Key Points
-
Demonstrates a firm association between oral health and atherosclerotic cardiovascular disease.
-
Suggests periodontal therapy is associated with reductions in surrogate markers of atherosclerotic cardiovascular disease.
-
Proposes that oral health promotion improves oral health-related quality of life measures in stroke patients.
Abstract
Aim This paper reports on one review of four rapid reviews undertaken to explore the relationships between oral health and general medical conditions, in order to support teams within Public Health England, health practitioners and policy makers. This review aimed to explore the most contemporary evidence on whether poor oral health and cardiovascular disease occurs in the same individuals or populations, to outline the nature of the relationship between these two health outcomes and to discuss the implication of any findings for health services and future research.
Methods The review was undertaken by a group comprising consultant clinicians from medicine and dentistry, trainees, public health and academics. The methodology involved a streamlined rapid review process and synthesis of the data.
Results The results identified a number of systematic reviews of low to high quality, which suggests that there is: (1) fairly robust evidence of an increased risk of atherosclerotic vascular disease (ASVD) amongst individuals with chronic periodontitis, independent of other established cardiovascular risk factors; (2) there is some evidence that the incidence of caries and tooth loss is higher in patients with cardiovascular disease; and (3) that orofacial pain can presents as the sole symptom of stroke in some patients. The findings are discussed in relation to implications for service and future research.
Conclusion There is high quality evidence to support an association between cardiovascular disease and oral health. This evidence is mainly related to the association between chronic periodontitis and atherosclerotic heart disease, and is independent of confounding factors as drawn from epidemiological observational studies.
Similar content being viewed by others
Background
Cardiovascular disease (CVD) is a major cause of morbidity and mortality in the UK, in spite of significant improvements in disease prevention, detection and treatment over recent decades.1 Principal disease categories include (a) atherosclerotic cardiovascular disease (coronary, cerebrovascular and peripheral vascular disease), (b) valvular heart disease, (c) heart failure and cardiomyopathies, (d) arrhythmias, (e) infective and autoimmune conditions (including infective endocarditis), and (f) hypertension.
In 2014, Coronary Heart Disease (CHD) alone was the leading single cause of death in the UK (15% of male and 10% of female deaths), and accounted for up to 1 in 20 inpatient episodes. Cerebrovascular disease (stroke) resulted in approximately 39,000 deaths in 2014, and was the third largest single cause of mortality in the UK (6% of male and 8% of female deaths).2 Data from NHS England spending for 2014 reveal that expenditure for CVD was in the region of £4.3 billion, with the highest amount (40% or £1.7 billion) arising from 'unscheduled' or emergency care.2 According to the Global Burden of Disease study, ischaemic heart disease is the leading cause of disability years of life lost in England.1
The two most common diseases affecting oral health are dental caries and periodontitis. Dental caries is the localised destruction of susceptible dental hard tissues by acidic by-products from bacterial fermentation of dietary carbohydrates.3 Periodontitis is a chronic inflammatory disease caused by bacterial infection of the supporting tissues around the teeth.4 Approximately half of all adults in the UK are affected by some level of irreversible periodontitis, which increases with age, and almost a third have obvious dental decay.5
Several direct and indirect mechanisms have been proposed as pathophysiological links between chronic periodontitis and atherosclerotic cardiovascular disease.6 Key concepts include the interplay between periodontal pathogens, vascular endothelial damage and atherogenesis. Systemic inflammation, with chronically elevated inflammatory markers, is common to both disease processes, though to what extent anatomically remote sources of inflammation interact in causative fashion is unclear. Molecular mimicry may additionally play a role, with evidence of cross reactivity between oral pathogens and both inflammatory and endothelial cell components. Finally, the direct actions of pathogenic bacteria have also been proposed as a potential explanation for the putative relationship between chronic periodontitis and atherosclerotic cardiovascular disease. This has been extensively investigated over recent decades with divergent results, based in no small part due to difficulties in pathogen detection, proof of causal association and challenges in undertaking clinical outcome studies.
This review was limited to synthesising the literature on the primary links between cardiovascular diseases and oral health. This includes the impact of therapeutic interventions to treat oral disease, but not complications that arise from them; acquired infective endocarditis related to oral disease therapy and cardiac drug-effects (eg gingival hyperplasia in response to dihydropyridines) and their effects on oral health are, therefore, not considered.
