Key Points
-
Cysts of the oral region occur commonly owing to the mouth's complex embryonic origins and frequency of inflammation.
-
The classification of cysts has been amended several times and some of the terminology can appear confusing.
-
Presents simple strategies to optimise the management of oral cysts.
Abstract
A cyst may be defined as a pathological (or abnormal) body cavity, usually lined by epithelium, which contains fluid (gas or liquid) or semi-solid substances other than (primarily) pus. Even this definition is contentious, as some pathologists prefer the term pseudocyst or cavity1 when there is no epithelial lining. However, the above definition, based on that of Kramer,2 is as inclusive as possible. Cysts of the mouth and jaws are fairly common and their management is an essential component of oral surgery. This third article in the series deals with the classification, diagnosis and management of the common cysts of the head and neck.
Similar content being viewed by others
Main
It is helpful for the surgeon to have a working classification of the cystic lesions of the oral cavity. There are, however, several systems of classifying such cysts, some of which overlap. Within the jaws, cysts can most usefully be classified according to their site – hard or soft tissue – and their tissue of origin – odontogenic when related to the teeth and non-odontogenic in all other cases (Table 1).
In practical terms, the site of origin of a cyst is generally self-evident. Correct diagnosis is essential as it will directly affect patient management and planned surgery.
Intraosseous cysts
Three major subdivisions of intraosseous cysts were originally proposed by the World Health Organization (WHO) (Table 1), but the most recent editions of the classification have been contentious and more focused on neoplastic lesions.3 The original categories were:
-
Odontogenic cysts (eg radicular cysts, dentigerous cysts and odontogenic keratocysts)
-
Non-odontogenic cysts
-
(eg incisive canal (nasopalatine duct) cysts)
-
Non-epithelial cysts (eg traumatic (solitary) bone cysts).
Histological findings remain the cornerstone of diagnosis, and the original paper by Pindborg et al. summarises these.4
Intraosseous cysts are commonly asymptomatic at presentation and are often noted as incidental radiographic findings. Moreover, because of their position and slow growth rates, they may go unnoticed for many years and reach a considerable size before any symptoms develop. When they do become apparent, the most frequent signs and symptoms are swelling, facial asymmetry, mobility of adjacent teeth and displacement of dentures (Fig. 1a).
Histopathology after enucleation confirmed a radicular cyst on lower right 3 and a keratocyst on lower right 4. The patient remains under review; (b) Large anterior mandibular cyst presenting with bluish discoloration of overlying mucosa confirming that the cyst has breached the underlying bone or is within soft tissue
At this stage, the overlying bone becomes considerably thinned by growth of the cyst and a characteristic 'egg-shell' crackling can often be elicited with gentle manual pressure. If the enlarged cyst breeches the bone or resides in soft tissue the mucosa may appear with a bluish hue (Fig. 1b). When cysts have reached this size another common late event is secondary infection (either acute or chronic) of the cyst cavity. The formation of pus within cyst cavities is not uncommon but, by definition, it needs to be a secondary process. In the mandible, cyst expansion may be so great that a pathological fracture occurs. While extensive cysts may physically displace the inferior alveolar neurovascular bundle, it should be remembered that paraesthesia is a more frequent indicator of serious conditions such as neoplasia or osteomyelitis.
Odontogenic cysts
Radicular cysts
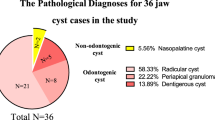
Radicular cysts are the most common of all odontogenic cysts, representing >50% of jaw cysts in several studies.5,6,7,20 They result from chronic inflammation around the apices of non-vital teeth, are lined by stratified squamous epithelium and usually have a chronic inflammatory infiltrate in the wall. There may be a previous history of trauma or failed endodontic therapy, or another cause for the loss of tooth vitality. These cysts occur more frequently in males in the anterior maxilla and present as unilocular periapical radiolucencies with well-circumscribed margins radiologically, and are often associated with root-canal-treated teeth (Fig. 2a) or carious non-vital teeth (Fig. 2b). Radicular cysts usually enlarge in the direction of least resistance. Though buccal expansion is more common, cysts on teeth whose root apices are palatally or lingually placed (ie maxillary permanent second incisors and first molars) may present initially as palatal or lingual swellings.
