Key Points
-
Informs practitioners about the most important things to consider when choosing a light-curing unit for their practice.
-
Warns practitioners about the risks behind using untested and unregulated LCU devices.
-
Discusses the blue-light hazard and advises how to protect dental personnel and patients.
Abstract
This paper is the second in a two-part series on the topic of LED light-curing units (LCUs). This part discusses LCU selection, cross infection and decontamination, maintenance, the blue-light hazard, and some possible future developments for LCUs. The article focusses on the practical aspects of the subject from the clinician's perspective. Scientific aspects are dealt with in the cited literature.
Similar content being viewed by others
Light curing unit selection
The light curing unit (LCU) and the process of light curing is a critical step in the restorative process when using light-activated resin-based composites (RBCs). It is recommended that new LCUs be purchased from a reputable manufacturer who will usually also market light-cured RBCs as well as LCUs. Some dentists buy their light units from budget online sources because they are cheaper than major dental manufacturers who produce high-quality well-tested units. There is no accountability regarding the manufacture or distribution of these budget lights and there is often a lack of electrical safety certification. These budget LCUs are usually flimsy and poorly made.1 Inadequate heat dissipation leads to premature LED failure. The electronics in many budget lights do not compensate for changes in battery output over the discharge cycle, and this may result in a sharp decline in output without warning.2,3 Instructions for use are often poorly translated into English and are sometimes missing or illogical. In order to deliver an acceptable irradiance, the light tips of budget lights are typically smaller than those of major manufacturers, and the light output is often highly inhomogeneous.3 The batteries in these unregulated LCUs may explode or catch fire with disastrous consequences and any perceived price advantage may turn out to be a false economy resulting in serious long-term negative clinical and financial consequences. A UK press release by the Medicines and Healthcare Regulatory Agency (MHRA) in October 2013 highlighted the issue of fake and unapproved dental LCUs being sold online and imported into the UK for sale.4 The MHRA cautioned that such devices had not been tested for safety or efficacy and warned dentists not to use such devices. The use of an unregulated and untested medical device on a patient should be regarded as in vivo testing on a patient who has not given informed consent.
LCUs that offer only a single fixed exposure time do not account for differing energy requirements of the RBCs being cured. Fans are incorporated into some light emitting diode (LED) LCUs to prevent the LED chip and the body of the unit from overheating. However, fans can only cool to the ambient temperature and thus such units are less appropriate for use in tropical regions. Well-designed LED units will have a protective thermal cut-off to protect the LED and electronics from overheating. Consequently, the unit may shut down during long exposure times. Some LED LCUs have batteries that can only be changed by the manufacturer at considerable expense. Some LED units have a corded backup option that negates the need for extra batteries or additional backup units. There is also a wide diversity of light unit styles ranging from mains-powered gun-style or pistol-grip handpieces to smaller lightweight pen style units (Fig. 1).
The vast majority of LED units only offer a single standard-diameter (7–8 mm) light guide tip, but due to the protective cladding, the active or light-emitting exit tip diameter of a standard multi-filament light guide is typically 1 mm less than the external diameter. For 'one-shot' light-curing, the active diameter of the tip must be greater than the greatest width of the restoration (Fig. 2). Small tips require overlapping cure cycles, reduce efficiency and increase the risk of missing a portion of the restoration. Wide tip diameters (10–13 mm) are required when the dentist seeks to cure large direct or indirect restorations efficiently.5 However, exposure times may need to be extended with larger tips, because the irradiance declines greatly as the tip area increases, for example increasing the tip size from 7 to 10 mm doubles the area and halves the irradiance. Small- or narrow-diameter guides (2-3 mm) are useful for spot or tack curing of indirect restorations and large-diameter tips can be used for 'single-shot' light curing of larger restorations.
The outer white circles show the areas covered by the tip of the light guides. The inner black circles define the effective light-emitting areas of the light guide tips. The average radiant exitance (within the black circle) for the BA Ultimate 1400 was 1,497 mW/cm2 and 1,234 mW/cm2 for the Deep Cure-S unit when measured accurately with laboratory grade equipment. Note the homogeneous light output for the Deep Cure-S unit. However, the power (W) output for the Deep Cure-S unit (785 mW) was 40% more than for the BA Ultimate 1400 unit (560 mW). The inhomogeneous output and smaller light-emitting area of the BA Ultimate 1400 LCU mean that the critical peripheral regions of the MOD restoration would not be adequately cured in a single light exposure
Some of the LED units do not have audible or visual countdown timer displays indicating the progress of curing. While some view the lack of a timed display as a minor inconvenience, it may lead to insufficient curing if the operator loses track of time or makes errors in counting the number of curing cycles in units with automatic shut-off intervals. Dentists who undertake extended orthodontic and restorative treatments, such as multiple-bracket and multiple veneer placements, require long uninterrupted run times and some LED units fail to meet this requirement. Radiometers that are built into the LCU allow the dentist to monitor the light output from their unit over time. Other important considerations include ergonomic features and unit costs.
