Key Points
-
Highlights that compliance with supportive periodontal therapy is universally low; this study reports that only 32% of patients were compliant.
-
Reports that males and non-smokers were more compliant with supportive periodontal therapy.
-
Finds that no quantitative factor is a definitive indicator of compliance with supportive periodontal therapy.
Abstract
Background The importance of supportive periodontal therapy following active treatment has been well documented but numerous studies have shown patient compliance to be poor. The aim of this study was to ascertain which factors affect patient compliance and whether this included routinely recorded periodontal indices.
Methodology This was a five-year retrospective service evaluation study set within a private general dental practice. It utilised demographic and periodontal data from patients who attended the practice for chronic periodontal treatment in 2009 and ascertained whether there were links between this data and compliance with the supportive phase of periodontal treatment.
Results Three hundred and ten patients satisfied the inclusion criteria of which 32.3% were categorised as compliant, 45.5% non-compliant and 22.3% erratic attenders. Patients who were statistically significantly more compliant were males (p = 0.03) and non-smokers (p = 0.01). There was a trend for older people to be more compliant; however this was not statistically significant. Plaque and bleeding scores were lower in the compliant group but only the bleeding scores were statistically significant (p = 0.03). The pocket probing depths were used as an indicator of disease severity and showed no significant relationship with compliance.
Conclusion Although some of the periodontal parameters showed a statistically significant relationship with compliance, the difference between the parameters was clinically minimal suggesting that there is no definitive physical characteristic which is an indicator of patient compliance.
Similar content being viewed by others
Background
Periodontitis affects 45% of the UK's adult population.1 With such a high prevalence and potential for morbidity the management of this mainly chronic condition is an economic and epidemiological necessity. The principal treatment for chronic periodontitis is non-surgical intervention;2 however, due to the cyclical and unpredictable nature of periodontitis, an imbalance between the host response and the bacterial infection can lead to reactivation of the disease, hence the need for close monitoring following active treatment.3 It has been suggested that this phase of treatment, commonly referred to as supportive periodontal therapy (SPT), is more important than the active phase in the long-term management of periodontitis.4 The goal of SPT is to prevent or retard the progression of periodontitis and ultimately try and avert tooth loss5 and for this to occur long-term compliance is required.6,7 Periodontitis is often a chronic disease with few symptoms. Treatment compliance with any chronic disease is notoriously poor and the World Health Organisation (WHO) estimated that treatment conformity in chronic disease, in the developed world, was less than 50%.8
Although compliance with SPT is key, many studies have shown that compliance is generally poor.9,10,11 Identifying likely non-compliant patients at an early stage and putting measures in place to secure their return would improve the outcome of periodontal treatment and subsequently the patient's periodontal health. Various factors have been linked with compliance, including socio-economic factors and personality traits;11 however, these are difficult to quantify, whereas periodontal parameters, which are routinely recorded at hygiene appointments, are more easily quantified. The aim of this study was to discover possible links between compliance and periodontal indices such as plaque index, bleeding index and pocket probing depths, and patient factors such as age, gender, and smoking status. Should such a relationship exist then supportive care could be more appropriately tailored to the individual. Greater emphasis could then be placed on those likely non-compliers towards motivation and appointment upkeep to maintain compliance during the critical period of SPT.
Method and methodology
This study was a retrospective service evaluation using existing anonymised patient data from the computerised records of adult patients who attended the author's private general dental practice in Scotland for chronic periodontal treatment in the year 2009. By being a retrospective clinical practice study, this study had some inevitable flaws including a lack of both calibration and blinding of the clinician giving rise to the potential for recording bias.