Residual cysts
Residual cysts are almost certainly radicular cysts that were present when a non-vital tooth was extracted and which did not resolve spontaneously. While there is little good research on the subject, it appears that many radicular cysts resolve without any further surgical intervention once the offending tooth has been removed; those that do not are often histologically indistinguishable from a radicular cyst other than having a general tendency to show less inflammation in the wall of the cyst as time elapses.5,8
Dentigerous cysts
These are the second most common odontogenic cysts, representing ∼20% of cases.20 They arise from the reduced enamel epithelium after amelogenesis is complete and are associated with a failure of eruption. The precise definitions differentiating enlarged dental follicles (Fig. 3a), paradontal cysts (Fig. 3b) to dentigerous cysts (Figs 3c–e) are not clinically obvious, and patients may require review to assess lesion progression before surgery is prescribed. The dentigerous cyst encloses the crown of an unerupted tooth (being attached at the cemento-enamel junction) and is lined by cuboidal or low columnar epithelium. The cysts commonly arise on teeth that normally erupt last in the dental sextants as these are most likely to be impacted. The cysts are almost always unilocular. Unerupted teeth may be considerably displaced and if the associated teeth are high risk for nerve injury, coronectomies may be considered. Dentigerous cysts are also known as follicular cysts, but this terminology has never been popular with pathologists.9
(a) Enlarged dental follicle on lower right unerupted third molar; (b) Bilateral paradontal cysts on lower third molars and radicular cyst on lower right first premolar; (c) Radiolucency associated with the crown of the mandibular right third molar, confirmed to be a dentigerous cyst. Note the resorbed distal root of the first molar; (d) Cystic radiolucency, later confirmed to be a dentigerous cyst, associated with maxillary bilateral supernumerary teeth; (e) Large left monolocular radiolucency associated with an unerupted lower left third molar in an edentulous patient; (f) CBCT sections of a dentigerous cyst arising on a mandibular third molar
Odontogenic keratocyst
There is considerable variation in the reported prevalence of odontogenic keratocysts but they are probably the third most common of all the odontogenic cysts. Of these, they have been the subject of the most research, debate and name changes, which have included primordial cysts, keratocystomas, ortho-keratinised/para-keratinised odontogenic cysts and keratocystic odontogenic tumours.10,11,12,13,14 This divergence is, at least in part, due to the behaviour and presentation of odontogenic keratocysts, which varies considerably from other dental cysts in that they tend to be:
-
More rapidly growing
-
Prone to recurrence after inadequate treatment
-
Difficult to treat
-
Commoner in younger age groups
-
Frequently larger.
However, keratocysts can often mimic other, more common cysts (Figs 4a–c) and as a result may not be appropriately managed. There is no suggestion that odontogenic keratocysts metastasise and so any nomenclature that suggests they are tumours is generally considered to be unhelpful.
Odontogenic keratocysts arise from remnants of the dental lamina (known as rests or glands of Serres) and typically occur as a multilocular radiolucency in the posterior body/ramus of the mandible. Occasionally however, these cysts occur in a multifocal distribution as part of the naevoid basal cell carcinoma syndrome (Gorlin–Goltz syndrome), which may include multiple basal cell carcinomas, cervical ribs and calcification of the falx cerebri. The cysts are normally thinly lined by epithelium and exhibit distinct para-keratinisation. (Those cysts with ortho-keratinisation are now recognised as a separate and rarer entity). The fibrous capsule of these lesions is normally thin, and satellite or daughter cysts are often evident in the cyst wall. They are often difficult to manage, having a greater propensity to recur following removal than other types of cyst.12 This may be due to the presence of island cysts or it may be the result of incomplete enucleation.