The light curing times recommended by LCU and RBC manufacturers can be very different. Curing times cited by LCU and RBC manufacturers may differ greatly. As they will have carried out extensive testing, a manufacturer who markets light-cured RBCs as well as their own LCUs is best placed to advise the end user regarding appropriate exposure times for their products (these can vary eightfold between 5 and 40 seconds for one manufacturer's products/shades alone). At least one manufacturer who incorporates non-proprietary or alternative photoinitiators in their materials markets only broad-spectrum polywave® LED LCUs for this reason. If very light or 'bleach' shades of RBCs are used, the dentist should find out whether alternative photoinitiators are used because a polywave LED or quartz-tungsten-halogen (QTH) LCU may be a better option than a single blue peak LED LCU in this situation.
Recommended exposure times made by various authors have declined over the last 20 years; this is understandable given improvements in light curing technology. Light exposure times of between 1 and 60 seconds are currently proposed by manufacturers of different light sources and resin-based materials, and dental authors. Short exposure times are driven both by the practitioner's desire for speed and increased clinical efficacy, and also by competition between manufacturers of LCUs. Before purchasing a new LCU, the dentist is advised to assess the manufacturer's data and the related evidence base behind any marketing and performance claims.
Ideally the radiant power (W) should be given by manufacturers as well as irradiance figures. The dentist would then know if they were purchasing a powerful light, or just an average power light that has a small tip. If LCU manufacturers stated radiant exposures (J/cm2) for their units at available settings, dentists would be in a better position to identify appropriate exposure times for their materials. Manufacturers should also state irradiance values at clinically relevant distances in addition to their usual zero source distance figures. Appropriate exposure times are a subject of much debate and are influenced by many variables. Irradiance declines with increasing distance, but the rate of decline varies greatly with unit design and beam collimation (Fig. 3).
A survey of over 400 dental practices recently conducted across 18 cities in North America found that dentists' cure times ranged from 3 to 90 seconds.6 Recent studies have concluded that at least 10 seconds exposure time with a second-generation LED LCU (average irradiance >1,000 mW/cm2) is indicated for lighter shades of fast-curing materials under optimal clinical circumstances.7 How fast the RBC is able to polymerise is a significant factor. As exposure time increases, the extent of cure lateral to the directly-irradiated area may increase somewhat, and spectral matching between light source and initiator absorption may not be quite so critical, but most authorities recommend that a new LED unit should deliver a minimum irradiance of 1,000 mW/cm2 and be used for at least 10 seconds.
Cross infection and decontamination
Fan exits, protective tips and pistol grips are common areas for clinical contamination of QTH LCUs. In a pilot study, better results from a cross infection viewpoint have been reported for pen-style LED units with autoclavable light guides.8 Autoclavable light guides are the gold standard from an infection control viewpoint, but they can be easily damaged or contaminated with scale and should ideally be replaced on a regular basis. Fixed-lens-type light sources require barrier protection that can reduce light output by 10% or more.9 Ingress of disinfectant fluids into the LED unit can lead to contamination and loss of reflector efficiency, or even total unit failure of the electronics.
