Abstract
Human β defensin DEFB103 acts as both a stimulant and an attenuator of chemokine and cytokine responses: a dichotomy that is not entirely understood. Our predicted results using an in silico simulation model of dendritic cells and our observed results in human myeloid dendritic cells, show that DEFB103 significantly (p < 0.05) enhanced 6 responses, attenuated 7 responses and both enhanced/attenuated the CXCL1 and TNF responses to Porphyromonas gingivalis hemagglutinin B (HagB). In murine JAWSII dendritic cells, DEFB103 significantly attenuated, yet rarely enhanced, the Cxcl2, Il6 and Csf3 responses to HagB; and in C57/BL6 mice, DEFB103 significantly enhanced, yet rarely attenuated, the Cxcl1, Csf1 and Csf3 responses. Thus, DEFB103 influences pro-inflammatory activities with the concentration of DEFB103 and order of timing of DEFB103 exposure to dendritic cells, with respect to microbial antigen exposure to cells, being paramount in orchestrating the onset, magnitude and composition of the chemokine and cytokine response.
Similar content being viewed by others
Introduction
Human β defensin 3 (DEFB103) is a small, yet potent antimicrobial host defense peptide with diverse innate immune activities1. It is prominent throughout the oronasal cavity and is present in nasal mucus, saliva and gingival crevicular fluid at concentrations as high as 6.2 μg/ml2. Monocytes or dendritic cells treated with DEFB103 alone or with a microbial antigen have both pro-inflammatory and anti-inflammatory activities: a dichotomy that is not entirely well understood, but important given the recent recognition of the role of DEFB103 in the production of cytokines and inflammation associated with mucosal infections3,4, aerodigestive cancers like squamous cell carcinoma of the head and neck5, auto-immune and auto-inflammatory diseases6 and severe trauma7. Furthermore, DEFB103 is overexpressed in individuals with intense inflammation associated with squamous cell carcinoma of the head and neck5 where it may function as a chemo-attractant to recruit macrophages8.
The role of DEFB103 in regulating chemokine and pro-inflammatory cytokine responses to specific pro-inflammatory antigenic exposure is largely unknown, particularly the effects of DEFB103 concentration, like overexpression in squamous cell carcinomas and order of timing of DEFB103 with respect to antigen exposure to dendritic cells. Compelling evidence clearly suggests that DEFB103 and other α- and β-defensins have pro-inflammatory activities; and chemokines and pro-inflammatory cytokines are upregulated and produced in stimulated cells8,9,10,11. Equally compelling evidence suggests that DEFB103 and other α- and β-defensins have opposite and potent anti-inflammatory activities12,13. Human neutrophil peptide α-defensin DEFA1 blocks the release of IL1B, but not TNF, from lipopolysaccharide-activated human monocytes14; DEFA1-3 inhibit the secretion of multiple pro-inflammatory cytokines from macrophages15; and DEFB103 attenuates the IL6, IL10, CSF2 and TNF responses of human myeloid dendritic cells to Porphyromonas gingivalis hemagglutinin B (HagB)16.
Influencing events in ‘defensin controlled inflammation’ likely involve extracellular binding of defensins to microbial antigens17,18,19; defensin-altered binding of antigens to cell surfaces20,21; or defensin-altered signaling12,22.
Here we report the conditions in which DEFB103 bidirectionally regulates the chemokine and cytokine responses of human myeloid dendritic cells to a pro-inflammatory stimulus and demonstrate that the concentration of DEFB103 and order of timing of DEFB103 exposure to cells, with respect to microbial antigen exposure to cells, are paramount in orchestrating the onset, magnitude and composition of the dendritic cell chemokine and cytokine response.
Results
The predicted influence of DEFB103 on a HagB-induced response in an in silico simulation model of human dendritic cells
HagB stimulates dendritic cells in a TLR4-dependent manner and MyD88 and TRIF are required for their optimal activation23 and DEFB103 affects the activity of pro-inflammatory pathways associated with MyD88 and TRIF12,13 (Figure 1c). Therefore to determine the parameters of DEFB103 influencing the HagB-induced responses seen at 16 hours, we utilized a simulation model of dendritic cells that provides a dynamic and transparent view of the dendritic cell physiology in silico. This simulation technology has been used to predict biomarker responses, phenotype responses and chemokine and cytokine responses in various disease based cell systems including epithelial-based tumor cells, keratinocytes, monocytes and other immune cells24,25,26,27,28,29. Such an approach has enabled design and validation of therapy against rheumatoid arthritis, neuroprotective targets with implications for Parkinson's therapy28 and anti-tumor combination targeted therapy against specific tumor baselines. The predictions of the dendritic cell model for HagB and E. coli 55:B5 endotoxin were tested and prospectively validated by our observed responses with the same triggers. The blinded predicted results and observed responses for HagB and E. coli 55:B5 endotoxin had a high correlation of greater than 80% (Supplemental Table 1). At a 10:1 molar ratio of DEFB103 to HagB, like that used in our prior studies16, the dendritic cell model predicted a DEFB103-induced attenuation in expression levels of CCL3, CCL4, CSF2, IL6, IL10 and TNF in HagB-exposed human myeloid dendritic cells compared to that of HagB stimulation alone on the referenced baseline (Figure 1a). This predicted response correlated with the observed attenuated response of chemokines and pro-inflammatory cytokines in our previous work16; the attenuated HagB-induced responses after co-DEFB103 treatment in human myeloid dendritic cells (Figure 3, response seen in group 3, Table 1); and our observed results (p < 0.05) for Cxcl2, Il6 and Csf3 with similar trends for Ccl3 and Tnf in murine JAWS II dendritic cells (Figure 4, Table 2).
The predictive in silico dendritic cell model generated response to Porphyromonas gingivalis hemagglutinin B (HagB).
