Key Points
-
Highlights a shift in practice from traditional concepts of practice to MI.
-
Suggests that a coherent approach to planning organisational change in practice is required.
-
Provides suggestion of an overall planning process in practice.
Abstract
Minimum intervention dentistry (MID) is the evidence-based delivery of oral healthcare which aims to maximise preservation of tooth structure and longevity of tooth life, improving long-term oral health and wellbeing. In general dental practice implementing such an ethos and approach can require change in the practice structure and processes. Such change in processes requires careful management and planning. Planning should include financial as well as business planning. A detailed understanding of the planning that may be required is described here as a guide to help oral healthcare practice staff and other stakeholders to facilitate the delivery of MID.
Similar content being viewed by others
Introduction
Minimum intervention dentistry (MID) is the contemporary response to the traditional, surgical operative approach to managing dental caries based on the operative concepts of G. V. Black more than a century ago. MID is a philosophy that attempts to ensure that teeth are kept functional for life. This term is not restricted to the management of dental caries but is also applicable to other aspects of oral health including periodontology, toothwear, endodontics, oral rehabilitation and oral surgery.1
The MID approach to the management of caries has evolved and continues to do so through improved understanding of disease processes, the biological healing ability of the oral tissues and their environment, and the rapid development in the last two decades of dental bio-active and bio-interactive materials. Such improvements in knowledge help us to better utilise patient risk/susceptibility assessments, focus on early prevention and control, minimally invasive restoration of irreversible cavitated lesions in a biologically favourable way, and better monitoring of the patient and any adopted behavioural changes.
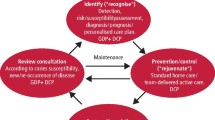
In practice this involves moving the focus away from the surgical restoration of teeth allowing the clinician and patient to achieve optimal disease control by employing the four core principles of MID. These are: (a) Detection – early identification and assessment of potential caries risk factors through anamnesis, lifestyle analysis, clinical examination and diagnostic tests; (b) Prevention/control – to eliminate or minimise disease risk factors by helping to alter lifestyle behaviour and professional preventive interventions; (c) Minimally invasive (MI) restoration – when cavitation is present and operative intervention is required, selective MI caries removal and restoration carried out to maximise the repair potential of the tooth and preserve tooth structure and pulp sensibility; and (d) Recall – with patient-focused/appropriate intervals, monitoring to maintain oral health where treatment and patient behavioural adherence outcomes can be reviewed.2,3,4
This contemporary approach to the delivery of oral healthcare brings opportunity for change to care delivery, and therefore general dental practices, or perhaps more appropriately termed 'oral healthcare centres', need to reflect this in their logistical and business planning.
Business planning
Angela Hatton, in her book “The Definitive Guide to Marketing Planning” outlines a hierarchy of plans that businesses may find useful.5 The size of organisation will determine how formalised and detailed each of these individual plans is, but even in a one-person business (practice) it should be possible to identify and plan at each level.
From this hierarchy, the functional or operational level plans of finance, marketing, human resources and operations flow from the core business plan. These functional plans themselves lead to tactical level plans, like a procurement plan for finance, a communications plan for marketing, personal development plans within the human resources group and a patient journey plan within operations. In this paper, the above planning hierarchy is used to discuss the needs to address these and implications for a modern MI-based oral healthcare practice.
