Key Points
-
Describes impression making to maximise retention, stability and soft tissue support by managing flange thickness.
-
Describes shaping the wax occlusal record rims to prescribe appropriate lip support and natural tooth positions.
-
Demonstrates the shape and extension of dentures giving optimum aesthetics.
Abstract
Even dentures exhibiting superb aesthetics are of no use if they visibly move during speech and social intercourse. In this, the second paper of three on removable denture aesthetics, we describe impression making and shaping the wax occlusal record rims. Not only are the impressions important for producing dentures with maximum retention, stability and support, but their extensions and the thickness of their borders have a decisive influence on lip support and profile. This article shows how the contours of the definitive impressions and the wax rims are developed so as to prescribe the overall form of the replacement gums and teeth. Properly trimmed rims are in essence an early three-dimensional rehearsal, an opportunity for developing the patient's preferred lip support and natural positioning of the denture teeth at subsequent stages. They can also give an early indication of what speech will be like with the new dentures. Without this 3D clinical information, laboratory technicians have to guess where to put the teeth and have little option but to fall back on the stereotypes of their textbook training.
Similar content being viewed by others
Denture production
'Of course, dentures are essentially social appliances,' Per-Olof Glantz.1
It is outside the scope of these articles to provide a step-by-step guide to state-of-the-art complete denture construction. However, producing complete dentures which look wonderful is pointless if they are unwearable owing to poor fit and function. To have a chance of working well in the physical sense, dentures must have sufficient stability for the patient not to be constantly reminded of their presence. And for that dentures must rely on their fitting surfaces, polished surfaces and occlusal surfaces being optimally shaped and positioned for each individual mouth.
Impression making
It is worth highlighting here our conclusion, from experience, that the quality of the primary impression is crucial in determining the quality of all subsequent stages. Linda Blakely puts it well: 'Developing a good primary impression may be seen as an investment'.2
Traditionally the edentulous impression process is thought of only as that which defines the 'denture bearing area', that which supports and retains 'the fit surface' of the denture. However, it is also possible to make simultaneous or consecutive impressions of the cheeks, lips and tongue as they move naturally when in contact with the superstructure of the denture (that is, the gums and the buccal and lingual surfaces of the teeth). We call the trayless version of this 'the French impression', because we learnt it from from a gifted French prosthodontist, Hubert Aïche. It is also known as a piezographic impression.
Denture retention and aesthetics
The first and most obvious connection between retention and aesthetics is that any movement of a denture which is visible to an onlooker amounts to an aesthetic disaster as well as a potentially humiliating social experience. This is what the wearers of dentures with unreliable retention usually fear most.
Denture retention has a second relevance to appearance: when the dentures are well retained, the visible anterior teeth may be placed in any position which is attractive and appropriate (personal) for the individual. Deep overbites and large overjets present no problem. This opens up the aesthetic possibilities for the patient/clinician team and allows the denture patient to have virtually any dental appearance he or she desires. And this in turn frees the dental team, time and cost permitting, from the constraints of stereotype 'on-the-ridge' denture set-ups and the classic 'false teeth' appearance.
Without access to the stabilising effects of overdenture abutments, natural or implanted, the retention of a conventional complete denture (in the presence of adequate saliva) will depend mainly upon the accuracy of its fit to the soft tissues. And this in turn will depend on the quality of the primary and secondary impressions.
Impressions themselves directly affect the appearance of the complete (or nearly complete) denture wearer's face. By influencing the thickness of the labial flanges they can have a noticeable positive or negative effect on the support of the denture wearer's lips. In the upper jaw too thick a labial flange border causes a lip bulge under the nose and inversion of the vermillion border, making the wearer look older. With the lower primary impression, over-extension of the labial sulcus zone, as still traditionally taught in textbooks and dental schools, often leads to an over-extended labial flange. Apart from discomfort and an unnatural lower lip appearance, this can cause visible instability of the final denture as it bobs up and down.
A full description of impression techniques is not provided here. Instead, points are made about those aspects of impressions which the authors believe to have a direct impact upon denture wearers' appearance. The interested reader can find further detailed instructions on impression making in the references.
Maxillary impressions
Removable prosthodontics is the only branch of dentistry where accurate sulcus impressions are required.