The percentage change mentioned in the figures is with respect to the control reference baseline. (a) The predicted effect of lower over-expression of DEFB103 along with P. gingivalis HagB stimulation on CCL3, CCL4, CSF2, IL6, IL10 and TNF. Compared to HagB stimulation alone on the referenced baseline, the levels of CCL3, CCL4, CSF2, IL6, IL10 and TNF were significantly reduced. (b) The predicted effect of very high over-expression of DEFB103 along with HagB stimulation on CCL3, CCL4, CSF2, IL6, IL10 and TNF. Compared to HagB stimulation alone on the referenced baseline, the levels of CCL3, CCL4, CSF2, IL6, IL10 and TNF had significantly increased. (c) The network schematic of the HagB and DEFB103 regulations in the virtual dendritic cell platform. HagB provides activating signals to CD14 and activin receptors. On binding to CD14 and activin receptors, it stimulates the release of pro-inflammatory cytokines like CCL3, CCL4, CSF2, IL6, IL10 and TNF via activation of MYD88/TRAF6 and SHC1/ERK pathways respectively. Both activin and CD14 signals converge at the activation of MAPKs, AKT and PKC to activate the transcription factors NFKB, AP1, SP1, CREB1, NFAT and IRFs, which transcribes different cytokines. DEFB103 exerts both an activating and inhibitory effect on dendritic cells. It binds to G-protein coupled receptors CCR2B and CCR6, which stimulate Gi and Gq respectively and activate LYN/SYK/PLC/PKC-DAG pathway converging at the activation of AKT, NFKB and NFAT. DEFB103 also negatively regulates the pro-inflammatory signal by inhibiting CD14, CD40 and IFNG receptors. The dotted red lines in the figure indicate inhibitory links and dotted fluorescent green lines indicate activation links. Downstream effects (activation links) of each transcription factor are shown by unique colored solid lines.
Porphyromonas gingivalis hemagglutinin B (HagB) is a potent pro-inflammatory stimulus.
Bar graphs show the IL6, IL10, CSF2, TNF, CCL3 and CCL4 responses of human myeloid dendritic cells at 16 hours after exposure to inocula containing 2.0, 0.2, 0.02 and 0.002 µM HagB (Groups 1–4, respectively), 2.0, 0.2, 0.02 and 0.002 µM heated HagB (ΔHagB, Groups 5–8, respectively), 847.0, 79.0, 8.1 and 0.9 ng/ml detected endotoxin (Groups 9–12, respectively) and 0.01 M PBS, pH 7.2 (Group 13). HagB, but not ΔHagB, induced the production of chemokines and cytokines comparable to that of E. coli 55:B5 endotoxin (*, p < 0.05). Statistical analysis was performed as described in the Methods on all log10-transformed chemokine and cytokine concentrations and the significant differences among all groups (p < 0.05) are listed in Supplemental Table 2.
The influence of DEFB103 on the 0.02 μM Porphyromonas gingivalis hemagglutinin B (HagB)-induced chemokine and cytokine responses of human myeloid dendritic cells.
(a) The TNF response of human myeloid dendritic cells exposed for 0, 2, 4, 8 and 16 hours to HagB (Group 1); DEFB103 and then exposed to HagB one hour later (pre-DEFB103 treatment, Group 2); a mixture of DEFB103 and HagB (co-DEFB103 treatment, Group 3); DEFB103 and HagB at the same time but not mixed together like that in Group 3 (Group 4); HagB and then exposed to DEFB103 one hour later (post-DEFB103 treatment, Group 5); DEFB103 (Group 6); or 0.01 M PBS, pH 7.2 (Group 7). (b) The TNF response of human myeloid dendritic cells exposed for 2 hours to Groups 1–7 and (c) the TNF response of human myeloid dendritic cells exposed for 16 hours to Groups 1–7. (d) At 2 hours, 18 of 42 HagB-induced chemokine and cytokine responses were not enhanced or attenuated after pre-, co-, or post-DEFB103 treatment (p > 0.05) and 6 of 42 HagB-induced responses were enhanced after pre- or post-DEFB103 treatment (p < 0.05). At 16 hours, 13 of 42 HagB-induced chemokine and cytokine responses were not enhanced or attenuated after pre-, co-, or post-DEFB103 treatment (p > 0.05); 6 of 42 responses were enhanced after either pre- or post- DEFB103 treatment (p < 0.05); 7 of 42 responses were attenuated after co-DEFB103 treatment (p < 0.05); and 2 of 42 responses were both enhanced and attenuated after pre-, co-, or post-DEFB103 treatment (p < 0.05). Statistical analysis was performed as described in the Methods on all log10-transformed chemokine and cytokine concentrations and the significant differences among all groups (p < 0.05) are listed in Supplemental Table 3.
The influence of DEFB103 on the 0.02 μM Porphyromonas gingivalis hemagglutinin B (HagB)-induced chemokine and cytokine responses of murine JAWSII dendritic cells.
(a) The Cxcl2 response of JAWSII dendritic cells exposed for 0, 2, 4, 8 and 16 hours to HagB (Group 1); DEFB103 and then exposed to HagB one hour later (pre-DEFB103 treatment, Group 2); a mixture of DEFB103 and HagB (co-DEFB103 treatment, Group 3); DEFB103 and HagB at the same time but not mixed together like that in Group 3 (Group 4); HagB and then exposed to DEFB103 one hour later (post-DEFB103 treatment, Group 5); DEFB103 (Group 6); or 0.01 M PBS, pH 7.2 (Group 7). (b) The Cxcl2 response of JAWSII dendritic cells exposed for 2 hours to Groups 1–7 and (c) the Cxcl2 response of JAWSII dendritic cells exposed for 16 hours to Groups 1–7. At 16 hours, 0.2 μM DEFB103 significantly attenuated the 0.02 μM HagB-induced Cxcl2 response (*, p < 0.05, Group 3). Statistical analysis was performed as described in the Methods on all log10-transformed chemokine and cytokine concentrations and the significant differences among all groups (p < 0.05) are listed in Supplemental Table 4.
The model also prospectively predicted that an increase in DEFB103 could account in part for the enhanced DEFB103-induced chemokine and cytokine responses of HagB-exposed human myeloid dendritic cells observed in Figure 3 (e.g., the responses seen in Groups 2, 4 and 5). For example, with a 10,000:1 molar ratio of DEFB103 to HagB, the dendritic cell model predicted that DEFB103 would enhance the expression of CCL3, CCL4, CSF2, IL6, IL10 and TNF in HagB-exposed human myeloid dendritic cells compared to that of HagB stimulation alone on the referenced baseline (Figure 1b). This phenomenon was observed (Table 1) and results using 20 µM DEFB103 resulted in high concentrations of CCL3, CCL4 and TNF.
