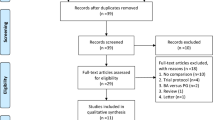
Abstract
Pancreaticojejunostomy is the key procedure of pancreaticoduodenectomy. Our study introduced a new pancreaticojejunal (PJ) anastomosis named “papillary-like main pancreatic duct invaginated” pancreaticojejunostomy. Nighty-two patients underwent pancreaticojejunostomy with either conventional duct-to-mucosa pancreaticojejunostomy or the new “papillary-like main pancreatic duct invaginated” techniques were analyzed retrospectively from January 2010 to September 2012. The incidence of pancreatic fistula was 15.7% (8/51) for the “papillary-like main pancreatic duct invaginated” group and 19.5% (8/41) for the duct-to-mucosa fashion respectively. It is noteworthy that the rate of grade B/C postoperative pancreatic fistula (POPF) in the “papillary-like main pancreatic duct invaginated” group was significantly lower than that of the duct-to-mucosa group (P = 0.039). There were no differences in the incidence of postoperative morbidity and mortality such as postoperative hemorrhage, delayed gastric emptying or remnant pancreatitis. The “papillary-like main pancreatic duct invaginated” pancreaticojejunostomy could provide a feasible option to pancreatic surgeons for patients with normal soft pancreas.
Similar content being viewed by others
Introduction
Presently, pancreaticoduodenectomy is widely accepted as the standard surgical procedure for patients with resectable tumor in the pancreatic head and periampullary region1. Although a great challenge for a surgeon, pancreaticojejunostomy will directly contribute to the success of the pancreaticoduodenectomy regardless of procedural success. Postoperative pancreatic fistula (POPF) is a major complication for pancreaticojejunostomy and most often results in poor surgical outcomes2,3,4,5. Duct-to-mucosa pancreaticojejunostomy is commonly used in the modern pancreatic surgery. The duct-to-mucosa method is not affected by the size of pancreatic stump or jejunal lumen and does not need too much free pancreatic remnant, making it a widely used anastomotic technique, with the postoperative pancreatic leakage rate ranging from 4.2% to 24%6,7,8,9. However, for cases with small main pancreatic duct and soft pancreatic texture, its advantages appear to be limited and the incidence of pancreatic leakage is still relatively high10,11,12. Recently, we have developed a “papillary-like main pancreatic duct invaginated” pancreaticojejunostomy after pancreaticoduodenectomy in our clinical practice and have obtained some promising results.
Results
Operation-related clinical data in two PJ anastomosis
All 92 patients had normal soft pancreas textures, among which 41 cases were performed with conventional duct-to-mucosa pancreaticojejunostomy and the other 51 cases underwent a “papillary-like main pancreatic duct invaginated” method. As described in Table 1, the two groups were compared in age, sex, BMI and pathological types. No statistical differences were found between the two groups. Both the operative time and anastomotic time were slightly longer in the “papillary-like main pancreatic duct invaginated” group than in the duct-to-mucosa group, but without statistical difference. For the other operation-related data, including intraoperative hemorrhage, diameter of pancreatic duct and hospital stay time, differences between the two groups were not statistically significant (Table 2).
“Papillary-like main pancreatic duct invaginated” pancreaticojejunostomy decreased the rate of Grade B/C POPF
POPF occurred in eight patients (8/41) in the duct-to-mucosa group, compared with eight patients (8/51) in the “papillary-like main pancreatic duct invaginated” group. In the duct-to-mucosa group, three patients were in grade A, four patients were in grade B and one patient was in grade C. In the “papillary-like main pancreatic duct invaginated” group, seven patients were in grade A and one was in grade B (Table 3). The POPF grade B/C rate in the “papillary-like main pancreatic duct invaginated” group was significantly reduced than that in the duct-to-mucosa group (P = 0.039, Table 3). All the patients in Grade A POPF were just treated with delayed removal of the drainage tubes. The five cases in Grade B POPF were treated with enteral nutrition, antibiotics and repositioning the drainage tubes. One patient in Grade C attempted to receive a CT-guided percutaneous drainage after developing a local peripancreatic abscess, but failed. Ten days after surgery, the patient underwent a second operation to relieve the abdominal abscess.