Lateral periodontal cysts
Lateral periodontal cysts are developmental in nature and usually arise in younger patients with no apparent periodontal destruction. These cysts present with a similar radiographic appearance to apical cysts, but are associated with the lateral aspect of a root and usually have vital pulps. The diagnosis of odontogenic keratocyst must be excluded in confirming the definition of lateral periodontal cyst.15
Paradental cysts
These enigmatic cysts are inflammatory in nature and commonly arise in association with buccal furcations of vital molar teeth (Fig. 3b) – most commonly lower third molars. They are characterised by a well-circumscribed unilocular radiolucency and are more common in males in their third decade. Unlike radicular cysts, however, the associated teeth are vital and occasionally bilateral. Another fairly common presentation is in juveniles, which, although similar in its mechanism of formation as an inflammatory response, is sometimes categorised as a separate entity (the juvenile paradental cyst).16,17,18
Gingival cysts
Gingival cysts are soft tissue cysts of which two types are recognised: the relatively common gingival cyst of infants and the much rarer gingival cyst of adults. The former appear as small creamy-white lesions on the surface epithelium and may occur in isolation or in clusters. In any event, they regress spontaneously and are rarely visible by the time the primary dentition begins to erupt. The gingival cyst of adults is frequently applied synonymously with the lateral periodontal cyst, despite the fact that the periodontium is not always involved. They are relatively rare and their pathogenesis remains unclear. Simple excision is curative and, as long as the diagnosis is correct and a gingival cyst is not mistaken for a true lateral periodontal cyst, there is minimal tendency to recurrence.15
Other odontogenic cysts
Among the other odontogenic cysts are the calcifying odontogenic cyst, the botryoid cyst and the glandular odontogenic cyst. Although they are rare, the clinician should be aware of their existence and arrange appropriate referral to a specialist unit for treatment. For those wishing to study the subject in greater depth, Shear and Speight's classic textbook Cysts of the Oral and Maxillofacial Regions has much to commend it.19
Non-odontogenic cysts
Nasopalatine duct cysts
These are the commonest of the non-odontogenic cysts and are also known as incisive canal cysts.18 They are more common in males and, although seen in all age groups, are most common between the ages of 20 and 60 years. Their origin is somewhat controversial but they probably arise from embryonic duct remnants. It has been suggested that they may be noted as incidental radiographic findings in approximately 1.0–1.5% of individuals and this has also been seen in some cadaveric studies. The most frequent presentation is a swelling in the anterior midline of the palate. The adjacent teeth are vital and therefore typically of normal colouration. The lesion (which is situated within the incisive canal) is best seen on an upper occlusal film and, although round, may have a pear-shaped appearance. These cysts are best treated by enucleation via a palatal flap from canine to canine; recurrences are probably due to inadequate enucleation. The cyst is usually lined with a combination of stratified squamous and ciliated columnar epithelia. The previous terminology of globulomaxillary cysts and median cysts found in older textbooks has now been abandoned following their exclusion from the 1992 WHO classification.21
Other epithelially lined non-odontogenic cysts
Other epithelially lined non-odontogenic cysts occasionally occur. Of these, the midline (mid-palatal) raphé cyst of infants is probably the most common, but overall they are exceedingly rare and beyond the scope of this BDJ Clinical Guide. Importantly, non-odontogenic lesions will most commonly occur below the inferior alveolar canal as odontogenic epithelium only originates above the canal.
Non-epithelially lined cysts
Solitary bone cyst
A solitary bone cyst may occur within any bone of the body, but typically occurs in the lower molar region of the jaws. It is the commonest non-epithelially lined cyst (pseudocyst). The associated teeth are vital and the cysts are frequently asymptomatic – probably representing <1% of all intraosseous cysts. Their aetiology is uncertain but they tend to occur in young adults (<20 years) with no definite gender imbalance (despite some reports of a male preponderance). Although the cyst lacks an epithelial lining it sometimes contains blood-stained serous fluid, but many are gas filled. Occasionally, a loose, fibrous tissue lines the inner surface of the cyst with evidence of mild osteoclastic activity. The solitary bone cyst is also known as the haemorrhagic bone cyst, the simple bone cyst and the traumatic bone cyst. Surgical exploration of the lesion and primary closure is almost always curative, presumably by inducing wound healing. Recurrence is rare but has been reported.22
Aneurysmal bone cyst (or cavity)
The aneurysmal bone cyst1 is an even rarer cyst, which occurs in a similar age group and has a similar site distribution to the solitary bone cyst although enlargement of the mandible is a more typical feature. The lesion typically contains numerous blood-filled spaces interspersed with giant cells and fibroblasts and it is much more aggressive than the solitary bone cyst. Recurrence following exploration and enucleation is common and further curettage of the lesion may be required. Some pathologists would argue that the aneurysmal bone cyst is actually neoplastic and should be treated accordingly. There is no doubt that recurrence rates following curettage are high and that the lesions frequently show evidence of dysplastic if not frank neoplastic change.