The observed influence of DEFB103 on a HagB-induced human myeloid dendritic cell response
HagB is a potent pro-inflammatory stimulus. HagB induced the production of chemokines and cytokines comparable to that of E. coli 55:B5 endotoxin (Supplemental Table 2, Figure 2). To establish that HagB was a comprehensive pro-inflammatory stimulus for human myeloid dendritic cells, LGM-3 containing 2.0, 0.2, 0.02 and 0.002 µM HagB; 2.0, 0.2, 0.02 and 0.002 µM heated HagB (ΔHagB); 847.0, 79.0, 8.1 and 0.9 ng/ml endotoxin; and 0.01 M PBS, pH 7.2 were added to adhered human myeloid dendritic cells and incubated for 0, 2, 4, 8 and 16 hours. At 16 hours post treatment, 0.02, 0.2 and 2.0 μM HagB induced a robust chemokine and pro-inflammatory cytokine response in 21 chemokines and cytokines (e.g., >100 pg/ml), a moderate response in 16 chemokines and cytokines (e.g., 11–100 pg/ml); and a negligible response in 13 chemokines and cytokines (e.g., <10 pg/ml).
HagB-induced responses were similar in magnitude to that induced by 847.0, 79.0, 8.1 and 0.9 ng/ml E. coli 55:B5 endotoxin and not due to any trace amounts of endotoxin that may have carried over from the Ni-NTA purification process and accompanied HagB in the inocula. This was confirmed by heating and denaturing HagB: ΔHagB induced significantly lower chemokine and cytokine responses (p < 0.05; Supplemental Table 2, Figure 2). Furthermore, there were no significant differences (p > 0.05) in the endotoxin content in cell culture inocula and these results are listed at the top of Supplemental Tables 2–4. Therefore, 0.02 µM HagB was selected as the stimulatory dose: the dendritic cell response to 0.02 µM HagB was both high enough and low enough to show chemokine and cytokine fluctuations and the response to 0.02 µM ΔHagB was negligible and significantly lower (Supplemental Table 2).
Influence of DEFB103 on the HagB-induced response. We observed that DEFB103 induced a unique bidirectional modulation of the chemokine and pro-inflammatory cytokine response of HagB-exposed human myeloid dendritic cells. By 2 hours, the DEFB103-induced responses of 42 chemokine and cytokines of HagB-exposed human myeloid dendritic cells start to separate into 3 distinct groups: 18 chemokine and cytokine responses that are low or negligible; 18 responses that are neither enhanced nor attenuated after pre-, co-, or post-DEFB103 treatment (p > 0.05); and 6 responses that are enhanced after pre- or post-DEFB103 treatment (p < 0.05, Supplemental Table 3, Figure 3). By 16 hours, the DEFB103-induced chemokine and cytokine responses of HagB-exposed cells separate into 5 distinct groups: 14 chemokine and cytokine responses that are low or negligible; 13 elevated responses that are neither enhanced nor attenuated after pre-, co-, or post-DEFB103 treatment (p > 0.05); 6 responses that are enhanced after pre- or post-DEFB103 treatment (p < 0.05); 7 responses that are attenuated after co-DEFB103 treatment (p < 0.05) and 2 responses that are bidirectionally pliable and are both enhanced and attenuated after pre-, co-, or post-DEFB103 treatment (p < 0.05) (Supplemental Table 3, Figure 3). This latter group includes CXCL1 and TNF.
In another series of experiments, we assessed the effect of DEFB103 and HagB concentration on the temporal exposure of DEFB103 to HagB-exposed human myeloid dendritic cells. DEFB103 (0.2, 2.0, or 20.0 µM) was given to human myeloid dendritic cells pre- (1 hour before), co-, or post- (1 hour after) HagB treatment (0.02 or 0.2 µM). DEFB103 had a concentration dependent ability to both attenuate and enhance the chemokine and pro-inflammatory cytokine response (Table 1). Timing was still important. CCL3, CCL4 and TNF responses to 0.02 µM HagB were both enhanced and attenuated when 0.2 and 2.0 µM DEFB103 was given pre-/post- or co-HagB exposure, respectively.
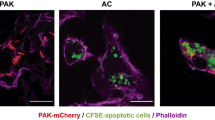
DEFB103 attenuated the HagB-induced chemokine and cytokine responses of murine JAWS II dendritic cells
In JAWS II dendritic cells, only one aspect of the bidirectional mechanism was seen. DEFB103 significantly attenuated, yet rarely enhanced, the chemokine and pro-inflammatory cytokine response to HagB (Supplemental Table 4, Figure 4, Table 2). Seven of ten chemokines and pro-inflammatory cytokines were detected 16 hours after treatment to 0.02 μM HagB (Table 2). DEFB103 did not enhance any chemokine or pro-inflammatory cytokine responses to HagB. DEFB103 attenuated the HagB-induced response only after JAWS II dendritic cells were exposed to a mixture of DEFB103 and HagB that was prepared by adding DEFB103 to HagB in tissue culture medium and incubating the mixture at 37°C for 30 minutes (e.g., Group 3, Figure 4c). Cxcl2, Il6 and Csf3 responses were attenuated (e.g., Group 1 vs. Group 3, p < 0.05, Table 2); Ccl3 and Tnf responses showed similar attenuated response trends but were not significantly different. Ccl2 and Ccl4 responses were not attenuated.
DEFB103 enhanced the HagB-induced chemokine and cytokine responses of mice
In mice, the opposite aspect of the bidirectional mechanisms was seen. DEFB103 significantly enhanced, yet rarely attenuated, the chemokine and pro-inflammatory cytokine response to intranasal administration of HagB (Supplemental Table 5, Figure 5, Table 2). HagB alone induces Ccl2, Ccl3, Ccl4, Cxcl1, Cxcl2, Il6, Tnf, Csf1, Csf2 and Csf3 responses in the nasal wash fluid supernatant (Table 2), all important in the initiation and maintenance of murine oronasal inflammatory responses30. Prior administration of DEFB103 intranasally enhances (p < 0.05) the HagB-induced Cxcl1, Csf3 and Csf1 responses with Ccl3, Ccl4, Cxcl2, Il6 and Tnf showing similar, but not quite significant trends. Furthermore, the DEFB103 enhanced response occurs early (e.g., 2 hours in Cxcl1), becomes robust and remains sustained throughout the 16 hour response (Figure 5a). At 2 hours post intranasal inoculation, DEFB103 enhances (p < 0.05) the HagB-induced Cxcl1 response with Ccl2, Ccl3, Il6, Tnf and Csf3 responses again showing similar trends (Figure 5a). Negligible chemokine and cytokine responses were induced by administration of 0.01 M PBS or DEFB103 alone.