Review methods
A rapid review of systematic reviews and/or meta-analyses published between 2005 and 2015 investigating the relationship between cardiovascular disease and oral health was performed. A rapid review involves synthesis of the most current and best evidence to inform decision-makers. It combines elements of systematic reviews with a streamlined approach to summarise available evidence in a timely manner.
Search syntax was developed based on subject knowledge, MESH terms and task group agreements (Box 1); followed by duplicate systematic title and abstract searches of three electronic databases: Cochrane, PubMed, OVID (Embase, MEDLINE [R], and PsycINFO). Two independent searches were carried out, followed by screening papers by abstract and title for relevance and duplication. Where there was a large body of evidence regarding a particular element, articles were limited to 2010 onwards to reduce the repetition of evidence.
Studies were included if they were either a systematic review and/or meta-analysis and explored a link between cardiovascular disease and oral health. Disagreements between the reviewers and the wider research group were resolved by discussion. Papers were excluded if they were not available in English, did not mention any term related to oral health or cardiovascular disease, full text was not available or related to acquired infective endocarditis related to dental intervention, or drug-induced gingival hyperplasia.
The following information was extracted from each paper: author, year, title, journal, population studied, oral disease/intervention, definitions used, methods, comparison/intervention and controls, outcomes, results, authors' conclusions, quality and quality justification, all shown in the data extraction table (online Supplementary Table).
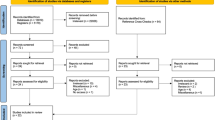
The search identified 247 potentially relevant abstracts, which were screened for duplicates and relevance. Those studies deemed not to have both an oral health and cardiovascular disease component to them were excluded at this stage. The remaining 42 articles were subject to full text review; 22 met the inclusion criteria. A flow diagram of this process is shown in Figure 1.
Quality assessment was undertaken for each systematic review using the PRISMA and AMSTAR tools to ascertain risk of bias. An AMSTAR assessment was carried out on all papers with the methodological quality of the review being rated as 'high' with a score between eleven and eight, 'moderate' between seven and four, and 'low' between four and zero. The quality of all papers was agreed in group discussion.
Within the themes identified by this review, most of the papers examined the link between atherosclerotic and oral disease, of which ten examined coronary heart disease and oral disease, and six cerebrovascular disease and oral disease. Of the 22 systematic reviews, 18 were found to be high quality based on AMSTAR tool,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23 three were of moderate,24,25,26 and one27 of low quality. For those with a score below 11, common quality issues were: lack of bias assessment, lack of publication bias assessment, lack of description of methodological rigour and lack of assessment of publication bias. Quality scores, together with the rationale, are presented for each paper in the online Supplementary Table.
Results: evidence synthesis
The results are synthesised into six sections. Each section combines evidence related to the relationship between a cardiovascular disease to an oral disease or impact of oral disease management.
Atherosclerotic cardiovascular disease and periodontitis
A number of systematic reviews of observational epidemiologic studies support an association between periodontal disease and atherosclerotic cardiovascular disease, independent of known confounders.6,13,23,24 Dietrich et al. (2013) found this association was stronger in younger compared with older patients, and in males compared with females. There is a limited evidence base for an association between chronic periodontitis and both the risk of recurrent cardiovascular events in patients with established atherosclerotic disease (secondary events) and peripheral vascular disease, respectively.13 There is no evidence to support or refute a causative relationship between cardiovascular disease and oral health.6
Five systematic reviews with meta-analyses have demonstrated patients with chronic periodontitis have an increased risk of developing coronary heart disease.7,8,15,18,23 Helfand et al. (2009) explored non-traditional cardiovascular risk factors (that is, those not included within traditional risk models, such as diabetes, blood pressure and cholesterol levels), to explain the risk for incident coronary heart disease (CHD) events in intermediate-risk individuals; chronic periodontitis was one of nine variables studied, but failed conclusively to improve risk prediction.14
A meta-analysis by Lafon et al. (2014) reported that periodontitis was associated with increased risk of stroke (relative risk 1.63 [1.25, 2.00]).16 Sfyroeras et al. (2012) also suggest an association between periodontitis and haemorrhagic stroke; this association was stronger in males, obese patients and non-diabetics.21
In summary, the evidence suggests that the incidence of atherosclerotic cardiovascular disease is higher in patients with periodontitis compared to those without.
Atherosclerotic cardiovascular disease and tooth loss
Four systematic reviews,14,15,16,20 suggest that tooth loss is associated with an increased risk of cardiovascular disease, in particular the risk of coronary heart disease and stroke, as outlined below.