Stafne's idiopathic bone cavity
Stafne's idiopathic bone cavity is sometimes included in this classification (Fig. 5). It is not a cyst but needs to be distinguished clinically and radiographically from the solitary bone cyst. The latter is almost always found above the inferior alveolar canal, whereas Stafne's bone cavity is an asymptomatic area of rarefaction entirely beneath the inferior dental bundle. In reality, it is no more than a lingual defect in the bone – often occupied by a lobular extension of the submandibular gland; indeed, some pathologists prefer the term salivary gland inclusions.
No treatment is indicated for these cavities, although Branstetter et al.23 suggest that magnetic resonance imaging should be undertaken if there is doubt about the diagnosis. There is some evidence that the lesions are developmental rather than congenital, although their aetiology remains uncertain. Other salivary inclusion cysts occasionally occur, as do various other lesions that can radiographically mimic a cyst.
Clinical & radiographic examination
Although a number of lesions may resemble cysts in their presentation, including central giant cell lesions, ameloblastomas or even tumours, a careful history and detailed investigation will refine the differential diagnosis in the majority of cases (Fig. 6).
Signs and symptoms that are important to note include:
-
Swelling (Fig. 7)
-
Tenderness
-
Discharge
-
Displacement of teeth
-
Tooth mobility
-
Disturbance of nerve function
-
Bluish discoloration of overlying mucosa (see Fig. 1b)
-
Absent or non-vital teeth.
A note should be made of a history of trauma in the region and previous dental treatment such as endodontics, extractions or apical surgery. Any evidence of displacement, caries, mobility and tenderness to percussion should also be recorded. If swelling is evident, its consistency should be determined by palpation and any fluctuance elicited. In extensive lesions of the upper jaw it is also useful to ascertain whether nasal obstruction is present. Worrying signs of malignancy are summarised in Table 2. Some neoplastic lesions manifest as cysts – occasionally because they were cysts that have undergone malignant transformation but more commonly as primary or secondary neoplasms. These lesions should never be regarded as cysts but must be distinguished diagnostically and treated accordingly.
Radiographic examination alone cannot provide a definitive diagnosis of any cyst but it may provide important clues to the diagnosis and suggest further investigations and patterns of treatment. The radiographs most frequently employed in the investigation of patients with intraosseous radiolucencies are dental panoramic tomographs (DPT), intraoral peri- apical views and, less frequently, occlusal radiographs. There is also increasing evidence that cone beam computed tomography (CBCT) can be a useful tool.
It is important to consider the following:
Site: What is the relationship of the radiolucency to non-vital, unerupted teeth and other anatomical structures such as the maxillary antrum and the inferior alveolar neurovascular bundle? It should be remembered that in the posterior maxilla the maxillary antrum is close to the roots of the upper posterior teeth and can display the classic appearance of a cystic lesion. Any evidence of tooth displacement or resorption, or the presence of radio-opaque areas, within the radiolucency should be recorded.
Shape: Is the radiolucency uni- or multilocular?
Outline: Is the lesion well circumscribed or not?
Radiodensity: What is the relative density of the lesion compared with the adjacent bone?
Spread: It is particularly useful in planning to determine the extent of the lesion. For lesions in the ascending ramus, the extent of lingual expansion and spread may be determined using two radiographs taken at right-angles – the DPT and postero-anterior view of the mandible. A more accurate 3D representation can, however, be obtained using CBCT. A preoperative radiograph is essential in determining the size and location of the lesion. It is also important in planning the removal of teeth at the time of operation, particularly those of poor prognosis due to resorption or those with inadequate bony support.
Vitality testing: For periapical radiolucencies, if loss of vitality is suspected (because of a history of trauma, extensive restoration or darkening of the tooth), then thermal or electric pulp testing should be performed.
Aspiration: Aspiration of cyst contents used to be a common procedure but has largely been abandoned for diagnostic purposes other than confirming the diagnosis of an odontogenic keratocyst that contains thick keratin. It is sometimes undertaken therapeutically to decompress a cyst prior to or during surgery but its original use for analysing cyst contents for substances such as cholesterol has been abandoned, as it had virtually no bearing on treatment planning but can help the surgeon ensure that the cavity is not solid, or blood- or keratin-filled (Fig. 8).
Table 3 summarises the investigation of lesions.
Management of common oral cysts
Once the diagnosis of a cyst has been made, there are various treatment options, including:
-
Observe and review
-
Dental treatment:
-
Endodontics
-
Apicectomy
-
Extraction
-
Marsupialisation
-
Enucleation
-
Enucleation plus supplementary treatment
-
Local excision.
