, discovered the inverted-fetus shape distribution pattern of auricular acupoints. AA works by stimulating the central nervous system through the cranial nerves/spinal nerves on the auricle of the ear and it can be easily accepted by people for its effectiveness and non-invasion.
In vitro fertilization (IVF), as a choice for over 1,000,000 infertile couples each year, represents the culmination of medical, scientific and social evolution, which is linked to over 3,000,000 babies born worldwide8. However, according to the reports of European Society of Human Reproduction and Embryology (ESHRE), no significant increase in the implantation rate (IR) of cleaving embryos has been obtained in the last years, although there have been many relevant techniques emerging to improve the IVF outcomes9,10,11.
IVF is a multidimensional stressor and the treatment itself constitutes the primary stressor, which is most likely to evoke anxiety12. As early as in 1990, anxiety was found in 10.6% of the infertile patients prior to IVF using the Spielberger's State Trait Anxiety Inventory (STAI)13. Anxiety disorders were found in 23.2% of Chinese patients undergoing IVF or ICSI14. In Sweden, approximately 30% of the infertile patients undergoing IVF fulfilled criteria for a depressive and/or anxiety disorder, including sub-threshold diagnosis15. The anxiety may be caused by the invasive nature of the therapy itself, the knowledge that IVF is often the last hope for a biological child and the high cost of treatment. The highest stress and anxiety levels during an IVF treatment existed shortly before trans-vaginal oocyte retrieval (TVOR), which might negatively influence the implantation phase16,17. Stress, anxiety and depression contribute to lower pregnancy rates among patients undergoing IVF18. Both anxiety and depression negatively influenced the clinical pregnancy rate (CPR) of IVF treatment in patients with tubal factor infertility19.
Recently, complementary and alternative medicines, especially acupuncture, have been chosen by numerous couples before they commenced infertility treatment and some of them chose to use it as an adjunct while undergoing infertility treatment. More than 40 studies have been conducted to explore the effects of acupuncture on IVF outcomes since 1996. However, the conclusions were inconsistent and few of them have systematically evaluated the effects of acupuncture on the psychological parameters of IVF patients. Moreover, none has been done to explore the effects of AA as an adjunct to improve the outcomes of IVF. We therefore designed a prospective, randomized and controlled trial to determine whether AA can relieve anxiety for infertile patients with tubal blockage during the period from TVOR to embryo transfer (ET) in IVF treatment and improve the outcomes of IVF. As neuropeptide Y (NPY) and transforming growth factor alpha (TGF-alpha) play important roles in regulation of ovarian functions and follicular growth20,21,22,23,24,25, we also measured the levels of NPY and TGF-alpha in the follicular fluids of the patients. In our study, a relatively large number of patients were included and two different psychological measurements were used.
Results
The baseline characteristics
As shown in Table 1, there were no significant differences among the control group, Sham-AA group and AA group in all the baseline characteristics, including ages, body mass index (BMI), duration of infertility, the serum levels of luteinizing hormone (LH), follicle stimulating hormone (FSH), total testosterone (TT) and estradiol (E2) on the 3rd day of spontaneous menstrual cycle, the cycle length, the dosage of recombinant FSH administered, induction length, number of follicles, number of follicles with diameters of more than 14 mm, number of embryos transferred per cycle, embryo cleavage rate, good-quality embryo rate, fertilization rate, the education levels, employment type and living area of the patients (P>0.05).
The levels of state anxiety, preoperative anxiety and need-for-information
No significant differences existed among the three groups on the levels of state anxiety, preoperative anxiety (including anesthesia related anxiety and surgery related anxiety) and need-for-information at T1 (Table 2). At T2, after AA treatment for five days, the levels of state anxiety, preoperative anxiety (including anesthesia related anxiety and surgery related anxiety) and need-for-information in AA group were markedly decreased compared with Sham-AA group and control group (P<0.05) (Table 2). There were no significant differences between Sham-AA group and control group on the levels of state anxiety and preoperative anxiety (including anesthesia related anxiety and surgery related anxiety) at T2, however, the need-for-information levels of Sham-AA group were markedly lower than those of the control group (P<0.05) (Table 2).
IVF outcomes
As shown in Table 2, the CPR, IR and live birth rate (LBR) of AA group were significantly higher than those of the Sham-AA group and control group respectively (P<0.017) and there was no significant difference between Sham-AA and control groups (P>0.017).