Coronary heart disease and tooth loss
Humphrey et al. (2008)15 pooled estimates, demonstrating that individuals with 0–10 teeth had a relative risk of coronary heart disease and coronary death of 1.34 (95% CI 1.10–1.63) compared to patients with 25–32 teeth (P = 0.02). A later meta-analysis by Helfand et al. in 200914 likewise demonstrated a 1.34 relative risk (CI, 1.10–1.63) of general cardiovascular disease for persons with 0–10 teeth compared to those with >10 teeth.
Cerebrovascular disease stroke and tooth loss
A meta-analysis by Lafon et al. (2014)16 indicated a pooled risk estimate of 1.39 (1.13, 1.65) when ischaemic and both ischaemic and haemorrhagic strokes were considered together for edentulous patients compared with dentate patients.
Circulatory mortality and tooth loss
Polzer et al. (2012)20 reported that 12 out of 15 studies showed an increased risk of all-cause mortality among individuals with high numbers of missing teeth; seven out of nine studies demonstrated increased circulatory mortality (defined as a primary cardiac cause) in this group.
In summary, although the cause of tooth loss is unclear, the evidence suggests that patients with fewer teeth are more likely to suffer cardiovascular disease and cardiovascular-related death.
Stroke and oral health related quality of life
The systematic review by Dai et al. (2015) highlights that stroke patients have poorer oral health-related quality of life and oral function.11 It is unclear whether this represents disease association or simply a manifestation of reduced dexterity.
In summary, oral health-related quality of life of stroke patients is significantly worse than those who have not suffered stroke.
Cardiovascular disease and caries/endodontic disease
A systematic review by Dai et al.10 found that patients with stroke have significantly higher caries prevalence (DMFT) scores than healthy controls. An earlier systematic review of moderate quality evaluated the potential association between apical periodontitis/endodontic disease and CVD, but found scarce evidence to support this link.27
In summary, there is some evidence that dental caries and disease associated with infections from dental caries or periodontal tissues are associated with incidence of cardiovascular disease.
Stroke and oral health promotion
Two systematic reviews,9,26 of which one was a Cochrane review,9 show that use of oral health promotion could improve oral health of stroke patients. This includes, periodontal therapy or prophylactic extractions and particularly healthcare training on oral health promotion
In summary, for patients who have suffered a stroke, oral health promotion can have a significant impact on their oral health.
Cardiovascular disease and periodontal treatment
Periodontal treatment has been shown to have the following effects on surrogate markers implicated in cardiovascular disease: reduction in levels of Creactive protein,12,19,22,25 improvement in endothelial function,6,12 and reduction in carotid intima-medial thickness (c-IMT).23 D'Aiuto et al. (2013) reported moderate evidence of a negligible effect of periodontal therapy in reducing interleukin6 and lipid levels, and limited evidence on the effects on the following surrogates: arterial blood pressure, leucocyte counts, fibrinogen, tissue necrosis factorα, sE-selectin, von Willebrand factors, D-dimers, matrix metalloproteinase, oxidative stress and CVD events. There was no evidence on the effects of periodontal therapy on subclinical atherosclerosis, serum levels of CD40 ligand, serum amyloid A and monocyte chemo attractant protein.
Although periodontal interventions result in a reduction of certain surrogate markers, there is no evidence that this is associated with changes in atherogenesis or disease outcomes.6 This is supported by Li et al. (2014), who suggest that there is insufficient evidence that periodontal therapy can impact on recurrence of coronary heart disease.17
In summary, there is a large body of evidence suggesting that periodontal therapy has a significant effect on a number of surrogate markers implicated in cardiovascular disease; however, there is insufficient evidence that periodontal therapy has an impact on recurrence or secondary events of coronary heart disease.
Summary
There is high quality evidence to support an association between cardiovascular disease and oral health. This evidence mainly is related to the association between chronic periodontitis and atherosclerotic heart disease and is independent of confounding factors as drawn from epidemiological observational studies. Notably, no causal relationship has been established between cardiovascular disease and periodontal disease6 and the results suggest associations of varied strength between other oral diseases such as caries and oral facial pain and cardiovascular disease.
This review was limited by the widespread discrepancy in the definitions of cardiovascular and chronic periodontitis used in the literature. Kelly et al. (2013) had similarly highlighted significant structural and methodological variability among the published systematic reviews and meta-analyses regarding the connection between periodontitis and CHD.28 A strength of this review is the high number of meta-analyses. Furthermore, the focus on a wide range of cardiovascular and oral disease provides a wider range of evidence identifying areas of interest that may require further research.
