Abstract
Omega-3 polyunsaturated fatty acids such as eicosapentaenoic acid (EPA) have anti-inflammatory effects. Preterm birth is an important problem in modern obstetrics and one of the main causes is an inflammation. We here showed that abundance of omega-3 fatty acids reduced the incidence of preterm birth induced by LPS with fat-1 mice, capable of converting omega-6 to omega-3 fatty acids. We also indicated that the gene expression of IL-6 and IL-1β in uteruses and the number of cervical infiltrating macrophages were reduced in fat-1 mice. The analyses of lipid metabolomics showed the high level of 18-hydroxyeicosapentaenoate in fat-1 mice, which was derived from EPA and was metabolized to anti-inflammatory product named resolvin E3 (RvE3). We finally showed that the administration of RvE3 to LPS-exposed pregnant wild type mice lowered the incidence of preterm birth. Our data suggest that RvE3 could be a potential new therapeutic for the prevention of preterm birth.
Similar content being viewed by others
Introduction
Preterm birth is a major unresolved problem in modern obstetrics. It is the leading cause of neonatal mortality and contributes to delayed physical and cognitive development in children. Over the last three decades, several investigators have reported a significant association between preterm birth and exaggerated immune cell activity within the womb1,2. Although preterm birth can have a variety of etiologies, inflammation is a common and important cause. Acute chorioamnionitis (CAM), acute inflammation occurring within the chorioamnion, is the principle antecedent of inflammation-associated preterm birth. The majority of cases of CAM are caused by microbes residing in the cervicovaginal region, including those caused by normal microbiota (bacterial vaginosis) and those resulting from colonizion by microbes from other sites3. The associated increases in inflammatory cytokine and local prostaglandin production within the cervix and uterine body stimulate uterine contractility and cervical ripening followed by initiation of premature labor in mice and humans (reviewed in4). Preterm birth may therefore be more closely associated with the magnitude of local inflammation accompanying microbial changes than with infection by a specific eliciting organism. Mechanistically, local pro-inflammatory cytokines primarily induce the production of prostaglandins (PGs) in uterine tissues5. These PGs, especially PGE2 and PGF2α, can promote cervical ripening6 and stimulate uterine contractility7.
The presence of bacterial lipopolysaccharide (LPS) has been associated with preterm birth in rodents8. LPS is a constituent of the plasma membranes of many of the microbes known to be associated with acute chorioamnionitis. Indeed, LPS-induced inflammation leads to the release of many of the pro-inflammatory cytokines and chemokines that induce uterine contractions and injure amnionic membranes9. Therefore, exposure to LPS is commonly used to induce preterm birth in animal models. Previous studies have described several agents that are effective in preventing LPS-induced preterm delivery in mice, including: betamethasone9, cyclooxygenase inhibitors10,11 and progestational agents12,13,14. However, the extension of these agents to clinical use in humans has been hampered by known adverse effects on the pregnant womanand/or her fetus.
Docosahexaenoic acid (DHA, 22:6n-3) and eicosapentaenoic acid (EPA, 20:5n-3) are representative omega-3 polyunsaturated fatty acids (PUFAs) that can block exaggerated inflammatory reactions. In many inflammatory conditions, increased tissue levels of omega-3 PUFAs are considered to be beneficial. However, studies on the effects of omega-3 PUFA supplementation on preterm birth have provided conflicting results. Olsen, et al., demonstrated that women taking fish oil capsules containing EPA and DHA had significantly lower preterm birth rates when compared to those taking placebo15. In contrast, Harper et al. concluded that among women receiving 17α-hydroxyprogesterone caproate for a history of preterm birth, supplementation with omega-3 PUFA soffered no benefit in reducing preterm birth16.
Dietary supplementation is the traditional approach to modifying tissue nutrient composition in animal nutrition studies. However, investigator-sepcific differences in baseline diets among the animals studied may have induced confounders that make comparison among studies difficult. Method descriptions among published studies often make exact replication of control and supplemented diets difficult. Kang, et al., recently engineered a transgenic mouse that carries a fat-1 gene from the roundworm, Caenorhabditis elegans17. This gene encodes an omega-3 fatty acid desaturase that catalyzes the conversion of oemga-6 to omega-3 PUFAs and that is absent in most animals, including mammals. A remarkable difference in tissue omega-6/omega-3 fatty acid ratios is seen in comparisons of wild type and the fat-1 transgenic mice. Further, fat-1 mice have a balanced ratio of omega-6 to omega-3 PUFAs in their tissues and organs that is independent of diet and this allows carefully-controlled studies to be performed in the absence of potential confounding dietary factors18,19. These animals are therefore an exceedingly useful model for investigating the biological properties of endogenous omega-3 PUFAs.
The strong association between omega-3 PUFAs and protection from inflammatory conditions led us to hypothesize that fat-1 mice would have lower preterm birth rates when compared to wild-type controls and that this would be the result of the local anti-inflammatory effects of omega-3 PUFAs. In this study, using the LPS-induced preterm birth mouse model, we investigated inflammation-induced premature pregnancy loss in fat-1 mice and determined the therapeutic potential of the recently-identified EPA-derived anti-inflammatory lipid mediator, RvE3, in preventing preterm birth.