Other postoperative complications and outcomes
Postoperative complications are listed in Table 3. In both groups, there were no perioperative deaths and no patients developed postoperative hemorrhage or biliary leakage. Delayed gastric emptying was found in two patients with the duct-to-mucosa method and two patients with the “papillary-like main pancreatic duct invaginated” method (Table 3), which were treated by reinsertion of the nasogastric tube, enteral nutrition support and the prokinetic drugs such as Domperidone. One postoperative remnant pancreatitis case was found in both the “papillary-like main pancreatic duct invaginated” group and the duct-to-mucosa group, as diagnosed by postoperative serum amylase and the abdominal CT scan. They were treated by somatostatin 0.1 mg in subcutaneous injection every 8 hours. Both cases were recovered. Other complications such as postpancreatectomy hemorrhage, liver abscess and biliary leakage did not occur in both groups.
Postoperative changes of pancreatic function
In Table 4, we compared some postoperative blood parameters relating to pancreatic function on POD 1 and 3, such as WBC, blood amylase and BG. No statistical difference was found between the two groups.
Discussion
Pancreaticoduodenectomy is a standard surgical approach for resectable pancreatic tumors and periampullary tumors. It is considered a safe procedure resulting from the continuous improvement in surgical techniques over the years13,14,15,16. Although postoperative mortality has obviously decreased, pancreatic fistula is still a major challenge in pancreatic surgery and remains the major cause of postoperative morbidity and mortality after PD, ranging from 5% to 30%11,12,17.
Currently, several techniques and modifications have been proposed for pancreatic anastomosis over the past few decades, including the conventional duct-to-mucosa method7,18,19, pancreaticogastrostomy20,21, Peng's binding method22, dunking method23 and end-to-side invaginated method24. Among them, the conventional duct-to-mucosa method, which is not affected by the size of pancreatic remnant as well as the jejunal lumen and doesn't need too much free pancreatic remnant for the anastomosis, is still the most popular anastomosis nowadays. Unfortunately, in the cases of normal soft pancreas with a small main pancreatic duct, it is difficult to perform the duct-to-mucosa approach. It always leads to a self-incision for the duct, along with an inadequate drainage for the pancreatic juice from the main pancreatic duct after the anastomosis. This results in a postoperative pancreatic fistula.
To overcome these shortcomings and reduce the incidence of postoperative pancreatic fistula, some surgeons attempted to position a stent in the main pancreatic duct across the PJ anastomosis to assure a fluent drainage of pancreatic juice from the main pancreatic duct to the jejunum22,25,26, this stent can also be a landmark for the orifice of the pancreatic duct, preventing accidental suturing of both anterior and posterior walls. However, other surgeons27 have indicated that the internal pancreatic stent does not decrease POPF in soft pancreatic texture. Markar, et al28 demonstrated that intra-operative blood loss, operation length and hospitalized duration were significantly increased in association with pancreatic stent placement according to the results of six clinical trials. In this study, we molded a “papillary-like main pancreatic duct” like “a physiological stent” and invaginate it into the jejunal lumen. This modified novel technique was used to connect the main pancreatic duct with the jejunal lumen, similar to the duct-to-mucosa method.
Sugiyama and colleagues examined four pancreatic specimens with soft pancreatic texture and small main pancreatic duct and found that there were about 5–7 tiny collateral pancreatic ducts on the cutting surface of the pancreatic remnant29. We thought that the secretion from the cut surface might be the risk factor for POPF, so we closed the pancreatic remnant to reduce the risk of the fistula as well as postoperative hemorrhage.
According to different definitions, the incidence of postoperative pancreatic fistula is highly variable11,12,17. In this study, POPF was defined according to the International Study Group of Pancreatic Fistula (ISGPF): drainage of any measurable volume of fluid with the amylase content greater than three times the normal serum value on or after POD 312. In the 51 cases using this “papillary-like main pancreatic duct invaginated” pancreaticojejunostomy, eight patients developed a postoperative pancreatic fistula. Although the overall POPF was not significantly reduced, the Grade B/C POPF rate of the “papillary-like main pancreatic duct invaginated” group was lower than that in the duct-to-mucosa group, which suggested that this novel “papillary-like main pancreatic duct invaginated” pancreaticojejunal anastomosis could reduce the incidence of the severe POPF. We speculate that the improvement was attributed to the following reasons: 1. Closure of the pancreatic stump lowered the opportunity of fistula from the collateral pancreatic duct. 2. We used a protruding “papillary-like main pancreatic duct” to take the place of the internal stent, avoiding the iatrogenic injury to the main pancreatic duct and following pancreatitis and anastomotic leakage. When the “papillary-like main pancreatic duct” had been invaginated into the jejunum, the pancreatic juice drained directly into the jejunal lumen. 3. We did not place the suture through the main pancreatic duct during the procedure, in order to avoid the leakage from the inaccurate sutures.
