Key Points
-
Explains why root fillings which may look successful radiographically can fail, and why root fillings which may not look successful radiographically can succeed.
-
Identifies clinical techniques which may contribute to the success of a root filling
-
Provides advice on retreatment options when a tooth with a radiographically successful root filling fails.
Abstract
This article will discuss why a root filling that appears satisfactory on a radiograph may fail, and why one which appears unsatisfactory on a radiograph may succeed. In doing so, this article will also discuss the criteria of endodontic success and failure and its implications on the decision to retreat.
Similar content being viewed by others
The role of radiographs in endodontics
In all endodontic cases, a good intra-oral parallel radiograph of the entire root and periapical region is mandatory. The Faculty of General Dental Practitioners1 recommends that all root treated teeth should have radiographs taken immediately following obturation, with a further follow-up radiograph to assess (radiographic) healing after one year and then annually until (radiographically judged) healing occurs. The European Society of Endodontology Quality Guidelines2 further adds that these radiographs should show the root apex with preferably at least 2–3 mm of the periapical region clearly identifiable.
A pre-operative radiograph allows the clinician to estimate working length and predict the curvature of the canal system. Radiographs come with limitations, however, they provide a two dimensional image of a three dimensional object, making it difficult to see the number of canals and the direction of curvature accurately, and an estimation of working length often has to be confirmed with an apex locater. Furthermore, information regarding the quality of disinfection of the root canal system, and the conditions in which the root filling was carried out in, are not provided on a post-operative radiograph. A post-operative radiograph, however, does provide a foundation to compare future radiographs against in order to assess healing.
Success and failure of root canal treatment
The use of the terms success and failure have a long tradition in dentistry. They convey a simple rationale for further treatment decisions for both clinician and patient. Radiographically, root canal treatment (RCT) has an unfavourable outcome when one of the following occurs:2
-
1
A visible lesion appears subsequent to treatment, or a pre-existing lesion increases in size
-
2
The lesion has remained the same size during the four year assessment period
-
3
Signs of continuing root resorption are present.
Root canal treatment has then failed when of the following is required:
-
1
Extraction of the tooth
-
2
Replacement of the root filling
-
3
Periradicular surgery performed on the tooth.
The success of a root filling is influenced by the tooth itself. A multi-rooted tooth is more technically difficult to root fill than a single rooted tooth because of the location of the tooth in the mouth and the complex morphology of the canal system.3 Also, radiographs of single rooted teeth can be easier to interpret and understand than those of maxillary permanent molar teeth.
Root canals of teeth with apical periodontitis comprise of gram- negative, gram- positive and mostly anaerobic microorganism.4 The success of a root filling can be compromised if this flora is altered by the ingress of saliva, which would provide a culture medium for any bacteria remaining within the tooth after treatment. Therefore, the isolation of the tooth using a rubber dam is essential to prevent further contamination of the root canal system, and to prevent strong intra canal medicaments escaping into the oral cavity.2
The success of a root filling is also dependent on the chemo-mechanical disinfection of the entire root canal system. Root canal instruments open the canals wide, creating space for the ingress of antibacterial solutions more effectively.5,6 Antibacterial solutions then penetrate the apical constriction and remain in contact with the canal walls and dentine tubules for a sufficient length of time.5 Hsieh et al.7 briefly mentioned that unless the tip of the needle was able to penetrate to 3 mm from the apical constriction, effective irrigation was not achieved. Nickel titanium instruments, with their characteristic super elasticity and shape memory can then be used to negotiate curved canals, reducing the incidence of ledges and perforations. This leads to improved success rates in root canal treatment.