The effect of DEFB103 on the Porphyromonas gingivalis hemagglutinin B (HagB)-induced chemokine and cytokine responses of mice.
(a) The Cxcl1 response of mice exposed for 0, 2, 4, 8 and 16 hours to HagB (Group 1); DEFB103 and then exposed to HagB one hour later (pre-DEFB103 treatment, Group 2); a mixture of DEFB103 and HagB (co-DEFB103 treatment, Group 3); HagB and then exposed to DEFB103 one hour later (post-DEFB103 treatment, Group 4); DEFB103 (Group 5); or 0.01 M PBS, pH 7.2 (Group 6). (b) The Cxcl1 response of mice exposed for 2 hours to Groups 1–6 and (c) the Cxcl1 response of mice exposed for 16 hours to Groups 1–6. At 16 hours, 0.2 μM DEFB103 significantly enhanced the 0.02 μM HagB-induced Cxcl2 response (*, p < 0.05, Group 2). Statistical analysis was performed on the mean and standard error (Std Err, n = 9) of log10 concentrations of Cxcl1 as described in the Methods on all log10-transformed chemokine and cytokine concentrations and the significant differences among all groups (p<0.05) are listed in Supplemental Table 5.
Discussion
In this study, we sought to identify the conditions in which DEFB103 regulates the chemokine and cytokine responses of human myeloid dendritic cells. DEFB103 and other α- and β-defensins are known in some experimental designs to enhance the production of chemokines and pro-inflammatory cytokines in stimulated cells8,9,10,11, yet in other experimental designs to attenuate the production of chemokines and pro-inflammatory cytokines in stimulated cells12,13. In this study, we developed a simulation model of human dendritic cells to assess both the effects of HagB and DEFB103 on a comprehensive panel of chemokines, cytokines and other cell products. We used the dendritic cell model to predict the effect of DEFB103 over-expression on cytokine and chemokine expressions in HagB-exposed dendritic cells. In the system, HagB is shown to activate dendritic cells through TLR and activin receptor signaling and DEFB103 is shown to inhibit the activation of dendritic cells by TLR signaling, CD40LG signaling and IFNG signaling. Along with the inhibitory role of DEFB103, the activation of CCR2B and CCR6 receptors by DEFB103 is also modeled (Figure 1c). The model also prospectively predicted that an increase in DEFB103 could account, in part for the enhanced DEFB103-induced chemokine and cytokine responses of HagB-exposed human myeloid dendritic cells observed in Figure 3 (e.g., responses seen in groups 2, 4 and 5). For example, with a 10,000:1 molar ratio of DEFB103 to HagB, the dendritic cell model predicted that DEFB103 would enhance the expression of CCL3, CCL4, CSF2, IL6, IL10 and TNF in HagB-exposed human myeloid dendritic cells compared to that of HagB stimulation alone on the referenced baseline (Figure 1b). This phenomenon was observed (Table 1) and results using 20 µM DEFB103 resulted in high concentrations of CCL3, CCL4 and TNF.
We validated the model by comparing the predicted and observed responses using HagB and lipopolysaccharide as pro-inflammatory stimuli (Supplemental Table 1). We then used the model to predict the effects of HagB and DEFB103 on the response. Our observed results suggest that DEFB103 can act as both a stimulant and an attenuator of chemokine and pro-inflammatory cytokine responses depending upon the timing of TLR stimulation. Both the concentration of DEFB103 and the temporal treatment of DEFB103 to cells, with respect to microbial antigen treatment of cells, were important in the magnitude of the overall chemokine and cytokine response. Some interesting trends are evident. First, when DEFB103 was mixed with HagB for 30 minutes at 37°C before exposure, co-DEFB103 treatment generally attenuated the HagB-induced chemokine and cytokine responses. When DEFB103 was given one hour before or one hour after exposure, pre-DEFB103 and post-DEFB103 treatment generally enhanced the HagB-induced chemokine and cytokine responses. Second, high 20 µM concentrations of DEFB103 generally enhanced responses of many chemokines and cytokines that typically were attenuated at lower 0.2 or 2.0 µM concentrations of DEFB103. Third, this phenomenon was observed only with select groups of chemokines and cytokines. The responses of many others were not affected. For example, out of 42 chemokines and cytokines assessed in human myeloid dendritic cells (Supplemental Table 3, Figure 3), 0.2 µM DEFB103 only significantly (p < 0.05) enhanced 6 responses, attenuated 7 responses and both attenuated and enhanced the CXCL1 and TNF responses of human myeloid dendritic cells to 0.02 µM HagB. Fourth, the results in human myeloid dendritic cells, murine JAWSII dendritic cells and mice had some subtle differences. For example, the bidirectional mechanism was seen in human myeloid dendritic cells but only partially in murine JAWSII dendritic cells and mice. Out of seven chemokines and cytokines assessed in murine JAWSII dendritic cells (Supplemental Table 4, Figure 4), 0.2 µM DEFB103 attenuated the Cxcl2, Il6 and Csf3 responses to 0.02 µM HagB and out of ten chemokines and cytokines assessed in mice (Supplemental Table 5, Figure 5), 0.2 µM DEFB103 significantly enhanced the Cxcl1, Csf3 and Csf1 responses to intranasal administration of 0.2 µM HagB. Thus, DEFB103 significantly alters the onset, magnitude and composition of the dendritic cell response to a pro-inflammatory stimulus, like HagB, depending upon the concentration and circumstances of exposure.
