Key Points
-
Looks into the possible reasons for reduced caries levels in the population of five-year-olds and informs the reader which are likely to have had impact on caries levels and which have not.
-
It suggests that wider use of higher fluoride children's toothpastes is a key contributory factor.
-
Readers can apply this knowledge to help prevent decay even further in children.
Abstract
Objective To explore possible reasons for the reduction in population caries levels among 5-year-old children in England since 2008.
Design An ecological study to explore possible reasons for the apparent reduction in dental caries, which included changes in survey methods, deprivation levels and ethnic mix of the population, impact of community level oral health improvement interventions, reductions in sugar intake, and increases in the availability of fluoride.
Setting Data were drawn from three consecutive epidemiological surveys undertaken in 2007/8 and 2011/12 (NHS Dental Epidemiology programme for England), and 2014/15 (Public Health England Dental Public Health Epidemiology Programme). Evidence about the possible reasons for the observed reduction in caries levels was drawn from a range of national sources.
Main outcomes measures Severity and prevalence of caries at dentinal level as measured by visual means alone among children aged five years.
Results Reasons relating to changes in methods used in the survey, deprivation and ethnicity were rejected, along with community level interventions, as reasons for whole population level change. The factor relating to reduced sugar intake was neither rejected nor sustained. Reasons relating to increased fluoride availability, in particular that for increased concentration in children's toothpastes, was sustained.
Conclusions The reduction in caries levels among 5-year-olds has most likely been brought about by the wider availability of children's toothpaste containing at least 1,000 ppm fluoride, along with other factors
Similar content being viewed by others
Introduction
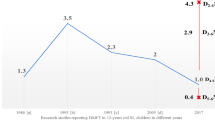
Robust epidemiological information about caries levels in children in the UK has been collected at local level and in a standard fashion since 1985 via surveys that were initially coordinated by the British Association for the Study of Community Dentistry (BASCD) and latterly by Public Health England (PHE). The application of consistent diagnostic and other standards has allowed trends over time to be recorded. The improvements in caries levels among 12- and 14-year-olds have continued since the introduction of fluoride toothpaste.1,2,3 In contrast, prevalence and severity had stayed around the same levels among 5-year-olds between 1992, when country level means became available, and 2006.
The reasons behind an apparent reduction in the severity and prevalence of caries in this age group in England and Wales in 2008 were unclear because a new method of obtaining consent, whereby parents had to 'opt in' to the survey rather than 'opt out', had been introduced, which was highly likely to have biased the sample (Fig. 1).4,5 Further improvements were recorded in England in the 2012 and 2015 surveys which used the same consent method as that in 2008.6,7 This improved picture is seen for all nine government regions of England but does not hold true for all local authority areas.
The magnitude of the difference is large enough to prompt further investigation into the likely cause, especially as there is no single, countrywide intervention in England, unlike in other countries of the UK, but the measured levels of improvement are similar. However, many local authorities commission community level oral health improvement programmes. The aim of this paper is to explore possible factors contributing to the apparent improvement in population levels of dental health in England between 2008 and 2015.
Possible contributory factors include:
-
Changes in methodology of the national survey in England
-
Changes in population demographics or other socio-economic factors
-
Changes in the intake of sugar
-
Changes in the availability of fluoride.
Method
A range of approaches were taken to explore each of the possible contributory factors.
-
The national protocols for each of the centrally coordinated surveys were obtained and reviewed. Particular reference was given to the stages which could have had an impact on the measured levels of disease. These were: sampling, consent, examination methods with regard to position, drying and lighting, use and application of diagnostic criteria including training and calibration, standards and conventions, methods and principles of analysis and reporting.
-
A search of literature was undertaken to identify authoritative information about trends in poverty and ethnic backgrounds of households containing children from 2002 to 2011. Analyses of caries levels by deprivation groups over the three recent surveys and analysis of the 2015 data by ethnic group were completed to explore how these variables may have affected caries levels over time.