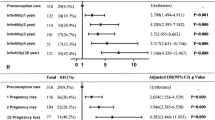
NPY and TGF-alpha levels in follicular fluids
As shown in Figure 1, NPY levels in the follicular fluids of the AA group was significantly higher than those of Sham-AA and control groups respectively (P<0.05) and no marked difference existed between Sham-AA and control groups. There were no significant differences on TGF-alpha levels in the follicular fluids among the three groups.
(A) Neuropeptide Y (NPY) levels in follicular fluids of auricular acupressure (AA) group, Sham-AA group and control group. (B) Transforming growth factor alpha (TGF-alpha) levels in follicular fluids of AA group, Sham-AA group and control group. For all panels, results were expressed as mean ± S.D. *P<0.05 (ANOVA).
Adverse result
No side-effect was reported in either group during the period of the research.
Discussion
The present study found that AA applied at three specific points is effective in relieving anxiety levels during the period from TVOR to ET and notably improves the outcomes of IVF partly through increasing the levels of NPY in the follicular fluids.
Acupressure involves stimulation of acupoints and meridians without use of needles. Stimulating a particular acupoint with acupressure can activate small myelinated nerve fibers that send impulses into the spinal cord, midbrain, pituitary and hypothalamus26. AA, a treatment method derived from acupressure and ear acupuncture, is a safer, more effective, economic and simple approach3,6,27,28,29,30,31. The practical advantages of AA include32,33: (1) only minimal equipment is needed and any physicians or nurses can perform this treatment; (2) physicians as well as other health care providers who have rare or no experience in traditional Chinese medicine can learn this technique within a few hours and can use it whenever indicated; (3) it is almost a “no-cost” intervention; (4) AA is non-invasive and does not affect the integrity of the epidermis. Acupressure, including AA, has been found to be safe and effective in decreasing prehospital anxiety32, reducing preoperative anxiety34,35, alleviating stress33 and improving quality of life36,37.
IVF is usually the final treatment option for infertile couples and failure will probably mean their remaining childless38. It is therefore not surprising that both patients and men always demonstrate elevated levels of anxiety during IVF treatment39,40. In IVF treatment, the state anxiety is caused by the fear of TVOR, or the strain of the emotional moment at ET, which can be measured by the levels of anxiety at a certain time-point41. Reviews have suggested distress including anxiety has adverse effects on IVF outcomes42,43,44, however, the conclusions were different in some other researches41. The differences of these findings may be caused by the variance on the population studied, time-points of assessments, details of the inclusion criteria, size of the studies, definition of indicators of IVF outcomes, types of psychological tests and stages of sampling. In the study, STAI was used to rate the levels of state anxiety and Amsterdam Preoperative Anxiety and Information Scale (APAIS) was applied to measure the levels of preoperative anxiety (including anesthesia related anxiety and surgery related anxiety) and need-for-information. STAI has been widely used as a standardized tool for assessment of state anxiety in acute settings45,46. To date, STAI has been used in more than 1,000 peer-reviewed medical publications46 and has recently been used as a control for other scales47,48. As a simple and reliable measure of preoperative anxiety and need-for-information, APAIS is easy to use and correlates well with other scales47,48,49. Here we translated APAIS into Chinese and compared it with a background questionnaire (STAI) to validate its use. In the present study, the correlation coefficient between the state anxiety items in STAI and the preoperative anxiety items in APAIS was 0.569 (P<0.001), which was consistent with the previously reported correlation between the state anxiety component of STAI and the preoperative anxiety component of APAIS in patients in the preoperative period. Factor analysis with oblique rotation revealed two factors: anxiety (with an eigenvalue of 2.877) and need-for-information (with an eigenvalue of 1.154), which explained 67% of the total variance. In this study, we found AA at the three auricular acupoints--Shenmen (TF4), Endocrine (CO18) and Internal Genitals (TF2) notably decreased the levels of state anxiety, preoperative anxiety (including anesthesia related anxiety and surgery related anxiety) and need-for-information of the patients undergoing IVF treatment. Consequently, AA at the three acupoints can be performed on the patients who feel anxiety during the period from TVOR to ET in IVF treatment. In the study, all the three acupoints used for the subjects of Sham-AA group have not been documented to relieve anxiety, improve functions of the endocrine system or regulate functions of the female reproductive system.
