Key Points
-
Discusses protection of root surfaces in older patients.
-
Suggests that a maximum interception approach means that specific efforts are needed to profile salivary, plaque and lifestyle risk factors.
-
Discusses the best ways to make the dentition able to be easily maintained.
-
Highlights how important it is to engage with other members of the health care team in oral health planning.
Abstract
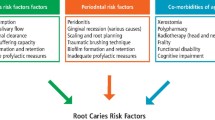
With an aging population, dentists need to be aware of the risks which come to their elderly patients from retained teeth and exposed root surfaces. Oral health problems in the later years of life are multifactorial, with lifestyle, plaque and salivary factors remaining paramount. Root surface caries is likely to present a challenge in patients with a strong history of past coronal caries (and who have the attendant lifestyle risk factors) as well as in elderly patients who suddenly develop salivary hypofunction. Following a maximum interception approach means that specific efforts are needed to profile salivary, plaque and lifestyle risk factors and ensure that the dentition can be cleaned by the patient and maintained in a way which gives comfort and function as well as aesthetics. Discussions around long-term objectives for oral health are important when there is a sudden decline in general health in the later years of life. It may be appropriate to use tooth surface protection for strategic anterior teeth and apply the shortened dental arch concept where patients cannot readily maintain their own oral health because of frailty or medical conditions. Glass ionomer materials can be used both for root surface protection and for conservative restoration where a minimally invasive preparation has been undertaken. In other cases, arrest of lesions using silver fluoride or CPP-ACP topical treatments can delay or obviate the need for restorative interventions, and forms part of the management of patients in high care units in nursing homes. Involving all members of the healthcare team in supporting oral health is an important strategy to ensure that oral health issues are not overlooked. The challenge is to promote evidence-based self-care. A key message is to promote oral health as part of overall health.
Similar content being viewed by others
Introduction
The modern clinical approach to caring for medically frail and elderly patients relies on using both maximum interception of existing oral disease and its causative factors, as well as minimum invasion of the patient's oral tissues. More emphasis on the former will result in less need for irreversible treatments. A key message for modern dental practice is that the demographics of population shifts in the UK and in other developed countries requires a proactive approach to the 'silver tsunami' of elderly patients who are progressively becoming a greater proportion of the total population. It has been estimated that by 2050, the number of people 65 years of age and older across the globe will reach 1.5 billion. Because this ageing population will be affected by chronic diseases, including diabetes mellitus, cardiovascular disease and dementia, the dental profession must prepare for the silver tsunami of older adults who have retained natural teeth but have more chronic diseases, are living longer and are medically more complex.1
With patients of advanced age retaining more teeth, this provides more at risk sites for dental caries, non-carious loss of tooth structure, and periodontitis. Many 'baby boomers' born between 1946 and 1964 will enter their older years with natural teeth (some of which may be heavily restored), and both their unfilled and filled teeth will be at risk of both coronal caries and root surface caries. As this situation has been documented in most developed countries as well as in developing countries,2,3,4,5,6,7,8 the solutions and approaches used elsewhere can often have merit for local application, rather than attempting to re-invent the proverbial wheel.
We as dentists need to be tuned into the range of functional, behavioural and situational factors that impact our elderly patients, lest they fall into a cycle of dental neglect and worsening oral disease.9 The systems and strategies we use need to work for public as well as private patients, whether living in the community, homebound, or residing in a nursing home or other long-term care facility. They also need to be both practicable and financially sustainable.10
The realisation that older patients pose particular challenges as they transition through the later phases of life drives a thought process which includes considerations around the types of treatments which are appropriate, and how the patient will be able to maintain oral health at a time when their general health may decline suddenly. Greater attention must be placed on healthy or successful ageing so that the quality of life of older adults across the spectrum can be improved, and transitions to frailty reduced.11 This principle of focussing on health rather than disease must be applied when considering changes in oral health that are likely to occur in the later years of the lifespan. At the extremes of the lifespan, a shift from 'cure-seeking care' focusing on disease treatment to 'cure and support-seeking care' is appropriate, including rethinking of how treatments can maximise the quality of life for the patient and make them comfortable and pain-free.12
This paper explains the rationale and application of the minimum intervention (MI) philosophy to elderly patients, and emphasises ways in which general dental practitioners can support their patients through the later phases of life. It builds on the modern principles of MI dentistry,13 but adapts these to the special challenges of the older patient. A recurring theme is that to achieve the best outcomes involves using the whole dental team as well as the general health team.14
Protection of tooth surfaces
While the benefits of community water fluoridation on coronal caries are well established and can still be seen when fluoridation is introduced into contemporary populations,15 many elderly patients are unaware that lifelong exposure to optimally fluoridated water leads to the accumulation of fluoride in root surfaces and in reductions in the incidence of root caries of between 30 and 75%.16 This good news must, however, be tempered with the knowledge that despite this benefit, the same dietary and lifestyle factors that have led to epidemic levels of obesity and type 2 diabetes in older patient cohorts will also drive up caries incidence.17,18,19,20,21
When root surfaces become exposed because of the accumulated attachment loss from periodontitis or gingival recession (particularly in patients with a thick biotype), a range of problems can arise, including dentinal hypersensitivity, and non-carious tooth structure loss from combinations of abrasion and erosion (Fig. 1). The major concern for most elderly patients is however dental caries. Elderly patients with exposed roots are prone to carious attack of both crowns and exposed roots; indeed a strong history of coronal caries is a powerful predictor of root surface caries.22,23 The attack rate for root surface caries of an exposed root surface varies according to the tooth surface, with mandibular molar teeth being the most frequently involved, on their buccal and approximal surfaces, followed by the buccal surfaces of mandibular premolars. For incisor teeth, attack rates are higher on approximal surfaces than on the labial surface, a feature which results in lesions which start interdentally eventually wrapping around the tooth in a circumferential pattern.16 Mandibular incisor teeth have low attack rates for root surface caries because they normally have continuous exposure to resting salivary secretions. When a patient develops root surface caries on the lingual aspects of their mandibular incisor teeth, this indicates there has been marked depression of the normal salivary defences against mineral loss.24