-
Existing literature and data were scrutinised to assess trends in sugar consumption over the relevant time period.
-
The availability of fluoride toothpaste of varying concentrations from 2006 to 2014 and the use of fluoride varnish in dental practices during the time period 2009 to 2015 was explored.
Results
1. Changes in methodology
The protocols relating to the nationally coordinated surveys carried out before 2006 and those for the surveys in 2008,8 20129 and 201510 all complied with British Association for the Study of Community Dentistry (BASCD) standards for training and calibration of examiners, sampling, and undertaking caries examinations with regard to volunteer position, drying of teeth and illumination.11,12
The same clinical recording criteria had been applied for visual caries into dentine, as had the conventions with regard to partly erupted and missing teeth for all the surveys since 1987.13
Analysis of the coded data into a variety of composite and singular measures was carried out automatically by a dedicated data collection and analysis programme, Dental SurveyPlus 2. This operated in the same way as its predecessor SurveyPlus and the same methods of calculation were used for a replacement programme which was used in a limited way in 2015. Reporting was also carried out in the same way with the benefits, since 2008, of national collation of raw data instead of simple collection of summarised data.
The only change in methodology that had occurred since the start of nationally coordinated surveys was the introduction, in early 2007, of explicit consent from parents for their children to take part in the surveys. Prior to this consent was passively sought. Analysis of the resulting data arising from the 2008 survey suggested that non-response to the request for consent was affected by factors related to the risk of caries and were over and above deprivation alone.4 There was a marked, apparent reduction in caries prevalence and severity associated with this change in consent. Similar suppression of caries levels were also found in Wales and the decennial national Child Dental Health survey, 2013, both of which had introduced an explicit consent system.14
The same method of seeking explicit consent has been employed in the 2008, 2012 and 2015 surveys in England but the trend of reducing caries levels continued over this time.5,6,7
2. Change in population demographics or other socio-economic factors
Deprivation
The association between caries and deprivation has been widely described and this relationship has remained while caries levels have reduced between 2008 and 2015.7 Statistically significant reductions in caries levels of similar magnitude were found within all deprivation groups between 2008 and 2012 and again in 2015.5,6,7 It was therefore necessary to look at family income levels and absolute and relative poverty to enquire further about the role of deprivation in explaining the change in caries levels.
The Office for National Statistics, using 'Households below average income' figures, reported in September 2010 that child poverty had reduced.15 Looking at relative low income ONS stated that on a national level there had been a fall in the number and the proportion of children living in households below 60% of contemporary median household income between the years 1998/99 and 2008/09 in the UK. These trends had decreased until 2004/05, followed by a slight increase, and then a small reduction between 2007/08 and 2008/09. Consideration of absolute low income showed there was also a marked fall in the proportion of children living in households in low-income thresholds held constant in real terms.
Further evidence of a reduction in child poverty over the relevant time periods is given by the Institute for Fiscal Studies16 which reported on recent trends and future prospects for child poverty in Britain (IFS, 2014). This stated that 'between the late 1990s and early 2000s there was the most sustained and sizeable fall in child poverty of any period over the past half-century, despite fast growth in median income, and hence the relative poverty line, over that period. After stalling in the mid-2000s, relative child poverty has fallen again in the period since 2007–08 though this is primarily due to falling median income, and hence a falling relative poverty line... absolute child poverty has been broadly stable since before the Great Recession. Between 2013–14 and 2015–16, the combination of falling inflation and continued strong employment growth is projected to have reduced the percentage of people living in “absolute” low-income poverty... Relative poverty and inequality are projected to have been roughly unchanged.'