In our study, the first psychological measurement was performed on the morning of one day before TVOR, as we wished to explore the baseline levels of the patients before TVOR. The time-point of the second measurement was chosen based on our clinical experiences that patients often express eminent feelings of anxiety during the period from one day before TVOR to the day of ET. It is valuable to measure the levels of state anxiety, preoperative anxiety and need-for-information on the morning of the day of ET because in that occasion, AA has been applied for five days and the ET operation will start shortly.
In the present study, no significant differences on the baseline characteristics existed among the three groups. The patients' age, BMI and other known confounding factors such as duration of infertility, the serum levels of LH, FSH, TT and E2 on the 3rd day of spontaneous menstrual cycle, the cycle length, the dosage of recombinant FSH administered, induction length, number of follicles, number of follicles with diameters of more than 14 mm, number of embryos transferred per cycle, embryo cleavage rate, good-quality embryo rate and fertilization rate have been well controlled in the present study. These factors have been shown important in large prospective studies50,51. The lifestyle factors such as smoking and alcohol intake were also well controlled in the study. The factors associated with cultural settings, such as the education levels, employment type and living area of the patients were also well controlled.
In the study, CPR, IR and LBR were selected as the parameters to evaluate the IVF outcomes. We found that AA at the three specific auricular acupoints eminently improves CPR, IR and LBR of the IVF patients, suggesting that AA may have promises to improve the outcomes of IVF. To further explore the possible mechanism underlying AA improving the outcomes of IVF, we detected the levels of NPY and TGF-alpha in the follicular fluids of the IVF patients. As the most widely distributed neurohormone in the body, NPY can regulate the functions of the hypothalamic-pituitary-ovarian axis. It reaches the ovary via the plexus ovarian nerve and high concentrations of NPY have been found in follicular fluids20,21,22,52. The concentration of NPY are finely tuned by fluctuations in the concentration of ovarian steroid hormones52. NPY is supposed to play important roles in regulating ovarian functions, follicular growth and ovulation. A prospective, randomized and multicentre clinical trial including 286 patients undergoing IVF treatment found electro-acupuncture significantly increased the levels of NPY in follicular fluids, which may be important for human ovarian steroidogenesis53. TGF-alpha, as a 50 amino acid polypeptide present predominantly in theca cells of antral follicle, has been found to regulate the growth of follicles23,24. TGF-alpha in the follicular fluids plays a pronounced role in oocyte maturation during late follicular phase and it simulates the action of LH in preovulatory follicles54. TGF-alpha also plays an important role in preventing apoptosis of granulosa cells in preovulatory follicles55. We found NPY levels in the follicular fluids of the AA group was significantly higher than those of Sham-AA and control groups respectively (P<0.05) and no marked difference existed between Sham-AA and control groups. There were no significant differences on TGF-alpha levels in the follicular fluids among the three groups. Consequently, NPY may be partly involved in AA improving outcomes of the IVF patients.
In the present study, no side-effect was reported in either group during the period of the research, demonstrating that AA is a safe and non-invasive intervention to improve the outcomes of IVF patients and to reduce the associated anxiety levels.
The present research was conducted in Reproductive Medicine Center of Zhejiang Province, China and more than 4000 IVF/ICSI cycles are performed in the Reproductive Medicine Center per year. Findings from this study have implications for health care providers to consider incorporating AA in their clinical practices when caring for infertile patients with IVF treatment. However, some further relevant indicators should be included, such as fertilization rate, embryo cleavage rate, good-quality embryo rate and incidence of birth defects. As some potential factors may influence the applicability of Sham-AA, including the patient's knowledge, expectation and experience of AA, these factors should be considered in the future studies. As multi-centre trials using the same study design may reduce the variation caused by the different protocols for IVF and differences in baseline CPR and LBR observed between different centers, more large-size, randomized, multicentre, double-blinded and placebo-controlled trials are supposed to be conducted in the future and further research should also be done on the mechanism involved.
Methods
Subjects
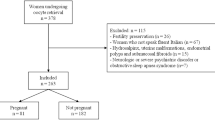
In a six-month period (January, 2011 to June, 2011), we screened 405 infertile patients with tubal blockage who were referred to Department of Reproductive Endocrinology, Women's Hospital, School of Medicine, Zhejiang University, China (Reproductive Medicine Center of Zhejiang Province, China) for IVF. Among the patients screened, 94 patients did not meet the inclusion criteria. For four patients, consents were not obtained and two patients were excluded for other reasons. Finally, 305 infertile patients with tubal blockage were included in the study. The randomization was done two days before TVOR, when the women came to the centre to prepare for TVOR. Having been randomized, the control group had 102 cases, Sham-AA group 102 cases and AA group 101 cases. The ET treatment was conducted three days after TVOR and all the patients had completed both of TVOR and ET. In the statistical analysis, all of the patients were included without missing cases during the research (Fig 2).