While the quality of shaping of root canals can be seen on a post-operative radiograph, Carrotte6 questioned the old technique of cleaning and shaping, and emphasised more on the importance of firstly opening and shaping the root canals to then create an effective access for antimicrobial irrigant. Because the complex morphology of the root canal system makes it impossible to render sterile.6 the aim, therefore, is to reduce the level of microorganisms and entomb the remaining ones with an effective three dimensional seal. Sodium hypochlorite is the irrigant of choice for this, but some microorganisms are more resistant to the effect of sodium hypochlorite than others.8
After shaping and cleaning, the canals are three-dimensionally filled in a process called obturation. By creating a hermetic seal at the apex, the process of obturation prevents entry of microorganisms into the root canal system from the oral cavity or via the blood system, and prevents the ingress of tissue fluid. Although this is very important, literature states other features such as shaping, cleaning and disinfecting the canals alone could produce favourable outcomes.6 This questions the significance of a radiographically well obturated root filling to the overall success of endodontic treatment. To support this, Dubrow9 suggested obturation was not required for the healing of radiographic periapical areas if there was an adequate seal maintained towards the oral cavity. Klevant and Eggink10 cleaned and shaped a number of root canals. The experimental group was not obturated, though they ensured an effective well sealed coronal restoration. Healing occurred in all cases.
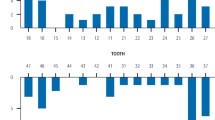
Carrotte6 discusses (Fig. 1) a lower right first molar presenting with a large periradicular lesion. The canal system was shaped and cleaned, with an inter-visit dressing of calcium hydroxide placed. The patient did not return for further treatment for 6 months, where a radiograph was taken (Fig. 2) showing evidence of bony repair, and a return of a normal periodontal ligament around the apex and furcation area was seen.
A large radiolucent area associated with the root apex and furcation area is seen. Reproduced with permission from Carrotte P. Br Dent J 2004;197: 181–183 (Ref. 6)
Reproduced with permission from Carrotte P. Br Dent J 2004;197: 181–183 (Ref. 6)
On the contrary, (Fig. 3) is a radiograph of a lower left second molar taken 12 months after RCT, showing an apparently effective obturation and successful root filling, yet no evidence of healing of the periradicular lesion.6
RCT was carried out 12 months previously, with a seemingly effective obturation, without healing of the peri- radicular lesion. Reproduced with permission from Carrotte P. Br Dent J 2004;197: 181–183 (Ref. 6)
In 1995, Ray and Trope11 found that root treated teeth with a radiographically poor obturation, but a good coronal restoration had a better prognosis than teeth with a good obturation and poor restoration. To ensure a high quality coronal restoration, the coronal seal margins need to be assessed clinically as well as radiographically. This is supported by Tickle et al.12 who categorised root filled teeth into two main groups according to the status of their root filling and the type of restoration placed after the root filling. The results showed that optimal and suboptimal root fillings had very similar failure rates and that a crown provided a greater survival rate than plastic intra coronal restorations. Therefore, a radiographically unsatisfactory root filling can still be successful if the coronal restoration is good.
As commonly acknowledged, root fillings can take up to three clinical sessions to complete. Throughout this, temporary restorations are placed using temporary restorative materials to provide a coronal seal. While temporary restorative materials have good sealing properties, delays in placing a definitive coronal restoration can cause recontamination13 as temporary restorative materials often dissolve in the presence of saliva14 and lose their seal. Although the type of temporary restoration is not visible radiographically, it is important to understand that its long term use could affect the long term success of a root filling even if it is satisfactory radiographically.
The majority of patients suffering from periradicular periodontitis are prescribed RCT because RCT addresses the microbial contamination of the entire root canal system.6 Cases of elective root canal treatment, however, have no periapical pathology15 and they have a good prognosis, as the canals are easy to access and are not infected. The success rate for teeth with periradicular periodontitis pre-operatively, which were subsequently root filled, is 58-86%, compared to a 93-97% success rate of teeth without periapical periodontitis pre-operatively.16
There is little information regarding the effects of medical conditions (such as HIV) or the effects of medically compromised patients (such as those on immunosuppressant therapy) on healing after endodontic procedures. For example, Quesnell et al.17 compared periradicular healing of HIV positive and HIV negative patients one year after endodontic treatment and found no statistical differences between the two groups with respect to degree of periradicular healing. However, Fouad18 found that patients with diabetes had increased periodontal disease in endodontically involved teeth and a reduced likelihood of success in endodontic treatment in cases with preoperative periradicular lesions.