A, Patient with prolonged xerostomia showing root surface caries developing on lingual surfaces of mandibular incisors. B, Patient with a thin biotype who is prone to root surface exposure from recession. There is tooth surface loss from erosion and abrasion. A strategy for root surface protection is essential. C, Patient with root caries whose glass ionomer restorations have begun to dissolve two years after placement because of sustained acidic oral pH at rest. The patient had not been using sodium bicarbonate mouth rinses to elevate salivary pH as instructed. D, Buccal surfaces of lower molars are the most at risk surface for root surface caries. This recently placed crown should have been fluted on the buccal aspect to aid oral hygiene of this area. E, Incipient caries with conservative excavation. F, Same case as E now restored with Fuji VII which will protect adjacent tooth structure by release of ions. Photographs E and F courtesy of Dr Andrew Brostek. G, Patient with autoimmune salivary gland disease with erosion of tooth structure and of GIC restorations. H and I, Exposed roots of overdenture abutments protected by placing CPP-ACP with fluoride (MI Paste Plus) into the overdenture each day. J, An early lesion in the aesthetic zone which is amenable to caries arrest by using high fluoride dentifrices and CPP-ACP products. K, Composite resin restorations with recurrent caries on coronal and root aspects because of failure to address causal factors. This is the same case as shown in C prior to restoration of root caries with glass-ionomer cement restorations. L, Extensive caries has destroyed the abutment teeth beneath an overdenture. The patient was not complaint at using CPP-ACP with fluoride inside the overdenture each day as instructed. M and N, Before and after images of a patient with primary Sjögren's syndrome with severe xerostomia and gastric reflux taken 6 years apart. Her daily preventive regimen includes use of topical CPP-ACP crème (GC Tooth Mousse) used in conjunction with a triclosan fluoride dentifrice
Prevention of root caries relies on a multifaceted approach involving: (1) methods to protect roots from exposure; (2) protection of roots once they become exposed to the oral environment by using various coating materials; and (3) the application of fluorides, CPP-ACP, and other materials to roots to make them more resistant to dental caries.26,27,28,29,30,31,32,33,34,35,36,37,38 An example of the combination approach is shown in panels M and N in Figure 1. This patient with primary Sjogren's syndrome has a low pH oral environment from her underlying salivary gland disease, and this problem is worsened by chronic gastric reflux. The patient suffers from non-carious tooth structure loss, root surface caries and periodontitis. Debridement of the roots during periodontal treatment will remove the fluoride-rich outer layer and increase the risk of both erosion and root surface caries. To help protect and preserve the dentition, the patient was provided with a triclosan fluoride dentifrice and CPP-ACP topical crème (GC Tooth Mousse). After periodontal treatment using closed debridement, her restorative treatment was undertaken, involving two labial adhesive restorations placed into erosive defects (32 and 41), and incisal restorations into non-carious defects in 3142 to prevent further breakdown. The situation after treatment has remained stable over 6 years from the multiple standpoints of periodontal status, non-carious tooth structure loss and caries activity. There has been no recurrent caries, and the incipient root surface caries lesions on the 42 and 43 have not progressed, despite the challenge created by the low pH oral environment. The patient is now 71 years of age and has an intact and stable dentition.
Because bacteria can penetrate readily through the thin cementum on a root surface into the underlying dentine,39 a logical strategy to protect exposed root surfaces is to apply a thin layer of a flowable glass-ionomer cement (GIC) onto them, as a form of tooth surface protection. While the concept of protecting pits and fissures of posterior teeth using resin or glass ionomer sealants is well established as a highly cost effective measure in moderate and high caries risk children and as an effective dental public health intervention at the community level, the notion of protection of exposed root surfaces using GIC in this manner in elderly patients has yet to attract great attention, despite its obvious clinical application.
Glass-ionomer cements through their fluoride release and subsequent recharging are the mainstay of current concepts for root surface protection. High fluoride releasing forms of such cements have been developed with enhanced fluoride exchange capabilities.40 Versions of such cements which incorporate active remineralisation technologies such as casein phosphopeptide amorphous calcium phosphate (CPP-ACP) have been available for several years.41
In a recent study, the ability of a high fluoride release tooth surface protection material (GC Fuji VII) and the same material with CPP-ACP (GC Fuji VII EP) were compared to three low viscosity resin sealants in terms of their ability to protect tooth surfaces. Under a sustained lactic acid challenge, all the resin materials protected the surfaces which were covered, although lesions developed at the periphery of the sealed surface. In contrast, with both the GIC materials there was protection of the covered tooth surface as well as the peripheral millimetre beyond the area covered. The 'halo' effect was attributed to the release of ions from the material.43
Applying such glass ionomer materials in a thin layer onto exposed roots provides another practical benefit when the standard of the patient's oral hygiene declines, eg due to impaired dexterity from arthritis or after a stroke. A tooth surface protection material is a physical barrier between the tooth surface and the overlying dental plaque biofilm, and in the case of GIC when there is a strong and sustained acid challenge the material rather than the tooth surface will dissolve slowly. While rates of dissolution of GIC materials vary considerably, the progressive loss or washout of GIC is an important clinical sign of a low pH environment, which must then be addressed as a clinical issue, and remedied using neutralising agents.
Root caries arrest
In addition to its use to protect sound roots, GIC can also be applied in thin layers over incipient lesions of root surface caries which have an intact leathery surface spread over a broad front. Such lesions can harden over time as ions diffuse across the thin layer of GIC.39
There are other approaches which can also be used to arrest early lesions of root surface caries so that cavitation does not occur. Key factors in deciding which approach to follow are the quality of the patient's saliva as a source of ions for remineralisation, and the degree of access for plaque removal. For lesions where plaque control is challenging, covering the incipient lesion with a thin layer of GIC is an appropriate strategy, whereas where the lesion is accessible, stimulating salivary flow (eg, with sugar-free chewing gum) or enhancing the remineralising capabilities of saliva is feasible. Topical application of CPP-ACP crèmes such as GC Tooth Mousse can arrest non-cavitated root surface caries lesions even in patients with compromised salivary parameters (Fig. 1, M and N).32,44
When following a root caries arrest approach, it is important to avoid damaging the surface by forceful probing with a sharp probe. Using a blunt periodontal probe applied with light force is recommended to avoid creating small cavitations on the root surface. In addition, care must be taken when using colour as a guide to the progress or stability of early root surface caries lesions, since lesion colour is influenced strongly by bacterial metabolism (for example, production of pigments) as well as by the uptake or trapping of exogenous pigments from the diet into the outer porous surface.45
Arrest of lesions using ozone, silver fluoride or CPP-ACP topical treatments can delay or obviate the need for restorative interventions.44,45,46,47,48 Repeated application of silver fluoride or silver diamine fluoride can form an essential part of the minimally invasive management of both root surface and coronal caries in patients who are institutionalised in high care units in nursing homes. This can be a definitive caries arrest treatment or can be followed when required by delayed restoration.47,48 Protocols for the arrest of root and coronal caries may use silver fluoride alone or in combination with stannous fluoride or potassium iodide (for example, as in SDI Riva Star). Arrested root lesions can be maintained in the fully arrested state over long periods of time because the silver provides a long-term disinfectant action. The choice of technique determines whether or not there will be staining from the silver, and if so whether it is likely to pose an aesthetic concern for the patient. The topical application of silver fluoride is easy to perform and is painless for the patient, and allows the possibility of later restoration of the tooth (if needed) with GIC with minimal need for local anaesthesia using the atraumatic restorative technique.
The provision of dental treatment to elderly patients must be sensitive to their ability to tolerate 'on site' care, as well as their propensity to seek care. As patients become progressively more frail over time, decisions around whether restorations are in fact necessary for cavitated lesions must factor in the social and personal context of each patient. Those patients who are aggressive and oral defensive may tolerate a one-minute treatment with silver fluoride but not caries excavation.
