Key Points
-
Outlines an alternative approach to management of patients with myofascial temporomandibular pain.
-
Emphasises the importance of education and conservative measures demonstrated as key treatment strategies for patients with simple myofascial pain.
-
Promotes self-care to improve quality of care both in the short and long-term.
Abstract
Background and aim To evaluate the outcome of a group therapy approach in the management of myofascial temporomandibular pain (TMD) through promotion of self-care.
Methods A group based interactive session was introduced for those patients who, at initial consultation, were diagnosed with myalgic TMD. Feedback forms and telephone interviews were used to record patient reported outcome measures to assess patient satisfaction with the service.
Results Fifty-five patients attended 17 group sessions over ten months. Feedback revealed a high level of satisfaction immediately after the session with 71% (n = 39) of patients opting for discharge, reporting confidence to self-manage in primary care. This effect appears to be sustainable up to 11 months.
Conclusions This approach benefits patients with myofascial TMD through promotion of self-management while utilising health care resources efficiently.
Similar content being viewed by others
Introduction
Temporomandibular disorders (TMD) encompass the disease processes involving 'the temporomandibular joints (TMJs), the masticatory muscles and all associated tissues'.1 Myofascial pain represents the largest subgroup of TMD2 with myalgia (pain from the muscles of mastication) alone accounting for 23% incidence and combined myalgia and arthralgia (pain from the muscles of mastication and temporomandibular joints itself) accounting for 73% of cases, according to the OPPERA study.3
Persistent myofascial pain not only disturbs oral function, but also can have a significant impact on quality of life and lead to psychological distress and social impairment.4 Early management using simple techniques including education and counselling can be highly effective in improving prognosis for patients with TMD and reducing negative impacts. The literature suggests that 75% to 90% of patients with TMDs will successfully respond to education, advice and conservative reversible treatments alone.5
TMD may affect up to a third of the general population, ranging from 5-50%.6
The Royal College of Surgeons England (RCSeng) released a commissioning guide in an attempt to meet the challenges that have arisen with regard to 'over-referral' to secondary care of patients with simple myofascial TMD pain, as the majority of these can be managed in primary care. It is reported that of those patients with TMD presenting to their GDP, less than 20% require referral.7
Within our unit there has been an increase in both volume and variety of non-odontogenic facial pain referrals, including TMD, in line with the national trends.
The average patient journey involved multiple review appointments, with no clear outcomes following the initial diagnosis, with eventual discharge occurring over a 3-12 month period. There was no information available as to patient satisfaction with the service or how efficient it was in terms of clinical time and cost.
Table 1 outlines some of the perceived challenges that clinicians faced with regard to this specific cohort of patients.
A group therapy approach was introduced with the aim of improving the effectiveness and efficiency of the service while obtaining patient outcomes to evaluate its impact.
Group programmes are described for their therapeutic use in the management of chronic pain conditions, such as fibromyalgia. Supportive group settings can give patients the opportunity to openly express concerns about their condition, exchange shared experiences and develop the ability to help themselves.8 We used principles from well-researched group-participation strategies in the management of chronic pain.9
This report evaluates our experience of group therapy techniques in managing patients with myofascial pain by encouraging self-management through the provision of early education, advice and conservative treatments. To our knowledge this is the only published report to explore the benefits of group therapy for the management of myofascial TMD pain.
Materials and methods
Starting in April 2015, the clinic took the form of an interactive group education session with up to six participants. All patients were required to have attended an initial oral surgery consultant clinic where a clear working diagnosis was made and an initial explanation given to the patient. Gaining the myofascial diagnosis was largely based on The Research Diagnostic Criteria recommendations.2 The diagnosis of parafunction was reached from either clinical evidence of parafunction or reported by patients.10 If any bite-raising-appliances were indicated, the impressions were taken at the initial consultation. A guidance leaflet was designed to ensure that only patients with 'simple' myalgic pain were referred to the group session.
Figure 1 shows the referral criteria for the group clinic.
Each group session lasted 30 minutes and was led by a single oral surgery clinician. The group setting took place in a non-clinical area and was aimed at providing an opportunity of social support for behaviour change, while reducing isolation. The interactive aspect of the group session was emphasised by the use of a presentation lasting 15 minutes that was delivered, which included animation, videos and diagrams to provide information and education, with opportunity for open discussion and questions throughout. The content was based on RCSeng6 recommendations and included:
-
1
Outlining population trends of jaw pain
-
2
Explanation of the structure of the jaw joint
-
3
Defining the nature and features of jaw pain
-
4
Explanation of the cyclic and self-limiting nature of myofascial pain with an emphasis on self-care
-
5
Discussion of the various simple, reversible conservative pain management techniques including: heat-packs, self-massage, motion exercises.