Unlike for malignant lesions, there is rarely any place for wide excision of the lesion and adjacent tissue, with or without adjunctive radiotherapy or chemotherapy and reconstruction. If a keratocyst recurs, consideration may be given to excision with a margin possibly with adjunctive use of Carnoy's solution, in an attempt to prevent recurrence.
Probably the most important aspect of any surgical intervention is to firmly establish the diagnosis of the lesion. Wherever possible this should be achieved by fully eradicating the lesion while minimising morbidity. This should allow rapid healing, enabling function to be restored quickly and removing any doubt about the nature of the cyst.
Strategies for applying these treatment options in the management of common oral cysts are summarised in Table 4. Simple endodontic treatment of radicular cysts has been a somewhat contentious issue, mainly due to fact that a confirmed diagnosis cannot be obtained when the lesion has not been fully excised. There are several studies on the efficacy of this treatment modality showing it is effective as a first-line treatment for a tooth with reasonable prognosis with a small, non-infected radicular cyst.8
Despite the various histological profiles of intraoral cysts, their surgical management consists of variations of two basic techniques: enucleation and marsupialisation.
Enucleation of cysts
Enucleation is the removal of the entire cyst lining and the primary repair of the resultant defect (Fig 9a–f). The cyst space becomes filled with blood clot that will organise and remodel, resulting in bony repair. Enucleation is the usual method of treatment for radicular, residual and dentigerous cysts, and is generally the preferred option for the majority of both intraosseous and extraosseous cysts (Figs 10a–e - overleaf). It is often carried out in the context of surgical endodontics.
(a) Preoperative dental panoramic radiograph; (b) Clinical appearance before excision; (c) Aspirate of pus contents; (d) Bone exposure with protection of dental nerves and bone; window cuts performed using a fissure bur; (e) Clean bone cavities after cyst removal; (f) Cyst specimen for histopathology
In removing large intraosseous cysts the incision should be well clear of the margins of the lesion, the aim being to ensure that the suture line will lie on healthy bone. When the cyst cavity is exposed, it is important to try to carefully remove the overlying bone to expose the maximum diameter of the cyst without damaging the lining. Enlargement of the access can be achieved with a large round bur and rongeur bone nibblers. Aspiration of the cyst contents at operation tends to cause separation of the cyst wall from the adjacent tissue. This facilitates dissection of the cyst lining from the bone or mucosa and decreases the risk of cyst rupture. Careful separation of the cyst lining from the surrounding structures should ensure removal of the lesion intact. The lining should be raised from the underlying bone using a spoon-shaped instrument such as a Mitchell trimmer or (where the cyst cavity is large) a Ward periosteal elevator. Where the cyst lining is firmly attached to the periapical tissues, a small curette is extremely useful.
Occasionally, it will be necessary to remove teeth associated with the cyst. The principal indications for this relate to poor postoperative functional prognosis and associated disease. Where teeth have a poor functional prognosis (being displaced, resorbed or lacking bone support), removal together with the cystic lesion is generally the only appropriate form of treatment. The necessity to remove teeth should be explained to the patient preoperatively and the discussion recorded in the patient's notes.
Odontogenic keratocysts may require adjunctive chemical treatment along with enucleation to minimise the risk of recurrence.9,10,11,12,13,14 Additionally, teeth associated with the lining of odontogenic keratocysts are also best removed to minimise the risk of recurrence as a result of incomplete removal of cyst epithelium from the root surface.
Following removal of the specimen (and associated teeth where necessary), debridement is performed. The rough edges of the cavity should be smoothed using a large round bur. In an attempt to decrease the high rate of recurrence of odontogenic keratocysts, treatment of the cyst cavity with cryotherapy and/or Carnoy's fluid is often employed. Extreme care should be taken in their application, especially where the cysts are in the soft tissue, as the solution is quite toxic – basically being designed to 'pickle' the remnant cyst island cells. However, it is non-discriminatory and can cause significant damage to the adjacent soft tissues and especially the inferior alveolar nerve if it has been exposed.
Where extensive bony destruction has resulted from the cystic expansion, attempts have sometimes been made to pack the cyst cavity using resorbable materials, autologous bone and even blood to facilitate the healing process. There is, however, little evidence that this is effective and in most cases the addition of exogenous material simply increases the risk of secondary infection. In some instances, however, where the mandible is severely structurally weakened, bone grafting and internal fixation may be essential to restore functional integrity.