Maintenance of oral hygiene
Tooth brushing followed by interdental cleaning is the standard methodology for removing plaque; however, in most patients substantial levels of dental plaque remain after mechanical plaque control. Indeed, a 2005 systematic review of 33 studies measuring the effectiveness of self-performed mechanical plaque removal in adults with gingivitis over 6 months concluded that in adults with gingivitis, the quality of self-performed mechanical plaque removal is not sufficiently effective.49 Many reasons for inadequate oral hygiene can be put forth, including suboptimal technique, inadequate frequency or duration, challenges of accessing hard-to-reach areas, poor compliance with professional instructions, and loss of individual motivation over time.50
With declining fine motor skills and reduced visual acuity in advanced age, many elderly patients struggle with manual tooth brushing, and may avoid interdental cleaning all together. This presents a major problem, as recurrent caries is a major contributor to failure of restorations. Moreover, poor oral hygiene in a patient who is susceptible to periodontitis will drive periodontal attachment loss around teeth as well as peri-implant inflammatory diseases. Maintaining high standards of oral hygiene is a challenge for healthy young adults whose motor skills and visual acuity are high, so the oral hygiene challenge for elderly patients is even greater when one considers the impact of missing or tilted teeth, recession, heavily restored teeth and the presence of partial dentures.
Considerable effort must also be directed to the effective cleaning of dentures, since it is common for patients to neglect those parts of partial dentures which come into contact with the teeth and soft tissues, leading to denture-related carious lesions and further periodontal destruction. In fact, wearing of partial dentures can lead to as much as a six-fold increase in the prevalence of root surface caries on the adjacent teeth.16 Disclosing dyes can be applied onto dentures when the patient is having oral hygiene instruction, so that areas which have been missed can be identified readily. The colours of combination dye products which show mature thick dental plaque in blue colours contrast well with pink coloured acrylic resin, making it easier to show the patient at the chairside the areas on their denture that more attention must be directed to.51 These products should be applied to the natural teeth once the prostheses have been removed from the mouth, so that advice on cleaning the teeth and the prostheses can be provided at the same appointment (Fig. 2).
A and B, C and D show before and after staining using GC TriPlaque ID™ gel, which shows acid producing mature plaque in light blue, mature plaque which is not producing acid after a sucrose challenge in dark blue, and thin young plaque less than 24 hours old in pink. Both these patients show extensive areas of cariogenic acid-producing plaque. E and F, Two different patients stained with a 2 tone dye (GC Plaque Check), with mature plaque stained in dark blue, and thin young plaque in pink. The teeth shown in panel F both have obvious cavitations which contain mature plaque. Photographs A–D courtesy of Carol Tran
For some patients the use of adjunctive devices such as powered brushes is highly beneficial to their plaque removal performance. There is support in the literature for the greater effectiveness of powered brushes over conventional manual toothbrushes. Likewise, there is evidence that the oscillation-rotation action of powered brushes can give superior plaque removal compared to a manual brush.52,53,54,55 Modern powered brushes include features such as force control, position sensing and timers, all of which can aid effective cleaning. The large handles of powered brushes are easier to hold than a conventional manual toothbrush. Thus, for elderly patients it is preferable to select a powered brush which uses a rotation-oscillation action to achieve the greatest reductions in plaque and gingivitis. Such powered brushes can be used every day as a normal part of an individual's oral hygiene routine, without concerns as to the potential for gingival recession and abrasion of tooth surfaces.
Because it can be expected that most elderly patients will struggle with interdental oral hygiene, some thought is required around aligning approaches for at-home care to the unique situation of the patient. Interdental brushes are the preferred approach for cleaning interdental spaces, with good supporting evidence for efficacy.56 They are preferred over dental floss for elderly patients. A systematic review of nine studies of interdental brushes used as an adjunct to brushing showed greater plaque removal, lower bleeding scores and reduced probing pocket depths. The majority of the studies showed better plaque removal for interdental brushes compared with floss.57 Once the approximal tooth surfaces have been cleaned, interdental brushes are a simple way to apply topical agents into the interdental spaces or into furcations.
For patients who struggle with interdental cleaning, the use of chemical plaque control agents such as essential oil mouthrinses (Listerine) or chlorhexidine can also be of benefit. For essential oil mouthrinses, one can expect that daily use should give worthwhile reductions in dental plaque and gingivitis.58,59,60
The selection of the appropriate dentifrice is a further consideration, taking into account the patient's caries risk when choosing the level of fluoride. Products with stabilised stannous fluoride are useful in older patients because they can slow the regrowth of dental plaque. Stannous fluoride exerts effects both on dental plaque and gingivitis, and is retained by plaque to give prolonged effects over time. Stabilised stannous fluoride dentifrices exert significant effects on dental plaque bacteria, giving a sustained reduction in the metabolic activity of dental plaque bacteria, and in plaque regrowth rates.61,62,63,64,65,66,67,68,69 Likewise, there is strong evidence supporting the use of a triclosan/copolymer/sodium fluoride combination in a dentifrice, both for caries prevention as well as for slowing the progression of periodontitis.71,72,73,74,75,76
The initial reduction of plaque bacteria from tooth brushing is caused by both physical disruption of plaque and the effects of detergents/surfactants on dental plaque bacteria.70 For this reason, patients should avoid using so-called 'natural' toothpastes which lack either fluoride or surfactants. It is also important to recognise that there are therapeutic effects which continue on after brushing, due to the subsequent slow release of ingredients that have bound to oral tissues or have been taken up by areas of the plaque biofilm that were not removed by brushing.77
Practitioners should take an evidence-based approach and choose dentifrice products for patients which meet their individual requirements.78 Appropriate advice to the patient on the selection of dentifrices can come from the dentist, dental hygienist or dental/oral health therapist, as part of clinical sessions focussed on oral hygiene. Certain aspects, such as tooth brushing techniques or oral health education, could also be carried out by appropriately trained dental chairside assistants, if permitted by local regulations. The front desk of the practice can add to these efforts by ensuring that patients are supplied with the correct products and are reminded to restock as required when attending for dental care. Front desk staff can also reinforce key oral health messages with patients. This is an opportunity that is often overlooked.
While powered toothbrushes and antibacterial dentifrices can both provide improvements in plaque control and oral health, practitioners should not rely only on one approach but rather should combine multiple home care measures; eg a powered brush with an antibacterial dentifrice and a post-brushing antibacterial mouth rinse. Following a multipronged attack can yield important benefits when the agents used have additive or synergistic effects.