The study's sample population (n = 727) excluded patients if they failed to complete the chronic periodontal treatment, also known as the active phase of treatment (APT), or if they had died or were known to have moved out of the area. The data collated were plaque and bleeding scores, recorded at the start and on completion of APT before the commencement of the supportive phase of treatment (SPT). Both scores were measured as a percentage of surfaces that recorded a positive score in relation to the total number of tooth surfaces in the mouth. Pocket probing depths were also recorded at the start of APT. The collected data reflected the percentage of sites that had periodontal pocketing greater or equal to 5 mm in relation to the total number of sites in the mouth. The rationale for using a percentage was that if a mean pocket probing depth was used then disease severity might be skewed by the healthy site 'masking' the unhealthy sites.6 The percentage pocket probing depths were then used as an indicator of disease severity since this has been previously linked with patient compliance and SPT.13
The patient's age and gender and smoking status were recorded since an association has been found between these factors and compliance.8,10,14,15
Compliance was assessed for a period of five years as it has been shown that if supportive therapy is maintained for five years then there is minimal or no progression of periodontal disease.2,16 The patients were divided into the following groups:
-
Compliant patients were patients who attended within the recommended recall period. The recommended recall for periodontal patients is three monthly intervals;26 however, in this study the recall interval was set to six monthly intervals to take into account external factors such as patient and practitioner holidays that may prolong the recall interval and potentially render a patient an erratic attender
-
Erratic compliance patients were those who continued to attend the practice for supportive therapy but did not attend within the recommended recall period
-
Non-compliant patients were patients who failed to return for supportive therapy following an active phase of chronic periodontal treatment. The timing of when the patient failed to return for treatment was also noted as previous research has shown that the first year is 'critical' for compliance.13,17
The resulting data were then analysed statistically using SPSS Statistics (IBM SPSS Statistics Version 22) and StatPlus (StatPlus: Mac Version 5 AnalystSoft Inc.). Statistical significance was shown using either Chi-square or ANOVA one-way testing.
Results
Compliance
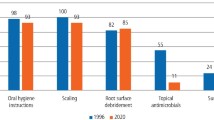
Three-hundred and ten patients were included in the study; of these 32% (n = 100) were compliant, 46% (n = 141) were non-compliant and 22% (n = 69) were erratic attenders. The mean number of years that patients became non-compliant was 2.04 years (SD ± 0.7), indicating that the majority of non-compliant patients dropped out of supportive treatment within 12–24 months of completing their course of active periodontal therapy (Fig. 1).
Gender
There were slightly more females (53%; n = 164) who took part in the study compared to males (47%; n = 146). However males were statistically significantly more compliant (p = 0.03) (Fig. 2).
Age
The mean age of the participants in this study was 44 years old. The majority of patients in the compliant (33%; n = 33) and erratic attenders (41%; n = 28) group were in the 50–59 -year-old age bracket, whereas the non-compliant patients (28%; n = 39) were predominately within the 30–39-year-old age bracket. The distribution was statistically insignificant (p = 0.08).
Smoking status
Seventy-eight percent (n = 243) of the patients in the study were non-smokers and the results showed that compliant patients were statistically significantly more likely (p = 0.01) to be non-smokers than non-compliant patients.
Plaque scores
The results of this study showed that there was a trend for the plaque scores, recorded at the start and end of the active periodontal phase of therapy (APT), to be lower in the compliant group of patients, although this was not statistically significant (p = 0.18).
Bleeding scores
This study demonstrated that the bleeding scores were lowest in the compliant group, with the initial scores being statistically significant (p = 0.03).
Pocket probing depths
In this study the mean percentage of pocket probing depths greater or equal to 5 mm, which was used as an indicator of disease severity, was similar in both the compliant and non-compliant groups, with the lowest being in the erratic group; however, the difference was not statistically significant (p = 0.28).
Interval between initial and final scores
As expected the time taken to complete the active phase of treatment was greatest in the erratic attenders group (p = 0.04). This may be explained by the cancelling or missing of appointments in this group, subsequently prolonging treatment time, hence indicating a possible predictive indicator of future attendance and compliance. Ironically, the lowest time to complete treatment was in the non-compliant group; however, this may be an indicator of a relationship with disease severity. The shorter time may be an indicator of mild disease levels and fewer active appointments required.
Discussion
It has been shown that one of the main reasons for lack of compliance in private referral periodontal practices and dental hospitals are patients returning to their own general dental practitioner (GDP) for supportive care.10,12 It was therefore hypothesised before the start of this study that compliance levels would be greater in a general dental practice. However, compliance levels (32%, Fig. 1) were very similar to those found in the literature that showed compliance levels in private periodontal practices to range widely from 3%18 to 53%19 and in a dental hospital setting to be 25%.20
When adherence to a supportive periodontal therapy programme is so important to prevent progression of periodontal disease,26 it is surprising that compliance levels are so low; especially as most patients comply with the active phase of treatment.27 In this study only 12% (n = 90) of patients failed to complete the active phase of treatment, much lower than the 46% (n = 141) who became non-compliant during the supportive phase of periodontal treatment. Patient compliance with health issues is generally low, and even with health conditions that are life-threatening patient compliance has been shown to be poor.4,28 It is therefore not surprising that a largely asymptomatic, non-life-threatening chronic condition such as periodontal disease has such low compliance levels.29 Understanding why patients are not more compliant may identify improvements in treatment planning and help in the prediction of disease progression.