The exact mechanism for DEFB103 altered chemokine and cytokine responses is not known. The binding of DEFB103 to HagB17,21 may play a partial role by altering the binding of HagB to TLR on the dendritic cell surface partially retarding the activation of underlying MAPK pathways leading to the attenuated HagB-induced response. However, when administered separately and in differing order to dendritic cells, DEFB103 and HagB may synergistically activate similar pathways and exaggerate a HagB-induced response stronger than that seen by HagB alone. Finally, it is also possible that the ability of DEFB103 to rapidly enter cells21 also plays a part. The trend in responses seen after temporal exposure of human and murine JAWS II dendritic cells to DEFB103 and HagB are similar to the responses seen after temporal exposure of JAWS II dendritic cells to surfactant protein-A (SP-A)-derived peptides and E. coli lipopolysaccharide31. In the study by Awasthi, et al, JAWS II dendritic cells were treated with SP-A-derived peptides for 1 hour before the addition of lipopolysaccharide and 4 hours after incubation with lipopolysaccharide. Three of seven SP-A-derived peptides increased and two of seven peptides decreased lipopolysaccharide-induced Tnf responses in JAWS II dendritic cells. In our study, JAWS II dendritic cells were treated with DEFB013 for 1 hour before the addition of HagB and 1 hour after incubation with HagB. DEFB103 only decreased HagB-induced Cxcl2, Il6 and Csf3 responses in JAWS II dendritic cells. It is not yet known whether the 3-hour difference in post exposure times is important. Overall, the concentration of TLR ligands, the composition of LTR ligands and the temporal exposure cells to innate immune molecules vs. the pro-inflammatory stimulus all seem to be important in influencing the magnitude and composition of the chemokine and cytokine response.
The ability of DEFB103 to bidirectionally modulate chemokine and cytokine responses of dendritic cells is novel and would clearly be important to early events of mucosal inflammation, early innate immune responses and adaptive immune responses. DEFB103 and other defensins in mucosal secretions would be readily available to quickly bind to exogenous antigens before they are perceived by antigen presenting cells. Such a mechanism would attenuate the resulting chemokine and pro-inflammatory cytokine response and thus maintain normal tissue homeostasis with minimal mucosal inflammation. This likely occurs in an oral cavity ‘bathed’ by a plethora of antimicrobial substances32,33 with nearly minimal inflammation given the considerable antigenic burden endured in this limited area on a daily basis. Alternately, in situations where DEFB103 and other defensins are induced and produced in increased concentrations, they may ‘prime’ cells that later over produce chemokines and pro-inflammatory cytokines when exposed to exogenous antigens. Such a situation may be the overexpression of DEFB103 in individuals with squamous cell carcinoma5, the presence of a diversity of bacterial groups within oral squamous cell carcinoma tissue34 and the intense inflammation that is often seen.
The innovative approach of using a predictive model alongside different experimental systems allowed us to tease out the phenomenon of bidirectional regulation at the cellular network level. Our future work will look closely at the signaling pathways (Figure 1c) involved in the process to help understand the role of controlling factors and pathway intermediates in the development and magnitude of chemokine and cytokine responses to pro-inflammatory stimuli.
Methods
In silico simulation model of dendritic cells
A simulation model of dendritic cells was developed and used to assess the parameters of and the intermediate pathways and transcription factors possibly involved in, the DEFB103-induced chemokine and cytokine responses of HagB-exposed human myeloid dendritic cells (Figure 1). The physiologically aligned and extensively validated model is a functional proteomics representation of the receptors and signaling pathways representing dendritic cell physiology and supports triggers from both adaptive and innate immune responses. This platform is similar to that used to predict biomarker and phenotype responses including chemokines and cytokines in other cellular disease systems including cancer, autoimmune disorder such as Rheumatoid Arthritis, Parkinson's Disease and other infectious diseases24,25,26,27,28,29. The dendritic cell model was assembled from published data on signaling pathways, intermediates, transcription factors, enzyme kinetics and gene regulations comprising 2,560 biological species with over 9,300 cross-talk interactions and includes: a) factors related to antigen uptake and presentation including FC receptors, Toll-like receptors (TLRs) etc.; b) factors associated with the adhesion of dendritic cells including integrin receptors ITGAL, ICAM1, CD44 and CD58 and CD209; c) factors associated with the migration of dendritic cells, which includes different chemokine receptors; d) signaling pathways related to maturation and activation of dendritic cells, which include tumor necrosis factor family members comprising TNF, LTA, TNFSF14, TNFSF18, CD40LG, interleukins IL12, IL4, IL1B, IL2, IFNA1 and IFNG, growth factors EGF and CSF2 and others (CLEC7A, INHBE, etc.); e) inhibitory pathways VEGFA, IL10, IL6 and TGFA; f) kinases and transcription factors associated with dendritic cell physiology; and g) apoptotic pathways FAS and TNFSF10. The time-dependent changes in the fluxes of the constituent signaling pathways were modeled utilizing modified ordinary differential equations (ODEs) and mass action kinetics. A proprietary technology platform and simulation engine created by Cellworks Group Inc., was used to simulate the dendritic cell model with ODEs solved by the Radau method. The model was prospectively and retrospectively validated against an extensive set of in vitro and in vivo studies and here against HagB and lipopolysaccharide (Supplemental Table 1). Simulation protocol: in the dendritic cell model, HagB was introduced with a concentration of 0.001 uM along with a 10-fold over-expression of DEFB103 and the effect on downstream markers were analyzed compared to HagB stimulation alone on the referenced baseline. A second study was carried out in the control system wherein HagB was introduced with a concentration of 0.001 uM along with very high (10000 fold) over-expression of DEFB103 and the effect on downstream markers were analyzed compared to HagB stimulation alone on the referenced baseline. The key biomarkers analyzed include CCL3, CCL4, CSF2, IL6, IL10 and TNF. There is no statistical variation in the results of the kinetic based, deterministic, simulation model. However, there can be variations with varying the simulation protocols – i.e., strength of triggers etc.
Solutions and inocula
Weight per volume endotoxin content was determined on all solutions, media and on all cell culture inocula (QCL-1000, Lonza Walkersville, Inc., Walkersville, MD) in triplicate using E. coli 055:B5 endotoxin as the standard (Lonza Walkersville, Inc., Walkersville, MD). Endotoxin content of the dendritic cell inocula was determined and is listed at the top of Supplemental Tables 2–4.
0.01 M sodium phosphate with 0.140 M NaCl, pH 7.2 was used as a diluent and as a control solution. It was prepared using pyrogen-free water (Lonza Walkersville, Inc., Walkersville, MD), filtered (0.22 μm filter, Millipore, Billerica, MA) and contained 0.004 ± 0.0007 (Std Err, n = 3 tests) ng/ml endotoxin.