Marsupialisation of cysts
The marsupialisation of cysts involves the creation of a surgical window in the lining of the cyst by removal of the overlying mucosa, mucoperiosteum and bone to decompress the lumen (Figs 11a–i). This procedure involves minimal trauma to the adjacent structures and is simple and relatively quick to perform, often being carried out under local anaesthesia.
(a) Preoperative dental panoramic radiograph; (b) Mucosa overlying the cyst; (c) Aspiration of cyst contents; (d) Incision for the buccal two-sided flap; (e) Elevated flap exposing bone; (f) Window cuts in the bone using a fissure bur to expose and enucleate the cyst; (g) Radiopaque 'spray' of bismuth iodoform paste lining the shrinking cyst cavity with h) bony infill of the cavity; (i) Post extraction of lower left 8 once there was sufficient bone to minimise risk of mandibular fracture
It should involve incision around the cyst margin; tissue is removed for histology to confirm the putative diagnosis, the mucoperiosteal flap is reflected and bone is removed to expose as much of the cyst as possible. The patency of the hole should then be secured by suturing the cyst lining to the mucosa using sutures such as black silk or Vicryl. The cyst cavity can then be carefully packed open using a non-resorbable material such as ribbon gauze soaked in Whitehead's varnish or bismuth iodoform paste. The overlying mucoperiosteum and the small amount of cyst lining removed are sent for histopathological diagnosis. The pack should remain in situ for at least 10 days, when it can be removed and replaced as necessary. As the cavity shrinks in size it is repacked with smaller dressings, and even gutta-percha plugs, acrylic stoppers or extensions to dentures have been employed. This procedure not only allows decreases in the hydrostatic pressure (which is an essential component of cyst formation in most instances) but also allows the cyst lining to be repopulated by keratinocytes migrating in from the oral mucosa at the edge of the wound.
An alternative technique is to leave the cavity open and instruct patients on the use of irrigation using an antiseptic medicament and a blunt-ended syringe. In either case, regular follow-up is a necessary component of treatment.
There are disadvantages to marsupialisation as it offers decreased amounts of tissue for histological examination and protracted inconvenience and repeated visits for the patient and clinician alike over months or even years until healing is complete. Nonetheless, while enucleation is the treatment of choice for the surgical treatment of the majority of cysts there are four situations where marsupialisation is invaluable:
-
1
Where the patient is unfit because relatively large cysts can be treated quickly under local anaesthesia.
-
2
Where a high rate of recurrence is anticipated – for example in the treatment of odontogenic keratocysts. In such cases proponents argue that any recurrence is directly visible, but marsupialisation of such cysts remains controversial and primary enucleation is usually the preferred option unless there are overriding factors concerning the patient's general health.
-
3
Where it is desirable that the teeth within the cyst are allowed to erupt. In these cases, ie eruption and dentigerous cysts (where the operator wishes to retain the tooth/teeth), most of the cystic lesion is excised, and the crown of the tooth is surgically exposed.
-
4
Where the cyst is associated with the roots of many vital teeth, the inferior alveolar nerve or a risk of fracture.
Postoperative care
Patients are usually initially reviewed 5-7 days post-operatively regardless of the treatment modality. The prescription of antibiotics is contentious but still commonly employed along with postoperative analgesia. The use of intraoperative steroids to reduce postoperative swelling also remains controversial.
Clinical and radiographic follow-up of the treated cyst will depend largely on the histopathological diagnosis. Clinical examination accompanied by intermittent radiographic examination to observe new bone formation is usually sufficient to assess the degree of healing. In large cysts that have been marsupialised, it may be 18 months before there is any appreciable diminution in size on radiographs. However, enucleated cysts usually heal uneventfully and show rapid bony repair such that patients can often be discharged at the 6-monthly review.
In the case of odontogenic keratocysts, follow-up is essential over a long period of time (at least 5 years) due to the high frequency with which they recur and the rate of growth they can exhibit.
It should be noted that if resolution does not take place when root canal treatment is performed for what is presumed to be a radicular cyst (Fig. 12) associated with a non-vital tooth, then biopsy may be necessary. The lesion in Fig. 12 proved to be an eosinophyllic granuloma (a form of Langerhans cell histiocytosis) which requires medical management, not surgery and long-term review.