Ethnic backgrounds
Analysis of the 2015 survey data showed that the highest levels of severity and prevalence of caries was found in the children from a Chinese, Eastern European, Asian or 'other ethnic group' background.6
The census survey figures of 2001 and 2011 show that the proportion of 0 to 4-year-old children from white ethnic groups decreased over this decade from 82.6% to 78.6%, and among five to 7-year-olds from 84.1 to 79.1%.17,18 During this period there was an increase in the proportion of children of Asian or Asian British background from 7.0 to 11.7% in 0 to 4-year-olds and 6.5 to 11.5% in five to 7-year-olds. There was no change in the proportion of children of Chinese background and no figures that show how the proportions of children from Eastern Europe changed during the period of interest which is 2008 to 2015. It might be anticipated that the increase in the proportion of Asian/Asian British children might lead to higher levels of caries but, at a population level the opposite is true.
3. True improvement in oral health due to reduced sugar intake and increased exposure to fluoride
Changes in sugar intake
A search was made of existing literature to seek evidence for changes in sugar consumption over the time when the children examined in the recent surveys would have been affected. The focus was on free sugars as it is these that are cariogenic. The National Diet and Nutrition Survey programme provides detailed information on food consumption and nutrient intake by a random, nationally representative sample of adults and children from 18 months upwards living in private households. The data from years 1-6 of the rolling programme give an indication of the patterns of intake over the time period 2008 to 2014, which would have impacted on children who were examined at age five in 2012 and 2015.19,20 These show that there was no significant change in the average daily weight of free sugars consumed in the 1.5 to 3-year-old age group over this period or in the proportion of energy derived from free sugars (Table 1).
Changes in fluoride availability
There are a number of ways fluoride can be available to improve children's teeth. The main vehicles are fluoride toothpaste, fluoride varnish, fluoridated water and milk.
Toothpaste – Factors with regard to the anti-caries benefits of fluoride toothpaste over the time period in question were considered. These were: fluoride concentration of children's toothpaste and frequency of brushing.
Concentration – National guidance, Delivering better oral health (DBOH), recommends that children under three should use toothpaste containing no less than 1,000 ppm fluoride and children from age three should use paste containing no less than 1,350 ppm fluoride.21 Following first publication of this guidance most major manufacturers of children's toothpaste changed many of their formulations. By 2009 and the second edition of the guidance most major manufacturers had increased the concentration of fluoride in children's toothpastes from 550 ppm or less to 1,000 ppm F− or more.22 This process continued until 2014 when only four types of children's toothpastes could be found which contained low levels of fluoride and none which were fluoride free.23 This would suggest that none of the children aged five who were examined in the 2008 survey would have benefited from increased fluoride concentration levels in children's toothpaste. Those examined in 2012 would have been exposed for their most recent three years, while those examined in 2015 would have received the benefits for all of their lives.
One major manufacturer reports that its children's toothpaste makes up 4% of its overall annual volume sales. Children aged one to five years make up 6% of the overall population. If the one manufacturer is similar to the rest then this suggests that about two-thirds of the population aged one to five years old use children's toothpaste. It therefore follows that any changes to the concentration of fluoride in such toothpaste could have a far reaching effect.
The magnitude of the population level change in dental caries levels is similar to that found in trials that distributed toothpaste at 1,450 ppm fluoride to children up to five years old, displacing the use of traditionally low-fluoride children's toothpaste.24
In addition to the clear support for higher fluoride toothpaste the first edition of DBOH gave support for twice daily brushing based on the evidence that this was associated with reduced caries levels.25
Chesters et al. (1991) showed that there could be a 40 to 50% difference in caries levels between those that have optimal habits regarding toothbrushing and those with sub-optimal habits: using toothpaste with fluoride concentration of 1,000 ppm fluoride or less, brushing less often than twice daily and using large amounts of water to rinse after brushing.27
Analysis of caries severity by plaque classification group for each of the three surveys show that children with clean upper anterior teeth had the lowest mean severity, while those with visible plaque had higher levels of decay (Fig. 2).28 The highest decay severity was observed among the small proportion (2%) of children with substantial amounts of plaque visible. This association would suggest that these children were rare or non-brushers and so had less exposure to fluoride toothpaste. In all groups there has been a reduction of caries over time.