DEFB103 used in this study is a synthetic 45 amino acid residue peptide derived from DEFB103A and DEFB103B (PeproTech, Inc. Rocky Hill, NJ). It has a +11 net cationic charge and a monoisotopic mass of 5,157.7 Da. Reconstituted DEFB103 solutions contained 0.00007 ng endotoxin/µg (n = 3 tests).
E. coli 055:B5 endotoxin (Lonza Walkersville, Inc., Walkersville, MD) was suspended in pyrogen-free water and heated at 56°C for 30 minutes to facilitate complete solubilization. Weight per volume solutions of 1000.0, 100.0, 10.0 and 1.0 ng/ml endotoxin contained 847.0, 79.0, 8.1 and 0.9 ng/ml detected endotoxin (QCL-1000, Lonza Walkersville, Inc., Walkersville, MD).
HagB is a 49 kDa pro-inflammatory protein and was prepared by cloning hagb of P. gingivalis (1.4 kb) into the vector pQE31 (QIAGEN Inc., Valencia, CA); expressing HagB in E. coli M15(pREP4)pQE-31-TX1; and isolating HagB from E. coli lysate supernatants with a Ni-NTA spin column (HisPur, Pierce Biotechnology, Rockford, IL)16,32. Bound HagB was eluted with 0.25 M imidazole in 0.01 M Tris, 0.5 M NaCl, 20% glycerol, pH 7.4 and dialyzed against 0.01 M Tris with 0.5 M NaCl, pH 7.4 at 4°C. The purity of HagB was verified by SDS-PAGE and contained 0.014 ng endotoxin/µg HagB. An aliquot of HagB (called ΔHagB) was inactivated by heating at 121°C for 15 minutes.
Cell Lines and media
Human myeloid dendritic cells
Human myeloid dendritic cells were prepared as previously described16 from human peripheral blood mononuclear cells (Lonza Walkersville, Inc., Walkersville, MD). Commercially derived human myeloid dendritic cells were also used (Lonza Walkersville, Inc., Walkersville, MD). Cells were grown in Lymphocyte Growth Media-3 (LGM-3, Lonza Walkersville, Inc., Walkersville, MD), a serum-free, complete medium containing 0.053±0.001 (Std Err, n = 3 tests) ng/ml endotoxin; counted to determine the total and viable cell concentrations, the latter using immunofluorescence in the presence of 25 ng/ml propidium iodide to detect dead cells; and adjusted to contain 1 × 105 viable cells per ml. Cells were plated at a density of 2.6 × 104 viable cells per cm2 and allowed to attach for 2 hours. Media and non-adherent cells were removed by aspiration just before adding inocula.
Murine JAWSII dendritic cells
Murine JAWSII dendritic cells (CRL-11904, ATCC, Manassas, VA) were also used, similar to that of other temporal studies of this kind31. These cells are an immortalized cell line derived from the bone marrow of C57BL/6 mice and have been used to show temporal enhancement and attenuation of synthetic surfactant protein-A-derived peptide on lipopolysaccharide-induced release of Tnf31. They were grown in Minimum Essential Medium Alpha Medium with 1% L-glutamine, 20% fetal bovine serum, 5 ng/ml Csf2 and 50 μg/ml gentamicin sulfate. This media contained 0.040 ± 0.0003 (Std Err, n = 3 tests) ng/ml endotoxin. Cells were counted to determine the total and viable cell concentrations, adjusted to contain 1 × 105 viable cells per ml and plated at a density of 2.6 × 104 viable cells per cm2.
Dendritic cell response to HagB and DEFB103
In the first series of experiments, human myeloid dendritic cells were first exposed to HagB to i) establish an exposure dose capable of inducing a comprehensive chemokine and pro-inflammatory cytokine response, ii) establish that HagB and not endotoxin contamination was responsible for the pro-inflammatory response and iii) validate the virtual, integrated dendritic cell model. In Groups 1–4, cells were exposed to 2.0, 0.2, 0.02 and 0.002 µM HagB (Supplemental Table 2, Figure 2). In Groups 5–8, cells were exposed to 2.0, 0.2, 0.02 and 0.002 µM ΔHagB. In Groups 9–12, cells were exposed to 847.0, 79.0, 8.1 and 0.9 ng/ml E. coli 55:B5 endotoxin. In Group 13, cells were exposed to 0.01 M PBS, pH 7.2. At 0, 2, 4, 8 and 16 hour time points, 300 μl culture media was removed for the determination of chemokines and cytokines and 300 μl of LGM-3 was added back to each flask.
In the second series of experiments, human myeloid dendritic cells and murine JAWSII dendritic cells were then exposed to DEFB103, HagB and 0.01 M PBS, pH 7.2 to assess the effect of DEFB103 on the HagB-induced chemokine and cytokine response (Supplemental Table 3, Figure 3). In Group 1, cells were exposed to HagB. In Group 2, cells were first exposed to DEFB103 and then exposed to HagB one hour later (pre-DEFB103 treatment). In Group 3, cells were exposed to a mixture of DEFB103 and HagB (co-DEFB103 treatment). The mixture was prepared by adding DEFB103 to HagB in LGM-3 and incubating the mixture at 37°C for 30 minutes. In Group 4, cells were exposed DEFB103 and HagB at the same time but they were not mixed together like that in Group 3. In Group 5, cells were first exposed to HagB and then exposed to DEFB103 one hour later (post-DEFB103 treatment). In Group 6, cells were exposed to DEFB103. In Group 7, cells were exposed to 0.01 M PBS, pH 7.2. At 0, 2, 4, 8 and 16 hours, post-inoculation, 300 μl tissue culture media was removed and 300 μl of tissue culture media was added back to each flask.
Murine response to HagB and DEFB103
Mice are good models to assess the in vivo effects of DEFB103 on HagB-induced responses: HagB induces a chemokine and pro-inflammatory cytokine response35 and mouse β defensin 14 is the orthologue of DEFB10336,37,38,39. In this study, 90 adult female C57BL/6 mice (5–7 months of age; Charles River Breeding Laboratories, Inc., Willingham, MA) were used and housed in The University of Iowa Medical Laboratory rodent facility. The facility is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care, International; is a registered research facility with the United States Department of Agriculture (no. 42-R-0004); and has a Public Health Services Animal Welfare Assurance (A3021-01) on file. All mice were handled humanely according to The University of Iowa Animal Care and Use protocol number 1005104.