Cysts involving the maxillary antrum
Surgical pathology of the maxillary antrum is covered in Part 2 of this series (BDJ 2017; 223: 483–493) or Chapter 2 in the associated BDJ Clinical Guide).
Many cysts that arise within the maxilla will expand upwards, pushing the antral lining superiorly and leaving the antral airspace separate from the cyst cavity. However, in some cases (especially as a result of secondary infection), the very thin antral lining may break down, allowing the cyst to expand into the maxillary antrum itself. In determining the extent of the cyst and destruction of the thin antral wall, conventional and 3D reformatted CT scans may be useful. In situations where the maxillary antrum is in continuity with the lining of the cystic lesion, enucleation can be performed safely so long as the antral floor remains intact, the defect becoming re-epithelialised from the residual antral lining. Enucleation is therefore the principal treatment of choice, with a few notable exceptions (see 'Enucleation of cysts' in this chapter).
Where a cyst involves the maxillary antrum, inhalation and sympathomimetic agents may be of some additional benefit.
Soft tissue cysts
Mucocoeles
By far the most frequently encountered soft tissue cysts of the oral cavity are the minor salivary gland cysts. These can be formed by mucous extravasation (into the adjacent tissues) or mucous retention (within the small ducts) and are seen most frequently in the lower lip and floor of the mouth (although they can occur anywhere there are mucous glands. Collectively, these tend to be referred to as mucocoeles as they are clinically indistinguishable.26 Mucocoeles are normally treated by excising an ellipse of soft tissue and enucleating the lesion. A proportion of these recur but this can almost certainly be reduced by excising the tiny adjacent mucous glands along the incision line.
Dermoid and epidermoid cysts
These cysts are uncommon in the mouth although both can occur. Usually asymptomatic, they typically occur in young adults in the floor of the mouth, in the sublingual and submandibular region. Patients may present with an enlarging swelling under the tongue that is affecting speech and eating. Both types of cyst are developmental, the dermoid cyst being lined with ectodermal tissue and the epidermoid cyst with epidermis-like cells. The epidermoid cyst is found more commonly on the external skin whereas the dermoid cyst may present either above or below the mylohyoid muscle, but is bimanually palpable in the submental region and in the floor of the mouth. King et al. review 195 cases of dermoid and epidermoid cysts in their paper.27
Aspiration, which is often not possible, produces keratin. These lesions can grow to several centimetres in diameter and are generally better treated in the hospital setting under general anaesthesia. They are enucleated via intraoral, extraoral or occasionally combined approaches. An intraoral approach involves an incision being made in the depth of the lingual sulcus in the floor of the mouth. Blunt dissection is carried out to avoid damage to the submandibular ducts. The lesion has a thick lining, which aids enucleation. A sublingual drain may be required for 24 hours to reduce the size of any sublingual haematoma and steroids should be administered. Ultrasound is of use when investigating such soft tissue lesions of the neck to determine their distribution.
Thyroglossal cysts
Thyroglossal cysts may present anywhere along the tract resulting from the migration of the thyroid gland from the foramen caecum, at the junction of the anterior two-thirds and posterior third of the tongue. Pathognomonically, and in contrast to the dermoid cyst, the cyst moves with the larynx when swallowing or protruding the tongue. These cysts should be treated in the hospital setting under general anaesthesia.
Nasolabial cysts
Nasolabial cysts arise as a swelling between the upper lip and lateral aspect of the alar cartilage of the nose. Occurring most frequently in females in the 20- to 40-year age group, the cysts are superficially placed and not visible radiographically unless they resorb the underlying bone. Lined with stratified squamous or respiratory epithelia, these cysts are best removed via an intraoral approach and enucleation is curative.
Other soft tissue cysts
Other soft tissue cysts occur infrequently and may involve the face, the mouth or the neck. Of these the branchial cleft cyst (cervical lympho-epithelial cyst) is probably the most common, with rarer examples including the thymic cyst, cystic hygroma, lingual cysts and various intrasalivary gland cysts. This list is not exhaustive and readers are again directed to Shear and Speight's textbook for a more detailed treatise on the subject.19
References
Reichart P A, Philipsen H P . Aneurysmal bone cavity (cyst). In: Odontogenic tumours and allied lesions. London: Quintessence, 2004.
Kramer I R . Changing views on oral disease. Proc R Soc Med 1974; 67: 271–276.
Barnes L, Eveson J W, Reichart P, Sidransky D . World Health Organization classification of tumors. Pathology and genetics of head and neck tumours. Lyon: IARC Press, 2005.