Factors that have been attributed to lack of compliance include expense,10,30 patients returning to their own general dental practitioner for treatment,10,12 anxiety31,32and lack of perceived need for treatment.10
Without further qualitative research, such as non-compliant patient interviews or questionnaires, it can only be surmised that some of these factors may have influenced the compliance of the patients in this study. However, returning to their own general dental practice for treatment, by its very nature, cannot be a reason for lack of compliance in this study, but changing dental practices could be. Most dental practices report a 50% turnover of patients in a five year period.31 Aberdeen has a very transient population due to the oil industry33 and this local factor could potentially lead to a higher than average practice patient turnover, subsequently resulting in a perceived increase in lack of compliance. This can be seen by comparing compliance levels in this study (32%) to those of a more static population in rural Norway, where compliance levels after ten years were reported to be 87%.31 For those reasons the results may not be generalisable across the UK.
Expense could have had a bearing on lack of compliance in this study. Expense can be a disincentive in the treatment of chronic disease, as the perceived benefit of treatment is not always obvious to a patient, leading to a sense of a lack of 'value for money'.10 The practice in this study is wholly private so all periodontal treatment is self-funded; however, in this sample only 3% of patients were known to have transferred to a National Health Service (NHS) dental practice and if cost were a significant issue then this figure could have been expected to have been higher.
While anxiety could potentially be a factor that could affect compliance with SPT, it would also be expected to impact on compliance with the active phase of chronic periodontal treatment. However, in this study non-compliance during the active phase of treatment was nearly 25% of what it was during the supportive phase of treatment.
When considering gender as a potential predictive indicator of compliance, a review of the literature suggests that it is an unreliable predictive parameter with some studies showing females to be more compliant,14,19,21 while others show no significant relationship.11 In contrast to those previous findings, this study showed males to be more compliant.
The findings with respect to age and compliance were not endorsed by other studies which have shown there to be a significant relationship, with older patients being more compliant,14,15,19,22 but conversely some have shown no relationship.11 Thus the results of this study and the review of the literature suggest age is an unreliable predictor of compliance.
The trend for non-compliant patients to be smokers seen in a previous study by Ramseier et al.8 and in the study described in this paper may be explained by the various behavioural models and a patient's lack of regard or belief that their actions will affect their health. It has been suggested that as smokers are more likely to be non-compliant, and that both these factors are significant risk factors for disease reoccurrence,23 then a more stringent supportive periodontal regime should be advocated.8
Plaque scores in this study tended to be lower in compliant patients and a similar trend was seen in a study by Mendoza et al.;10 however, once again the results were not statistically significant (p >0.05); conversely a study by Konig et al.,20 showed plaque scores to be statistically significantly higher in non-compliant patients (p <0.05). Potential recording bias in this study due to both lack of calibration of the examiners and lack of conclusive support in the literature suggests that plaque scores are an unreliable predictive indicator.
Disease severity has been shown to have a positive correlation with compliance.24,25 This link may be explained by various behavioural science concepts; in more advanced disease the threat to patients of losing their teeth is more apparent and realistic than those with mild chronic periodontal disease, thus the patient has a greater 'belief' in the effectiveness of and need for treatment. However, the results of this study suggest that there is no relationship between disease severity and compliance.
Compliance is a complex conundrum and, like periodontal disease, has a multifactorial aetiology.34 Addressing all these factors and tailoring care for an individual is a time-consuming and demanding challenge; thus finding a simple predictive indicator of a patient's likely compliance would improve treatment planning and treatment outcomes.35 Although the aim of this study was to identify simple periodontal parameters that would indicate a patient's compliance, only some of the periodontal parameters showed a trend and in some cases a statistically significant relationship with compliance. However, the difference between the parameters was clinically minimal and not definitive; additionally, the literature reviewed suggests that there is no definitive physical characteristic that can be an indicator of a patient's compliance.