In order to produce a maxillary complete denture with good retention, support and stability, it is important to make a definitive (working) impression which records functionally moulded sulci and a slightly compressed posterior border. The purpose of this 'border seal' in the finished complete denture is to preserve the saliva/air meniscus between mucosa and denture surface. The surface tension of this meniscus is greater the closer the fit and resists the ingress of air or other fluids which would destroy the 'suction retention' of the denture.
A primary impression must be made to produce a cast which allows the fabrication of a correctly extended custom tray. The custom (special) tray borders are moulded functionally, preferably by adding a thermoplastic material such as impression compound (Fig. 1) to the special (custom) tray posterior to the upper premolars. Thermoplastic materials, such as impression compound can be re-softened and border-moulded until a perfect shape is achieved. A light bodied material such as alginate or silicone finalises the impression (Figs 2 and 3).3,4
Upper lip support
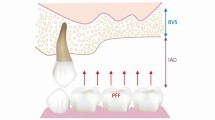
Care is taken to keep the labial border of the impression very thin (Figs 2 and 3), without a border moulding material, corresponding with the minimal bone loss (Fig. 4) which occurs at the top of the labial sulcus region after the anterior teeth have been extracted.5 This thinness will allow the upper lip to assume its pre-extraction form when the new dentures are worn. (Note: the final relaxation of the lip towards its natural form may require a few weeks of wearing.)
Note the absence of resorption at the top of the labial sulcus, where the bone behind the anterior nasal spine may be considered respiratory, not dental, and its post-extraction function therefore unchanged. To restore the lip to its pre-extraction contour, a denture should replace only what is missing. Reproduced with permission from B. Bergman et al., Clinical long-term study of complete denture wearers, Prosth. Dent. 2018, Vol. 53, Elsevier
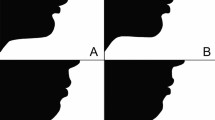
We take issue with those published texts which show thickened labial flanges, formerly known as having 'rolled borders' or 'plumping' (Fig. 5). This is still taught on the pretext of: a) creating a border roll that the lip muscles are supposed to grip (they do not); or b) perhaps influenced by the appearance by the labial sulcus when the lip has been distorted by lifting in order to view the sulcus. These conceptual errors of shape produce a classic bulge of the upper lip under the nose and reduce the visible height of the vermillion border as it curves inwards under the bulge. This unattractive thin-lipped appearance is characteristic of many upper dentures with rolled labial flange borders and front teeth set 'on the ridge' (Fig. 5). Most upper lips resting on natural teeth and gums have a concave profile in the philtrum area. With a well-shaped labial flange in place, it should be possible to run one's finger down the face next to the nose on to the upper lip and not feel the start of the flange (Fig. 6). (In the lower denture such thickening or overextension of the labial flange usually does not push out the lower lip; instead the mentalis muscle pushes the denture up during speech, kissing, etc, or even at rest.)
Mandibular impressions
Producing a lower complete denture with good retention and stability is challenging. A recent improvement in the production of mandibular complete dentures has been developed by Jiro Abe in the form of the mandibular suction-effective denture.6 This requires covering the entire retromolar pad and produces an intact peripheral seal around the lower denture (Fig. 7). A definitive impression is made in a special tray during which the patient performs particular functional movements whilst the impression material hardens (Fig. 8). One of the authors has used a modified form of this technique for the past two years with impressive results7 and improved clinical outcomes.
The denture teeth are positioned and the shapes of the polished surfaces are designed to facilitate suction, maximising support and stability.
Lower piezographic impression (French impression)
This trayless mandibular impression procedure is useful in restoring natural undistorted lower lip support. An impression made without any supporting tray was devised in Paris by Pierre Klein because of the over-extension which manufactured edentulous stock trays always cause (Fig. 9).8 He coined the term piezograph (Greek: piezo – force, graphos – form). The technique is fully described by Hubert Aïche.9 Instead of a tray a wire stiffener supports medium viscosity silicone impression material injected into the denture space over the mandibular ridge. The patient performs functional movements, speaking and swallowing during setting of the silicone. One or two layers of low viscosity silicone impression material are added until the piezograph has a smooth continuous surface, limited labial sulcus extension, somewhat wider extension in the molar regions, lingual surfaces which are concave, and frequently a posterior 'occlusal' surface which bears the marks of the opposing teeth or record rim (Figs 10 and 11). This piezograph, an unbiased record of the movement of the soft tissues in function, gives the tongue and lips all the space they need in function and produces immediately a marked increase in stability compared with the existing lower denture. The tooth positions and polished surfaces of the new lower denture are copied from the piezograph, resulting in optimal lower lip support (Figs 12, 13, 14, 15).