The findings in this review have significant implications for health services and research. In relation to health services generally, healthcare professionals diagnosing and managing oral and cardiovascular disease should be aware of the associations highlighted in this review and the implications for patient care and health outcomes. A concerted effort is necessary across disciplines to ensure relevant cross-referrals and risk assessments in order to reduce the incidence and improve prognosis of these diseases.
Dental professionals should provide health promotion advice and signposting for patients presenting with chronic periodontitis in the presence of other cardiovascular disease risk factors such as obesity, diabetes and increased age. For example, the NHS Health Check has been introduced for people aged 40–74 to focus on the principle behavioural and physiological risk factors for CVD. Dental professionals should encourage uptake of this service for those considered at increased risk of CVD.
Quality of life of patients who have suffered stroke is significantly altered and the implication of changes in dexterity and oral muscular function can cause further challenges. A daily regime of care should be instituted to maintain oral health, and activities to support carers in this role will also be helpful.11
There is room for well-designed longitudinal studies which can further examine the associations between these two diseases and surrogate markers of disease. It is only following this that firm recommendations can be made with regards to whether further interventions are required. Therefore, observational studies should evaluate the association between periodontitis and adverse events in high-risk populations. Randomised controlled trials are required to establish the effectiveness of periodontal treatment in high risk groups on surrogate cardiovascular endpoints (Box 2).
In summary, there is a firm association between oral health (periodontitis, caries and tooth loss) and atherosclerotic cardiovascular disease; that is coronary heart disease, stroke, and peripheral vascular disease. There is little or no evidence to support any links between oral health and other forms of cardiovascular disease that is non-atherosclerotic such as hypertension, arrhythmias and heart failure. Periodontal therapy is associated with reductions in surrogate markers of atherosclerotic cardiovascular disease such as endothelial function, inflammatory and oxidative stress markers. There is evidence that oral health promotion interventions, involving staff and patients, improve oral health-related quality of life measures in stroke patients.
References
Newton J N, Briggs A D M, Murray C J L et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386: 2257–2274.
Townsend N, Bhatnagar P, Wilkins E, Wickramasinghe K, Rayner M . Cardiovascular Disease Statistics. London: British Heart Foundation, 2015.
Fejerskov O, Kidd E . Dental caries: the disease and its clinical management. UK: John Wiley & Sons, 2009.
Eke P I, Page R C, Wei L, Thornton-Evans G, Genco R J . Update of the case definitions for population-based surveillance of periodontitis. J Periodontol 2012 Dec; 83: 1449–1454.
Steele J, O'Sullivan I . Adult Dental Health Survey 2009. Available online at http://www.hscic.gov.uk/catalogue/PUB01061/aduldenthealsurvfirsrele2009rep.pdf (accessed November 2016).
Lockhart P B, Bolger A F, Papapanou P N et al. Periodontal disease and atherosclerotic vascular disease: does the evidence support an independent association?: a scientific statement from the American Heart Association. Circulation 2012; 125: 2520–2544.
Bahekar A A, Singh S, Saha S, Molnar J, Arora R . The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J 2007; 154: 830–837.
Blaizot A, Vergnes J N, Nuwwareh S, Amar J, Sixou M . Periodontal diseases and cardiovascular events: meta-analysis of observational studies. Int Dent J 2009; 59: 197–209.
Brady M, Furlanetto D, Hunter R V, Lewis S, Milne V . Staff-led interventions for improving oral hygiene in patients following stroke. Cochrane Database Syst Rev 2006; 18: CD003864.
Dai R, Lam O L, Lo E C, Li L S, Wen Y, McGrath C . A systematic review and meta-analysis of clinical, microbiological, and behavioural aspects of oral health among patients with stroke. J Dent 2015; 43: 171–180.
Dai R, Lam O L, Lo E C, Li L S, Wen Y, McGrath C . Orofacial functional impairments among patients following stroke: a systematic review. Oral Dis 2015; 21: 836–849.
D'Aiuto F, Orlandi M, Gunsolley J C . Evidence that periodontal treatment improves biomarkers and CVD outcomes. J Periodontol 2013; 84 (4 Suppl): S85–S105.
Dietrich T, Sharma P, Walter C, Weston P, Beck J . The epidemiological evidence behind the association between periodontitis and incident atherosclerotic cardiovascular disease. J Periodontol 2013; 84(4 Suppl): 134: 008.