There is no difference in post-operative healing in young and old patients after RCT.19 This is because vascularity is critical to healing and periradicular blood flow in healthy individuals is not impaired with age.20 Smoking, however, does have an adverse effect on vascularity and, therefore, on wound healing.21 When the host is compromised, or if invading microorganisms are sufficiently pathogenic, disease can develop and healing can be delayed. Pathogens such as bacteria which remain in root canals or in periradicular sites due to inadequate disinfection can survive, colonise and evade host defence mechanisms such as neutrophils, complement and antibodies.22 This can delay endodontic healing.
Retreatment
Before deciding to retreat, it is important to use a long enough observation period after treatment has been completed. Healing of periapical tissues is a dynamic process and it is possible that a premature evaluation of periapical healing may occur if the repair process has not yet stabilised.23 Signs and symptoms of infection should be analysed as well.
If the patient had a root filling carried out by another clinician which was radiographically satisfactory but then failed, the current clinician will need more information about the endodontic treatment carried out. The following questions could be considered:
-
Where was the initial RCT performed? It may have been carried out in a dental hospital, general or specialist practice.
-
What techniques were used during RCT? Questioning the patient on the use of rubber dam, the number of radiographs taken and irrigant odours (for example, bleach) during disinfection24 will help the clinician determine the quality of the root filling and whether an improvement can be made on retreatment.
-
What is the functionality of the tooth in the mouth?
If the root filling looks radiographically unsatisfactory but is successful, then it would be beneficial to further monitor this given that the quality of shaping and obturation of the canals are not the only determining features of endodontic success, though they may be the only features presented on an endodontic radiograph.
Conclusion
Similar failure rates for teeth with radiographically optimal and suboptimal root fillings suggest RCT is not as technique sensitive as once thought. Although radiographs provide valuable information, a more unequivocal approach of outcome measurement should be used. For example, a longer radiographic observation period, assessing signs and symptoms of infection, such as pain and discomfort, analysing clinical notes and questioning the patient to determine the conditions in which treatment was conducted.
The following features, which are integral to the success of a root filling, may not be visible on a post-operative radiograph: the quality of disinfection; the appropriateness of medicaments used; signs of apical periodontitis pre-operatively; the use of rubber dam to prevent contamination of the root canals by saliva; and also the quality of intermediate temporary coronal restorations.
Features that are visible on a radiograph which influence success include the number and curvature of canals and the angulation and position of the tooth in the oral cavity. The quality of shaping of the canals with instrumentation is also visible, but should precede chemical disinfection of the canal system. A well condensed radiopaque obturation is important, but studies suggest complete healing can occur without any obturation, provided the canals are effectively disinfected followed by a good coronal seal.
When subjected to stresses, the true character of the root-filled tooth may be surprising. There is limited evidence to suggest that root fillings can fail due to the stresses of age as there is little change in vascularity and nerve supply with aging. There is no conclusive evidence that the stresses of HIV and immunosuppressant therapy on the immune system affect post-operative healing.
It is difficult to decide to retreat a tooth based only on a post-operative radiograph unless a long enough observation period is assessed. A clinician is unlikely to extract a tooth with a radiographically unsatisfactory root filling, or replace its root filling, unless the patient is experiencing recurrent severe symptoms. Therefore, the outcome measure used should include what is most relevant to the clinician and most suitable to patients.
References
Faculty of General Dental Practitioners, Royal College of Surgeons of England. Selection criteria for dental radiography. 2nd ed. Pendlebury M E, Horner K, Eaton K A (eds). London: Royal College of Surgeons of England, 2004.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921–930.
Friedman S . Prognosis of initial endodontic therapy. Endod Topics 2002; 2: 59–88.