Given that patients may not learn improved oral care techniques readily,79 the question then arises as to which methods of oral hygiene instruction are most effective? Based on more than 30 studies of at least 6 months duration, a single episode of oral hygiene instruction, describing the use of a mechanical toothbrush, in addition to a single professional 'oral prophylaxis' provided at baseline, is known to have a significant, albeit small, positive effect on the reduction of gingivitis.55
Nowadays there is a growing appreciation of the need to change methods of oral hygiene instruction to better reflect modern behavioural theory and thereby achieve greater outcomes. Motivational interviewing is an effective patient-centred method for enhancing intrinsic motivation to change by exploring and resolving ambivalence. Under this framework, direct persuasion is not seen as useful for resolving ambivalence, and indeed the patient is supported in identifying and resolving their own ambivalence about change. Motivation is elicited from the patient rather than imposed from without, and the patient's values and autonomy are respected. A 2009 systematic review of 32 studies showed that while traditional approaches to individual oral health education are largely ineffective, interventions based on motivational interviewing were the most effective method for altering health behaviours in a clinical setting.80 Such techniques should form the basis of chairside oral health promotion efforts with elderly patients. Often oral health therapists and dental hygienists have been trained formally in using such methods as part of their university education, so those skills should be utilised as part of the overall team approach. Where the dental team includes oral health therapists or dental hygienists, a concerted effort to enhance oral hygiene can be mounted using techniques such as motivational interviewing, as opposed to the traditional approach of telling the patient what to do and then demonstrating the correct technique. Oral hygiene needs reinforcement over time, as most patients cannot maintain good oral hygiene over prolonged periods.
The team concept
Effective maintenance of oral health in elderly patients requires dentists as the leaders of the oral health team to think outside the walls of the dental surgery, and find ways to establish multidisciplinary approaches so that doctors, nurses, and carers share in the responsibility for maintaining oral health.81 Applying this team concept is critical to identifying problems when elderly patients first enter long-term care facilities and are screened for oral diseases. Close collaboration with non-dental members of the health care team is important for planning not only clinical care provided by the dentist or dental hygienist, but how everyday oral hygiene is undertaken or provided.
Within the dental practice setting, a range of team members other than the dentist may be able to contribute to the overall care of elderly patients (Table 1). It is essential that the use of team members who are not dentists aligns with local regulatory controls on the scope of practice in terms of clinical procedures. Team members such as dental hygienists, oral health therapists and dental chairside assistants can only undertake those procedures for which they are legally qualified. This varies between countries as well as between individual practitioners according to the training they have undertaken.
Elderly patients who are medically frail and have high levels of dependency are best managed as much as possible on site where they live, so developing a partnership and strong relationships with aged care facilities is important for the dental practice. A preferred model of care may use dental hygienists or oral health therapists to drive a program which is focussed on prevention and early intervention.82 Protocols for oral care must be tailored to the patient's needs and be realistic given the limitations in time, finance and energy which can be expended. It is important that a close eye is kept on compliance and on how the patient's oral health is tracking over time, as the situation of an individual elderly patient can change rapidly after major health events such as a fall or a stroke.
The final and often most difficult part of any discussion around the team approach to oral hygiene for elderly patients is the vexed question of who should perform oral hygiene when the patient is unable to? It is often assumed by relatives that nurses or carers will undertake oral care as part of general body hygiene, but this is rarely the case, unless they have been specially trained to do this safely and effectively. Carers working in aged care facilities are often reluctant to provide oral care due to feelings of lack of knowledge and skills, and a lack of confidence regarding how to do this safely. These barriers add to a perception (which is true from a purely microbial point of view) that the mouth is both a 'dirty' place as well as being an intimate personal space.83 Consequently, many carers believe that patients should be looking after their own teeth and dentures.
When patients develop dementia, the problems of oral care can magnify because of passive resistance and aggression; for example, when patients refuse to open their mouth or have oral hygiene care undertaken by carers. Once a particular patient has been labelled as being 'difficult', staff may simply ignore orders for regular oral hygiene, which then only perpetuates and magnifies a cycle of oral neglect.
Oral health therapists and dental hygienists are trained to develop individualised oral health care plans for patients with different needs. During their university education, they may have had clinical placements in hospitals, nursing homes and long-term care facilities where they have had the opportunity to develop and implement programs to reduce oral diseases in elderly patients. Through these experiences, their skills at coping with the challenges of providing preventive oral care to patients with mild to moderate dementia will have been sharpened. They can pass on such skills to carers and nurses, serving as a dental hygiene champion and bringing a helpful face to the staff who work in long-term care facilities thereby making a positive impact by directly assisting and training carers and nursing staff in preventive practices.84
Control of lifestyle factors
In 1994, Aubrey Sheiham commented that: 'In future, dentists should do fewer restorations, but of higher quality, and offer more appropriate prevention. A central tenet of modern preventive dentistry is to avoid intervening before prevention has been given a chance to work'.85 In the context of the elderly patient, this means addressing risk factors for oral diseases, recognising that many of these factors are shared with the systemic diseases which are common in the same population cohort.
Assessing dental plaque, saliva and lifestyle risk factors for dental caries and other oral diseases is a platform of modern minimum intervention dentistry. In the elderly patient, issues around salivary flow are common, because of problems with hydration, xerostomic side effects of medicines, and systemic diseases. Xerostomia cannot be attributed only to the ageing process, thus when it is detected a careful history and examination is essential to determine whether it is a side-effect of disease or medicines the patient is taking.86 Because the frequency of chronic diseases increase with age, the prevalence of salivary function rises progressively in the later years, such that over 50% of patients aged 65years and above are likely to have issues with salivary parameters, particularly resting flow and resting pH.87,88 The impact of depressed salivary output on salivary pH and buffer capacity can be assessed and demonstrated to the patient (Fig. 3).
A, The patient has brought in her list of prescription medicines. These lists are often incorrect and overlook over the counter medicines which can contribute to dry mouth. In this particular medication list, xerostomic actions are known for venlafaxine, spironolactone, atenolol and fexofenadine. B, The threshold for normal stimulated saliva production is 0.7 mL/min, which corresponds to 3.5 mL of liquid after 5 minutes of chewing. Less than this is abnormal and requires further investigation. C, Assessment of salivary pH using the GC Saliva Check Buffer™ test kit, which comes with a colour guide showing the correlation of colour and pH. The pH paper for this kit follows a traffic light pattern, with dark green indicating alkaline pH, light green neutral pH, orange colours a pH from 6.0–6.6, pink a pH from 5.2 to 5.8, and red a pH of 5.0 and below. The pH test strip is placed into the sample of resting saliva for 10 seconds, and then the colour of the strip is read and compared with the supplied chart. In this case, the resting saliva is acidic (pH 5.8–6.0) but the patient has a normal pH for their stimulated saliva (pH 7.6). The buffer test has three concentrations of lactic acid as a challenge, and the sample has neutralized the low and moderate concentrations giving a green colour, indicating that the buffer capacity is high. This profile is readily amenable to change once lifestyle and medical factors are addressed. D, There was no resting saliva at all, the stimulated saliva is acidic (pH 6.0), and the buffer capacity is unusually low, with only partial neutralisation of two of the three lactic acid challenges. This profile indicates salivary gland damage or major saliva gland pathology. E, Association between colour and pH for measurement of resting and stimulated saliva
Taking a baseline measurement of salivary parameters is an important part of the initial assessment of oral health in an elderly patient. Within one minute one can assess minor salivary gland droplet formation and test the resting salivary pH, and this can then be used to monitor changes over time resulting from lifestyle alterations or the introduction of new prescription or over the counter medicines.87 More extensive testing of salivary parameters, including stimulated flow rate, pH and buffer capacity, is warranted when there are clinical suspicions such as suddenly increased caries activity, pathological tooth wear, or the sudden appearance of signs and symptoms of dry mouth, particularly when the patient's medical history has changed. For example, elderly patients with diabetes mellitus can show reduced resting salivary parameters because of increased fluid loss from polyuria. Likewise, the introduction of an anticholinergic or antidepressant medicine can cause gradually increasing oral dryness or a sudden onset of oral dryness.