Thus the main characteristic that will determine a patient's compliance is their behavioural idiosyncrasies and their health beliefs. Behavioural scientists suggest that non-compliant patients have an 'indirect self-destructive behaviour' that is characterised by denial, negligence and a lack of responsibility for their health. They choose to adopt a philosophy that their health is the responsibility of the practitioner.27 Compliance with treatment is partially dependent on a patient's beliefs about their illness, both cognitively and emotionally. This includes whether a patient has the 'capacity' to comply with treatment and whether that treatment will lead to an improvement in their health. However, this is a complex field and unfortunately not one behavioural model has been suggested that explains dental compliance fully.28 As there is not a 'one size fits all recipe card' for ensuring a patient's compliance, the clinician needs to use all their skill and experience to gauge a patient's potential level of compliance and consider all patients as potential non-compliers.
Conclusion
From the evidence gained from this retrospective study and from reviewing the available literature it can be concluded that although some of the periodontal parameters showed a trend and in some cases a statistically significant relationship with compliance, the difference between the parameters was clinically minimal and not definitive; additionally flaws within this general practice study and other studies reviewed, suggests that there is no definitive physical characteristic that can be an indicator of a patient's compliance.
However, this study and the current literature suggest that the following factors should be considered when assessing a patient's compliance:
-
The patient's previous attendance history as this is often the most indicative sign of a patient's likely compliance
-
Age and gender: current evidence suggests that younger males are more likely to be non-compliant
-
Smoking status: since smokers have been shown to be more likely to be non-compliant.
However, the main characteristics that will determine a patient's compliance are their behavioural idiosyncrasies and their health beliefs. This is a complex field and unfortunately not one behavioural model has been suggested that explains dental compliance fully. Thus further research could therefore be directed at qualitative research to identify behavioural reasons why patients in this specific practice demonstrated a lack of compliance and how staff and clinicians could improve patient compliance.
Compliance to treatment of chronic disease is universally low, both in the medical and dental fields. However, the importance of adherence to a maintenance scheme is paramount in preventing the relapse of periodontal disease. Unfortunately, most studies, including this study, demonstrate that compliance levels are low. However, having identified potential causative factors, implemented change to practice protocols and improved focus on the education of both the dental team and patients, then it is suggested that compliance should improve, and with it the periodontal health of the patients within a general practice environment.
References
White D A, Tsakos G, Pitts N B et al. Adult Dental Health Survey 2009: common oral health conditions and their impact on the population. Br Dent J 2012; 213: 567–572.
Greenstein G . Periodontal response to mechanical non-surgical therapy: a review. J Periodontol 1992; 63: 118–130.
Lang N P, Tonetti M S . Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev Dent 2003; 1: 7–16.
Wilson Jr T G, Glover M E, Schoen J, Baus C, Jacobs T . Compliance with maintenance therapy in a private periodontal practice. J Periodontol 1984; 55: 468–473.
Renvert S, Persson G R . Supportive periodontal therapy. Periodontol 2000; 2004: 36: 179–195.
Konig J, Plagmann H-C, Ruhling A, Kocher T . Tooth loss and pocket probing depths in compliant periodontally treated patients: a retrospective analysis. J Clin Periodontol 2002; 29: 1092–1100.
Kocher T, Konig J, Dzierzon U, Sawaf H, Plagmann H C . Disease progression in periodontally treated and untreated patientsa retrospective study. J Clin Periodontol 2000; 27: 866–872.
Ramseier C A, Kobrehel S, Staub P, Sculean A, Lang N P, Salvi G E . Compliance of cigarette smokers with scheduled visits for supportive periodontal therapy. J Clin Periodontol 2014; 41: 473–480.
Novaes A B, Jr., Moraes N, Campos G M, Grisi M F . Compliance with supportive periodontal therapy. J Periodontol 1996; 67: 213–216.
Mendoza A R, Newcomb G M, Nixon K C . Compliance with supportive periodontal therapy. J Periodontol 1991; 62: 731–736.
Delatola C, Adonogianaki E, Ioannidou E . Non-surgical and supportive periodontal therapy: Predictors of compliance. J Clin Periodontol 2014; 41: 791–796.
Fardal O . Interviews and assessments of returning non-compliant periodontal maintenance patients. J Clin Periodontol 2006; 33: 216–220.
Novaes Jr A B, Reno De Lima F, Novaes A B . Compliance with supportive periodontal therapy and its relation to the bleeding index. J Periodontol 1996; 67: 976–980.
Novaes A B . Compliance with supportive periodontal therapy. Part II: Risk of non-compliance in a 10-year period. Braz Dent J 2001; 12: 47–50.