Gomes BP, Pinheiro ET, Gade- Neto CR et al. Microbiological examination of infected dental root canals. Oral Microbiol Immunol 2004; 19(2): 71–76.
Carrotte P . A clinical guide to endodontics – update part 1. Br Dent J 2009; 206: 79–84.
Carrotte P . Endodontics: Part 1. The modern concept of root canal treatment. Br Dent J 2004; 197: 181–183.
Hsieh Y D, Gau C H, Kung Wu S F, Shen E C, Hsu P W . Dynamic recording of irrigating fluid distribution in root canals using thermal image analysis. Int Endod J 2007; 40: 11–17.
Radcliffe C E, Potouridou L, Qureshi R et al. Antimicrobial activity of varying concentrations of sodium hypochlorite on the endodontic microorganisms Actinomyces israelii, A. naeslundii, Candida albicans and Enterococcus faecalis. Int Endod J 2004; 37: 438–446.
Dubrow H . Silver points and gutta-percha and the role of root canal fillings. J Am Dent Assoc 1976; 93: 976–980.
Klevant F J, Eggink C O . The effect of canal preparation on periapical disease. Int Endod J 1983; 16: 68–75.
Ray H A, Trope M . Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 1995; 28: 12–18.
Tickle M, Milsom K, Qualtrough A, Blinkhorn F, Aggarwal V R . The failure rate of NHS funded molar endodontic treatment delivered in general dental practice. Br Dent J 2008; 204: DOI:10.1038/bdj.2008.133
Safavi K E, Nichols F C . Effect of calcium hydroxide on bacterial lipopolysaccharide. J Endod 1993; 19: 76–78.
Saunders W P, Saunders E M . Coronal leakage as a cause of failure in rootcanal therapy: a review. Endod Dent Traumatol 1994; 10: 105–108.
Carrotte P . Endodontics: Part 2 Diagnosis and treatment planning. Br Dent J 2004; 197: 231–238.
Friedman S, Mor C . The success of endodontic therapyhealing and functionality. California Dent Assoc J 2004; 32: 493–503.
Quesnell B T, Alves M, Hawkinson R W, Jr Johnson B R, Wenckus C S, BeGole E A . The effect of human immunodeficiency virus on endodontic treatment outcome, J Endod 2005; 31: 633–636.
Fouad A F . Diabetes mellitus as a modulating factor of endodontic infections. J Dent Educ 2003; 67: 459–467.
Walton R . Geriatric endodontics. In Torabinejad M, Walton R E (eds) Endodontics: principles and practice. 4th ed. pp 405–418. Missouri: Elsevier, 2009.
Johnson G . Effects of aging on microvasculature and microcirculation in skin and oral mucosa. In: Squier C A, Hill H (eds) Effect of aging on oral mucosa and skin. pp 99–107. Boca Raton: CRC Press, 1994.
Sjögren U, Figdor D, Persson S, Sundqvist G . Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J 1997; 30: 297–306.
Narayanan L L, Vaishnavi C . Endodontic microbiology. J Conserv Dent 2010; 13: 233–239.
Strindberg L Z . The dependence of the results of pulp therapy on certain factors. An analytic study based on radiographic and clinical followup examinations. Acta Odontologica Scandinavia 1956; 14: 1–175.
Patel S, Kanagasingam S . Dealing with posttreatment disease. In: Patel S, Barnes J J (eds) The principles of endodontics. 2nd ed. pp 144–158. Oxford: Oxford University Press, 2013.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Hansrani, V. Assessing root canal fillings on a radiograph – an overview. Br Dent J 219, 481–483 (2015). https://doi.org/10.1038/sj.bdj.2015.882
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.882
This article is cited by
-
Assessment of the quality of root canal fillings performed on extracted teeth by undergraduate dental students in a sample from Saudi Arabia
BMC Medical Education (2024)
-
An audit of root canal filling quality performed by undergraduate pre-clinical dental students, Yemen
BMC Medical Education (2019)