Fluoridated water - During the relevant period 2003 to 2014 there have been no new community water fluoridation schemes. The existing schemes, which cover less than 10% of the population, will have continued with the same concentration and coverage so will have continued to provide the same level of benefit to the recipient populations, but no additional impact will have been felt for the wider population over and above that which was present before 2003.
Fluoride varnish – fluoride varnish has been available for use in the UK since the 1960s but its use as an agent for caries control was encouraged by the first edition of Delivering better oral health in 2007.21 This advocated twice yearly application of fluoride varnish for all children from the age of three years onwards and more frequently, and on younger children where caries risk was judged to be higher. Evidence from two Cochrane systematic reviews support the statements which have appeared in subsequent editions of DBOH22,23 with average reductions in caries increment of 37% in the primary dentition with twice yearly application.29
Recording of the use of fluoride varnish started from 2008 when dentists working under NHS regulations were required to note this on their claims for courses of treatment. Some commissioning organisations used the application of varnish as a key performance indicator and this further stimulated its use.
The proportion of children reported as receiving fluoride varnish, albeit with unknown frequency, has increased since 2009 reaching 23%, 31% and 34% for 3-, 4- and 5-year-olds respectively by 2015.30 It cannot be known which children examined in the surveys in 2008, 2012 and 2015 had received applications of fluoride varnish in the preceding years as they were drawn from the whole population, not just from those who attended the dentist. However, it is known that during the period 2006 to 2015 the proportion of all children making an attendance at a dentist has remained steady at 69%.31 If varnish application was evenly distributed among these, then it could be estimated that only approximately 2% of children examined in the survey at age five in 2008 would have received fluoride varnish in the two preceding years (2.8% X 69% = 1.9%) (Table 2).32 Among those examined in 2012, 10% would have received fluoride varnish in the preceding year and in the year before that. For children examined in 2015 about 24% would have received an application of fluoride varnish in the preceding year and 22% in the one before. While individual child patients would have benefited from the application of fluoride varnish the effect on the population overall from this source is unlikely to be significant. Community based fluoride varnish schemes would have benefited the recipients similarly but the impact of this at whole population level cannot be known.
Discussion
All proposed reasons for reduction in measured caries levels were tested by the planned method and informed the conclusions that could be drawn.
During the period 2008 to 2015 there had been no change in methodology of the surveys which could have contributed to a continuing decrease in caries levels at population level. This conclusion is supported by the observation that similar reductions in caries levels have been observed in the Child Dental Health Survey 2013 and in the recent surveys in Wales once explicit consent was introduced.3334 Sampling and analysis methods in these surveys do not follow the same processes as are carried out in England but still resulted in the same pattern of caries reduction. It can be concluded that the continuing changes in caries levels are not an artefact caused wholly by a change in method.
Investigation of the change in population with regard to deprivation and ethnicity revealed that absolute poverty levels in families with children had reduced during this time. The potential effect of this on caries levels is unclear as there has only been an association noted between deprivation and caries, with limited evidence of the effects of changing deprivation levels in a community on caries levels. Hence no conclusion can be made about the likely contributory effect of changes in deprivation on caries levels.
The 2015 survey allowed analysis which showed higher caries levels among Asian/Asian British children, those from Eastern Europe and those with a Chinese ethnic classification compared with other ethnic groups. There had been an increase in the proportion of children from these higher caries risk groups over much of the relevant time period. This would potentially be consistent with an increase in caries levels, however the proportions of children from Asian or Asian/British, Chinese or Eastern Europe are still very low and the effects of higher caries levels among them would be small on the population level overall. It can be concluded that the change in ethnic mix in the population is more likely to increase caries levels and so is unlikely to be a contributory factor to the decline in caries.
Decreases in caries levels could follow changes in health behaviours. These changes could be in response to population and community level promotional interventions or due to individual advice given by primary dental care teams.