Vision and mission within the business plan
The strategic intent/vision refers to the aspirations of the organisation (the oral healthcare practice) rather than purely its current activity. It defines a long-term drive for improvement that is essential to long term success. It provides a model that helps break the mould, moving the oral healthcare practice away from simply doing the same things a bit better and working a bit harder than the year before. It has the capability to elevate and extend the oral healthcare team, helping it reach levels it might not otherwise attain.6
Vision (strategic intent) combines a dream that energises the practice and a motivational aid, which implies 'stretch' where the practice looks for new opportunities rather than relying on existing custom. It gives a sense of discovery, a sense of direction and coherence to all the models.7
The shift from traditional dentistry to MID brings significant change in both ethos and methodology. Encapsulating this within the entire business planning process is essential. Core values of the practice and the overriding reasons as to why it operates need to be agreed explicitly and clarified.8 In reality, this and further discussions can lead to a period of adjustment manifesting in a 'stormy' phase in the process.9 At this level as elsewhere in healthcare, service redesign will benefit from good leadership, often provided by the lead clinician or a suitably appointed manager.10
Human resources planning
There is perhaps an implicit assumption in discussions of internal marketing, that effective use of inwardly directed marketing techniques can solve all employee-related quality issues and all customer satisfaction problems. Where the personnel and the services they perform form a large part of the 'offering', then human resources management (HRM) needs to be as closely involved as marketing. In particular, the recruitment, training, and rewarding of team staff (by salary and incentive), along with their motivational aspirations, constitutes an essential element in the successful delivery of MID.11
For a successful transition from operational focus and methodology to MID, the practice will need to operate, successfully, as a team, with clear goals. This is where strong human resource planning is required. The best way for a team to achieve its goals is for the team to be structured logically around those goals. Individual team members need to have clear roles and accountabilities. They need to have a clear understanding, not only of what their individual role is, but also what the roles and accountabilities of other team members are. During times of change, when typically pressure and priorities can push people into a silo mentality, and away from the team, the team operating process can act like a lubricant, enabling healthy team functioning to continue.12
Team structure and development
For an oral healthcare practice to effectively reach its objectives, it can, and often will, require the collaboration and support of all stakeholders. These include practice staff, patients, and higher-level management. Inadequate support and poor collaboration can, especially in a minimum intervention practice, lead to ineffective team working, and practice strategies and objectives not being met. Not all internal conflict should be thought of as damaging, as some, if managed well, may actually help to improve services.13
In the United Kingdom, dentists and dental care professionals (dental nurses, dental technicians, dental hygienists/therapists, orthodontic therapists, and clinical dental technicians) have to be registered with the General Dental Council (GDC). In 2013 the GDC made a significant change to the ways that dental care professionals can see patients. It removed the barrier to direct access for some DCPs. Under direct access (excluding NHS care at present) dental care professionals can now treat patients directly without the need for this to be prescribed by a dentist. The scope of practice for each member of the oral healthcare team is detailed in the document published by the GDC entitled Scope of practice.14 This document is available on the General Dental Council website www.gdc-uk.org.
This enables better use of the oral healthcare team to provide the holistic approach to dental care that supports provision of MID. For example, now a dental therapist can be utilised to deliver minimally invasive restorations when required, and an extended duties dental nurse (EDDN) can provide oral health education. In the UK, the Department of Health (DoH) has made available the document showing the evidence basis for preventive care that a dental practice would be expected to provide.15 However, the use of team members with differing skill sets will require good collaboration, including delegation, accepted referral pathways, and central to this will be good patient care planning. Some examples of how a dental nurse with extended duties can be utilised in an MID practice can be seen in Box 1.
In the NHS, direct access is limited and as such oral healthcare practices will need to inform patients that their care is being provided under the direction of a dentist.16 DCPs may be able to change the detail but not the direction of a care plan.
Financial planning
Since April 2006, UK NHS dentists have been paid according to how many 'Units of Dental Activity' (UDA) they carry out in a year. The monetary value assigned to a UDA varies across the country (usually between £15 and £28) and generally historical activity has been used to derive the actual cash value of a UDA.
Routine courses of treatment fall into three bands attracting differing number of UDAs. This is shown in Table 1. A brief description of items of treatment is included, and it also showing accredited UDAs.
Working within the current UDA system does in theory allow for prevention. The level of preventive care that is actually feasible to provide under such a UDA system has been rightly questioned.18
This level is not monitored longitudinally and the system does not recognise when it happens. More pragmatic research and modelling is required in NHS practice to explore what elements of MID can realistically be provided at a sustainable level. Practices need to financially model the system that they will use to provide MI preventive care. In NHS practice this may be facilitated by the redesigning of associate dentist remuneration systems to allow funding for DCPs and better use of the workforce skill-mix. Also this can include the provision of some interventions on an independent basis with agreement and consent of the patient. In independent practice the correct setting of fee levels (fee per item and/or monthly dental plans) is critical.