The flow chart of the progress of participants through the trial.
The subjects of auricular acupressure (AA) group and Sham-AA group were asked to press the acupoints four times a day (08:00, 12:00, 16:00 and 20:00 h respectively) with 15 min each time by themselves. The AA treatment consisted of six days (from 12:00 h of one day before trans-vaginal oocyte retrieval to 20:00 h of the next day of embryo transfer) and was conducted on the two ears simultaneously.
All experimental protocol was approved by the Institutional Review Board of Women's Hospital, School of Medicine, Zhejiang University. The aim and methodology of the study were explained to the patients. The methods were carried out in accordance with the approved guidelines. The study was undertaken with the understanding and appropriate informed consent of each participant. The infertile patients with tubal blockage who were referred to our department for IVF were included in the study. They were otherwise healthy women with regular menstrual cycles and normal sex hormone levels and no other pelvic pathology existed. No structural abnormalities of uterus and ovaries were found by vaginal ultrasound or laparoscopy. None of the patients had received salpingectomy or assisted reproductive technology (ART) therapy before. We excluded all the patients who were not fluent in Chinese, the patients with neurologic or psychiatric disorders, the patients who were taking any tranquillizer, acupressure or acupuncture therapy, patients with an ear deformity, or the patients with a history of smoking or drinking. All the partners of the patients had normal spermiograms and sperm morphology. The present study adheres to the Consolidated Standards of Reporting Trials (CONSORT) statement and Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA). The trial was registered at Australian New Zealand Clinical Trials Registry (ANZCTR) with the identifier ACTRN 12611000899943 (http://www.ANZCTR.org.au/ACTRN12611000899943.aspx).
Subjects were randomized into an AA group, a Sham-AA group or a control group with the use of a randomization chart constructed in Microsoft Excel that randomized numbers into three groups. The random allocation sequence was concealed until interventions were assigned. A nurse enrolled the participants and assigned participants to their groups. The IVF clinicians and laboratory staff were blinded to the group assignment. The AA protocol was developed based on the clinical experiences of our hospital, literatures and the consultation with 10 experts in Chinese medicine. The AA treatment was performed by two independent trained nurses who were not involved in the study and they were blinded to the group assignment.
Group and administration
AA group: Shenmen (TF4, located at the bifurcation of the crura of antihelix), Endocrine (CO18, located at the bottom part of the incisura intertragica) and Internal Genitals (TF2, located at the middle point of the anterior portion of the triangular fossa) were selected as the auricular acupoints (Fig 3). Shenmen (TF4) functions to relieve anxiety. Endocrine (CO18) and Internal Genitals (TF2) improve functions of the endocrine system and regulate functions of the female reproductive system. After the above acupoints were sterilized with 75% alcohol, AA was performed by using acupressure seeds named Semen vaccariae. The seed was kept in place by a piece of opaque adhesive patch and fixed onto the acupoint selected. The subjects were asked to press the acupoints four times a day (08:00, 12:00, 16:00 and 20:00 h respectively) with 15 min each time by themselves. The strength should make the local auricle congestive, flushed and ache. The AA was conducted on the two ears simultaneously. The AA treatment consisted of six days (from 12:00 h of one day before TVOR to 20:00 h of the next day of ET). All the subjects were instructed on: the procedure, duration and intensity of AA; the methods of keeping acupressure patches in the right place and protecting them; and recording the time of application of AA and any side-effects in a diary.
The auricular acupoints selected.
Shenmen (TF4, located at the bifurcation of the crura of antihelix), Endocrine (CO18, located at the bottom part of the incisura intertragica) and Internal Genitals (TF2, located at the middle point of anterior portion of the triangular fossa) were selected in auricular acupressure (AA) group; Triple Energizer (CO17, located in the cavum conchae), Stomach (CO4, located at the commissure of superior concha and inferio concha, just below the disappearance of the crus of the helix) and Large Intestine (CO7, located at the inner 1/3 of the crus of the helix, lying at the lower portion of the superior concha) were selected in Sham-AA group.