For each experiment, 15 mice (3 mice per each of 5 time periods) were sedated by a brief 30 second exposure to an oxygen/carbon dioxide inhalation mixture and 10 μl of inoculum containing 0.2 µM HagB, 0.1 µM DEFB103, or 0.01 M PBS, pH 7.2 was dispensed with a micropipette into the nares (5 μl/nare). All mice were maintained in sternal recumbency until awake. In Group 1, mice were exposed to HagB only. In Group 2, mice were first exposed to DEFB103 and then exposed to HagB one hour later. In Group 3, mice were exposed to a mixture of DEFB103 and HagB. The mixture was prepared by adding DEFB103 to HagB in 0.01 M PBS, pH 7.2 and incubating the mixture at 37°C for 30 minutes. In Group 4, mice were first exposed to HagB and then exposed to DEFB103 one hour later. In Group 5, mice were exposed to DEFB103. In Group 6, mice were exposed to 0.01 M PBS, pH 7.2. At 0, 2, 4, 8 and 16 hours, post-inoculation, mice were euthanized. 200 μl nasal wash fluid was collected and centrifuged to pellet the cells and debris36. The nasal wash fluid supernatant was removed and stored at −80°C.
Determination of chemokines and cytokines
The concentrations of chemokines and cytokines in 25 μl dendritic cell culture supernatants or 25 μl mouse nasal wash fluid supernatants were determined with commercial multiplexed fluorescent bead-based immunoassays (EMD Millipore, Billerica, MA) in the Luminex 100 IS Instrument (Luminex, Austin, TX) as previously described in detail for dendritic cell culture supernatants16 and mouse nasal wash fluid supernatants16. Chemokine and cytokine standards ranged from 3.2 to 10,000 pg/ml and concentrations of chemokines and cytokines in each unknown sample were interpolated from plotted curves of the known standards vs. their median fluorescent intensities. The HUGO Gene Nomenclature for chemokines, cytokines and defensins (http://www.genenames.org/) was used throughout the maunscript40.
Statistical analysis
A log10-transformation was applied to all the chemokine and cytokine concentrations detected in the tissue culture supernatants and mouse nasal wash supernatants. The log transformation attenuates the positive skew in the distributions of the chemokine and cytokine concentrations and makes the normality assumption more defensible. For the mouse nasal wash fluid supernatants, a two-way mixed effects Analysis of Variance (ANOVA) was fit to the log-transformed concentrations, where the two fixed factors were group and time. A group/time interaction effect was included. To account for the repeated measures on each mouse, a mouse-specific random effect was employed. For the tissue culture supernatants, an analogous two-way fixed effects ANOVA was fit to the log-transformed concentrations, where again, the two fixed factors were group and time. Pairwise group comparisons were conducted using the method of Tukey's Honest Significant Differences (HSD). A 0.05 level was used to determine statistically significant differences. All analyses were conducted using JMP (Version 10.0, SAS, Cary, NC).
References
Harder, J., Bartels, J., Christophers, E. & Schroder, J. M. Isolation and characterization of human β-Defensin-3, a novel human inducible peptide antibiotic. J. Biol. Chem. 276, 5707–5713 (2001).
Tao, R. et al. Salivary antimicrobial peptide expression and dental caries experience in children. Antimicrob. Agents Chemother. 49, 3883–3888 (2005).
Dommisch, H., Acil, Y., Dunsche, A., Winter, J. & Jepsen, S. Differential gene expression of human beta-defensins (hBD-1, -2, -3) in inflammatory gingival diseases. Oral Microbiol. Immunol. 20, 186–190 (2005).
Zilbauer, M. et al. Expression of human beta-defensins in children with chronic inflammatory bowel disease. PLoS One 5, e15389 (2010).
Kesting, M. R. et al. Expression profile of human beta-defensin 3 in oral squamous cell carcinoma. Cancer Invest. 27, 575–581 (2009).
Frasca, L. & Lande, R. Role of defensins and cathelicidin LL37 in auto-immune and auto-inflammatory diseases. Curr. Pharm. Biotechnol. 13, 1882–1897 (2012).
Lippross, S. et al. Multiple trauma induces serum production of host defence peptides. Injury 43, 137–142 (2012).
Jin, G. et al. An antimicrobial peptide regulates tumor-associated macrophage trafficking via the chemokine receptor CCR2, a model for tumorigenesis. PLoS One 5, e10993 (2010).
Boniotto, M. et al. Human β-defensin 2 induces a vigorous cytokine response in peripheral blood mononuclear cells. Antimicrob. Agents Chemother. 50, 1433–1441 (2006).
Niyonsaba, F. et al. Antimicrobial peptides human beta-defensins stimulate epidermal keratinocyte migration, proliferation and production of proinflammatory cytokines and chemokines. J. Invest. Dermatol. 127, 594–604 (2007).
Presicce, P., Giannelli, S., Taddeo, A., Villa, M. L. & Della Bella, S. Human defensins activate monocyte-derived dendritic cells, promote the production of proinflammatory cytokines and up-regulate the surface expression of CD91. J. Leuk. Biol. 86, 941–948 (2009).
Semple, F. et al. Human β-defensin 3 affects the activity of pro-inflammatory pathways associated with MyD88 and TRIF. Eur. J. Immunol. 41, 3291–3300 (2011).
Semple, F. et al. Human β-defensin 3 has immunosuppressive activity in vitro and in vivo. Eur. J. Immunol. 40, 1073–1078 (2010).
Shi, J. et al. A novel role for defensins in intestinal homeostasis: regulation of IL-1β secretion. J. Immunol. 179, 1245–1253 (2007).
Miles, K. et al. Dying and necrotic neutrophils are anti-inflammatory secondary to the release of α-defensins. J. Immunol. 183, 2122–2132 (2009).
Pingel, L. C. et al. Human β-defensin 3 binds to hemagglutinin B (rHagB), a non-fimbrial adhesin from Porphyromonas gingivalis and attenuates a pro-inflammatory cytokine response. Immunol. Cell Biol. 86, 643–649 (2008).
Dietrich, D. E. et al. Human α- and β-defensins bind to immobilized adhesins from Porphyromonas gingivalis. Infect. Immun. 76, 5714–5720 (2008).
Gallo, S. A. et al. Theta-defensins prevent HIV-1 Env-mediated fusion by binding gp41 and blocking 6-helix bundle formation. J. Biol. Chem. 281, 18787–18792 (2006).