Lifestyle advice for elderly patients needs to consider fluid intake (the volume of water as well as the acid and sugar content of liquids), the use of nicotine and other substances, and the pattern and nature of food intake. Diet can undergo dramatic changes with major life events in the later years, such as the loss of a spouse who did most of the cooking, or relocation to a residential aged care facility, where access to sweets both at mealtimes and between meals is often much greater than when living in the community. The use of stevia, sucralose and Isomalt as alternative non-cariogenic sweeteners of natural origin to replace sucrose in sweets and baked items is an important aspect to then consider.
Advice to patients at high risk of root surface caries should include the following elements:
-
1
Dietary restriction of sucrose, other fermentable simple sugars, and starches between meals, and the replacement of sucrose by alternative sweeteners such as stevia, sucralose, Isomalt or others
-
2
Dietary restriction of highly acidic foods and drinks
-
3
Use of sorbitol- or xylitol-containing chewing gums to boost salivary flow
-
4
Use of milk-based foods, such as low fat cheese, as between-meal snacks, rather than confectionery
-
5
At-home topical application of CPP-ACP with fluoride (for example, MI Paste Plus) before bed to elevate salivary levels of bio-available calcium ions
-
6
Twice daily tooth brushing with a high fluoride dentifrice, to reduce the thickness of the dental plaque biofilm and its acid production
-
7
Use of a neutral or alkaline saliva substitute if there are symptoms of xerostomia or low salivary pH at rest. Patients can also rinse with a home-made sodium bicarbonate solution.24,51
While taking a thorough history of lifestyle factors in the dental surgery provides many insights into a patient's living situation, a professional visit to the patient's place of abode is even more informative, since one can see firsthand what the patient is eating and drinking, and how they are using various oral hygiene products in their everyday life. A home visit is also a powerful behavioural intervention which can have dramatic benefits for oral health.89
Maintenance
Making the patient's mouth easy to care for is one of the most valuable services we as dentists can provide for our elderly patients. This extends from simple things to make oral hygiene easier (polishing and recontouring restorations, removing overhangs, shaping buccal restorations on roots to follow the anatomy of furcation entrances) to including identification into dentures and ensuring that any elderly patient with complex devices (including dental implants and precision attachments for bridges and dentures) has a paper 'passport' which records the details of these specialised components. A hard copy of this document is kept in the dental practice and another copy is given to the patient so that they have this on hand when they move to another district or into a long-term care facility, such as a residential aged care facility or nursing home. The next dentist who treats the patient will then know what is needed when these specialised devices need maintenance and repair.
It is oft remarked that 'Failing to plan is planning to fail', and thus it is essential to consider how the patient's current dental status is likely to decline over time as restorations and other treatments fail. Determining the patient's wishes for their dentition is essential when the patient is of advanced years but has not yet developed dementia. Retaining natural teeth is important from a quality of life perspective, since tooth loss is associated with impairment of oral health-related quality of life, and the location and distribution of tooth loss influence how severe that impairment is.90 Today, loss of teeth is not as acceptable as it was in previous generations, and this change in community perceptions and expectations affects demands for care.91,92
Considering what tooth loss is expected to occur in the future influences the design of bridgework and partial dentures. The situation of a patient who is transitioning to immediate dentures and is becoming edentulous in one or both arches requires careful planning around their ability to tolerate the procedure from both medical and psychological standpoints, their adaptability for the change to dentures, and how the dentures will have retention and stability over coming years as resorption of edentulous ridges occurs. A discussion around these issues with the patient (and as needed with their relatives or carers) ensures that the patient's wishes are considered fully at a time when they have capacity and can provide informed consent. For example, simplifying the patient's oral status to a shortened dental arch (8–10 occluding pairs for those over 70 years of age, or premolar to premolar occlusion) makes the dentition easier to care for and provides function and aesthetics. Population-based studies of patients with shortened dental arches have shown comparable oral health-related quality of life to those having more natural teeth,93 making this an acceptable option to consider in many cases. Nevertheless, each patient needs to be assessed from a biological and problem-oriented approach, on the basis that the anterior teeth and premolars should receive the best quality care and the highest priority.
Restorative interventions
With an increase in the number of frail elderly patients in the population, specific efforts should be made to proactively screen older adults for root surface lesions, so that only the least invasive methods of care are needed and teeth are not lost because of pulpal involvement. When restorations are indicated for cavitated lesions on the root surface, glass-ionomer cements are preferred over other materials.39
As mentioned previously, it can be expected that most elderly patients with exposed root surfaces who develop root surface caries will do so on the buccal aspects of their mandibular molars and premolars. While these particular areas are easy to examine clinically, it must be remembered that lesions on interdental root surfaces will often be missed by clinical examination, unless magnification (for example, an intraoral camera) is employed. Clinical examinations if used without radiographs are likely to underscore the true number of root surface caries lesions by as much as 50%.94 The true prevalence of root surface caries lesions in many community-based studies may well have been underestimated because many past studies have not used radiographs.
Root surface caries lesions can be identified on bitewing and periapical radiographs once sufficient mineral loss has occurred; however, as such lesions are typically broad and slowly progressing, they may not be visible on radiographs until they are at an advanced stage. This is a problem as the distance for caries to progress from the root surface into the dental pulp is quite small when compared to coronal caries. Corresponding with this, the chance for iatrogenic pulp exposure during removal of caries with rotary instruments is high.
A range of methods can be used to ensure restorative interventions for cavitated root surfaces do not result in iatrogenic pulpal exposure, including stepwise and partial excavation (ensuring a sound periphery for a high quality seal of the GIC bulk restorative material), chemo-mechanical caries removal (Carisolv), and fluorescence-assisted caries excavation.95,96 In the latter method, the fluorescence from infected dentine is identified (for example, red fluorescence elicited using 405 or 450 nm violet-blue light, as in the SiroInspect and SoproLife respectively) and used to guide selective caries removal.
Appropriate dentistry
Whether practising under the National Health Service or under a private practice model, one of the more challenging aspects of minimum intervention dentistry applied for the situation of the older patient is how the dentist can provide appropriate care that satisfies that patient's need for treatment to achieve a pain-free, functional and aesthetic dentition that is within their economic reach. This does not necessarily mean minimalist care or supervised neglect; indeed the standard of treatment should also be professionally satisfying to the dentist.97 Not all missing molar teeth have to be replaced, and a bridge or implant can obviate the need for partial denture. If patients choose the partial denture option, the consequences of increased caries risk for the remaining teeth need to be taken on board.