Helfand M, Buckley D I, Freeman M et al. Emerging risk factors for coronary heart disease: a summary of systematic reviews conducted for the U S. Preventive Services Task Force. Ann Intern Med 2009; 151: 496–507.
Humphrey L L, Fu R, Buckley D I, Freeman M, Helfand M . Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med 2008; 23: 2079–2086.
Lafon A, Pereira B, Dufour T et al. Periodontal disease and stroke: a meta-analysis of cohort studies. Eur J Neurol 2014; 21: 1155–1161.
Li C, Lv Z, Shi Z et al. Periodontal therapy for the management of cardiovascular disease in patients with chronic periodontitis. Cochrane Database Syst Rev 2014; 15: CD009197.
Mustapha I Z, Debrey S, Oladubu M, Ugarte R . Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: a systematic review and meta-analysis. J Periodontol 2007; 78: 2289–2302.
Paraskevas S, Huizinga J D, Loos BG . A systematic review and meta-analyses on Creactive protein in relation to periodontitis. J Clin Periodontol 2008; 35: 277–290.
Polzer I, Schwahn C, Volzke H, Mundt T, Biffar R . The association of tooth loss with all-cause and circulatory mortality. Is there a benefit of replaced teeth? A systematic review and meta-analysis. Clin Oral Investig 2012; 16: 333–351.
Sfyroeras G S, Roussas N, Saleptsis V G, Argyriou C, Giannoukas A D . Association between periodontal disease and stroke. J Vasc Surg 2012; 55: 1178–1184.
Teeuw W J, Slot D E, Susanto H et al. Treatment of periodontitis improves the atherosclerotic profile: a systematic review and meta-analysis. J Clin Periodontol 2014; 41: 70–79.
Zeng X T, Leng W D, Lam Y Y et al. Periodontal disease and carotid atherosclerosis: A meta-analysis of 17,330 participants. Int J Cardiol 2016; 203: 1044–1051.
Azarpazhooh A, Tenenbaum H C . Separating fact from fiction: use of high-level evidence from research syntheses to identify diseases and disorders associated with periodontal disease. J Can Dent Assoc 2012; 78: c25.
Freitas C O, Gomes-Filho I S, Naves R C et al. Influence of periodontal therapy on Creactive protein level: a systematic review and meta-analysis. J Appl Oral Sci 2012; 20: 1–8.
Lam O L T, Zhang W, Samaranayake L P, Li L S W, McGrath C . A systematic review of the effectiveness of oral health promotion activities among patients with cardiovascular disease. Int J Cardiol 2011; 151: 261–267.
Cotti E, Dessi C, Piras A, Mercuro G . Can a chronic dental infection be considered a cause of cardiovascular disease? A review of the literature. Int J Cardiol 2011; 148: 4–10.
Kelly J T, Avila-Ortiz G, Allareddy V, Johnson G K, Elangovan S . The association between periodontitis and coronary heart disease: a quality assessment of systematic reviews. J Am Dent Assoc 2013; 144: 371–379.
Acknowledgements
We would like to acknowledge the support of Dr Francesco D'Aiuto of University College London on this paper and during workshops. We would like to acknowledge the support of Public Health England, the Royal College of Surgeons and the British Dental Association.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Supplementary information
Supplementary information S1 (table)
Cardiovascular disease and oral health: papers included in rapid review (PDF 292 kb)
Rights and permissions
About this article
Cite this article
Dietrich, T., Webb, I., Stenhouse, L. et al. Evidence summary: the relationship between oral and cardiovascular disease. Br Dent J 222, 381–385 (2017). https://doi.org/10.1038/sj.bdj.2017.224
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.224
This article is cited by
-
A test of pre-exposure spacing and multiple context pre-exposure on the mechanisms of latent inhibition of dental fear: A study protocol
BMC Psychology (2024)
-
Utilization of machine learning models in predicting caries risk groups and oral health-related risk factors in adults
BMC Oral Health (2024)
-
A study protocol testing pre-exposure dose and compound pre-exposure on the mechanisms of latent inhibition of dental fear
BMC Psychology (2024)
-
Association between toothbrushing and cardiovascular risk factors: a cross-sectional study using Korean National Health and Nutrition Examination Survey 2015–2017
BMC Oral Health (2024)
-
Exploring the presence of oral bacteria in non-oral sites of patients with cardiovascular diseases using whole metagenomic data
Scientific Reports (2024)