Patients were encouraged to ask questions and discuss issues raised with the facilitator and other participants throughout the session. If required there was opportunity for further one-to-one consultation with the clinician and fit of prefabricated bite-raising-appliances (BRA). All patients were advised to discontinue the use of their BRAs on the rare occasion that they found it worsened parafunction and TMD symptoms.11
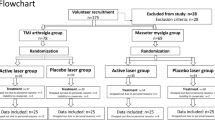
All patients were given the option of discharge back to practice or review in secondary care in order to empower them in contributing to their own management. Figure 2 shows the management pathway.
Feedback questionnaires were used before and after each session in order to evaluate patient satisfaction and capture patients' attitudes and expectations regarding their myofascial jaw pain. The same three questions were asked before and immediately after the group session with a scoring system of 1 (lowest) to 5 (highest). Written informed consent was obtained for each patient to approve the use of these results and comments. For those patients who opted for discharge to primary care immediately following the session, a phone interview was carried out using the same questions after two months and 11 months to evaluate the long-term impact. This is shown in Figure 3.
Results
A one month (October 2014) local service evaluation showed that there were a total of 51 referrals for non-odontogenic facial pain. Of these 48 (94%) were TMD, two (4%) idiopathic odontolagia and one (2%) ear pathology. Of the TMD cases 41 (85%) were diagnosed with myofascial pain, with the remaining seven (15%) cases experiencing internal joint derangement. The case mix within the myofascial pain group was 4:1 female to male with age range of 14 to 80 years.
Fifty-five patients attended the 17 group sessions over a ten month period between April 2015 and February 2016. There were 47 females and eight males (approximate female to male ratio of 6:1). Age range 18 to 59 years with a mean age of 35.8 years and a median of 37 years.
The majority of the patients required fitting of a pre-fabricated bite-raising-appliance and 39 (71%) patients opted for discharge as they felt confident to self-manage. The remaining 16 patients requested review for the following reasons:
-
4 for physiotherapy
-
1 to follow-up prescription medication
-
10 patients did not feel confident enough to self-manage their jaw pain
-
1 follow-up for MRI results.
Of the 39 patients that had opted for discharge immediately after the session, 18 were contactable for telephone interview over a time period of two to 11 months after the session.
At the initial consultation, the diagnosis was explained to the patient and management information was provided before referral to the group session where the following questions were asked:
Question 1: How well informed do you feel about your jaw pain?
Question 2: Do you understand your jaw pain?
There was a large variation in scores before the group session with over half of the patients (n = 31) giving the lowest scores of 1, 2 and 3. Immediately after the session, an improvement was observed where all the patients recorded the highest scores of 4 and 5 indicating better knowledge and understanding of their condition. This was maintained for all 18 patients following the phone interview.
Question 3: Are you confident in managing your jaw pain?
Approximately 70% (n = 38) of the patients scored 2 and 3 before the session, with a large variation. 93% (n = 51) of patients scored 4 and 5 after the session, which showed a marked improvement. However four patients (7%) did not feel confident to self-manage and requested review appointments at this point. On telephone follow up, all of the contactable patients scored 3 or more and none required re-referral for their TMD, stating that they were managing this well in primary care.
See Figure 4 for these results.
Expectations
The results for patients' expectations before the interactive session are shown in Table 2.
Following the group session 96% of these expectations were met. Those not met included: more information about jaw exercises, more advice on coping strategies and the lack of information leaflets.
Quotations from the feedback forms were reviewed to demonstrate the authenticity of the patients' experiences. All patients emphasised (either verbally or written) the usefulness of the education session and appreciated the time taken for comprehensive explanation and advice for their condition. The general consensus about the group setting was positive overall and many patients left comments, for example: 'This was helpful as I needed to know that I am not alone' and 'I enjoyed meeting other people who are going through a similar situation as I am'. One patient said: 'This is a worthwhile idea. The presentation was clear and informative, with all my questions answered by the professional and caring dentist leading the session'. Many expressed a sense of relief after learning that: 'the pain will eventually disappear' and 'it is not a brain tumour' with one patient stating that: 'this had answered my concerns about my pain, which has reduced stress from this for both myself and my husband.' At the end of the session, most patients' outlook into their long-term care appeared to be positive: 'I feel more confident in managing my pain and prevent it from worsening' and 'I feel that I can better communicate with my dentist and GP about my pain'.