Results
Comparison of the incidence of preterm birth between the fat-1 and wild type mice
The induction of local inflammation in the murine uterus using LPS is the most commonly used method to model preterm birth. In these models, pregnant mice are commonly exposed to LPS via the peritoneal cavity, myometrium, or cervix21. Preterm birth in humans is thought to result from microbes, and/or microbe-induced inflammation, that enter the pregnant woman via the cervicovaginal canal and spread to the uterine cavity. We therefore chose to model this clinical mechanism of preterm birth using transvaginal, intracervical injection of LPS into pregnant mice. Animals were injected once into their cervices with various doses (5–50 μg/head) of LPS. As an injection control, an identical amount (200 μl/head) of saline was injected into the cervices of pregnant mice. Control animals are indicated as the 0 μg/head group in Table 1. Fat-1 and littermate wild type mice were injected with LPS using this protocol and comparisons were made between the resulting fat-1 and wild type preterm birth (PTB) rates (Table 1). No mouse injected with saline alone or with low-dose LPS (5 to 10 μg/head) suffered preterm birth (0/10 in wild type and 0/4 in fat-1 mice), demonstrating that the procedure of transvaginal injection itself did not induce preterm birth. In contrast, transvaginal injection with high-dose LPS (50 μg/head) induced universal preterm birth in both fat-1 and wild type mice. Among mice exposed to 15 to 30 μg/head of LPS, there was a significant difference in the incidence of preterm birth between the fat-1 and wild type mice. Preterm birth occurred frequently in wild type mice exposed to these doses of LPS (14/23 = 60.9%) but significantly less in similarly-exposed fat-1 mice (4/17 = 23.5%) (p = 0.0267). The fat-1 mice injected with 15 μg/head of LPS also displayed a significantly lower incidence of preterm birth when compared with wild type mice injected with the same dose of LPS (p = 0.0461). We therefore chose an exposure dose of 15 μg/head of LPS for transvaginal injection into the cervix for the following experiments.
LPS-induced inflammatory cytokine production in the uteri of fat-1 and wild type mice
The mechanisms underlying LPS-induced preterm birth are reported to include LPS-induced local pro-inflammatory cytokine production, cytokine-mediated elevations in the production of PGE2 and PGF2α and, ultimately, uterine contraction, cervical ripening and preterm delivery5,6,7. All of these cascades occur in the placenta and the uterine myometrium. We hypothesized that the anti-inflammatory effects of omega-3 PUFAs may suppress LPS-induced local inflammation and PGE2 and PGF2α production within the uterus. Pregnant fat-1 and wild type mice were injected transvaginally and intracervically with 15 μg/head of LPS or saline. The myometria of exposed animals were collected six hours after injection. The local production of the pro-inflammatory cytokines, IL-6, IL-1β and TNFα, which are known to be involved in the mechanism of preterm birth22,23,24,25, were quantitated in all animals and compared between groups. As reported previously, the production of IL-6, IL-1β and TNFα was induced in the myometria of all LPS-injected mice. IL-6 and IL-1β mRNA levels in fat-1 mice were significantly lower than those in wild type mice, but no differences in TNF-α mRNA levels were noted (Fig. 1). Fat-1 mice appeared to be at least partially resistant to the induction of pro-inflammatory cytokine production in myometrial tissues upon LPS exposure.
Induction of pro-inflammatory cytokines by LPS intracervical LPS.
LPS (15 microgram) or saline was injected into the cervices of pregnant fat-1 or wild type mice at 15 days of gestation. The uteri of injected mice were harvested six hours after LPS-injection and total RNA was extracted. mRNA levels of IL-6 (A), IL-1β (B) and TNF-α (C) were measured using RT-qPCR. Comparisons were made between wild-type (black) and fat-1 (white) animals. IL-6, IL-1β and TNF-α mRNA levels were normalized to β-actin. Mean mRNA levels and standard deviations were plotted. Asterisks indicate those comparisons (wild type vs. fat-1 mice) with statistical significance (p < 0.05). (n = 4).
Macrophage infiltration into uterine myometria and cervices
Of the leukocytes that may contribute to recruitment and amplification of inflammatory reactions, macrophages are the predominant immune cell subtype residing in the uterus26. Macrophages produce a variety of factors, including prostaglandins and cytokines, that regulate uterine contractile activity25,27. We therefore studied the macrophages infiltrating the myometria and cervices of fat-1 and wild type mice using immunohistochemical detection of F4/80-immunoreactive cells (Fig. 2A). Infiltration of F4/80-immunoreactive macrophages into the myometrium was observed in both wild type and fat-1 mice exposed to LPS (Fig. 2A, left lower two panels). Cervical infiltrating macrophages were also observed in LPS-injected wild type mice (26 ± 5.7 macrophages per 10 microscope fields, n = 3) but were quite infrequent in LPS-injected fat-1 mice (11 ± 2.0 macrophages per 10 microscope fields, n = 3) (right, lower two panels). F4/80 positive macrophages were quantitated and comparisons were made between fat-1 and wild type mice (Fig. 2B). No differences were detected in the number of myometrial infiltrating macrophages in LPS-injected fat-1 and wild type mice. In contrast, the number of cervical infiltrating macrophages in fat-1 mice was significantly lower than that in the wild type mice.
Macrophage infiltration into myometria and cervices of LPS-injected fat-1 and wild type mice.