When an elderly patient has no functional or aesthetic problems and has a sufficient number of opposing contacts according to the shortened dental arch concept, they should continue with their natural teeth alone and not be given a partial denture. On the other hand, if there continues to be poor oral hygiene over time and no apparent prospects for change, the emphasis should be on maintaining function with natural teeth as long as possible. This could include using overdentures on natural teeth which have reduced coronal tooth structure, ensuring that patients apply a smear of remineralising agents such as neutral fluoride gels or MI Paste Plus onto the fitting surface after cleaning, so that caries is prevented. Retaining roots in this manner gives proprioception and maintains alveolar bone.
The timing of recall visits needs to be aligned to the patient's risk status, and not established as a blanket rule of one size fits all. Not all patients need six-monthly recalls, as some need to be seen more often and some less often. A maximum suggested recall time for older patients, even those who are fully edentulous, is 12 months, because of the high prevalence of oral mucosal diseases and the need to screen them for oral cancer. Regrettably, many patients do not attend this regularly, and as a result diseases often go unnoticed. The problem is even more pronounced for those in long-term care facilities who require support for everyday oral hygiene from a carer. Such patients typically show a decline in their oral health after admission. The responsibility for a patient's oral health is ultimately in their own hands or in that of their carers. As already discussed, many carers lack skills in performing oral hygiene on patients, and this lack of education is an area of pressing need. Consequently, the traditional concept of the dental team needs to expand to include not only staff in the dental practice but those in long-term care facilities who are involved in patient care – particularly carers, registered nurses and medical staff. There is evidence that, with appropriate training and support, registered nurses can perform very well in screening hospitalised patients for oral health issues and scoring their oral health status in a way that drives interventions.98
Applying a pre-emptive approach in line with the minimum intervention philosophy, there is evidence that if one follows 3–4 month recalls for examination, and includes in these same appointments oral hygiene instruction and intensive education, then this will improve dental health indicators over time and lower the need for repeated restorative and periodontal care.99 This timing should also ensure the maximum benefit is obtained from interventions such as application of fluoride varnish for caries prevention. Especially in times of economic difficulty, patients may be unable to afford such regular recall; however, the longer term benefits in terms of reduced treatment needs make this sound economics. There must be a set of oral health priorities negotiated between the patient and the dentist, so that both feel that the appropriate goals and outcomes are being achieved.
Summary
Minimal intervention dentistry for the elderly patient emphasises maximum interception of disease, beginning with managing risk factors, protecting at risk tooth surfaces, and ensuring that the dentition can be cleaned and maintained (see Table 2). There are now a range of devices, techniques and technologies that can help the dental team stabilise patients during the later years of their life when frailty is a challenge to maintaining oral health. Recognising oral health as part of general healthcare is critical for applying team models which involve all members of the dental team and extend to include carers as well as nursing and medical staff.
References
Lamster I B . Geriatric periodontology: how the need to care for the aging population can influence the future of the dental profession. Periodontol 2000 2016; 72: 7–12.
Yellowitz J A, Schneiderman M T . Elder's oral health crisis. J Evid Based Dent Pract 2014; 14 (Suppl): 191–200.
MacEntee M I . Oral care for successful aging in long-term care. J Public Health Dent 2000; 60: 326–329.
Petersen P E, Yamamoto T . Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2005; 33: 81–92.
MacEntee M I . Missing links in oral health care for frail elderly people. J Can Dent Assoc 2006; 72: 421–425.
Arai H, Ouchi Y, Yokode M et al. Toward the realization of a better aged society: messages from gerontology and geriatrics. Geriatr Gerontol Int 2012; 12: 16–22.
Dandakeri S, Dandekeri S, Rai B G, Suvarna N, Ragher M, Prabhu R . India's baby boomers: In driving need for dental care. J Pharm Bioallied Sci 2015; 7 (Suppl 2): S438–442.
Bharti R, Chandra A, Tikku A P, Arya D, Gupta R . Oral care needs, barriers and challenges among elderly in India. J Indian Prosthodont Soc 2015; 15: 17–22.
Silva M, Hopcraft M, Morgan M . Dental caries in Victorian nursing homes. Aust Dent J 2014; 59: 321–328.
Calache H, Hopcraft M S, Martin J M . Minimum intervention dentistry – a new horizon in public oral health care. Aust Dent J 2013; 58 (Suppl 1): 17–25.
Friedman S M, Shah K, Hall W J . Failing to focus on healthy aging: a frailty of our discipline? J Am Geriatr Soc 2015; 63: 1459–1462.
Arai H, Ouchi Y, Toba K et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr Gerontol Int 2015; 15: 673–687.
Banerjee A . 'MI'opia or 20/20 vision? Br Dent J 2013; 214: 101–105.
Pretty I A . The life course, care pathways and elements of vulnerability. A picture of health needs in a vulnerable population. Gerodontology 2014; 31 Suppl 1: 1–8.
Koh R, Pukallus M L, Newman B, Walsh L J, Foley M A, Seow W K . Effects of water fluoridation on caries experience in the primary dentition in a high caries risk community in Queensland, Australia. Caries Res 2015; 49: 184–191.
Walsh L J . Root caries – The emerging challenge in dental caries management. Annals Roy Australas Coll Dent Surg 2014; 22: 60–63.
Griffin S O, Barker L K, Griffin P M, Cleveland J L, Kohn W . Oral health needs among adults in the United States with chronic diseases. J Am Dent Assoc 2009; 140: 1266–1274.
Timonen P, Niskanen M, Suominen-Taipale L, Jula A, Knuuttila M, Ylöstalo P . Metabolic syndrome, periodontal infection, and dental caries. J Dent Res 2010; 89: 1068–1073.
Prpić J, Kuis D, Pezelj-Ribarić S . Obesity and oral healthis there an association? Coll Antropol 2012; 36: 755–759.
Ojima M, Amano A, Kurata S . Relationship between decayed teeth and metabolic syndrome: data from 4716 middle-aged male Japanese employees. J Epidemiol 2015; 25: 204–211.
Furuta M, Liu A, Shinagawa T, Takeuchi K, Takeshita T, Shimazaki Y, Yamashita Y . Tooth loss and metabolic syndrome in middle-aged Japanese adults. J Clin Periodontol 2016; 43: 482–491.
Locker D, Leake J L . Coronal and root decay experience in older adults in Ontario, Canada. J Public Health Dent 1993; 53: 158–164.
Beck J D, Drake C W . Do root lesions tend to develop in the same people who develop coronal lesions? J Public Health Dent 1997; 57: 82–88.
Walsh L J . Preventive dentistry for the general dental practitioner. Aust Dent J 2000; 45: 76–82.
Nyvad B, Fejerskov O . Active root surface caries converted into inactive caries as a response to oral hygiene. Scand J Dent Res 1986; 94: 281–284.
Billings R J, Brown L R, Kaster A G . Contemporary treatment strategies for root surface dental caries. Gerodontics 1985; 1: 20–27.
Jensen M E, Kohout F . The effect of a fluoridated dentifrice on root and coronal caries in an older adult population. J Am Dent Assoc 1988; 117: 829–832.