But compare to the conventional duct-to-mucosa method, there were some arising problems to be solved for the new anastomosis in our clinic practice. First, we had to isolate a small part of the free pancreatic tissues for the moulding of “papillary-like main pancreatic duct” in the new anastomosis, but it was quite easy to perform in normal soft pancreas cases. Second, some pancreatic parenchyma around the “papillary-like main pancreatic duct” should be removed, which might lead to a light increase of hemorrhage and a loss and dysfunction of the pancreas. Moreover, this was only a retrospective study with a small sample size, so the result only represented for a small group of patients, which needs to be further validated by large-scale clinical trial.
In summary, this “papillary-like main pancreatic duct invaginated” PJ anastomosis may reduce the grade B/C POPF after pancreaticoduodenectomy without prolonged operation time and is relatively simple and easy-to-learn. With a further randomized trial, it may provide a better option to pancreatic surgeons for cases with soft pancreatic texture and a small main pancreatic duct.
Methods
Patients
This study was approved by the Human Research Ethics Committee at Shanghai Cancer Center, Fudan University. Informed consent was obtained from each patient according to the committee's regulation. In this study, we summarized the related data of 51 patients treated with the new method from January 2010 to September 2012 in Shanghai Cancer Center. We retrospectively compared these cases with other 41 cases that underwent the duct-to-mucosa method during the same period. All of the pancreatic remnants were of the normal soft pancreas variety. The normal soft pancreas had a main pancreatic duct diameter of <3.5 mm in the head, normal exocrine and endocrine functions and an absence of pancreatitis or fibrosis in postoperative pathologic specimens. We use a ruler to measure the diameter of the main pancreatic duct on the cutting surface of the remnant pancreas after the incisal margin has been proved negative by the intraoperative fast frozen pathology. The two groups were not consecutive and one experienced surgeon performed all the cases. Drainage amylase, blood amylase, white blood cells (WBC) and blood glucose (BG) were measured on postoperative day (POD) 1 and 3. Computed tomography (CT) scans were performed for suspicion of intraabdominal abscess, fluid collection, or fistula after surgery. Complications were graded according to Clavien's classification10 and the POPF was diagnosed according to the International Study Group of Pancreatic Fistula (ISGPF) guidelines. The definition of pancreatic fistula is a drain output of any measurable volume of fluid on or after POD 3 with the amylase content greater than 3 times the serum amylase activity. Three different grades of POPF (grades A, B, C) are defined by ISGPF according to the clinical impact on the patient's hospital course. Grade A, also called “transient fistula”, has no clinical impact. A CT scan typically shows no peripancreatic collections and the use of total parenteral nutrition, antibiotics, or somatostatin analogues are not needed. Grade B is always associated with abdominal pain, fever, and/or leukocytosis and antibiotics are usually required; somatostatin analogues may also be used. A CT scan may show peripancreatic collections requiring repositioning of the drains. Often the patient is fasting and supported with partial or total parenteral or enteral nutrition that usually leads to a delayed discharge. Grade C is severe and always shows a major change in clinical management or a deviation from the normal clinical pathway. A CT scan usually shows worrisome peripancreatic collections that require percutaneous drainage or re-exploration. There are often associated complications such as sepsis and organ dysfunction and the possibility of postoperative mortality rises12.
Duct-to-Mucosa pancreaticojejunal anastomosis
The excision of pancreas was performed slightly left to the neck of pancreas according to the position of the tumor. Prolene sutures were used to repair the obvious bleeding points on the cut surface of the pancreatic stump and electrocoagulation for hemostasis was used to confirm the masked bleeding points. After locating the main pancreatic duct, the surgeon performed a suturing of the back layer of the duct-to-mucosa anastomosis between the pancreatic parenchyma and seromuscular jejunum by interrupted 4-0 absorbable sutures (ETHICON, VCP771D). A small enterotomy was then performed on the jejunum wall in order to connect the main pancreatic duct. The suture of the main pancreatic duct to the enterotomy site was secured by an interrupted 4-0 absorbable suture with 2–3 stitches for both anterior and posterior walls of the duct. This completes the anterior layer of the anastomosis9,13.