Digital calliper measuring a typical distance (1.58 mm) from crest of ridge to front of labial sulcus on a trayless primary impression. With an over-extended stock tray impression this distance would be several times greater. A lower complete denture made to those over-extended dimensions will bob up and down under the influence of the active mentalis muscle, and the lower lip posture could be compromised (JB*)
Same lips as Figure 12 (overextended lower labial flange)
It is possible to combine Jiro Abe's definitive impression technique with the French impression on a base made on the definitive cast. An extremely thickly mixed tissue conditioner (for example, Viscogel, or Lynal) is built up on the base in quantities representing the teeth and gums. The patient carries out speech and sipping movements until the tissue conditioner has set, resulting in a piezograph (Fig. 16). The tooth positions and polished surfaces of the new lower denture are later copied from the piezograph using lingual and labio-buccal indices. This results in enhanced stability as well as improved speech and lower lip posture.
Shaping the wax occlusal record rims
For optimum appearance in complete denture wearers: start with the face, not the teeth.
While opinions vary about which dental appearance is most attractive in any particular person's face, there is usually less disagreement when it comes to the shape of the face itself. Most people, apart from those given to the regular use of lip fillers, botox, etc., agree when lips appear under- or over-full, when the jaws are propped open or 'overclosed'. We generally agree, too, when the contours of the face are right, the lips look 'at peace' and the overall dimensions seem normal.
Initial experiments
Assuming the patient already wears an upper denture replacing the front teeth, he/she may have an opinion, if asked, about whether the support of the upper lip looks normal and attractive. Where the upper lip looks to the clinician under-supported (the front teeth too far back), a warmed strip cut from a sheet of modelling wax or carding wax can be placed while still warm on the labial surfaces of the front teeth (Figs 17 and 18), and the denture returned to the patient. This simple demonstration can, in many cases, produce a dramatic improvement in the appearance of the mouth and face (Fig. 19), as well as increasing confidence in the clinician.
This has the effect of exposing more of the vermillion border of the lip and may even soften (but not remove!) any vertical wrinkles which the ageing process has brought. This simple trial of improved lip support will often make the patient's face look younger, sometimes by as much as five years. It illustrates at the first appointment what a well-designed new denture could achieve (JB*)
The record rims used in denture construction are intended only to replace the tissues missing as a result of the loss of teeth.
Wax is an ideal material from which to make record rims. It can be added to, subtracted from, moulded, trimmed, smoothed with a flame or hot instrument, and later form an ideal platform in which to set up the denture teeth. Modification of the record rims is the simplest and most perfect way of creating the overall shapes which define the optimum forms of the dentures; and the optimum forms are those which return the face to harmony and normality.10
To achieve the most natural appearance it is necessary to place the artificial teeth in positions as close as possible to those of their natural predecessors. Not only does this restore natural lip support, it also increases the stability and retention of the dentures because the artificial teeth and gums lie within the neutral zone (more specifically called the 'denture space') where forces from the soft tissues are least disruptive. Bone, constantly remodelled in response to the forces which are applied to it, may be regarded as akin to an extremely viscous, slow moving fluid; natural teeth maintain their positions in the jaws because the net forces of the cheeks, lips, tongue and contact with other teeth keeps them there.
To mimic an edentulous patient's natural dentition, casts of that dentition would provide an ideal three-dimensional reference. However, it is rare to have such casts available, even soon after the last natural teeth have been removed (casts of the natural dentition are a service which the forward-thinking practitioner might easily provide for any interested patient – especially for wind instrument players, whose tooth-supported embouchure may have taken years to perfect). Dentate photographs are frequently available, however, such as on the patient's wedding day or in school photographs or as holiday snaps. Full smiling photographs can be used to calculate the size, shape and position of the teeth (Fig. 20). Closed mouth photographs of the face from different angles give a good indication of natural lip support.