Wei, G. et al. Through the looking glass, mechanistic insights from enantiomeric human defensins. J. Biol. Chem. 284, 29180–29192 (2009).
Gallo, R. L. & Hooper, L. V. Epithelial antimicrobial defence of the skin and intestine. Nat. Rev. Immunol. 12, 503–516 (2012).
Van Hemert, J. R. et al. Human β-defensin-3 alters, but does not inhibit, the binding of Porphyromonas gingivalis haemagglutinin B to the surface of human dendritic cells. Int. J. Antimicrob. Agents. 40, 75–79 (2012).
Semple, F. & Dorin, J. R. β-Defensins: Multifunctional Modulators of Infection, Inflammation and More? J. Innate Immun. 4, 337–348 (2012).
Gaddis, D. E., Michalek, S. M. & Katz, J. TLR4 signaling via MyD88 and TRIF differentially shape the CD4+ T cell response to Porphyromonas gingivalis hemagglutinin B. J. Immunol. 186, 5772–5783 (2011).
Vali, S., Pallavi, R., Kapoor, S. & Tatu, U. Virtual prototyping study shows increased ATPase activity of Hsp90 to be the key determinant of cancer phenotype. Syst. Synth. Biol. 4, 25–33 (2010).
Rajendran, P. et al. Suppression of signal transducer and activator of transcription 3 activation by butein inhibits growth of human hepatocellular carcinoma in vivo. Clin. Cancer Res. 17, 1425–1439 (2011).
Equils, O. et al. A computer simulation of progesterone and Cox2 inhibitor treatment for preterm labor. PLoS One 5, e8502 (2010).
Barve, A. et al. A kinetic platform for in silico modeling of the metabolic dynamics in Escherichia coli. Adv. Appl. Bioinform. Chem. 3, 97–110 (2010).
Sultana, Z. et al. Dynamic modeling of alpha-synuclein aggregation in dopaminergic neuronal system indicates points of neuroprotective intervention: experimental validation with implications for Parkinson's therapy. Neuroscience 199, 303–317 (2011).
Roy, K. R. et al. Celecoxib inhibits MDR1 expression through COX-2-dependent mechanism in human hepatocellular carcinoma (HepG2) cell line. Cancer Chemother. Pharmacol. 65, 903–911 (2010).
Ao, X. et al. Radiation produces differential changes in cytokine profiles in radiation lung fibrosis sensitive and resistant mice. J. Hematol. Oncol. 2, 6 (2009).
Awasthi, S., Brown, K., King, C., Awasthi, V. & Bondugula, R. A toll-like receptor-4-interacting surfactant protein-A-derived peptide suppresses tumor necrosis factor-α release from mouse JAWS II dendritic cells. J. Pharmacol. Exp. Ther. 336, 672–681 (2011).
Gorr, S. U. Antimicrobial peptides of the oral cavity. Periodontology 2000 51, 152–180 (2009).
Gorr, S. U. & Abdolhosseini, M. Antimicrobial peptides and periodontal disease. J. Clin. Periodontol. 38 Suppl 11, 126–141 (2011).
Hooper, S. J. et al. Viable bacteria present within oral squamous cell carcinoma tissue. J. Clin. Microbiol. 44, 1719–1725 (2006).
Kohlgraf, K. G. et al. Defensins attenuate cytokine responses yet enhance antibody responses to Porphyromonas gingivalis adhesins in mice. Future Microbiol 5, 115–125 (2010).
Rohrl, J., Yang, D., Oppenheim, J. J. & Hehlgans, T. Identification and biological characterization of mouse β-defensin 14, the orthologue of human β−defensin 3. J. Biol. Chem. 283, 5414–5419 (2008).
Roop, R. M., 2nd et al. Brucella stationary-phase gene expression and virulence. Annu. Rev. Microbiol. 57, 57–76 (2003).
Hinrichsen, K. et al. Mouse beta-defensin-14, an antimicrobial ortholog of human beta-defensin-3. Antimicrob Agents Chemother 52, 1876–1879 (2008).
Taylor, K. et al. Analysis and separation of residues important for the chemoattractant and antimicrobial activities of β-defensin 3. J. Biol. Chem. 283, 6631–6639 (2008).
Seal, R. L., Gordon, S. M., Lush, M. J., Wright, M. W. & Bruford, E. A. genenames.org: the HGNC resources in 2011. Nucleic. Acids. Res. 39, D514–519 (2011).
Acknowledgements
This work was supported by NIH, NIDCR grant R01 DE014390. The authors would like to thank Patricia Conrad for preparation of the figures.
Author information
Authors and Affiliations
Contributions
K.A.B. designed the experiments, analyzed the data and wrote the manuscript. S.V., S.R., S.A.P. and R.V. developed the virtual integrative dendritic cell model (Supplemental Table 1 and Figures 1a, b and c) and S.V., using this model, assessed the activation pathways and virtual outcome of dendritic cells treated with HagB, endotoxin and DEFB103 (Supplemental Tables 1 and 2 and Figures 1a, 1b, 1c and 2). L.A.M. and M.R. performed the work with K.A.B. in Supplemental Table 2 and Figure 2. L.E.H. performed the work with human myeloid dendritic cells and JAWSII dendritic cells (Supplemental Tables 3 and 4 and Figures 3 and 4). K.K. performed the work with mice in Supplemental Table 5 and Figure 5. E.N.R. performed the work with K.A.B. in Table 1. A.P.F. provided the HagB, E. coli M15(pREP4)pQE-31-TX1 expressing HagB and helped troubleshoot the HagB purification process. J.E.C. supervised and assisted with the statistical analysis of the study.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Harvey, L., Kohlgraf, K., Mehalick, L. et al. Defensin DEFB103 bidirectionally regulates chemokine and cytokine responses to a pro-inflammatory stimulus. Sci Rep 3, 1232 (2013). https://doi.org/10.1038/srep01232
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep01232
This article is cited by
-
Computational Models Accurately Predict Multi-Cell Biomarker Profiles in Inflammation and Cancer
Scientific Reports (2019)
-
Tissue- and age-dependent expression of the bovine DEFB103 gene and protein
Cell and Tissue Research (2016)
-
Histatin 5 binds to Porphyromonas gingivalis hemagglutinin B (HagB) and alters HagB-induced chemokine responses
Scientific Reports (2014)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.