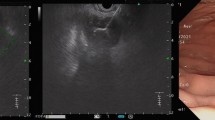
“Papillary-like main pancreatic duct invaginated” pancreaticojejunostomy
Management of the pancreatic stump: The operation was performed when the intraoperative frozen section confirmed there was no residual tumor at the resection margin of the pancreatic stump. A 1–1.2 cm pancreatic stump was carefully isolated (Figure 1A) and the pancreatic stump was molded into a “fish mouth-like” shape, with the “papillary-like main pancreatic duct” protruding out of the stump 6–8 mm. Briefly, an annular incision of 6–8 mm depth was made carefully about 2–3 mm around the main pancreatic duct and then the pancreatic parenchyma around the main pancreatic duct was removed to leave the “papillary-like main pancreatic duct” protruding out of the stump. Before closure of the remnant, any bleeding points and visible branches of pancreatic duct on the cut surface should be repaired preciously with 4-0 absorbable sutures or coagulated by electrocautery. The pancreatic stump was then closed using interrupted inverting sutures around the “papillary-like main pancreatic duct” (Figure 1B).
Management of the pancreatic stump.
(A) A 1–1.2 cm pancreatic stump was isolated. (B) The pancreatic stump was molded into a “fish mouth-like” shape, with the pancreatic duct protruding out of the stump. The pancreatic stump was closed with interrupted inverting sutures around the “papillary-like main pancreatic duct”.
Pancreaticojejunal (PJ) Anastomosis: PJ anastomosis was performed in a retrocolic manner. On both sides of the main pancreatic duct, the back wall of pancreatic stump and the seromuscular layer of jejunum were sewn together using 4-0 absorbable sutures by interrupted sutures (Figure 2A). A small full-thickness enterotomy was penetrated on the jejunal wall for connection to the “papillary-like main pancreatic duct” (Figure 2B). The “papillary-like main pancreatic duct” was then invaginated into the jejunal hole by firmly placing 4-6 sutures from the “periductal” parenchyma to the whole-layer jejunal hole (Figure 2B, Figure 3A). It is worthy to note that stitches should be placed into the tissues just around the “papillary-like main pancreatic duct” rather than into the pancreatic duct itself. Interrupted 4-0 absorbable sutures were placed between the front wall of pancreatic stump and the seromuscular jejunum to complete the anastomosis (Figure 3B).
Treatment of the posterior wall of “papillary-like main pancreatic duct invaginated” pancreaticojejunostomy.
(A) The back wall of pancreatic stump and the seromuscular layer of jejunum were sewn together using 4-0 absorbable sutures by interrupted sutures. (B) A small full-thickness enterotomy was penetrated on the jejunal wall for connecting to the “papillary-like main pancreatic duct”.
Treatment of the anterior wall of “papillary-like main pancreatic duct invaginated” pancreaticojejunostomy.
(A) The “papillary-like main pancreatic duct” is invaginated into the jejunum hole firmly by placing 4–6 sutures from the “periductal” parenchyma to the whole-layer jejunum hole. (B) The interrupted sutures between the front wall of pancreatic stump and the seromuscular jejunum were performed by 4-0 absorbable sutures to complete the anastomosis.
Hepaticojejunostomy anastomosis and drain management: In order to guarantee that there was no tension for the PJ anastomosis in the case of jejunal peristalsis, an end-to-side single layer interrupted hepaticojejunostomy was performed using the jejunal loop at about 8–10 cm from the PJ anastomosis. One drain was placed anterior to the PJ anastomosis and another posterior to the anastomosis (Figure 4). The nasogastric tube and nasal feeding tube were placed during the surgery.
Statistical analysis
Comparisons between the two groups were measured using the Fisher exact test and the averages were compared using the Student's t-test. Differences were considered significant at P<0.05. Numerical data was expressed as Mean ± SD (SD = standard deviation).
References
Schmidt, C. M. et al. Pancreaticoduodenectomy: a 20-year experience in 516 patients. Arch. Surg. 139, 718–727 (2004).
Adams, D. B. The pancreatic anastomosis: the danger of a leak, which anastomotic technique is better? J. Gastrointest. Surg. 13, 1182–1183 (2009).
Hidalgo, M. Pancreatic cancer. N. Engl. J. Med. 362, 1605–1617 (2010).
Aranha, G. V., Aaron, J. M., Shoup, M. & Pickleman, J. Current management of pancreatic fistula after pancreaticoduodenectomy. Surgery 140, 561–569 (2006).
Liu, C. et al. Pancreatic stump-closed pancreaticojejunostomy can be performed safely in normal soft pancreas cases. J. Surg. Res 172, e11–17 (2012).
Tsuji, M. et al. Management of continuous anastomosis of pancreatic duct and jejunal mucosa after pancreaticoduodenectomy: historical study of 300 patients. Surgery 123, 617–621 (1998).