With the exception of the incisive papilla the authors do not endorse a one-scheme-fits-all approach to tooth positioning as advocated in some complete denture systems (BPS and PTC system, formerly Swissadent) which use anatomical landmarks for positioning the teeth. Indeed there seems to be a divergence in concepts of shape within the teaching of complete denture construction.
Mechanical vs morphological concepts of denture shape
On the one hand there is what might be called the geometric approach. Landmarks are identified in the patient's mouth and on the working casts and strict rules are established for placing teeth along lines connecting those points. These rules follow simple mechanical principles and are intended to minimise the tilting of dentures during unilateral chewing. One example of this would be setting the lower first molar at the lowest point of the residual ridge and directly above the crest of the ridge (Condylator/Gerber system). Another example is setting posterior teeth along a straight line connecting the centre of the retromolar pad with the imagined original position of the absent mandibular canine. What these geometric concepts have in common is: a) they are intended to minimise tilting during mastication; and b) the patient is required to adapt to the denture shape that these rules impose. Similar strictures may be applied to the positions of upper anterior teeth, whose incisal edges are placed a fixed distance below the residual ridge and with tooth necks close to its crest, so as to minimise tipping of the denture during incising.
This approach seems to find favour in cultures where rules and protocols are welcomed as bringing order and controlling the variability of nature. Patients are required, and perhaps expect, to comply with the rules laid down in the denture clinic. In some centres, for example, they are expected to learn to chew on both sides of the mouth at once (an awkward and unnatural accomplishment) and to keep their tongues out of the way of the lower denture.
At the other end of the denture shape spectrum is what might be called the biomorphic approach. This starts with the assumption that the optimum shape of a complete denture is one which most easily co-exists with established movement patterns of the soft tissues of the mouth and thus is expected to require the least adaptation by the patient. Cine-radiographic studies have shown that most well-fitting complete dentures move about in the mouth a great deal during eating, however carefully made and however much the geometrists might imagine that they don't. The functional success of complete dentures at these moments will depend on the neuromuscular skill of the denture wearer, and this will be enhanced if the foreign objects (the dentures) clash with the soft tissues as little as possible. The impression technique for this end is radically different in that the primary lower is carried out without the use of any tray, impression material being injected directly into the mouth (see the French impression above).
The incisive papilla
There is one landmark on the residual ridges which has proved a very useful reference point. The centre of the incisive papillae is often cited as a useful reference for positioning the upper front teeth. Most studies indicate the actual position of the labial surface of the upper central incisors' incisal edges is within a range of 5 to 12 mm in front of the centre of the incisal papillae.11,12,13,14,15,16,17,18,19,20,21,22 The papilla therefore gives a guide for positioning the upper front teeth and before that to the sculpting of the wax occlusal rim to indicate the position of those teeth. The use of dentate photographs is invaluable (Fig. 20). In addition, the Alma Gauge (Fig. 21) is an extremely useful diagnostic tool for measuring the existing denture, the wax rim and new dentures to check that the teeth within the position of the upper central incisors are within this range.
If the patient doesn't have dentate photographs of their own, photographs of a sibling or son/daughter may be used as a guide (Figs 22, 23, 24). Dental technicians report that clinicians rarely carve wax rims and simply use the rims as sent from the lab to record the maxilla-mandibular relationship. As a result the dental technician does not know the correct labial position of the upper front teeth and has to guess it. This is another good reason for setting up the upper front eight teeth at the chairside, to the patient's satisfaction.
If the clinician is reluctant to set the front teeth, the ideal sequence of information transfer between clinic and laboratory using two Alma Gauges (one in each location) would go as follows:
-
1
Visual assessment of lip support with current dentures in place
-
2
Assessment of location of upper denture front teeth with Alma Gauge. (If less than 5 mm in front of the incisive papilla, they are almost certainly too far back)
-
3
If lip support is inadequate, with thin upper lip (thin vermillion border), add diagnostic wax to front teeth to produce lip support which the patient approves
-
4
Trace the outline of the modified dental arch shape on the protective Alma Gauge sleeve with a waterproof marking pen and write the horizontal and vertical readings on the sleeve
-
5
Send the definitive upper impression to the lab with the Alma sleeve, requesting an occlusal rim which conforms to those measurements
-
6
Receive the rim and the sleeve back from the laboratory.
The clinician should now have a record rim that requires little modification. However if the laboratory has not followed instructions, it will be blindingly obvious (Figs 25 and 26).