(A) Immunostaining of the myometria and cervices of LPS- or saline-injected mice for F4/80, a pan macrophage marker. Macrophages were detected using a specific anti-F4/80 mAb (1:500) (lower panels). An isotype-matched control mAb was used as a negative control (lower panels) (200×). Results are representative of two to ten normal tissues for each site. (B) The number of F4/80-positive cells detected in all fields of the myometrium or cervix were counted for wild type (black) or fat-1 (white) mice. Asterisks indicate those comparisons (wild type vs. fat-1 mice) with statistical significance (p < 0.05).
Responsiveness of peritoneal macrophages from fat-1 and wild type mice to LPS
Next, we assessed the responsiveness of peritoneal macrophages to LPS and made comparisons between fat-1 and wild type mice. Peritoneal macrophages were isolated from the peritoneal cells of untreated fat-1 or wild type mice. Collected macrophages were exposed to LPS in the conditioned medium and collected after 0, 1 and 3 hours of exposure. Macrophage IL-6 and IL-1β mRNA levels were measured by RT-qPCR at each time point (Fig. 3). At baseline (0 hours), macrophages derived from fat-1 and from wild type mice had equal IL-6 and IL-1β mRNA levels. Macrophage IL-6 and IL-1β mRNA levels in wild type mice increased in a manner dependent on LPS exposure time. No significant increases in IL-6 and IL-1β mRNA levels were detected in the macrophages derived from fat-1 mice. In fact, IL-1β mRNA levels in the macrophage derived from fat-1 mice after 3 hours of exposure were markedly lower than those in wild type murine macrophages.
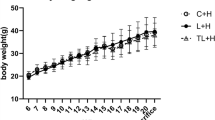
LPS-responsivity in peritoneal macrophages isolated from the fat-1 or wild type mice.
Peritoneal macrophages were isolated from untreated wild-type (black) and fat-1 (white) mice by positive magnetic bead selection. Isolated macrophages were exposed to LPS in the condition medium. Total RNA was extracted from the macrophages 0, 1, 3 hours after LPS exposure. ΙL−6 (A) and IL−1β (B) mRNA levels were measured by RT-qPCR, normalized to β-actin and plotted against time after LPS exposure (0, 1, or 3 hours). Mean mRNA levels and standard deviations are shown. Asterisks indicate those comparisons (wild type vs. fat-1 mice) with statistical significance (p < 0.05). (n = 8).
Mediator lipidomics in myometria from pregnant fat-1 and wild type mice
We next assessed the profiles of PUFA-derived lipid mediators in the myometria of LPS-exposed and control animals using liquid chromatography coupled to tandem mass spectrometry. We hypothesized that the differences in lipid mediator profiles between fat-1 and wild type mice may explain the resistance of fat-1 mice to LPS-induced preterm birth. Myometria were resected from pregnant mice 6 hours after saline or LPS injection and evaluated using LC-MS/MS-based lipidomic analyses (Fig. 4). Most of the arachidonic acid (AA) metabolites in the myometrial tissues were increased in LPS-injected wild type mice when compared with saline-injected mice. Similar AA metabolite increases were not observed in the myometria from fat-1 mice. In particular, PGE2 and PGF2α, which are representative AA metabolites that can induce uterine contractions in pregnant fat-1 mice7 were significantly lower than those in wild type mice (Fig. 4A). In contrast, many of the EPA metabolites in the myometrial tissues were markedly elevated in LPS-injected fat-1 mice but not in wild type mice. Among those, EPA-derived 18-hydroxyeicosapentaenoic acid (HEPE) and 17(18)- epoxy-eicosatetraenoic acid (EpETE) levels in fat-1 mouse myometria were approximately ten fold higher than those in wild type counterparts (Fig. 4B). No significant differences in DHA metabolites were seen between LPS-injected fat-1 and wild type mice. In summary, mediator lipidomics revealed higher levels of the EPA metabolites, 18-HEPE and 17(18)-EpETE and lower levels of the AA metabolites, PGE2 and PGF2α, in fat-1 mice when compared to wild type controls.
Lipid mediator analyses of the myometria from LPS/saline-injected fat-1 and wild type pregnant mice.
Metabolites derived from omega-3 PUFAs were analyzed by LC-MS/MS-based lipidomic analyses. The content of AA-derived (A) and EPA-derived (B) metabolites in the myometria were measured. Myometrial tissues were collected from saline-injected wild-type (dark gray), saline-injected fat-1 (light gray), LPS-injected wild-type (black) and LPS-injected fat-1 (white) mice. Asterisks indicate those comparisons (wild type vs. fat-1 mice) with statistical significance (p < 0.05). LOX; lipoxygenase, COX; cyclooxygenase.
Preventing preterm birth by administration of resolvin E3 (RVE3)
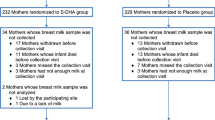
Based on the mediator lipidomics, we hypothesized that 18-HEPE and/or 17(18)-EpETE may play a role in protection against LPS-induced preterm birth. We therefore administer these lipid mediators intravenously in a variety of doses (10–100 microgram) to LPS-injected pregnant wild type mice. Such exposures did not prevent preterm birth (data not shown). These PUFAs, however, need to be converted to their active forms to exert effects at the tissue level. The resolvins are important representative active metabolites of PUFAs. The 18-HEPE-derived metabolites, resolvins E1–E3 (RvE1, -E2 and -E3), are bioactive and can directly exert robust anti-inflammatory activities on inflammatory cells such as neutrophils and macrophages20. Among the resolvins, RvE3 has been recently shown to inhibit neutrophil infiltration in zymosan-induced peritonitis28. To test whether the resoolvin metabolites may be responsible for the protective effects of PUFAs on preterm labor, LPS-injected pregnant wild type mice were exposed twice to 10 ng/head of RvE3 or ethanol (vehicle) intravenously at 0 and 6–12 hours after LPS injection. Preterm birth rates (Table 2) were determined 48 hours after the LPS-injection by calculating the number of delivered/pregnant mice. All mice (9/9) injected with LPS delivered within 48 hours after injection. In contrast, seven of 12 RvE3-exposed mice did not develop preterm birth, giving a preterm birth rate of 41.6% (Table 2). RvE3 administration in the preterm birth model mice resulted in significant reduction of preterm birth (p = 0.007). 36 of 37 fetuses remaining in implantation sites (97.2%) were viable in the pregnant mice given RvE3 in addition to LPS (data not shown).