Under the proposed prototype contracts being evaluated by the DoH at the time of writing this paper, dentists are given a capitation fee for their patient, which may allow budgets to be set for some prevention through the work of an extended duties dental nurse, a dental therapist, or even a GDP for the more complex oral hygiene patients. This framework may enable dentists to project NHS related revenue income streams, but in practices where there is both NHS and private dentistry being carried out, the various revenue streams from private treatments will also need to be identified and forecast.
It is important to make the forecasts in the financial plan as realistic and practical as possible. It would be beneficial to identify if the business model is unsustainable at the planning stage rather than some time after implementation. The mental anguish and financial problems that can be caused by a struggling business can be very significant.19 A useful monitoring tool is cash flow data collection and analytics. This monitors three vital variable datasets. Profit (or loss) is monitored monthly through a profit and loss account, how much the business owes, or is owed, checked by keeping up to date creditor and debtor records, and cash availability in the business being monitored through a cash flow forecast. There is often a lack of understanding about cash flow. It is important that the relevant lead individual in the team masters the essentials of cash flow (including good management of debtors and creditors, short term finance and other knowledge). It should be borne in mind that the practice accountant may not be able to provide this on-going information or even be responsible for such data.20
Expenditure is the other area that needs to be monitored and controlled carefully. There are four main expenses in an oral healthcare business. Crucially, the responsible person, eg, CEO, finance manager, would not only know these numbers at all times, but need to keep them in line with the organisation's financial standards. An example of a financial framework for dental practices is suggested in Table 2, but this cannot be taken as a definitive guide.
It is suggested that staff expenses ideally be kept to no more than 20–25% of the total expenses incurred by the practice. Increasing staff production may keep percentages down in this area. Laboratory costs possibly kept to a maximum of 10%. Supply expenses should be monitored closely and a practice may decide to set them at 5% of total expenses. Finally, overheads could try to be contained to 5% if possible, unless they might be thought of as part of a practice marketing plan. An operative principle would keep these within set ranges, to ensure entire expenditure within the parameters necessary to keep costs at, for example, 50% overall.10,21
The above cost base example may be proposed for a MID-oriented practice. However, the emphasis on disbursement of the remaining 50% of revenue, which typically includes all the associate dentist costs and may allow a 15–20% net margin, could see a shift towards preventative measures, such as increased use of EDDNs, therapists and oral healthcare marketing. The key is in understanding the potential growth of the practice's revenue – from all sources. For example, by improving the oral health of patients, fewer restorations should be required in the medium to long term. Improved oral health and the time spent with individual patients, and the frequency of their visits, should reduce over time, but might be increased at the outset. Working more effectively and efficiently in this way enables a practice not only to maintain revenues, but to actively grow them. A practice may see an increasing of independent revenue by clinicians being able to spend more time explaining and offering services not available under an NHS contract. Revenues will increase due to a better understanding of patient desires.
An additional income stream can be derived from oral hygiene product sales. As part of the holistic approach, therapists and EDDNs can play an active role in this revenue generation. All the above should be planned to ensure staff remuneration and productivity is sustainable, socially responsible, ethical and will maintain practice growth.
Integrating new technology and materials
MID is greatly enhanced by the use of modern interventions that improve detection, prevention and restoration elements of the MID cycle. However, their costs needs to justified in the financial planning and team members need to understand the benefits and pitfalls of their use. Here, good research understanding is beneficial, and this can be disseminated by in-practice training and courses.
Marketing planning
Organisations such as dental practices can benefit in communicating and collaborating with other organisations including suppliers, commissioners, and patients/public groups. This can optimise acquirement of materials, organisation of services, and engagement of stakeholders, to help ensure delivery of services is more efficient and responsive. In the real world consumers (including individuals) are free to choose among the many hundreds and thousands of product and service offerings and in dentistry can exercise this choice by moving from one practice to another.22 In business language this adequately describes outward facing marketing communications. However, since the mid-1970s the concept of internal marketing has been proposed as a way of achieving consistent service quality – a major problem in the services area, where of course, dentistry sits. Its basic premise was that 'to have satisfied patients, the practice must also have satisfied employees', that is, by applying the principles of marketing to job design and employee motivation.