Sham-AA group: Triple Energizer (CO17, located in the cavum conchae), Stomach (CO4, located at the commissure of superior concha and inferio concha, just below the disappearance of the crus of the helix) and Large Intestine (CO7, located at the inner 1/3 of the crus of the helix, lying at the lower portion of the superior concha) were selected as the “sham” auricular acupoints (Fig 3). All the manipulation and process were exactly the same as the AA group above.
Control group: The patients in the control group only followed the routine procedure of IVF treatment and no AA was applied on them.
Collection of follicular fluids
The long agonist protocol for controlled ovarian hyperstimulation (COH) was used as previously described56. The follicular fluids were sampled by trans-vaginal ultrasound-guided puncture and aspiration of the follicles with diameters of 16–18 mm.
Index and method
The levels of state anxiety, preoperative anxiety (including anesthesia related anxiety and surgery related anxiety) and the need-for-information were evaluated respectively on the morning of one day before TVOR (defined as time-point T1) and on the morning of the day of ET (defined as time-point T2) by an independent gynecologist and two independent psychologists who were both out of the research team. They were all blinded to the group assignment. The levels of state anxiety were measured with the Chinese version of STAI, which is characterized by high reliability and good construct validity57,58. STAI consists of 20 short items measuring state anxiety which refers to transitory emotional arousal or situational distress at a particular moment in time59. These items reflect experiential, cognitive and behavioral aspects of state anxiety59. The score of each item ranges from 1 to 4 and a higher score reflects a higher level of state anxiety59. In the present study, the STAI's reliability was 0.899 and 0.911 respectively at T1 and T2. The levels of preoperative anxiety and the need-for-information were measured with the APAIS, a simple and reliable measure with good validity48,49,60. The score of each item ranges from 1 to 4 and higher scores reflect higher levels of preoperative anxiety and the need-for-information. APAIS's reliability with the present samples was 0.794 and 0.738 respectively at T1 and T2. Data of CPR (defined as the presence of at least one gestational sac or fetal heartbeat, confirmed by trans-vaginal ultrasound), IR (defined as the number of gestational sacs per number of transferred oocytes) and LBR (defined as the presence of a baby born alive after 24 weeks gestation) for all the patients were obtained. The levels of NPY and TGF-alpha in the follicular fluids were detected with ELISA (R&D Systems, MN, U.S.A).
Sample size and Data analysis
The sample size was analyzed using Power Analysis and Sample Size (PASS 11.0). Based on the records of our hospital, a CPR of 0.35 was estimated in the control population and a CPR of 0.41 and 0.53 was respectively estimated in Sham-AA population and AA population. A sample size of 298 achieves 80% power to detect an effect size (W) of 0.18 using a 2 degrees of freedom Chi-Square Test with a significance level (alpha) of 0.05. Based on the records of our hospital, an IR of 0.20 was estimated in the control population and a CPR of 0.22 and 0.39 was respectively estimated in Sham-AA population and AA population. A sample size of 267 achieves 80% power to detect an effect size (W) of 0.19 using 2 degrees of freedom Chi-Square Test with a significance level (alpha) of 0.05.
Data were analyzed using the Statistical Package for Social Sciences (SPSS 19.0 for Windows). The data of ages, BMI, duration of infertility, the serum levels of LH, FSH, TT and E2 on the 3rd day of spontaneous menstrual cycle, the cycle length, the dosage of recombinant FSH administered, induction length, number of follicles, number of follicles with diameters of more than 14 mm, number of embryos transferred per cycle, STAI scores, APAIS scores and the levels of NPY and TGF-alpha were found normally distributed using the Kolmogorov-Smirnov (KS) test. The comparisons among different groups were performed with one-way analysis of variance (ANOVA) and multiple comparison tests were conducted with Bonferroni correction procedure. Chi-Square tests were used to detect the data of CPR, IR, LBR, embryo cleavage rate, good-quality embryo rate, fertilization rate, the education levels, employment type and living area of the patients. For Chi-Square tests among three groups, the adjusted significance level for each comparison was set at P = 0.017(0.05/3) to give a significance level of 0.05 over all three tests. For all the other hypothesis tests, significance level was set at P = 0.05 and two-tailed tests were used.
References
Wang, S. M., Peloquin, C. & Kain, Z. N. The use of auricular acupuncture to reduce preoperative anxiety. Anesth Analg 93, 1178–1180 (2001).