Discussion
Fat-1 mice allow carefully controlled studies to be performed in the absence of the potential confounding factors of diet. Numerous studies have utilized the fat-1 mouse to examine the role of omega-3 PUFAs and downstream anti-inflammatory mediators in retarding inflammatory disease development. Here we have demonstrated that fat-1 mice are protected against LPS induced-preterm birth by PUFAs through anti-inflammatory pathways. Further, we describe a potential therapeutic use for the EPA-derived bioactive mediator, RvE3, in the prevention of preterm birth.
Prior epidemiological investigations have provided conflicting results on the utility of omega-3 fatty acids in preventing preterm delivery15,29,30,31. This controversy may reflect unintended confounders inherent in study designs that do not control for differences in the dietary habits of the selected patient cohorts. This potential confounder may be particularly limiting for epidemiological investigation or studies on the effects of PUFA supplementation in humans, although comparisons of animal models studying PUFA supplementation may be similarly affected. The dietary characteristics of study animals may differ fairly dramatically among investigative groups. Since Kang et al. first engineered the fat-1 mouse, many insights have been gleaned concerning the anti-inflammatory actions of omega-3 PUFAs using this model17,19. In hepatitis models, use of fat-1 mice has uncovered a reduction in severe inflammatory liver injury that is associated with reduced hepatic gene expression of TNF-α, IL-1β, IFN-γ and IL-632. Similar results have also been reported using fat-1 mice in studies on allergic airway responses33 and pancreatitis34.
In our preterm birth model, production of IL-6 and IL-1β after LPS-injection in fat-1 mice was clearly lower than that in wild type controls. IL-6 and IL-1β are known to be elevated after LPS injection and are hypothesized to be pro-inflammatory markers of preterm birth35,36. In human chorioamnionitis, high grade leukocyte infiltration into placenta tissues is associated with elevated levels of IL-1β, IL-6, IL-8, TNF-α and C-reactive protein in umbilical serum37. IL-6 plays a key role in controlling the progression of events culminating in parturition38. Cervico-vaginal concentrations of IL-6 are reported to be excellent predictors of preterm birth39. Cervical fluid concentrations of IL-1β are elevated in symptomatic women destined to have a spontaneous preterm birth40. The enrichment of omega-3 PUFAs in the myometrium of fat-1 mice suggest that the reduced risk of LPS-induced preterm birth in these animals may be the result of PUFA-mediated inhibition of the local production of pro-inflammatory cytokines, especially IL-1β. It has been shown that omega-3 PUFAs regulate neutrophil and macrophage functions41,42. We therefore hypothesized that the number of neutrophils and macrophages infiltrating in the uterus of the LPS-injected fat-1 mice may differ from that of wild type controls. While the number of neutrophils and the number of macrophages infiltrating the myometrium did not differ between the fat-1 mice and wild type mice six hours after LPS injection (data not shown) the number of macrophages infiltrating the cervix was lower in fat-1 mice. Further, this difference appears to be dependent on time from LPS-injection. At six hours after LPS injection, the macrophages that rapidly infiltrated the cervix may migrate to the other sites such as draining lymph nodes. Alternatively, some macrophages may still be present in the myometrium. Of course, uterine stromal cells also produce pro-inflammatory cytokines and these cells may play a complementary role in the suppression of pro-inflammatory cytokine production observed in fat-1 mice.
To better understand how increased tissue levels of omega-3 PUFAs protect against LPS-induced preterm birth, mediator lipidomics were performed to monitor lipid mediator profiles in the myometrium tissue. AA-derived PGE2 and PGF2α, which are known to induce uterine contractions in pregnancy, were not increased in fat-1 mice even when LPS was injected in the cervix. This effect was accompanied by a reduction in preterm delivery, possibly because of a suppression of uterine contractions. In fat-1 mice, since the production of pro-inflammatory cytokines and the activation of inflammatory cells were suppressed, PGs production via cyclooxygenase should also be suppressed. Interestingly, pro-inflammatory cytokines such as IL-6 are reported to act downstream of leukolysis in the uterus to regulate genes involved in the prostaglandin-mediated uterine activation cascade38. Omega-3 PUFAs also antagonize AA-derived biosynthesis of PGs by competing with omega-6 PUFA for the cyclooxygenase pathway43,44. In fat-1 mice, the suppression of PGE2 and PGF2α seems to be the result of both inhibitory effects of omega-3 PUFAs on the AA-metabolic pathway.