Matsumoto, Y. et al. Successful pancreatojejunal anastomosis for pancreatoduodenectomy. Surg. Gynecol. Obstet. 175, 555–562 (1992).
Howard, J. M. Pancreatojejunostomy: leakage is a preventable complication of the Whipple resection. J. Am. Coll. Surg. 184, 454–457 (1997).
Berger, A. C. et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. J. Am. Coll. Surg. 208, 738–747 (2009).
Yang, Y. M. et al. Risk factors of pancreatic leakage after pancreaticoduodenectomy. World. J. Gastroenterol. 11, 2456–2461 (2005).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240, 205–213 (2004).
Bassi, C. et al. International Study Group on Pancreatic Fistula Definition: Postoperative pancreatic fistula: An international study group (ISGPF) definition. Surgery 138, 8–13 (2005).
Kennedy, E. P. & Yeo, C. J. Dunking pancreaticojejunostomy versus duct-to-mucosa anastomosis. J. Hepatobiliary. Pancreat. Sci. 18, 769–774 (2011).
Yamaguchi, K. et al. Early and late complications of pylorus-preserving pancreatoduodenectomy in Japan 1998. J. Hepatobiliary. Pancreat. Surg. 6, 303–311 (1999).
Shi, S. et al. Combinational therapy: New hope for pancreatic cancer? Cancer. Letters. 317, 127–135 (2012).
Luo, G. et al. Stroma and pancreatic ductal adenocarcinoma: An interaction loop. Biochim. Biophys. Acta. 1826, 170–178 (2012).
Yeo, C. J. et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: Pathology, complications and outcomes. Ann. Surg. 226, 248–260 (1997).
Okamoto, K. et al. Duct-to-mucosa pancreaticojejunostomy for small main pancreatic duct by the parachute technique after pancreatoduodenectomy. Hepatogastroenterology 58, 1025–1028 (2011).
Suzuki, S. et al. Pancreaticojejunostomy of duct to mucosa anastomosis can be performed more safely without than with a stenting tube. Am. J. Surg. 198, 51–54 (2009).
Oida, T. et al. Pancreaticogastrostomy in patients with considerably dilated pancreatic ducts. Hepatogastroenterology 59, 2330–2332 (2012).
Bassi, C. et al. Reconstruction by pancreaticojejunostomy versus pancreaticogastrostomy following pancreatectomy: results of a comparative study. Ann. Surg. 242, 767–771 (2005).
Peng, S. et al. Binding pancreaticojejunostomy is a new technique to minimize leakage. Am. J. Surg. 183, 283–285 (2002).
You, D. et al. Comparison of different pancreatic anastomosis techniques using the definitions of the International Study Group of Pancreatic Surgery: a single surgeon's experience. Pancreas 38, 896–902 (2009).
Bassi, C. et al. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery 134, 766–771 (2003).
Roder, J. D. et al. Stented versus nonstented pancreaticojejunostomy after pancreatoduodenectomy: a prospective study. Ann. Surg. 229, 41–48 (1999).
Poon, R. T. et al. External drainage of pancreatic duct with a stent to reduce leakage rate of pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann. Surg. 246, 425–435 (2007).
Winter, J. M. et al. Does pancreatic duct stenting decrease the rate of pancreatic fistula following pancreaticoduodenectomy? Results of a prospective randomized trial. J. Gastrointest. Surg. 10, 1280–1290 (2006).
Markar, S. R. et al. The impact of pancreatic duct drainage following pancreaticojejunostomy on clinical outcome. J. Gastrointest. Surgery. 16, 1610–1617 (2012).
Sugiyama, M. et al. Pancreatic transection using ultrasonic dissector in pancreaticoduodenectomy. Am. J. Surg. 182, 257–259 (2001).
Acknowledgements
This study was partially supported by Shanghai Municipal Commission of Economy and Informatization (2010CH-016) and Joint Project for Emerging Frontier Technology of Shanghai Hospitals of Municipal Level (SHDC12010120).
Author information
Authors and Affiliations
Contributions
X.Y. and M.L. conceived the idea. B.Z., J.X. and C.L. designed of the study and wrote the manuscript. J.L., L.L. and Y.X. were involved in the collection and assembly of data. C.W., G.L. and Q.N. were involved in data analysis. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Zhang, B., Xu, J., Liu, C. et al. Application of “Papillary-Like Main Pancreatic Duct Invaginated” Pancreaticojejunostomy for Normal Soft Pancreas Cases. Sci Rep 3, 2068 (2013). https://doi.org/10.1038/srep02068
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep02068
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.