Wang, S. M. & Kain, Z. N. Auricular acupuncture: a potential treatment for anxiety. Anesth Analg 92, 548–553 (2001).
Zhou, J., Qu, F., Sang, X., Wang, X. & Nan, R. Acupuncture and Auricular Acupressure in Relieving Menopausal Hot Flashes of Bilaterally Ovariectomized Chinese Women: A Randomized Controlled Trial. Evid Based Complement Alternat Med 2011, 1–8 (2011).
Kung, Y. Y., Yang, C. C., Chiu, J. H. & Kuo, T. B. The relationship of subjective sleep quality and cardiac autonomic nervous system in postmenopausal women with insomnia under auricular acupressure. Menopause 18, 638–645 (2011).
Hsieh, C. H. The effects of auricular acupressure on weight loss and serum lipid levels in overweight adolescents. Am J Chin Med 38, 675–682 (2010).
Wang, M. C., Hsu, M. C., Chien, L. W., Kao, C. H. & Liu, C. F. Effects of auricular acupressure on menstrual symptoms and nitric oxide for women with primary dysmenorrhea. J Altern Complement Med 15, 235–242 (2009).
Liu, C. F., Yu, L. F., Lin, C. H. & Lin, S. C. Effect of auricular pellet acupressure on antioxidative systems in high-risk diabetes mellitus. J Altern Complement Med 14, 303–307 (2008).
Horsey, K. 3,000,000 IVF Babies born worldwide since 1979. Presented at the annual conference of the European Society of Human Reproduction and Embryology. (ESHRE), Prague, Czech Republic. (2006, June 18–21).
Nygren, K. G. & Andersen, A. N. Assisted reproductive technology in Europe, 1998. Results generated from European registers by ESHRE. European Society of Human Reproduction and Embryology. Hum Reprod 16, 2459–2471 (2001).
Chambers, G. M., Sullivan, E. A., Ishihara, O., Chapman, M. G. & Adamson, G. D. The economic impact of assisted reproductive technology: a review of selected developed countries. Fertil Steril 91, 2281–2294 (2009).
Andersen, A. N. et al. Assisted reproductive technology in Europe, 2004: results generated from European registers by ESHRE. Hum Reprod 23, 756–771 (2008).
Verhaak, C. M. et al. Women's emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update 13, 27–36 (2007).
Newton, C. R., Hearn, M. T. & Yuzpe, A. A. Psychological assessment and follow-up after in vitro fertilization: assessing the impact of failure. Fertil Steril 54, 879–886 (1990).
Chen, T. H., Chang, S. P., Tsai, C. F. & Juang, K. D. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod 19, 2313–2318 (2004).
Volgsten, H., Skoog Svanberg, A., Ekselius, L., Lundkvist, O. & Sundstrom Poromaa, I. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Hum Reprod 23, 2056–2063 (2008).
Boivin, J. & Takefman, J. E. Stress level across stages of in vitro fertilization in subsequently pregnant and nonpregnant women. Fertil Steril 64, 802–810 (1995).
Smeenk, J. M. et al. Stress and outcome success in IVF: the role of self-reports and endocrine variables. Hum Reprod 20, 991–996 (2005).
Klonoff-Cohen, H. & Natarajan, L. The concerns during assisted reproductive technologies (CART) scale and pregnancy outcomes. Fertil Steril 81, 982–988 (2004).
Li, X. H. et al. Baseline psychological stress and ovarian norepinephrine levels negatively affect the outcome of in vitro fertilisation. Gynecol Endocrinol 27, 139–143 (2011).
McNeill, D. L. & Burden, H. W. Peripheral pathways for neuropeptide Y- and cholecystokinin-8-immunoreactive nerves innervating the rat ovary. Neurosci Lett 80, 27–32 (1987).
Jorgensen, J. C. et al. Neuropeptide Y in the human female genital tract: localization and biological action. Am J Physiol 257, E220–227 (1989).
Jorgensen, J. C., O'Hare, M. M. & Andersen, C. Y. Demonstration of neuropeptide Y and its precursor in plasma and follicular fluid. Endocrinology 127, 1682–1688 (1990).
Tamura, M. et al. Expression of epidermal growth factors and epidermal growth factor receptor in normal cycling human ovaries. Hum Reprod 10, 1891–1896 (1995).