On the other hand, EPA metabolites such as 18-HEPE and 17(18)-EpETE were found to be significantly increased in the myometria from pregnant fat-1 mice exposed to LPS. These EPA metabolites serve as potent inhibitors of inflammation. In particular, 18-HEPE is a common metabolic precursor of EPA-derived E-series resolvins. RvE1 and E2 are biosynthesized by neutrophils via the 5-lipoxygenase pathway and elicit potent anti-inflammatory actions in vivo41,42,45,46,47,48,49. Recently a novel EPA-derived anti-inflammatory mediator, RvE3, was identified. RvE3 is biosythesized via the 12/15-lipoxygenase pathway and has been shown to suppress neutrophil infiltration in zymosan-induced peritonitis28.
Our data on the administration of EPA-derived metabolites suggested that RvE3, rather than 18-HEPE, could suppress LPS-induced uterine inflammation and protect against preterm birth. In our investigations, repeated (twice) administration of RvE3 was effective in mediating a 60% reduction LPS-induced preterm birth in wild type mice. Although further studies will be required to define the precise mechanisms of RvE3's action on preterm birth, our results suggests that this EPA-derived anti-inflammatory mediator has the potential to treat and/or prevent preterm birth in humans.
Methods
Animals
Procedures that involved mice were approved by our Institutional Committee on Animal Use and Care and were conducted in strict accordance with guidelines for the use and care of laboratory research animals promulgated by the National Institutes of Health. Fat-1 breeders were obtained from Dr. Jing Kang at Harvard Medical School. These animals were mated with WT C57BL6 female mice (CLEA Tokyo, Japan) to obtain female fat-1 positive C57BL6 mice (fat-1) and fat-1 negative C57BL6 mice (WT) as identified by genotyping using a KOD FX PCR kit from TOYOBO LIFE SCIENCE (Osaka, Japan). Weight-matched mice were housed in an animal care facility in cages and fed semi-purified AIN-76A diets containing 10% safflower oil. The fat-1 or wild type female mice were mated with C57BL/6J male mice for 48 hours. The day of vaginal plug detection after the first day of mating was designated as day 0 of gestation. Animals were maintained at room temperature in a humidity-controlled room with a 12 h-light/12 h-dark cycle and were given sterilized solid food and water ad libidum during the entire experimental period.
LPS-injection into the cervix of the pregnant mice
Pregnant fat-1 and wild type mice (C57BL/6J) were chosen for LPS-induced preterm birth on day 15 of gestation. LPS derived from Escherichia coli (055;B5, Sigma-Aldrich Japan, Tokyo, Japan) was injected into the murine cervices as follows. A small guide tube was inserted approximately 10–12 mm into the vaginas of the pregnant mice. A long needle attached to a syringe was threaded through the guide, into the vagina and advanced 3 mm into the cervix. Two hundreds microliters of saline containing various doses (5–50 μg/head) of LPS was injected through the needle and into the cervix. After injection, animals were recovered in individual cages and observed every 12 hours for 48 hours following LPS injection to check for signs of morbidity and/or birth. The delivery time of the first fetus was recorded and defined as a preterm (<19 days) or term (19–21 days).
Tissue collection
Pregnant fat-1 and wild type mice that had been exposed to saline or LPS were sacrificed 6 hours after intracervical injection and the uterine myometria and cervices were collected. Total RNA was extracted from the tissues using RNAlater (Life Technologies Japan, Tokyo, Japan) and frozen for group analyses. Peritoneal fluids and cells were collected by washing the peritoneal cavities with 5 ml PBS. Peritoneal cells were isolated by centrifugation, dissolved in MACS buffer (Miltenyi Biotec K.K., Tokyo, Japan) and exposed to anti-mouse CD11b antibody (Miltenyi Biotec K.K.). Peritoneal macrophages were isolated separately using magnetic beads and positive selection.
RT-quantitative PCR (RT-qPCR)
Mice were sacrificed 6 hours after LPS injection and murine uteri were removed immediately. To measure TNF-α, IL-1β and IL-6 mRNA levels in the uterine myometrium, total RNA was extracted from the myometrium using a QIAGEN RNeasy Mini Kit (QIAGEN, Tokyo, Japan). One μg of total RNA and random primers were used for the reverse transcriptase (RT) reaction (TOYOBO, OSAKA, Japan) according to the manufacturer's specifications. Total cDNA reaction samples were used as templates for amplification of each gene fragment using the LightCycler 480 PCR machine (Roche Diagnostics K.K., Tokyo, Japan). Primer pair sets for each gene were purchased from Sigma-Aldrich, Japan. The primer pairs and the universal probes corresponding to the each primer that were used in amplifications were as follows: mouse β-actin, 5′- ATTGAAACATCAGCCAAGACC-3′ and 5′-CCGAATCTCACGGACTAGTGT-3′ probe88; mouse IL-1β, 5′-TTGACGGACCCCAAAAGAT-3′ and 5′- GAAGCTGGATGCTCTCATCTG-3′ probe26; mouse IL-6, 5′- GCTACCAAACTGGATATAATCAGGA-3′ and 5′- CCAGGTAGCTATGGTACTCCAGAA-3′ probe6; mouse TNF-α, 5′-TCTTCTCATTCCTGCTTGTGGA-3′ and 5′-GGTCTGGGCCATAGAACTGA-3′ probe49. The universal probes were chosen from a universal probe library (Roche Diagnostics K.K.). The mRNA levels of TNF-α, IL-1β and IL-6 were normalized to those of β-actin, the internal control.