There are two significant marketing considerations if the practice emphasis moves to MID. Firstly, education and secondly retention. Externally, a regularly delivered programme of patient facing oral healthcare messages will help to reinforce regular and more acceptable visits to the dentist as individual patient oral healthcare improves. As well as educating, this regular communication gives a platform to maintain patient retention and build loyalty, through satisfaction.
Satisfied patients (customers) are the best advertisement for any business and are more likely to introduce new patients (customers) to the practice through word of mouth and through social media interaction. Satisfied patients (customers) are often willing to pay premium prices to a supplier they know, like and trust. Retaining customers makes gaining market entry or share difficult for competitors.20
The oral healthcare practice industry is not entirely exempt from the pressures of a competitive retail service sector. Internally, regular communication is also paramount. There is a culture change occurring in transitioning from traditional operative-based dentistry to MID. Employees constitute an internal market and in that sense need to be communicated with just as much as external stakeholders, through effective marketing communications. Marketing communications should be used to differentiate, remind/reassure, inform and persuade employees just as much as any patient/customer, target segment.23
Explanations/education about changes in the patient journey, the increased focus on prevention and control, the emphasis on 'self-help' and the decreasing frequency of visits to the practice (possibly a two-year cycle), will need to be delivered as often by dental receptionists, dental nurses, hygienists and therapists, as by the GDPs themselves. One consistent and integrated message, delivered and understood internally, and successfully relayed to the patient base in the form of one-to-one, and one-to-many communications is required.
Patient communication
Effective communication and discussion helps patients understand any proposed treatment. It is imperative to take the patient along the decision-making process that affects them and ensure that valid consent is achieved. This way they also perceive ownership of the care they are receiving. The use of intraoral photography can assist greatly in this process with immediate and direct feedback of patient findings during examinations. It is important for all clinicians to be able to take and record any images required with suitable consent having been granted. Both intraoral cameras and digital single lens reflex cameras (DSLR) can be helpful. It's helpful to have these available and easily accessible for each clinician.
Patient and public involvement
There are a variety of research methods to gain feedback from patients (including parents of children) and the following list can be used to do this with some rigor:
-
Suggestion boxes
-
1-to-1 feedback
-
Postal surveys
-
Online survey (via various online providers)
-
Consensus making activities
-
Patient forums/focus groups.
The information gained here can be used in several ways to market and involve patients in their MI services. Some examples include:
-
Help in designing practice literature
-
Engaging local media
-
Helping with CQC compliance
-
Helping the practice direct services including research priorities.
Operational planning
A move to MID may well require changes to an established patient journey, and the sequence of patient and practice staff contacts may alter to ensure delivery of MID care. For example, the first point of contact may be a patient coordinator explaining the change in MI methodology to a patient, helping them to understand their own oral health and take more responsibility for it. This would not constitute a diagnosis and care planning appointment, but would be an informative session for the patient to understand a traffic light system, dento-legal risk transfer, and to understand that they, together with the oral healthcare team, will now work to improve and maintain long-term health and wellbeing.
The utilisation of the wider dental practice team can be beneficial and certainly help facilitate the delivery of MID. There is a real agenda to remove patients' reliance on the dentist, encouraging, if not demanding, that the patient is responsible for their oral health. This focus starts the prevention-based MID journey, and educating patients about the self-improvement of their own oral healthcare is key to the MID philosophy. Increased exposure to a wider dental team including EDDNs, hygienists and therapists all reinforcing healthcare messages can play a vitally important role in the delivery of this approach to management. Using a broader workforce skill-mix may well produce conflicts in the financial re-organisation of a practice and as highlighted previously will need robust business modelling. Such a model will need to be re-assessed and analysed regularly, as it will have implications on the traditional associate performer remuneration model. For example, an organisation may choose to top slice its budget and reserve this for the provision of dental therapist services. It would then need to factor in changes to the associate dentist remuneration, which would hopefully allow associates time to feel less rushed, develop their interests, increase quality of working life, and result in better clinical care pathways for the patient.
Conclusions
Business planning is a multi-faceted discipline. When the planning process is being driven by organisational change particular attention has to be paid to the core drivers of the business in order to deliver a successful outcome. MID is the way forward. It will benefit the practices and patients that become early adopters, but the need for intelligent business planning is unquestionable.