The blue-light hazard
The optical hazards for patients and staff of retinal exposure to light in the blue region of the spectrum (the blue-light hazard) have been documented and deserve greater attention given the popularity of light curing and the trend towards ever more powerful light curing units. Our eyes are at risk from acute and cumulative effects, mainly due to the significant reflection of blue light from the tooth surface. Phototoxic and photoallergic reactions may also occur from absorbed radiation in endogenous or exogenous substances which may accumulate in the operator's eyes and hands as well as in the patient's oral mucosa.10,11 The greatest retinal hazard from blue light occurs at 440 nm and, unfortunately, this is close to the peak spectral emission from many blue LED LCUs. Eye protection is required to protect against this blue light photochemical hazard. Filters may take the form of protective spectacles, stationary lamp shields or hand-held shields. Insufficient protection may occur if the filter is of poor quality, has aged, or is used to protect against emission from a light source with output characteristics different from the filter's intended use. Labrie et al.12 assessed the ocular hazard potential of four types of LCU by estimating the maximum permissible ocular exposure times for each unit during an 8-hour work day. The maximum permissible daily exposure limits for UV light was greater than 8 hours at all working distances and light source orientations. However, the maximum permissible cumulative daily exposure time to blue light was only 6 seconds when irradiating from the upper anterior palatal aspect with a PAC light and was up to 1.5 hours when the light from a low-power blue LED LCU was reflected back from the facial aspect of a central incisor. McCusker et al.13 have assessed the weighted irradiance and safe exposure times of 11 dental LCUs at six different working distances from the light guide exit. Corresponding parameters were assessed for reflected light from the most powerful unit during simulated bonding of different orthodontic brackets. Bracket material and shape affected the amount of reflected light. The maximum cumulative exposure from reflected light when viewed at typical tooth to operator distance of 30 cm was between 22 and 123 minutes each day for different LCUs. Although the risk was judged to be low if adequate safety precautions were employed, the authors concluded that the potential long-term ocular risks of prolonged exposure to blue light in a busy dental surgery were still uncertain. However, any long-term risks can be presented by using suitable blue light-blocking glasses or hand-held shields.
Maintenance of LED light curing units
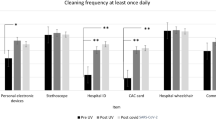
It is well reported that many dental LCUs are not properly maintained. Regular testing and maintenance of any piece of dental equipment is recommended to maintain effectiveness. Quality LED LCU manufacturers give detailed maintenance protocols which should be referred to. General recommendations that all can follow are:
-
Keep a record to show that the light output from the LCU was checked. Verify adequate unit output before each clinical session by comparing the value with the value recorded when the unit was new using the unit's built-in radiometer (if present), or a radiometer recommended by the manufacturer. Although radiometers may give reproducible irradiance values, do not rely on radiometers to give accurate irradiance values. Simply use the radiometer to determine whether the light output has changed from new. If the output has reduced it will be necessary to increase the exposure time
-
Only use the LCU if the light source tip or exit window is clean and undamaged. Check multi-filament light guides for broken fibres (which may show as black or dark areas). Do not touch the unpolymerised resin-based bonding agent or RBC with the light guide tip. Check the light source for contaminants immediately after patient use. Remove contaminants and if the light guide or lens is scratched or damaged, replace the component if possible. Alternatively, return the unit to the manufacturer for repair
-
Do not immerse the system components in water or disinfectant solutions. Do not spray liquid disinfectants directly onto the LCU handpiece or charger base. Prevent liquids from entering unit ports or openings. If the light guide is removed for autoclaving, use a protective cap to seal the light guide portal when cleaning the handpiece
-
Follow the manufacturer's protocol and local regulations for appropriate disinfection regimes for handpiece and battery charger base units. Avoid flammable or corrosive or abrasive cleaning agents
-
Autoclavable light guides are the 'gold standard' from a cross infection viewpoint. Polyethylene barrier sleeves will reduce light output by approximately 10%. Thus the light output should be tested with the barrier in place, if they are used. Ensure that the seam of the barrier sleeve does not cross the light source exit, because this will further reduce output. Barrier sleeves are single use, and elastomer or rubber light shields should be inspected and cleaned immediately after use. Clean contaminants off immediately and discard the shield if damaged.
Current and future developments
Work into designing modified LED LCUs that have a more uniform irradiance distribution has been reported. The Deep Cure-S LED LCU recently introduced by 3MESPE is an example of such a unit (Fig. 2).14 This unit and the Bluephase Style from Ivoclar Vivadent feature 'low-profile' light guides that allow the operator improved access posteriorly which may be critical for patients with restricted mouth opening. Other units like the Smartlite Focus (DENTSPLY) and Valo (Ultradent) have the LEDs incorporated directly into their low profile heads. One manufacturer (Satelec, ACTEON) has already introduced a unit with a low-power laser aiming function (ScanWave) that puts a red light circle on the tooth before light curing and an 'autofocus' LED LCU (AutoFocus Mark II) designed to compensate for the decline in the irradiance with increased distance by automatically increasing exposure time to counter this issue.15 Work has also been reported into developing a method that allows the operator to determine the appropriate exposure time for any light-activated material, irrespective of the characteristics of the LCU, or the material to be cured.16 These and other future developments will hopefully assist in improving the success and longevity of light-cured RBC restorations in dental practice.