Immunohistochemistory
For immunohistochemical studies, uterine corpi and cervical tissues were paraffin-embedded, cut into 5-μm sections, mounted on microscope slides, dewaxed and rehydrated. Antigen retrieval involved 5 min of exposure to microwaves in target buffer (DAKO Japan, Tokyo, Japan) and subsequent treatment with 3% H2O2 for 5 min. After a 10 min block at room temperature with protein blocking buffer (DAKO), the tissues were stained with Rat anti-mouse macrophage F4/80 (1-μg/ml; Abcam, Cambridge UK). Horseradish peroxidase-labeled goat anti-rat secondary antibody (Nichirei, Tokyo, Japan) and aminoethylcarbazole (AEC) (Nichirei) substrate were used to develop the reactions.
Culture and characterization of macrophages
Peritoneal cells were collected from fat-1 and wild type mice by washing peritoneal cavities with 5.0 ml of PBS and collecting the resulting peritoneal fluids. Macrophages were isolated from the collected peritoneal cells using a magnetic cell sorting kit (MACS®, Miltenyi Biotec K.K.). Briefly, CD11b+ cells were magnetically labeled with CD11b MicroBeads, the cell suspension was loaded onto a MACS® column and the column was placed into the magnetic field of a MACS separator. The magnetically labeled CD11b+ cells that were retained on the column were then eluted as a positively-selected cell fraction. Macrophages were cultured overnight in RPMI with 10% FBS and exposed to LPS (1 microgram/ml). Total RNA was extracted from macrophages at 0, 1 and 3 hours post-exposure and used for RT-qPCR for IL-6 and IL-1β.
Mediator lipidomics, product isolation and extractions
Whole uterine myometria were obtained from fat-1 and WT mice 6 hours after intracervical LPS or vehicle injection and were immediately frozen in liquid nitrogen. Samples were kept freeze for batched analyses. LC-MS/MS-based mediator lipidomics was performed as described previously20. Briefly, samples were extracted by solid-phase extraction using Sep-Pak C18 cartridges (Waters, Milford, MA, USA) with deuterium-labeled internal standards (PGE2-d4, LTB4-d4, 15-HETE-d8, arachidonic acid-d8). LC-MS/MS-based lipidomic analyses were performed on Acquity UPLC BEH C18 columns (1.0 mm × 150 mm × 1.7 μm) using an Acquity UltraPerformance LC system (Waters Co.) coupled to an electrospray (ESI) triple quadrupole mass spectrometer (QTRAP5500; AB SCIEX). The MS/MS analyses were performed in negative ion mode and the eicosanoids and docosanoids were identified and quantified by multiple reaction monitoring. Calibration curves between 1 and 1000 pg and the LC retention times for each compounds were constructed with synthetic standards.
Intravenous administration of resolvin E3 in wild type preterm birth models
Pregnant wild type mice (C57BL/6J) were subjected to LPS-induced preterm birth on day 15 of gestation as described above. Resolvin E3 (RvE3; 17R, 18R-dihydroxy-eicosapentaenoic acid) was chemically synthesized as described in50 and was provided from Shionogi Co. Ltd. (Osaka, Japan). 10 ng of RvE3 diluted in 100 ml of saline was administered intravenously two times in the LPS-injected mice via the tail vein at 0 and 6–12 hours after LPS injection. Ethanol alone was administered similarly to pregnant wild type mice as a control for RVE3 exposure. These mice were carefully observed every 12 hours over 48 hours following LPS injection to detect preterm birth and any signs of morbidity. The preterm birth rate was calculated as the number of delivered/pregnant mice at 48 hours after LPS-injection. All mice were sacrificed at 48 hours post-exposure and the number of viable fetuses and implantation sites in a pregnant uterus was recorded. Intrauterine fetal deaths were identified by white fetal discolorations, markedly smaller fetal size and lack of blood flow in umbilical cords. Fetal viability rates were determined by the number of viable fetuses/total implantation sites.
Statistical analyses
Pregnancy outcomes were statistically analyzed using the Cochran-Armitage-trend test and Fisher's exact test. Changes in mRNA expression and changes in lipid mediators as detected by LC/MS/MS were analyzed using Mann-Whitney U testing. Differences were considered significant when p was < 0.05.
References
Dudley, D. J., Chen, C. L., Branch, D. W., Hammond, E. & Mitchell, M. D. A murine model of preterm labor: inflammatory mediators regulate the production of prostaglandin E2 and interleukin-6 by murine decidua. Biol Reprod 48, 33–39 (1993).
Fidel Jr, P. L. et al. Systemic and local cytokine profiles in endotoxin-induced preterm parturition in mice. Am J Obstet Gynecol 170, 1467–1475 (1994).
Gibbs, R. S. Chorioamnionitis and bacterial vaginosis. Am J Obstet Gynecol 169, 460–462 (1993).
Romero, R., Mazor, M. & Tartakovsky, B. Systemic administration of interleukin-1 induces preterm parturition in mice. Am J Obstet Gynecol 165, 969–971 (1991).
Pollard, J. K. & Mitchell, M. D. Intrauterine infection and the effects of inflammatory mediators on prostaglandin production by myometrial cells from pregnant women. Am J Obstet Gynecol 174, 682–686(1996).
Kelly, R. W. Inflammatory mediators and cervical ripening. J Reprod Immunol 57, 217–224 (2002).