Discussion
The aim was to explore the effectiveness of group therapy in the management of myofascial TMD, through delivery of education and conservative advice to empower the patient to self-manage.
Following headache and backache, TMD is now considered the third most common chronic pain condition.6,12 Myalgic and arthralgic pain, followed by myalgic pain alone are the most common subgroups of TMDs.3,13 Our pilot study revealed that myofascial pain constituted 85% of TMD referrals. Clenching, female gender and facial trauma are reported to be the most common aetiological factors associated with increased risk of myofascial pain, as reflected in our service evaluation.10 Oral parafunctional activities that may overload the masticatory system, such as clenching or grinding of teeth (diurnal or nocturnal), chewing gum and nail biting, are thought to either damage muscle fibres or reduce perfusion to the muscle, hence causing myalgic pain.14,15,16
The evidence suggests that oral appliances are a cost effective, non-invasive, reversible adjunct to pain management techniques for symptom relief of myalgic TMD pain.17 The benefits include: reducing muscle activity, decreasing bruxism, enhancing the patient's cognitive awareness and protecting the dentition from the harmful effects of repeated hyperloading.11,16,17,18
Most of the patients that attended the group session were fitted with a pre-fabricated bite-raising-appliance, as parafunctional habit was identified as a contributing factor to the patient's myofascial pain. This was done hand in hand with careful patient education, explanation of conservative pain management techniques and encouragement of self-care, which is shown to be more effective than provision of an occlusal appliance alone.16
Reversible, conservative therapies have been described as the 'first line intervention' for any patient with TMD.19 Early education, simple advice and non-invasive treatments have a reported 68-95% success rates in patients across TMD subtypes.6 TMD sufferers often search for explanations of their symptoms, however are likely to experience difficulties in obtaining a clear diagnosis due to the lack of certainty among healthcare professionals in diagnosing, understanding and managing TMD.20,21,22 Consequently patients often develop anxiety from the confusion over the source of their pain, particularly seeking reassurance for its benign nature, and this worry can further exacerbate their TMD symptoms, leading to a vicious cycle, as reflected by some of our patients' open feedback comments.12,20,23
Uncertainty surrounding TMD can lead to non-efficacious care pathways with unclear outcomes, as demonstrated by our service evaluation. Clear explanations, using diagrams to increase knowledge alongside a clear initial diagnosis and conservative management advice are important.12 This approach may be unrealistic in the current primary care framework and could help to explain the apparently poor effectiveness of treatment of TMDs in primary care.
Surprisingly, despite being given information regarding their initial diagnosis, most patients wanted to gain more information and understanding of their TMD symptoms. This was the main factor that drove establishment of the group information session. Perhaps patients could not recall the information or the original clinical setting was not ideal for patient education. All of the patients reported the highest scores immediately after attending the interactive session regarding how well informed they felt about their jaw pain and that they better understood the nature of their pain, compared to the low and variable scoring given before the session. Telephone follow-up revealed a sustained improvement up to 11 months following the session for the 18 contactable patients. A limitation of this study is that while patients reported an increase in knowledge, this may not necessarily equate to their knowledge having necessarily improved as no further questioning to assess this was carried out. As myofascial pain can be ongoing and can vary in intensity over time, an 11 month follow-up period might not have picked up a relapse in patterns. This follow-up period will continue to be extended in the future.
It has been shown that an emphasis on self-care while educating patients about their TMD is beneficial, having both short and long-term positive effects.16,24,25 The success of this is largely dependent on the patient's motivation and compliance, as well as effective communication with the healthcare practitioner to encourage good patient-practitioner rapport.26 The cyclic and largely self-limiting nature of myofascial pain was emphasised during the session to help patients accept the likelihood of fluctuations in their symptoms and to better equip them with simple techniques in managing and preventing flare-ups. This appeared to reinforce the patients' responsibility while addressing control factors simultaneously, resulting in a better outcome through enhancement of self-care.6,12,16,25 Our group session appeared to have successfully promoted self-management for the majority of patients as 51 of the 55 patients gave the highest scores for this at the end of the session, with 39 of these opting for discharge to primary care. This was also reflected in the telephone follow-up where none of the patients that were contactable required re-referral to secondary care, as they felt confident to self-manage their pain. This patient pathway incorporates the RCSeng outlook in managing simple myofascial pain patients in primary care with referral to secondary care for the complex TMD cases requiring specialist services.