Conclusions
Many developments have taken place in the field of light curing since the first UV light-cured materials and LCUs were introduced. This two-part series has reviewed the development and current status of LED LCUs and should give a better insight into the complexities of the subject. The key points are:
-
1
LED units offer significant advantages
-
2
The use of an unregulated and untested medical device on a patient should be regarded as in vivo testing on a patient who has not given informed consent
-
3
Manufacturers should state the power output, the emission spectrum, beam profile and effect of distance on the irradiance from their LCU
-
4
When choosing an LCU the extent and quality of resin polymerisation and unit efficacy and reliability should be paramount over any price or convenience features
-
5
Use a light that is optimised to cure the resins you are using
-
6
At any given required radiant exposure, the exposure time is a critical factor.
-
7
Regular testing and maintenance are important. Keep a record to show that the light output from the LCU has been regularly checked against the output when new
-
8
Keep the light tip as close as possible to the restoration when light curing
-
9
Beware of the blue-light hazard and use suitable eye protection. If you just look away, you cannot see what you are doing with the LCU.
References
Gordon J . Christensen: Clinicians report. Available online at http://www.cliniciansreport.org/uploads/files/403/MktgRT0314.pdf (accessed October 2016).
Price R B . Light-curing units. Dent Advisor 2015; 32: 2–7.
AlShaafi M M, Harlow J E, Price H L et al. Emission characteristics and effect of battery drain in 'budget' curing lights. Oper Dent 2016; 41: 397–408.
Shortall A C . Fake and unapproved dental curing lights sold online – MHRA warns dentists. The Probe 2013; 10.
Palin W M, Senyilmaz D P, Marquis P M, Shortall A C . Cure width potential for resin composite MOD molar restorations. Dent Mater 2008; 24: 1083–1094.
Felix C, Ferracane J L . Curing light outputs, protocols and composite requirements at 422 dental offices. J Dent Res 2015; 94 (Spec Iss A); abstract #340.
Busemann I, Lipke C, Schattenberg A, Willershausen B, Ernst C P . Shortest exposure time possible with LED curing lights. Am J Dent 2011; 24: 37–44.
Janoowalla Z, Porter K, Shortall A C C, Burke F J T, Sammons R L . Microbial contamination of light curing units: a pilot study. J Inf Prev 2010; 11: 217–221.
Price R B, Shortall A C, Palin W M . Contemporary Issues in light curing. Oper Dent 2014; 39: 4–14.
Bruzell Roll E M, Jacobsen N, Hensten-Pettersen A. Health hazards associated with curing light in the dental clinic. Clin Oral Investig 2004; 8: 113–117.
Bruzell E M, Johnsen B, Aalerud T N, Christensen T . Evaluation of eye protection filters for use with dental curing and bleaching lamps. J Occup Envir Hyg 2007; 4: 432–439.
Labrie D, Moe J, Price R B, Young M E, Felix C M . Evaluation of ocular hazards from 4 types of curing lights. J Can Dent Assoc 2011; 77: b116.
McCusker N, Lee S M, Robinson S, Patel N, Sandy J R, Ireland A J . Light curing in orthodontics; should we be concerned? Dent Mater 2013; 29: e85–e90.
Shimokawa C A K, Turbino M L, Harlow J E, Price H L, Price R B . Light output from six battery operated dental curing lights. Mater Sci Eng-C 2016; 69: 1036–1042.
Shortall A C, Palin W M, Jacquot B, Pelissier B . Advances in light-curing units: Four generations of LED lights and clinical implications for optimizing their use: Part 2. From present to the future. Dent Update 2012; 39: 13–22.
Harrington E, Wilson H J, Shortall A C . Light-activated restorative materials: a method of determining effective radiation times. J Oral Rehabil 1996; 23: 210–218.
Acknowledgements
This article is dedicated to the memory of our former colleague and friend Edward Harrington.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Shortall, A., Price, R., MacKenzie, L. et al. Guidelines for the selection, use, and maintenance of LED light-curing units – Part II. Br Dent J 221, 551–554 (2016). https://doi.org/10.1038/sj.bdj.2016.814
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.814