References
Frencken J E, Peters M C, Manton D J, Leal S C, Gordan V V, Eden E . Minimal intervention dentistry for managing dental caries – a review: report of a FDI task group. Int Dent J 2012; 62: 223–243.
Walsh L J, Brostek A M . Minimum intervention dentistry principles and objectives. Aust Dent J 2013; 58 Suppl 1: 3–16.
Domejean-Orliaguet S, Banerjee A, Gaucher C et al. Minimum Intervention treatment Plan (MITP) –practical implementation in general dental practice. J Minim Interv Dent 2009.
Banerjee A, Domejean S . The contemporary approach to tooth preservation: minimum intervention (MI) caries management in general practice. Prim Dent J 2013; 2: 30–37.
Hatton A . The Definitive Guide to Marketing Planning. London: Pearson Education Limited, 2000.
Aaker D . Developing Business Strategies. Sixth Edition. Wiley, 2001.
Hamel G, Prahalad C K . Strategic Intent. Harvard Business Rev 1989: 67: 63–76.
Sinek S . Start With Why. Penguin Random House, 2009.
businessballs.com. tuckman forming storming norming performing model. Bruce Tuckmans 1965 Model. Available at http://www.businessballs.com/tuckmanformingstormingnormingperforming.htm (accessed July 2017).
NHS Leadership Academy. Clinical Leadership Competency Framework. 2011. Available at http://www.leadershipacademy.nhs.uk/wp-content/uploads/2012/11/NHSLeadership-Leadership-Framework-Clinical-Leadership-Competency-Framework-CLCF.pdf (accessed November 2016).
Ahmed P K, Rafiq M . Internal Marketing, Tools and Concepts for Customer Focused Management. Oxford: Butterworth – Heinemann, 2002.
Cameron, E, Green, M . Making sense of change management: a complete guide to the models, tools and techniques of organizational change. London: Kogan Page Limited, 2004.
MindTools. Resolving Team Conflicts. Available at https://www.mindtools.com/pages/article/newTMM_79.htm (Accessed November 2016).
GDC. Scope of Practice. 2013. Available at https://www.gdc-uk.org/api/files/Scope%20of%20Practice%20September%202013.pdf (accessed November 2016).
Public Health England. Delivering better oral health: an evidence-based toolkit for prevention. Third Edition. Department of Health. Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/605266/Delivering_better_oral_health.pdf (accessed November 2016).
NHS National Workforce Projects. Dental Workforce Resource Pack. Available at https://www.pcc-cic.org.uk/sites/default/files/articles/attachments/dental_workforce_resource_packnational_workforce_projectsaug_07.pdf (accessed November 2016).
Perryer, G . Units of Dental Activity. University of Birmingham. http://www.mecourse.com/ecourse/pages/page.asp?pid=1375 (accessed October 2016).
Page J, Weld J A, Kidd E A . Caries control in health service practice. Br Dent J 2010; 208: 449–450.
Williams S . Small Business Guide. London: Vitesse Media Group, 2002.
Ulhaner L . The Growing Business Handbook: Inspiration and advice from successful entrepreneurs and fast growing UK companies. Twelfth Edition. London: Kogan Page Limited, 2010.
Runkle K . The Business of Dentistry. 2011. Available at http://www.dentaleconomics.com/articles/print/volume-101/issue-1/features/the-business-of-dentistry.html (accessed October 2016).
Fill C . Marketing Communications Contexts, Strategies and Applications. Second edition. London: Pearson Education Limited, 2002.
Fill C, Yeshin T . Integrated Marketing Communications. Oxford: Butterworth – Heinemann, 2001.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Dawett, B., Atkins, B. & Banerjee, A. A guide to building 'MI' oral healthcare practice. Br Dent J 223, 223–227 (2017). https://doi.org/10.1038/sj.bdj.2017.673
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.673
This article is cited by
-
Top tips for minimally invasive dentistry in primary care
British Dental Journal (2023)
-
A scoping literature review on minimum intervention dentistry for children with dental caries
British Dental Journal (2022)
-
Dental Policy Lab 1 - towards a cavity-free future
British Dental Journal (2021)