Miyamoto T, Kumagai T, Jones J A, Van Dyke T E, Nunn M E . Compliance as a prognostic indicator: retrospective study of 505 patients treated and maintained for 15 years. J Periodontol 2006; 77: 223–232.
Kaldahl W B, Kalkwarf K L, Patil KD . A review of longitudinal studies that compared periodontal therapies. J Periodontol 1993; 64: 243–253.
Novaes A B, Jr., Novaes A B . Compliance with supportive periodontal therapy. Part 1. Risk of non-compliance in the first 5-year period. J Periodontol 1999; 70: 679–682.
Soolari A, Rokn A R . Adherence to periodontal maintenance in Tehran, Iran. A 7-year retrospective study. Quintessence Int 2003; 34: 215–219.
Novaes A B . Compliance with supportive periodontal therapy. Part 1. Risk of non-compliance in the first 5-year period. J Periodontol 1999; 70: 679–682.
Konig J, Plagmann H C, Langenfeld N, Kocher T . Retrospective comparison of clinical variables between compliant and non-compliant patients. J Clin Periodontol 2001; 28: 227–232.
Demetriou N, Tsami-Pandi A, Parashis A . Compliance with supportive periodontal treatment in private periodontal practice. A 14-year retrospective study. J Periodontol 1995; 66: 145–149.
Ojima M, Hanioka T, Shizukuishi S . Survival analysis for degree of compliance with supportive periodontal therapy. J Clin Periodontol 2001; 28: 1091–1095.
Rieder C, Joss A, Lang N P . Influence of compliance and smoking habits on the outcomes of supportive periodontal therapy (SPT) in a private practice. Oral Health Prev Dent 2004; 2: 89–94.
Novaes A B, Jr., de Lima F R, Novaes A B . Compliance with supportive periodontal therapy and its relation to the bleeding index. J Periodontol 1996; 67: 976–980.
Kakudate N, Morita M, Kawanami M . Oral health care-specific self-efficacy assessment predicts patient completion of periodontal treatment: A pilot cohort study. J Periodontol 2008; 79: 1041–1047.
Darcey J, Ashley M . See you in three months! The rationale for the three monthly periodontal recall interval: a risk based approach. [Erratum appears in Br Dent J 2011; 211: 598]. Br Dent J 2011; 211: 379–385.
Fardal O . Periodontal maintenanceovercoming the barriers. Dent Update 2011; 38: 38–38.
Wilson Jr T G . Compliance. A review of the literature with possible applications to periodontics. J Periodontol 1987; 58: 706–714.
Becker B C, Karp C L, Becker W, Berg L . Personality differences and stressful life events. Differences between treated periodontal patients with and without maintenance. J Clin Periodontol 1988; 15: 49–52.
Glavind L . The result of periodontal treatment in relationship to various background factors. J Clin Periodontol 1986; 13: 789–794.
Johannessen A C, Linden G J . Compliance in a Norwegian periodontal practice. Oral Health Prev Dent 2003; 1: 93–98.
Wilson T G Jr., Compliance and its role in periodontal therapy. Periodontol 2000 1996; 12: 16–23.
National Records of Scotland. Population Projections for Scottish Areas: National Records of Scotland; 2014. Available online at http://www.nrscotland.gov.uk/news/2014/population-projections-for-scottish-areas (accessed November 2016).
Inglehart M, Tedesco L A . Behavioral research related to oral hygiene practices: a new century model of oral health promotion. Periodontol 2000 1995; 8: 15–23.
Hancock E B, Newell D H . Preventive strategies and supportive treatment. Periodontol 2000 2001; 25: 59–76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
This research was completed as part award of a Master of Science degree in Restorative Dentistry from the University of Warwick. Ethical approval was obtained as part of an MSc dissertation through the University of Warwick Biomedical and Scientific Research Ethics Committee.
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Perrell-Jones, C., Ireland, R. What factors influence patient compliance with supportive periodontal therapy in a general practice setting?. Br Dent J 221, 701–704 (2016). https://doi.org/10.1038/sj.bdj.2016.904
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.904
This article is cited by
-
Impact of COVID-19 on patient follow-up during supportive periodontal therapy: a retrospective study based on phone call survey
BMC Oral Health (2023)
-
Why do patients follow physicians’ advice? The influence of patients’ regulatory focus on adherence: an empirical study in China
BMC Health Services Research (2019)