Qu, J., Nisolle, M. & Donnez, J. Expression of transforming growth factor-alpha, epidermal growth factor and epidermal growth factor receptor in follicles of human ovarian tissue before and after cryopreservation. Fertil Steril 74, 113–121 (2000).
Reeka, N., Berg, F. D. & Brucker, C. Presence of transforming growth factor alpha and epidermal growth factor in human ovarian tissue and follicular fluid. Hum Reprod 13, 2199–2205 (1998).
Hui, K. K. et al. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp 9, 13–25 (2000).
Zhou, J., Qu, F., Sang, X., Burrows, E. & Nan, R. Auricular acupressure may improve absorption of flavanones in the extracts from Citrus aurantium L. in the human body. J Altern Complement Med 14, 423–425 (2008).
Zhang, C. S. et al. Ear-acupressure for allergic rhinitis: a systematic review. Clin Otolaryngol 35, 6–12 (2010).
Wang, Y. Z., Chen, H. H., Yeh, M. L. & Lin, S. D. Auricular acupressure combined with multimedia instruction or alone for quitting smoking in young adults: A quasi-experimental study. Int J Nurs Stud 47, 1089–1095 (2010).
Mora, B. et al. Auricular acupressure as a treatment for anxiety before extracorporeal shock wave lithotripsy in the elderly. J Urol 178, 160–164 (2007).
Hsieh, C. H., Su, T. J., Fang, Y. W. & Chou, P. H. Effects of auricular acupressure on weight reduction and abdominal obesity in asian young adults: a randomized controlled trial. Am J Chin Med 39, 433–440 (2011).
Kober, A. et al. Auricular acupressure as a treatment for anxiety in prehospital transport settings. Anesthesiology 98, 1328–1332 (2003).
Fassoulaki, A., Paraskeva, A., Patris, K., Pourgiezi, T. & Kostopanagiotou, G. Pressure applied on the extra 1 acupuncture point reduces bispectral index values and stress in volunteers. Anesth Analg 96, 885–890 (2003).
Agarwal, A. et al. Acupressure for prevention of pre-operative anxiety: a prospective, randomised, placebo controlled study. Anaesthesia 60, 978–981 (2005).
Wang, S. M., Gaal, D., Maranets, I., Caldwell-Andrews, A. & Kain, Z. N. Acupressure and preoperative parental anxiety: a pilot study. Anesth Analg 101, 666–669 (2005).
Maa, S. H. et al. Effect of acupuncture or acupressure on quality of life of patients with chronic obstructive asthma: a pilot study. J Altern Complement Med 9, 659–670 (2003).
Bodhise, P. B., Dejoie, M., Brandon, Z., Simpkins, S. & Ballas, S. K. Non-pharmacologic management of sickle cell pain. Hematology 9, 235–237 (2004).
de Klerk, C. et al. Low negative affect prior to treatment is associated with a decreased chance of live birth from a first IVF cycle. Hum Reprod 23, 112–116 (2008).
Boivin, J. & Takefman, J. E. Impact of the in-vitro fertilization process on emotional, physical and relational variables. Hum Reprod 11, 903–907 (1996).
de Klerk, C. et al. The psychological impact of mild ovarian stimulation combined with single embryo transfer compared with conventional IVF. Hum Reprod 21, 721–727 (2006).
Lintsen, A. M., Verhaak, C. M., Eijkemans, M. J., Smeenk, J. M. & Braat, D. D. Anxiety and depression have no influence on the cancellation and pregnancy rates of a first IVF or ICSI treatment. Hum Reprod 24, 1092–1098 (2009).
Eugster, A. & Vingerhoets, A. J. Psychological aspects of in vitro fertilization: a review. Soc Sci Med 48, 575–589 (1999).
Klonoff-Cohen, H. Female and male lifestyle habits and IVF: what is known and unknown. Hum Reprod Update 11, 179–203 (2005).
Campagne, D. M. Should fertilization treatment start with reducing stress? Hum Reprod 21, 1651–1658 (2006).
Garip, H., Abali, O., Goker, K., Gokturk, U. & Garip, Y. Anxiety and extraction of third molars in Turkish patients. Br J Oral Maxillofac Surg 42, 551–554 (2004).
Tenenbaum, G., Furst, D. & Weingarten, G. A statistical reevaluation of the STAI anxiety questionnaire. J Clin Psychol 41, 239–244 (1985).