To our knowledge this is the only published report to look at the use of group therapy for the management of TMDs specifically. Group therapy was the intervention of choice as it provided opportunities for social comparison, as per behaviour change taxonomy.9 Universality is one of the main therapeutic factors of group sessions and we built on this concept first described by Yalom.27 Accessing other patients' experiences within a group can create a sense of community and encourage patients to take ownership of the self-care pain management strategies that are simultaneously being delivered throughout the interactive session.8 Principals from group-participation strategies in the management of chronic pain conditions were used to offer patients the opportunity to share experiences and to gain increased insight and acceptance of their pain that is not offered during individual clinical consultation.27,28,29
Despite initial reservations among some of the patient groups about others being in the room, once they had participated and received the intervention, the patients reported high satisfaction with the service and found this pathway beneficial. All the feedback comments were positive and this may be a reflection of the specific selection criteria, which was important in narrowing down the patient group to those who are likely to benefit the most from this management strategy.
Although only one patient openly requested to meet others with similar pain before the session, a large proportion of the open feedback comments from our patients were related to the usefulness and therapeutic effect of sharing experiences within the group. There was an emphasis on the importance of the supportive nature of the clinician leading the open discussion.
The clinician has a key role in engaging this group of patients, and their style of delivery, attitude and motivation is likely to influence how successful this management approach is. This could be seen as a drawback for the widespread implementation of this pathway, as selecting an appropriate clinician who can be trained to manage this cohort of patients in a group could be challenging.
When patients were seen in a group with fitting of the BRA the clinical time required was reduced by approximately 70%, allowing time and resources to be redistributed to delivering care in other areas. This could be seen as an efficient method for improving elements of health status while reducing health-care costs.25 We can only estimate the savings in clinical time and costs associated with group management and the significant reduction in unnecessary review appointments.
In our experience there are difficulties in obtaining patient reported outcome measures and delivering thorough advice and explanations individually at the chair side, therefore a group setting is a helpful alternative. Continuously obtaining and utilising feedback from our patients allowed us to tailor a comprehensive and effective care pathway to meet the patients' expressed desires for management, their priorities and expectations.30 However, there is a concern in being able to cater for all patient needs within a group. In an attempt to build on patient feedback and to deliver a more comprehensive service, we are currently liaising with clinical healthcare psychologists and physiotherapists to discuss future contributions from these specialties, which may provide a more holistic approach with favourable short and long-term benefit for myofascial TMD management.6,12,31,32 We are planning to include this in the group information session programme as well as preparing a patient information leaflet reinforcing the key points.
Conclusions
The delivery of targeted education and consistent counselling in a group setting results in patients reporting an increase in knowledge, understanding and confidence in self-managing their myofascial TMD pain which can be sustained up to 11 months post discharge.
Drawbacks include selecting and training a lead clinician as well as continuously adapting the sessions in response to patient feedback.
This novel care pathway for myofascial pain uses clinical time efficiently, appears cost effective while improving quality of care.
References
Greene C . Managing the care of patients with temporomandibular disorders. J Am Dent Assoc 2010; 141: 1086–1088.
Reiter S, Goldsmith C, Emodi-Perlman A, Friedman-Rubin P, Winocur E . Masticatory muscle disorders diagnostic criteria: the American Academy of Orofacial Pain versus the research diagnostic criteria/temporomandibular disorders (TMD). J Oral Rehabil 2012; 39: 941–947.
Slade G D, Bair E, Greenspan J D et al. Signs and symptoms of first-onset TMD and sociodemographic predictors of its development: The OPPERA prospective cohort study. J Pain 2013; 14: T20–T32.
Cioffi I, Perrotta S, Ammendola L et al. Social impairment of individuals suffering from different types of chronic orofacial pain. Prog Orthod 2014; 15: 27.
Greene C S . The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain 2001; 15: 93–105.
RCS Faculty of Dental Surgery. Temporomandibular Disorders (TMDs): an update and management guidance for primary care from the UK Specialist Interest Group in Orofacial Pain and TMDs (USOT). 2013 Available at: https://www.rcseng.ac.uk/dental-faculties/fds/publications-guidelines/clinical-guidelines/ (accessed: 22 June 2017).
British Association of Oral and Maxillofacial Surgeons. Commissioning guide: Temporomandibular joint disorders. 2014. Available at: https://www.rcseng.ac.uk/library-and-publications/college-publications/docs/tmj-commissioning-guide/ (accessed: 22 June 2017).