Baggia, S., Gravett, M. G., Witkin, S. S., Haluska, G. J. & Novy, M. J. Interleukin-1 beta intra-amniotic infusion induces tumor necrosis factor-alpha, prostaglandin production and preterm contractions in pregnant rhesus monkeys. J Soc Gynecol Investig 3, 121–126 (1996).
Silver, R. M. et al. Bacterial lipopolysaccharide-mediated fetal death. Production of a newly recognized form of inducible cyclooxygenase (COX-2) in murine decidua in response to lipopolysaccharide. J Clin Invest 95, 725–731 (1995).
Casey, M. L., Cox, S. M., Beutler, B., Milewich, L. & MacDonald, P. C. Cachectin/tumor necrosis factor-alpha formation in human decidua. Potential role of cytokines in infection-induced preterm labor. J Clin Invest 83, 430–436 (1989).
Lee, P. R. et al. Therapeutic effect of cyclo-oxygenase inhibitors with different isoform selectivity in lipopolysaccharide-induced preterm birth in mice. Am J Obstet Gynecol 189, 261–266 (2003).
Sakai, M. et al. Evaluation of the tocolytic effect of a selective cyclooxygenase-2 inhibitor in a mouse model of lipopolysaccharide-induced preterm delivery. Mol Hum Reprod 7, 595–602 (2001).
Elovitz, M. & Wang, Z. Medroxyprogesterone acetate, but not progesterone, protects against inflammation-induced parturition and intrauterine fetal demise. Am J Obstet Gynecol 190, 693–701 (2004).
Elovitz, M. A. & Gonzalez, J. Medroxyprogesterone acetate modulates the immune response in the uterus, cervix and placenta in a mouse model of preterm birth. J Matern Fetal Neonatal Med 21, 223–230 (2008).
Elovitz, M. A. & Mrinalini, C. The use of progestational agents for preterm birth: lessons from a mouse model. Am J Obstet Gynecol 195, 1004–1010 (2006).
Olsen, S. F. et al. Randomised clinical trials of fish oil supplementation in high risk pregnancies. Fish Oil Trials In Pregnancy (FOTIP) Team. BJOG 107, 382–395 (2000).
Harper, M. et al. Omega-3 fatty acid supplementation to prevent recurrent preterm birth: a randomized controlled trial. Obstet Gynecol 115, 234–242 (2010).
Kang, J. X., Wang, J., Wu, L. & Kang, Z. B. Transgenic mice: fat-1 mice convert n-6 to n-3 fatty acids. Nature 427, 504 (2004).
Kang, J. X. From fat to fat-1: a tale of omega-3 fatty acids. J Membr Biol 206, 165–172 (2005).
Kang, J. X. Fat-1 transgenic mice: a new model for omega-3 research. Prostaglandins Leukot Essent Fatty Acids 77, 263–267 (2007).
Arita, M. Mediator lipidomics in acute inflammation and resolution. J Biochem 152, 313–319 (2012).
Elovitz, M. A. & Mrinalini, C. Animal models of preterm birth. Trends Endocrinol Metab 15, 479–487 (2004).
Figueroa, R. et al. Evaluation of amniotic fluid cytokines in preterm labor and intact membranes. J Matern Fetal Neonatal Med 18, 241–247 (2005).
Hirsch, E., Blanchard, R. & Mehta, S. P. Differential fetal and maternal contributions to the cytokine milieu in a murine model of infection-induced preterm birth. Am J Obstet Gynecol 180, 429–434 (1999).
Steinborn, A. et al. Cytokine release from placental endothelial cells, a process associated with preterm labour in the absence of intrauterine infection. Cytokine 11, 66–73 (1999).
Steinborn, A., von Gall, C., Hildenbrand, R., Stutte, H. J. & Kaufmann, M. Identification of placental cytokine-producing cells in term and preterm labor. Obstet Gynecol 91, 329–335 (1998).
Hunt, J. S., Manning, L. S., Mitchell, D., Selanders, J. R. & Wood, G. W. Localization and characterization of macrophages in murine uterus. J Leukoc Biol 38, 255–265 (1985).
Norwitz, E. R., Starkey, P. M., Lopez, B. A. & Turnbull, A. C. Identification by flow cytometry of the prostaglandin-producing cell populations of term human decidua. J Endocrinol 131, 327–334 (1991).
Isobe, Y. et al. Identification and structure determination of novel anti-inflammatory mediator resolvin E3, 17,18-dihydroxyeicosapentaenoic acid. J Biol Chem 287, 10525–10534 (2012).
Oken, E., Kleinman, K. P., Olsen, S. F., Rich-Edwards, J. W. & Gillman, M. W. Associations of seafood and elongated n-3 fatty acid intake with fetal growth and length of gestation: results from a US pregnancy cohort. Am J Epidemiol 160, 774–783 (2004).
Olsen, S. F. Is supplementation with marine omega-3 fatty acids during pregnancy a useful tool in the prevention of preterm birth? Clin Obstet Gynecol 47, 768–774 (2004).
Olsen, S. F. & Secher, N. J. Low consumption of seafood in early pregnancy as a risk factor for preterm delivery: prospective cohort study. BMJ 324, 447 (2002).
Schmocker, C. et al. Omega-3 fatty acids alleviate chemically induced acute hepatitis by suppression of cytokines. Hepatology 45, 864–869 (2007).
Bilal, S. et al. Fat-1 transgenic mice with elevated omega-3 fatty acids are protected from allergic airway responses. Biochim Biophys Acta 1812, 1164–1169 (2011).