Pindborg J J, Kramer I R H, Torloni H . Histological typing of odontogenic tumours, jaw cysts, and allied lesions. Geneva: World Health Organization, 1971.
Soames J V, Southam J C . Oral pathology. Oxford University Press, 2005, p. 6f.
Hjørting-Hansen E, Andreasen J O, Robinson L H . A study of odontogenic cysts, with special reference to location of keratocysts. Br J Oral Surg 1969; 7: 15–23.
Meningaud J P, Oprean N, Pitak-Arnnop P, Bertrand J C . Odontogenic cysts: a clinical study of 695 cases. J Oral Sci 2006; 48: 59–62.
Lin L M, Ricucci D, Lin J, Rosenberg P A . Nonsurgical root canal therapy of large cyst-like inflammatory periapical lesions and inflammatory apical cysts. J Endod 2009; 35: 607–615.
Browne R M, Smith A J . Pathogenesis of odontogenic cysts. In: Browne R M (ed), Investigative pathology of odontogenic cysts. Boca Raton, FL: CRC Press, 1991.
Avelar R L, Antunes A A, Carvalho R W, Bezerra P G, Oliveira Neto P J, Andrade E S . Odontogenic cysts: a clinicopathological study of 507 cases. J Oral Sci 2009; 51: 581–586.
Mosqueda Taylor A, Irigoyen Camacho M E, Diaz Franco M A, Torres Tejero M A . Odontogenic cysts. Analysis of 856 cases. Med Oral 2002; 7: 89–96.
Shear M . Developmental odontogenic keratocysts. An update. J Oral Pathol Med 1994; 23: 1–11.
Stoelinga P J W, Peters J H . A note on the origin of keratocysts of the jaws. Int J Oral Surg 1973; 2: 37–44.
Pitak-Arnnop P, Chaine A, Oprean N, Dhanuthai K, Bertrand J C, Bertolus C . Management of odontogenic keratocysts of the jaws: a ten-year experience with 120 consecutive lesions. J Craniomaxillofac Surg 2010; 38: 358–364.
Shear M, Pindborg J J . Microscopic features of the lateral periodontal cyst. Scand J Dent Res 1975; 83: 103–110.
Main D M . Epithelial jaw cysts: a clinicopathological reappraisal. Br J Oral Surg 1970; 8: 114–125.
Craig G T . The paradental cyst. A specific inflammatory odontogenic cyst. Br Dent J 1976; 141: 9–14.
Main D M G . Epithelial jaw cysts: 10 years of the WHO Classification. J Oral Pathol 1985; 41: 1–7.
Shear M, Speight P M . Cysts of the oral and maxillofacial regions. 4th ed. Oxford: Blackwell Munksgaard, 2007.
Daley T D, Wysocki G P, Pringle G A . Relative incidence of odontogenic tumours and oral and jaw cysts in a Canadian population. Oral Surg Oral Med Oral Pathol 1994; 77: 276–280.
Kramer I R H, Pindborg J J, Shear M . Histological typing of odontogenic tumours. Berlin: Springer, 1992.
Horner K, Forman G H, Smith N J . Atypical simple bone cysts of the jaws. I: Recurrent lesions. Clin Radiol 1985; 39: 53–57.
Brandsetter B F, Weissman J L, Kaplan S B . Imaging of a Stafne bone cavity: what MR adds and why a new name is needed. Am J Neuroradiol 1999; 20: 587–589.
Evans G E, Bishop K, Renton T . Guidelines for surgical endodontics. London: Royal College of Surgeons of England, 2012. http://www.rcseng.ac.uk/fds/publications-clinicalguidelines/clinical_guidelines/documents/surgical_endodontics_2012.pdf
Stoelinga P J W . Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg 2001; 30: 14–21.
Bhaskar S N, Bolden T E, Weinmann J P . Pathogenesis of mucoceles. J Dent Res 1956; 35: 863–874.
King R C, Smith B R, Burk J L . Dermoid cyst in the floor of the mouth. Review of the literature and case reports. Oral Surg Oral Med Oral Pathol 1994; 78: 567–576.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Hill, C., Renton, T. Oral surgery II: Part 3. Cysts of the mouth and jaws and their management. Br Dent J 223, 573–584 (2017). https://doi.org/10.1038/sj.bdj.2017.916
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.916