Reported levels of sugar consumption were unchanged during the relevant time periods so it is unlikely this is a contributory factor to the reduction in caries levels.
The increased use of higher concentration fluoride toothpaste displacing the use of lower fluoride children's toothpaste, along with increased support for twice daily brushing, may be the main contributory factor in the reducing caries levels in England seen in 5-year-old children. The magnitude of the change is similar to that found in trials that distributed toothpaste at 1,450 ppm fluoride to children up to five years old, displacing the use of traditionally low-fluoride children's toothpaste.24 The increased use of fluoride varnish may also be a contributory factor.
Conclusions
Consideration of possible reasons for the decline in caries levels when examined at an England level would suggest that several factors have had an impact, the strongest being wider availability of children's toothpaste containing at least 1,000 ppm fluoride and the accompanying displacement of use of low fluoride children's toothpaste. Oral health improvement programmes which support the use of fluoride toothpaste and fluoride varnish among higher risks groups are likely to improve caries levels further and reduce inequalities.
References
Sheiham A . Changing trends in dental caries. Int J Epidemiol 1984 13: 142–147.
Anderson R J, Bradnock G, Beal J F, James P M C . Reduction of dental caries prevalence in English schoolchildren. J Dent Res 1982; 61 (Special issue): 1311–1316.
British Association for the Study of Community Dentistry. Changes in Dental Caries Levels. Report of a BASCD Workshop. BASCD Proceedings 1983, 5, No. 2, 17–23.
Davies G M, Robinson M, Neville J, Burnside G . Investigation of bias related to non-return of consent for a dental epidemiological survey of caries among five year olds. Community Dent Health 2014; 31: 21–26.
Rooney E, Davies G, Neville J et al. NHS Dental Epidemiology Programme for England. Oral Health Survey of 5-year-old children 2007/2008. Available from: http://www.nwph.net/dentalhealth/ (accessed December 2016).
Public Health England. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2012. A report on the prevalence and severity of dental decay (2013). Gateway number: 2013–183. Available from: http://www.nwph.net/dentalhealth/ (accessed December 2016).
Public Health England. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2015. A report on the prevalence and severity of dental decay (2016). Gateway No: 2016050. Available from: http://www.nwph.net/dentalhealth/ (accessed October 2016).
NHS Dental Epidemiological Oral Health Survey of 5-year-old children in England. 2007/2008. National protocol. 2007. Available on application via DentalPHIntelligence@phe.gov.uk.
NHS Dental Epidemiological Oral Health Survey of 5-year-old children in England. 2011/2012. National protocol. 2011. Available on application via DentalPHIntelligence@phe.gov.uk.
PHE Dental public health epidemiology programme. Oral health survey of five-year-old children 2014–15. National protocol. Version 2–2014. Available on application via DentalPHIntelligence@phe.gov.uk.
Pine C M, Pitts N B, Nugent Z J . British Association for the Study of Community Dentistry (BASCD) guidance on the statistical aspects of training and calibration of examiners for surveys of child dental health. A BASCD coordinated dental epidemiology programme quality standard. Community Dent Health 1997a; 14 (Supplement 1): 18–29.
Pine C M, Pitts N B, Nugent Z J . British Association for the Study of Community Dentistry (BASCD) guidance on sampling for surveys of child dental health. A BASCD coordinated dental epidemiology programme quality standard. Community Dent Health 1997b; 14 (Supplement 1): 10–17.
Pitts N B, Evans D J, Pine C M . British Association for the Study of Community Dentistry (BASCD) diagnostic criteria for caries prevalence surveys – 1996/97. Community Dent Health 1997; 14 (Supplement 1): 6–9.
Monaghan N, Morgan M Z . Do parents of children with caries choose to opt-out of positive consent dental surveys? Br Dent J 2011; 210: E1.
Office for National Statistics. Painting pictures of place series – topic profiles. A profile of Child Poverty, September 2010.