Weylandt, K. H. et al. Reduction of inflammation and chronic tissue damage by omega-3 fatty acids in fat-1 transgenic mice with pancreatitis. Biochim Biophys Acta 1782, 634–641(2008).
Christiaens, I. et al. Inflammatory processes in preterm and term parturition. J Reprod Immunol 79, 50–57 (2008).
Flidrova, E. & Krejsek, J. Innate immunity in pathogenesis of intraamniotic inflammation in pregnancies complicated by preterm premature rupture of membranes. Ceska Gynekol 76, 46–50 (2011).
Dollner, H., Vatten, L., Halgunset, J., Rahimipoor, S. & Austgulen, R. Histologic chorioamnionitis and umbilical serum levels of pro-inflammatory cytokines and cytokine inhibitors. BJOG 109, 534–539 (2002).
Robertson, S. A. et al. Interleukin-6 is an essential determinant of on-time parturition in the mouse. Endocrinology 151, 3996–4006 (2010).
Torbe, A. & Czajka, R. Proinflammatory cytokines and other indications of inflammation in cervico-vaginal secretions and preterm delivery. Int J Gynaecol Obstet 87, 125–130 (2004).
Edwards, R. K., Ferguson, R. J. & Duff, P. The interleukin-1 beta + 3953 single nucleotide polymorphism: cervical protein concentration and preterm delivery risk. Am J Reprod Immunol 55, 259–264 (2006).
Arita, M. et al. Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci U S A 102, 7671–7676 (2005).
El Kebir, D., Gjorstrup, P. & Filep, J. G. Resolvin E1 promotes phagocytosis-induced neutrophil apoptosis and accelerates resolution of pulmonary inflammation. Proc Natl Acad Sci U S A 109, 14983–14988 (2012).
Calder, P. C. N-3 polyunsaturated fatty acids and inflammation: from molecular biology to the clinic. Lipids 38, 343–352 (2003).
Bagga, D., Wang, L., Farias, E. R., Glaspy, J. A. & Reddy, S. T. Differential effects of prostaglandin derived from omega-6 and omega-3 polyunsaturated fatty acids on COX-2 expression and IL-6 secretion. Proc Natl Acad Sci U S A 100, 1751–1756 (2003).
Arita, M. et al. Stereochemical assignment, antiinflammatory properties and receptor for the omega-3 lipid mediator resolvin E1. J Exp Med 201, 713–722 (2005).
Arita, M., Clish, C. B. & Serhan, C. N. The contributions of aspirin and microbial oxygenase to the biosynthesis of anti-inflammatory resolvins: novel oxygenase products from omega-3 polyunsaturated fatty acids. Biochem Biophys Res Commun 338, 149–157 (2005).
Arita, M. et al. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J Immunol 178, 3912–3917 (2007).
Oh, S. F. et al. Resolvin E2 formation and impact in inflammation resolution. J Immunol 188, 4527–4534 (2012).
Oh, S. F., Pillai, P. S., Recchiuti, A., Yang, R. & Serhan, C. N. Pro-resolving actions and stereoselective biosynthesis of 18S E-series resolvins in human leukocytes and murine inflammation. J Clin Invest 121, 569–581 (2011).
Isobe, Y. et al. Stereochemical assignment and anti-inflammatory properties of the omega-3 lipid mediator resolvin E3. J Biochem 153, 355–360 (2013).
Acknowledgements
We gratefully thank Dr. Danny J. Schust for careful editing of the manuscript, Dr. Terufumi Yokoyama for excellent comments and advice on experiments using murine models and Ms. Michiko Kamio for technical assistance on LC-MS/MS analyses. This work was supported by a grant-in-aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (K.K., T. F.), by a grant-in-aid from the Tokyo IGAKUKAI (K.K.), by grant-in-aid from Japan Science and Technology agency Precursory Research for Embryonic Science and Technology (PRESTO) (M.A.) and by grant in aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (M.A.)
Author information
Authors and Affiliations
Contributions
A.Y., Y.I., R.I., H.F. and K.M. performed experiments. K.K., A.Y. and M.A. wrote the manuscript. K.K., A.Y., K.T., A.T., T.N., K.N., K.O., O.W-H., T.A., T.Y., Y.T., S.K., T.F., Y.O., H.A. and M.A. contributed in data interpretation. K.K., T.F., S.K. J.X.K. and M.A. contributed to experimental design.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareALike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Yamashita, A., Kawana, K., Tomio, K. et al. Increased tissue levels of omega-3 polyunsaturated fatty acids prevents pathological preterm birth. Sci Rep 3, 3113 (2013). https://doi.org/10.1038/srep03113
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep03113
This article is cited by
-
Prophylactic administration of human amniotic fluid stem cells suppresses inflammation-induced preterm birth via macrophage polarization
Molecular and Cellular Biochemistry (2023)
-
ASK1 promotes uterine inflammation leading to pathological preterm birth
Scientific Reports (2020)
-
Low Omega-3 intake is associated with high rates of depression and preterm birth on the country level
Scientific Reports (2020)
-
Alteration of erythrocyte membrane polyunsaturated fatty acids in preterm newborns with retinopathy of prematurity
Scientific Reports (2019)
-
Double Transgenesis of Humanized fat1 and fat2 Genes Promotes Omega-3 Polyunsaturated Fatty Acids Synthesis in a Zebrafish Model
Marine Biotechnology (2014)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.