Boker, A., Brownell, L. & Donen, N. The Amsterdam preoperative anxiety and information scale provides a simple and reliable measure of preoperative anxiety. Can J Anaesth 49, 792–798 (2002).
Nishimori, M. et al. Translation and validation of the Amsterdam preoperative anxiety and information scale (APAIS) for use in Japan. Qual Life Res 11, 361–364 (2002).
Moerman, N., van Dam, F. S., Muller, M. J. & Oosting, H. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg 82, 445–451 (1996).
Templeton, A., Morris, J. K. & Parslow, W. Factors that affect outcome of in-vitro fertilisation treatment. Lancet 348, 1402–1406 (1996).
Lintsen, A. M. et al. Predicting ongoing pregnancy chances after IVF and ICSI: a national prospective study. Hum Reprod 22, 2455–2462 (2007).
Markiewicz, W., Jaroszewski, J. J., Bossowska, A. & Majewski, M. NPY: its occurrence and relevance in the female reproductive system. Folia Histochem Cytobiol 41, 183–192 (2003).
Stener-Victorin, E. et al. Electro-acupuncture as a peroperative analgesic method and its effects on implantation rate and neuropeptide Y concentrations in follicular fluid. Hum Reprod 18, 1454–1460 (2003).
Tsafriri, A., Vale, W. & Hsueh, A. J. Effects of transforming growth factors and inhibin-related proteins on rat preovulatory graafian follicles in vitro. Endocrinology 125, 1857–1862 (1989).
Billig, H., Chun, S. Y., Eisenhauer, K. & Hsueh, A. J. Gonadal cell apoptosis: hormone-regulated cell demise. Hum Reprod Update 2, 103–117 (1996).
Qu, F. et al. Altered aquaporin expression in women with polycystic ovary syndrome: hyperandrogenism in follicular fluid inhibits aquaporin-9 in granulosa cells through the phosphatidylinositol 3-kinase pathway. Hum Reprod 25, 1441–1450 (2010).
Shek, D. T. The Chinese version of the State-Trait Anxiety Inventory: its relationship to different measures of psychological well-being. J Clin Psychol 49, 349–358 (1993).
Cheung, Y. L., Molassiotis, A. & Chang, A. M. The effect of progressive muscle relaxation training on anxiety and quality of life after stoma surgery in colorectal cancer patients. Psychooncology 12, 254–266 (2003).
Spielberger, C., Gorsuch, R. & Lushene, R. Manual for the State-trait Anxiety Inventory. (Consulting Psychologists Press, Palo AltoCA, 1970).
Berth, H., Petrowski, K. & Balck, F. The Amsterdam Preoperative Anxiety and Information Scale (APAIS) - the first trial of a German version. Psychosoc Med 4, Doc01 (2007).
Acknowledgements
This work was supported by Key Projects in the National Science Technology Pillar Program in the Twelve Five – year Plan Period, China (No. 2012BAI32B04). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We thank all the staff of Department of Chinese Medicine and Department of Reproductive Endocrinology, Women's Hospital, School of Medicine, Zhejiang University for their kind help with the present research and Professor Robert Norman (University of Adelaide, Australia) for his suggestions for the paper.
Author information
Authors and Affiliations
Contributions
F.Q., D.Z., L.T.C., L.F.X. and H.F.H. contributed to conception and design of the study. F.Q., D.Z., L.T.C., F.F.W., J.X.P., Y.M.Z., C.M.M., Y.T.H., X.Q.Y., S.J.S., W.J.Z., R.J.Z., J.X. and L.F.X. contributed to carrying out the work. F.Q., D.Z., L.T.C., F.F.W., J.X.P., Y.M.Z., L.F.X. and H.F.H. contributed to analysis and interpretation of data. F.Q., D.Z., L.F.X. and H.F.H. contributed to draft the article and revise it critically for important intellectual content. F.Q. and Y.T.H. prepared Figures 1–3. All authors reviewed the manuscript and approved the version to be published.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images in this article are included in the article's Creative Commons license, unless indicated otherwise in the image credit; if the image is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the image. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Qu, F., Zhang, D., Chen, LT. et al. Auricular Acupressure Reduces Anxiety Levels and Improves Outcomes of in Vitro Fertilization: A Prospective, Randomized and Controlled Study. Sci Rep 4, 5028 (2014). https://doi.org/10.1038/srep05028
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep05028
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.