Herkströter F M, Witjes M, Arends J . Demineralization of human dentine compared with enamel in a pH-cycling apparatus with a constant composition during deand remineralization periods. Caries Res 1991; 25: 317–322.
Ripa L W . A critique of topical fluoride methods (dentifrices, mouthrinses, operator, and selfapplied gels) in an era of decreased caries and increased fluorosis prevalence. J Public Health Dent 1991; 51: 23–41.
Lynch E, Baysan A . Reversal of primary root caries using a dentifrice with a high fluoride content. Caries Res 2001; 35 (Suppl 1): 60–64.
Baysan A, Lynch E, Ellwood R, Davies R, Petersson L, Borsboom P . Reversal of primary root caries using dentifrices containing 5: 000 and 1: 100 ppm fluoride. Caries Res 2001; 35: 41–46.
Hay K D, Thomson W M . A clinical trial of the anticaries efficacy of casein derivatives complexed with calcium phosphate in patients with salivary gland dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 93: 271–275.
Rodrigues J A, Lussi A, Seemann R, Neuhaus K W . Prevention of crown and root caries in adults. Periodontol 2000 2011; 55: 231–249.
Rethman M P, Beltrán-Aguilar E D, Billings R J et al. Nonfluoride caries-preventive agents: executive summary of evidence-based clinical recommendations. J Am Dent Assoc 2011; 142: 1065–1071.
Walsh L J, Brostek A M . Minimal intervention dentistry principles and objectives. Aust Dent J 2013; 58 (Suppl 1): 3–16.
Gluzman R, Katz R V, Frey B J, McGowan R . Prevention of root caries: a literature review of primary and secondary preventive agents. Spec Care Dentist 2013; 33: 133–140.
Hayes M . Topical agents for root caries prevention. Evid Based Dent 2015; 16: 10–11.
Zhao I S, Mei M L, Burrow M F, Lo E C, Chu C H . Prevention of secondary caries using silver diamine fluoride treatment and casein phosphopeptide-amorphous calcium phosphate modified glass-ionomer cement. J Dent 2017; 57: 38–44.
Ngo H, Opsahl-Vital S . Minimal intervention dentistry II: part 7. Minimal intervention in cariology: the role of glass-ionomer cements in the preservation of tooth structures against caries. Br Dent J 2014; 216: 561–565.
Arbabzadeh-Zavareh F, Gibbs T, Meyers I A, Bouzari M, Mortazavi S, Walsh L J . Recharge pattern of contemporary glass ionomer restoratives. Dent Res J (Isfahan) 2012; 9: 139–145.
Mazzaoui S A, Burrow M F, Tyas M J, Dashper S G, Eakins D, Reynolds E C . Incorporation of casein phosphopeptide-amorphous calcium phosphate into a glass-ionomer cement. Incorporation of casein phosphopeptide amorphous calcium phosphate into a glass-ionomer cement. J Dent Res 2003; 82: 914–918.
Yap J, Walsh L J, Naser-ud Din S, Ngo H, Manton D J . Evaluation of a novel approach in the prevention of white spot lesions around orthodontic brackets. Aust Dent J 2014; 59: 1–11.
Vlacic J, Meyers I A, Walsh L J . Combined CPP-ACP and photoactivated disinfection (PAD) therapy in arresting root surface caries: a case report. Br Dent J 2007; 203: 457–459.
Lynch E, Beighton D . A comparison of primary root caries lesions classified according to colour. Caries Res 1994; 28: 233–239.
Baysan A, Lynch E . Clinical reversal of root caries using ozone: 6month results. Am J Dent 2007; 20: 203–208.
Holmes J . Clinical reversal of root caries using ozone, double-blind, randomised, controlled 18-month trial. Gerodontology 2003; 20: 106–114.
Amer R S, Kolker J L . Restoration of root surface caries in vulnerable elderly patients: a review of the literature. Spec Care Dentist 2013; 33: 141–149.
Deutsch A . An alternate technique of care using silver fluoride followed by stannous fluoride in the management of root caries in aged care. Spec Care Dentist 2016; 36: 85–92.
van der Weijden G A, Hioe K P . A systematic review of the effectiveness of self-performed mechanical plaque removal in adults with gingivitis using a manual toothbrush. J Clin Periodontol 2005; 32 (Suppl 6): 214–228.
DePaola L G, Overholser C D, Meiller T F, Minah G E, Niehaus C . Chemotherapeutic inhibition of supragingival dental plaque and gingivitis development. J Clin Periodontol 1989; 16: 311–315.
Walsh L J . Dental plaque fermentation and its role in caries risk assessment. Int Dent SA 2006; 1: 4–13.
Niederman R . Manual versus powered toothbrushes: the Cochrane review. J Am Dent Assoc 2003; 134: 1240–1244.
Deery C, Heanue M, Deacon S et al. The effectiveness of manual versus powered toothbrushes for dental health: a systematic review. J Dent 2004; 32: 197–211.
Deacon S A, Glenny A M, Deery C et al. Different powered toothbrushes for plaque control and gingival health. Cochrane Database Syst Rev 2010; 12: CD004971.
Van der Weijden F A, Campbell S L, Dörfer C E, González-Cabezas C, Slot D E . Safety of oscillating-rotating powered brushes compared to manual toothbrushes: a systematic review. J Periodontol 2011; 82: 5–24.
Kiger R D, Nylund K, Feller R P . A comparison of proximal plaque removal using floss and interdental brushes. J Clin Periodontol 1991; 18: 681–684.
Slot D E, Dörfer C E, Van der Weijden G A . The efficacy of interdental brushes on plaque and parameters of periodontal inflammation: a systematic review. Int J Dent Hyg 2008; 6: 253–264.
Ross N, Charles C, Dills S . Long-term effects of Listerine Antiseptic on dental plaque and gingivitis. J Clin Dent 1989; 1: 92–95.
Charles C H, Sharma N C, Galustians H J, Qaqish J, McGuire J A, Vincent J W . Comparative efficacy of an antiseptic mouthrinse and an antiplaque/antigingivitis dentifrice. A six-month clinical trial. J Am Dent Assoc 2001; 132: 670–675.
Charles C H, Sharma N C, Qaqish J G, Galustians H J, Zhao Q . Comparative effectiveness of an essential oil mouthrinse and dental floss in controlling interproximal gingivitis and plaque. Am J Dent 2002; 15: 351–355.
Rølla G, Ellingsen J E . Clinical effects and possible mechanisms of action of stannous fluoride. Int Dent J 1994; 44 (Suppl 1): 99–105.
Miller S, Truong T, Heu R, Stranick M, Bouchard D, Gaffar A . Recent advances in stannous fluoride technology: antibacterial efficacy and mechanism of action towards hypersensitivity. Int Dent J 1994; 44 (Suppl 1): 83–98.
Tinanoff N . Progress regarding the use of stannous fluoride in clinical dentistry. J Clin Dent 1995; 6 (Spec Iss): 37–40.
White D J . A “return” to stannous fluoride dentifrices. J Clin Dent 1995; 6 (Spec Iss): 29–36.