Upper record rim not made according to instructions in Figure 25
In order for the shape of the upper wax rim to be accurately assessed it is important for the rim to have good retention. This is achieved by optimal definitive impression making and having a functioning post dam on the rim at this stage, rather than just before processing, as is more customary.
The rim is carved with repeated reference to the dentate photographs provided by the patient until the whole dental team (patient with two mirrors, clinician and nurse) approves. It is helpful to have these photographs enlarged on a TV screen in the surgery (Fig. 27). With the rims in place the patient's face can be examined from different angles including above and below. Holding a hand mirror under the patient's chin and looking down over their shoulder will immediately reveal any unwanted asymmetry of the upper lip relative to the lower.
The shape of the upper rim is prescribed in the following order:
-
1
Lip support
-
2
Incisal plane: viewed from the front this is usually parallel with the inter-pupillary line, unless the patient had a cant and wants this to be incorporated into the final denture (for example with an asymmetrical smile). Note: the prosthetic incisal plane and posterior occlusal plane are not necessarily related, just as the front teeth and back teeth are best considered to be independent of each other. An example would be creating Class II/div 2 dentures with a deep overbite; the upper incisal plane would be well below the posterior occlusal plane, and the lower incisal plane quite possibly above it
-
3
From the side view the occlusal plane is carved parallel with the ala-tragal line (Camper's plane) as this is approximately parallel with the occlusal plane in fully dentate people
-
4
The buccal corridors created by carving back the buccal walls of the rim with reference to the dentate photographs supplied
-
5
The centre line is scribed clearly on the rim and checked with the patient, looking in a mirror
-
6
Speech – when the exterior (bucco-labial) surfaces have been agreed, it is now possible to remove all the superfluous wax from the inner (lingual) surfaces, upper and lower, thinning it down to the approximate volume of incisors at the front and the greater volume of molars at the back. When the occlusal plane is finalised, the upper rim is an approximation to the dimensions of the forthcoming denture. This means it can be used to test clarity of speech, as additional confirmation of the shape, initially with the patient's current lower denture in place, and later, when both rims have been reduced to the approximate dimensions of final dentures, with both wax rims seated. Speech is conventionally considered only after the teeth have been set up at the try-in stage, but it is usually much easier to modify the shape of wax rims in the pursuit of clear speech than to move denture teeth around after they have been set up.
Clear speech must be regarded as an aesthetic requirement since 'aesthetics' has to do with beauty in any sphere, not only visual. However, if there are major changes from the existing dentures for positive visual gains, the patient may need a little time to adapt speech to those changes. Quite often that adaptation will occur automatically during the course of a single appointment, but if not, it is helpful to remind patients of the speech adaptation period needed initially with the dentures they are currently wearing. The issue should become clearer when the teeth are set up for the initial try-in, guided by the rim shapes. (The detailed relationship between dental arch shape and phonetics is beyond the scope of this article).23
Assessing the occluding vertical dimension (OVD)
This is a crucial determinant of the aesthetic result since changing the OVD considerably affects the appearance of the face. The aim is to create an OVD which would be the same as if the patient were still fully dentate. Yet there is no universally accepted or completely accurate method of determining the vertical dimension of occlusion in edentulous patients and it is famously prone to error. This is where experience comes in helpful, as the OVD of the rims is adjusted until the face 'looks right'. This apparently 'fuzzy' suggestion is surprisingly effective. Humans have evolved to be very good at pattern recognition, especially of the human face. Even untrained people can frequently distinguish between a face with the jaw at rest or in the occluding position, a difference of maybe only 2 mm intraorally.
A variety of methods have been advocated to determine OVD. Interested readers are referred to an excellent review article by Fayz and Eslami,24 which describes many of them. One point should be stressed, however, which is not always mentioned: when assessing the rest (postural) position it is important that the patient should be sitting upright without contacting the headrest of the dental chair. The headrest can easily falsify the rest position – too far back and the strap muscles of the neck will pull the mandible downwards; too far forwards and the opposite can happen. Neither will permit a true postural position.
Once the OVD has been finalised, the occlusal record rims are fixed together in retruded axis position (US: 'centric relation').