Furnes B, Natvig G K, Dysvik E . Therapeutic elements in a self-management approach: experiences from group participation among people suffering from chronic pain. Patient Prefer Adherence 2014; 8: 1085–1092.
Abraham C, Michie S . A taxonomy of behavior change techniques used in interventions. Health Psychol 2008; 27: 379–387.
Huang G J, LeResche L, Critchlow C W, Martin M D, Drangsholt M T . Risk factors for diagnostic subgroups of painful temporomandibular disorders (TMD). J Dent Res 2002; 81: 284–288.
Klasser G D, Greene C S . Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107: 212–223.
Durham J, Newton-John T R, Zakrzewska J M . Temporomandibular disorders. BMJ 2015; 350: h1154.
LeResche L . Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med 1997; 8: 291–305.
Ohrbach R, Markiewicz M R, McCall Jr W D . Waking-state oral parafunctional behaviors: specificity and validity as assessed by electromyography. Eur J Oral Sci 2008; 116: 438–444.
Michelotti A, Cioffi I, Festa P, Scala G, Farella M . Oral parafunctions as risk factors for diagnostic TMD subgroups. J Oral Rehabil 2010; 37: 157–162.
Michelotti A, Iodice G, Vollaro S, Steenks M H, Farella M . Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Am Dent Assoc 2012; 143: 47–53.
Dao T T, Lavigne G J . Oral splints: the crutches for temporomandibular disorders and bruxism? Crit Rev Oral Biol Med 1998; 9: 345–361.
Ekberg E, Vallon D, Nilner M . The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial. J Orofac Pain 2003; 17: 133–139.
Greene C S . Managing the care of patients with temporomandibular disorders. J Am Dent Assoc 2010; 141: 1086–108.
Durham J, Steele J G, Wassell R W, Exley C . Living with uncertainty temporomandibular disorders. J Dent Res 2010; 89: 827–830.
Just J K, Perry H T, Greene C S . Treating TM disorders: a survey on diagnosis, etiology and management. J Am Dent Assoc 1991; 122: 55–60.
Le Resche L, Truelove E L, Dworkin S F . Temporomandibular disorders: a survey of dentists' knowledge and beliefs. J Am Dent Assoc 1993; 124: 90–106.
Michelotti A, Steenks M H, Farella M, Parisini F, Cimino R, Martina R . The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. J Orofac Pain 2004; 18: 114–125.
Dworkin S F, Turner J A, Mancl L et al. A randomized clinical trial of a tailored comprehensive care treatment program for temporomandibular disorders. J Orofac Pain 2002; 16: 259–276.
Lorig K R, Ritter P, Stewart A L et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care 2001; 39: 1217–1223.
Wright E, Anderson G, Schulte J . A randomized clinical trial of intraoral soft splints and palliative treatment for masticatory muscle pain. J Orofac Pain 1995; 9: 192–199.
Yalom I D, Leszcz M . Theory and practice of group psychotherapy. Basic Books, 2005.
Dysvik E, Kvaløy J T, Furnes B . A mixed-method study exploring suffering and alleviation in participants attending a chronic pain management programme. J Clin Nurs 2014; 23: 865–876.
Keefe F J, Beaupre P M, Gil K M, Rumble M E, Aspnes A K . Group therapy for patients with chronic pain. Pain management: A practitioner's handbook 1996; 2: 234–255.
Kelleher M, Ray-Chaudhuri A, Khawaja N . Patients' priorities and attitudes towards their temporo-mandibular disorders. Prim Dent J 2015; 4: 17–21.
Aggarwal V R, Tickle M, Javidi H, Peters S . Reviewing the evidence: can cognitive behavioral therapy improve outcomes for patients with chronic orofacial pain? J Orofac Pain 2010; 24: 163–171.
Sturdivant J, Fricton J R . Physical therapy for temporomandibular disorders and orofacial pain. Curr Opin Dent 1991; 1: 485–496.
Acknowledgements
Anna Maciag, Dept. of Oral Surgery, Guys Dental Hospital, London, SE1 9RT
Jennifer Hare, Dept. of Sedation and Special Care Dentistry, Guys Dental Hospital, London, SE1 9RT
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Henien, M., Sproat, C. Interactive group therapy for the management of myofascial temporomandibular pain. Br Dent J 223, 90–95 (2017). https://doi.org/10.1038/sj.bdj.2017.622
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.622