Institute for Fiscal Studies. Child poverty in Britain: recent trends and future prospects. IFS Working Paper W15/07. Robert Joyce, 2014.
Office for National Statistics, CT0626 – Sex by age by ethnic group. Source: 2011 Census 2016.
Office for National Statistics. Nomis – official labour market statistics. ST101 – Sex and age by ethnic group. Available from: https://www.nomisweb.co.uk/ (accessed October 2016).
Public Health England, National Diet and Nutrition Survey. Results from Years 1, 2, 3 and 4 (combined) of the Rolling Programme (2008/2009–2011/2012). 2014. Gateway number: 2014051.
Public Health England, National Diet and Nutrition Survey Results from Years 5 and 6 (combined) of the Rolling Programme (2012/2013–2013/2014). 2016 Gateway number: 206248.
Department of Health with BASCD. Delivering better oral health – an evidence-based toolkit for prevention. London, 2007. Gateway Ref. 8504.
Department of Health with BASCD Delivering better oral health – an evidence-based toolkit for prevention. 2nd edition. London, 2009.
Public Health England. Delivering better oral health: an evidence-based toolkit for prevention. 3rd edition. 2014. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/605266/Delivering_better_oral_health.pdf (accessed August 2017).
Davies G M, Worthington H V, Ellwod R P, Blinkhorn A S, Taylor G O, Davies R M . A randomised controlled trial of the effectiveness of providing free fluoride toothpaste during pre-school years on reducing caries in 5–6 year old children. Community Dent Health 2002; 19: 131–136.
Marinho V C C, Higgins J P T, Logan S, Sheiham A . Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2003; CD002278.
Chestnutt I G, Schafer F, Jacobson A P, Stephen K W . The influence of tooth brushing frequency and post-brushing rinsing on caries experience in a caries clinical trial. Community Dent Oral Epidemiol 1998; 26: 406–411.
Chesters R K, Huntington E, Burchell C K, Stephen K W . Effect of oral care habits on caries levels in adolescents. Caries Res 1992; 26: 299–304.
Silness, J, Loe H . Periodontal disease in pregnancy. II Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 1964; 22: 121–135.
Marinho V C C, Worthington H V, Walsh T, Clarkson J E . Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2013; CD002279.
NHS Business Services Authority. Fluoride varnish applications recorded on FP17s for children. Ad hoc analysis (2016).
NHS Digital. NHS Dental Statistics for England 2014/15. Annex 2. Published 20 August 2015. Available at: https://digital.nhs.uk/catalogue/PUB18129 (accessed 16 August 2017).
NHS Digital. Child Dental Health Survey 2013, England, Wales and Northern Ireland [NS]. 2015. Available at: http://content.digital.nhs.uk/catalogue/PUB17137 (accessed December 2016).
Welsh Oral Health Information Unit. Picture of oral health 2016. Dental Epidemiological Survey of 5 year olds 2014/15. Available at: http://www.cardiff.ac.uk/__data/assets/pdf_file/0006/218589/Picture-of-Oral-Health-2016.pdf (accessed December 2016).
Acknowledgements
The authors acknowledge the considerable efforts of the fieldwork teams in collecting the data for the national surveys and the commissioners who support them. They also acknowledge the assistance given by NHS Digital, PHE Diet and obesity team, and other external partners, including those from industry, who have assisted with provision of information used in this investigation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Davies, G., Neville, J., Jones, K. et al. Why are caries levels reducing in five-year-olds in England?. Br Dent J 223, 515–519 (2017). https://doi.org/10.1038/sj.bdj.2017.836
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.836
This article is cited by
-
Caries prevalence and caries experience (ICDAS II criteria) of 5-, 12- and 15-year-old Greek children in relation to socio-demographic risk indicators. Trends at the national level in a period of a decade
European Archives of Paediatric Dentistry (2021)
-
A rapid review of variation in the use of dental general anaesthetics in children
British Dental Journal (2020)