All the above is classic denture technique, yet we are told that many practitioners simply use the rims to record the upper and lower jaw relationship, without any detailed indication of lip support or front tooth position. This is unfair to the technician and is bound to reduce the quality of the end result. However, we are also told that many technicians are reluctant to use the fully adjusted occlusal rims for setting up the teeth since they want to keep them as evidence in case of any dispute about the accuracy of jaw relations in the set-up.
It is important that the whole dental team are involved in shaping the occlusal rims. The dental nurse (and dental technician if present) should collaborate and participate in this process, but only by assisting the patient in deciding about the lip and face support and the speech, not by automatically confirming the clinician's opinion.
*Key to clinicians and technicians involved in these cases:
JB – John Besford (clin)
RG – Rowan Garstang (tech)
FS – Finlay Sutton (clin)
AT – Andrew Taylor (CDT)
REB – Ruth Bourke (tech)
References
Glantz P O . Personal communication to John Besford. 1981.
Blakely L . Presentation at Spring 2012 meeting of The Besford Study Club. 2012.
McCord J F, Grant A A . A clinical guide to complete denture prosthodontics. London: BDJ Books, 2000.
McCord J, Grant A . Prosthetics: Impression making. Br Dent J 2000; 188: 484–492.
Bergman B, Carlsson G . Clinical long-term study of complete denture wearers. J Pros Dent 1985; 53: 56–61.
Abe J, Kokubo K, Satõ K . Mandibular suction-effective denture and BPS. Tokyo: Quintessence, 2012.
Sutton A F . A series of 10 patients with suction on mandibular complete dentures. 2011. Video available at https://www.youtube.com/watch?v=Fn9UidXPYFQ. (accessed January 2018).
Klein P . Piezography: dynamic modelling of prosthetic volume. Actual Odontostomatol (Paris) 1974; 28: 266–276.
Aïche H . A preliminary functional impression for the mandibular complete denture. Int J Prosthodont 1989; 2: 543–548.
McGee G F . Tooth placement and base contour in denture construction. J Pros Dent 1960; 10: 651.
Harper R N . The incisive papilla—basis of technique to reproduce the positions of key teeth in prosthodontia. J Dent Res 1948; 27: 661–668.
McGee G F . Tooth placement and base contour in denture construction. J Pros Dent 1960; 10: 651.
Hickey J C, Boucher C O, Woelfel J B . Responsibility of the dentist in complete denture construction. J Pros Dent 1962; 12: 637–653.
Martone L C . Clinical application of concepts of functional anatomy and speech science to complete denture prosthodontics. J Pros Dent 1963; 13: 4–33.
Watt M D . Designing complete dentures. Philadelpia: W B. Saunders, 1976.
Ortman H R, Tsao D H . Relationship of the incisive papilla to the maxillary central incisors. J Prosthet Dent 1979; 42: 492–496.
Marvroskoufis F, Ritchie G M . Nasal width and incisive papilla as guides for selection and arrangement of maxillary anterior teeth. J Pros Dent 1981; 45: 592–597.
Grave A M, Becker P J . Evaluation of incisive papilla as a guide to anterior tooth position. J Pros Dent 1987; 22: 113–119.
Lau G. Clark R . The relationship of the incisive papilla to the maxillary central incisors and canine teeth in Southern Chinese. J Pros Dent 1993; 70: 86–93.
Sawiris M . The role of anthropometric measurements in the design of complete dentures. J Dent 1977; 5: 141–148.
Ehrlich J, Gazit E . Relationship of the maxillary central incisors and canines to the incisive papilla. J Oral Rehabil 1975; 2: 309–312.
Solomon E, Arunachalam K . The Incisive Papilla: A Significant Landmark in Prosthodontics. J Ind Pros Soc 2012; 12: 236–247.
Kong H J, Hansen C A . Customizing palatal contours of a denture to improve speech intelligibility. J Pros Dent 2008; 99: 243–248.
Fayz F, Eslami A . Determination of occlusal vertical dimension: A literature review. J Pros Dent 1988; 59: 321–323.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Besford, J., Sutton, A. Aesthetic possibilities in removable prosthodontics. Part 2: start with the face not the teeth when rehearsing lip support and tooth positions. Br Dent J 224, 141–148 (2018). https://doi.org/10.1038/sj.bdj.2018.76
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2018.76
This article is cited by
-
Reader panel profile
British Dental Journal (2019)