Perlich M A, Bacca L A, Bollmer B W et al. The clinical effect of a stabilized stannous fluoride dentifrice on plaque formation, gingivitis and gingival bleeding: a six-month study. J Clin Dent 1995; 6 (Spec Iss): 54–58.
Liang N, White D J, Cox E et al. Antimicrobial effects of a stabilized stannous fluoride dentifrice in reducing plaque acid production – a single-brushing PGRM study. J Clin Dent 1995; 6 (Spec Iss): 80–83.
Beiswanger B B, McClanahan S F, Bartizek R D, Lanzalaco A C, Bacca L A, White D J . The comparative efficacy of stabilized stannous fluoride dentifrice, peroxide/baking soda dentifrice and essential oil mouthrinse for the prevention of gingivitis. J Clin Dent 1997; 8 (2 Spec Iss): 46–53.
Ramji N, Baig A A, He T et al. Sustained antibacterial actions of a new stabilized stannous fluoride dentifrice containing sodium hexametaphosphate. Compend Cont Educ Dent 2005; 26 (suppl 1): 19–28.
Sensabaugh C, Sagel M E . Stannous fluoride dentifrice with sodium hexametaphosphate: review of laboratory, clinical and practice-based data. J Dent Hyg 2009: 83: 1–9.
Randall J, Seow W K, Walsh L J . Antibacterial activity of fluoride compounds and herbal toothpastes on Streptococcus mutans: An in vitro study. Aust Dent J 2015; 60: 368–374.
Cullinan M P, Westerman B, Hamlet S M, Palmer J E, Faddy M J, Seymour G J . The effect of a triclosan-containing dentifrice on the progression of periodontal disease in an adult population. J Clin Periodontol 2003; 30: 414–419.
Blinkhorn A, Bartold P M, Cullinan M P et al. Is there a role for triclosan/copolymer toothpaste in the management of periodontal disease? Br Dent J 2009; 207: 117–125.
Singh S, Chaknis P, DeVizio W, Petrone M, Panagakos F S, Proskin H M . A clinical investigation of the efficacy of three commercially available dentifrices for controlling established gingivitis and supragingival plaque. J Clin Dent 2010; 21: 105–110.
Boneta A E, Aguilar M M, Romeu F L, Stewart B, DeVizio W, Proskin H M . Comparative investigation of the efficacy of triclosan/copolymer/sodium fluoride and stannous fluoride/sodium hexametaphosphate/zinc lactate dentifrices for the control of established supragingival plaque and gingivitis in a six-month clinical study. J Clin Dent 2010; 21: 117–123.
Barnes V M, Richter R, DeVizio W . Comparison of the short-term antiplaque/antibacterial efficacy of two commercial dentifrices. J Clin Dent 2010; 21: 101–104.
Seymour G J, Palmer J E, Leishman S J et al. Influence of a triclosan toothpaste on periodontopathic bacteria and periodontitis progression in cardiovascular patients: a randomized controlled trial. J Periodontal Res 2017; 52: 61–73.
Otten M P, Busscher H J, Abbas F, van der Mei HC, van Hoogmoed C G . Plaqueleftbehind after brushing: intra-oral reservoir for antibacterial toothpaste ingredients. Clin Oral Investig 2012; 16: 1435–1442.
Ciancio SG . Controlling biofilm with evidence-based dentifrices. Compend Contin Educ Dent 2011; 32: 70–76.
Stewart J E, Wolfe G R . The retention of newly-acquired brushing and flossing skills. J Clin Periodontol 1989; 16: 331–332.
Yevlahova D, Satur J . Models for individual oral health promotion and their effectiveness: a systematic review. Aust Dent J 2009; 54: 190–197.
Kaufman L B, Henshaw M M, Brown B P, Calabrese J M . Oral health and interprofessional collaborative practice: examples of the team approach to geriatric care. Dent Clin North Am 2016; 60: 879–90.
Lewis A, Wallace J, Deutsch A, King P . Improving the oral health of frail and functionally dependent elderly. Aust Dent J 2015; 60 (Suppl 1): 95–105.
Yi Mohammadi J J, Franks K, Hines S . Effectiveness of professional oral health care intervention on the oral health of residents with dementia in residential aged care facilities: a systematic review protocol. JBI Database System Rev Implement Rep 2015; 13: 110–122.
Fried J . Interprofessional collaboration: if not now, when? J Dent Hyg 2013; 87 (Suppl 1): 41–43.
Sheiham A . The future of preventive dentistry. BMJ 1994; 309: 214–215.
Ettinger R L . Review: xerostomia: a symptom which acts like a disease. Age Ageing 1996; 25: 409–412.
Walsh L J . Clinical aspects of salivary biology for the dental clinician. Int Dent SA 2007; 9: 22–41.
Tanasiewicz M, Hildebrandt T, Obersztyn I . Xerostomia of various etiologies: a review of the literature. Adv Clin Exp Med 2016; 25: 199–206.
Plonka K A, Pukallus M L, Barnett A, Holcombe T F, Walsh L J, Seow W K . A controlled, longitudinal study of home visits compared to telephone contacts to prevent early childhood caries. Int J Paediatric Dent 2013; 23: 23–31.
Gerritsen A E, Allen P F, Witter D J, Bronkhorst E M, Creugers N H . Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes 2010; 8: 126.
Tsakos G, Steele J G, Marcenes W, Walls A W, Sheiham A . Clinical correlates of oral health-related quality of life: evidence from a national sample of British older people. Eur J Oral Sci 2006; 114: 391–395.
Cronin M, Meaney S, Jepson N J, Allen P F . A qualitative study of trends in patient preferences for the management of the partially dentate state. Gerodontology 2009; 26: 137–142.
Tan H, Peres K G, Peres M A . Retention of teeth and oral health-related quality of life. J Dent Res 2016; 95: 1350–1357.
Walsh L J, Gan A . Proximal root surface caries in an Australian periodontal population. Periodontol 1991; 12: 33–36.
Banerjee A, Sherriff M, Kidd E A, Watson T F . A confocal microscopic study relating the autofluorescence of carious dentine to its microhardness. Br Dent J 1999; 187: 206–210.
Schwendicke F, Paris S, Tu Y K . Effects of using different criteria for caries removal: a systematic review and network meta-analysis. J Dent 2015; 43: 1–15.
Smith I R, Brownlea A A . Cost-conservative dentistry: appropriate dentistry at lower cost. Aust Dent J 1993; 38: 360–366.
Walsh L J, Hill G, Seymour G J, Roberts A . A scoring system for the quantitative evaluation of oral changes during bone marrow transplantation. Spec Care Dent 1990; 10: 190–195.
Westerman B . A preventive dental care programme at the workplace. Aust Dent J 1993; 38: 210–215.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Walsh, L. Minimal intervention management of the older patient. Br Dent J 223, 151–161 (2017). https://doi.org/10.1038/sj.bdj.2017.660
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.660
This article is cited by
-
Is there a preferable management for root caries in middle-aged and older adults? A systematic review
British Dental Journal (2021)