Key Points
-
Describes the different indications for performing a root canal treatment.
-
Discusses the different technicalities of a root canal treatment in different clinical situations.
-
Discusses the influence of the pre-operative pulpal and peri-radicular status on the treatment outcome.
Abstract
Root canal treatment is a frequently performed procedure aimed to address pulpal and peri-radicular disease. It comprises a number of clinical steps regardless of the initial diagnosis. The emphasis of each step varies according to whether there is a vital pulp (non-infected) or if the pulp system contains necrotic, infected tissue and there is peri-apical pathology. This article aims to discuss the differences in performing root canal treatments on teeth with vital and non-vital pulps. The reader should understand the differences between performing a root canal treatment in teeth with vital pulps and those with infected root canal spaces and peri-radicular pathology.
Similar content being viewed by others
Introduction
When carious lesions extend into dentine, an inflammatory reaction in the pulp is initiated to protect it from bacteria and their toxins.1 If the carious lesion is not treated, the inflammatory reaction increases in intensity to a point at which the pulp cannot recover, a state referred to as irreversible pulpitis. This is frequently associated with pain and may force the patient to seek dental treatment. The treatment of choice in this case, if the tooth is to be retained, is root canal treatment. Relief of symptoms is achieved following extirpation of the inflamed pulp tissue. However, if the situation is not treated (as commonly occurs in cases in which the inflammatory reaction is asymptomatic), the pulp becomes necrotic and eventually the root canal system becomes infected.1 With time, microorganisms and toxins penetrate the dentinal tubules but frequently there are no symptoms. By the time infection reaches the apical foramen, a protective inflammatory reaction is evident in the peri-radicular tissues slowing further progression of the microbial infection.2 The clinical outcome at this stage can be either acute or chronic peri-radicular disease. This depends on several factors including the virulence of the microbial infection and the host defence reaction.2 If the tooth is to be retained, root canal treatment is indicated. The term root canal treatment describes a procedure in which the diseased pulp remnants are removed and pulp space is enlarged and sealed. However, the objectives and technicalities of the root canal treatments performed at each of the above mentioned stages are different. For vital cases, aseptic treatment is aimed at removing the inflamed pulp and providing a fluid-tight seal. In non-vital teeth, a more rigorous anti-septic protocol is required to rid the pulp space of its bacterial colonisation before a fluid-tight seal is provided to prevent re-infection. The differences in managing these two situations are discussed in the following sections and are summarised in Table 1. Root canal re-treatments are considered within the same category as the necrotic infected pulps. Therefore throughout this paper, the two categories to be considered are:
-
Teeth with infection-free vital or irreversibly damaged pulps
-
Those with infected pulp spaces and peri-apical pathology (both treated and de novo cases).
The need for local anaesthesia
Root canal instrumentation should not be undertaken on vital or inflamed pulps without prior anaesthesia, the achievement of which can be challenging, especially in mandibular molars diagnosed with symptomatic irreversible pulpitis. Inferior alveolar nerve blocks (IANB) have been shown to be ineffective in 61–72% of these cases.3 Supplemental anaesthetic techniques are frequently administered to augment the action of IANBs. These include the intra-ligamentary, intra-osseous, intra-pulpal, the Gow-Gates and Vazirani-Akinosi techniques.4 In treatment of teeth with necrotic pulps and peri-apical pathology the primary purpose of anaesthesia is to improve patient comfort. Buccal and lingual infiltrations, which are more accepted than IANB's by patients, are usually sufficient to allow for rubber dam placement and pain-free procedures.
Indication for antibiotics
In healthy individuals with irreversible pulpitis, antibiotics are contra-indicated as they have no role to play in either infection control or pain relief. Their prescription carries the risk of development of one or more of the negative side-effects of antibiotics which may include the development of antibiotic resistance.5 Antibiotics may occasionally be indicated in cases of acute apical abscess where there are signs of systemic involvement, manifesting in symptoms such as pyrexia, tachycardia, swelling, and trismus.6 Also, there is poor antibiotic penetration to sites in which bacterial biofilms are harboured. For teeth with chronic apical periodontitis and chronic apical abscess, antibiotics are rarely indicated in healthy individuals. Therefore, their prescription in these cases should be avoided.
Instrumentation
Coronal flaring
Coronal flaring serves both mechanical and biological roles. If the pulp is vital, coronal flaring serves a predominantly mechanical role by providing a straight-line access to the canal and therefore, reduces the risk of procedural errors.7 In infected teeth, the bulk of the infection is located in the coronal part of the pulp space8 and infection progresses in a corono-apical direction. Therefore, in addition to its mechanical role coronal flaring also removes of the bulk of the coronal infection and creates an irrigant reservoir. It is important to widen and clean the coronal portion of the canal before any attempt at apical instrumentation is made. This step is critical in addressing an infected root canal space as it significantly reduces the risk of carrying the infection to the apical part of the canal system and/or the peri-apical tissues.8
Apical preparation size
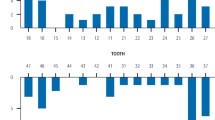
Certain mechanical factors determine the apical preparation size such as tooth type, pre-operative canal size, degree of curvature and the lengths of roots. The presence or absence of infection represents the biologic factor that determines the ideal mechanical shape. In teeth with vital pulps, minimal apical preparation with an appropriate taper is preferable to reduce the risk of procedural errors (Fig. 1). In treatment of infected pulp spaces, mechanical disruption of the bacterial biofilm and the removal of infected dentine are crucial in order for the treatment to be successful. Therefore preparation to larger apical sizes is usually preferable in these cases (Fig. 2).9 Furthermore, larger apical preparations facilitate irrigation which is of more critical consideration in infected teeth.10
The working length
Ideally, canals should be instrumented to the apical constriction, the narrowest cross section of the canal before it opens into the supporting apical tissues. Clinically, location of this point is critical and clinicians rely on apex locator readings in combination with radiographs to ensure a working length that is as close as possible to the apical constriction and not beyond. Teeth with vital pulps are more forgiving as it has been demonstrated that obturation 1–2 mm short of the radiographic apex can leave a vital pulp stump apically without negatively influencing the treatment outcome (Fig. 3).11,12 In infected root canal systems, leaving 1–2 mm of the canal uninstrumented, will most likely result in failure and therefore, instrumentation to the full working length is critical in these cases.11,12
Irrigation
Irrigant selection
In root canal treatment of vital teeth, the pulps are usually inflamed rather than infected. Therefore, the main functions of irrigation are to dissolve pulpal tissue, flush the debris and lubricate instruments. Sodium hypochlorite is the irrigant of choice due to its organic tissue-dissolving ability.13 EDTA, citric acid or other products containing these acids are frequently used as a final flush to remove the inorganic part of the smear layer left following instrumentation.13 Usually there is no need to use other irrigants in these cases.
In teeth with infected pulp spaces, the predominant function of the irrigant is to work as an anti-microbial agent in addition to the aforementioned functions for vital teeth. Sodium hypochlorite is yet again the irrigant of choice due to its tissue dissolving ability and broad-spectrum anti-microbial properties.14 However, other irrigants (such as chlorhexidine, iodine potassium iodide, hydrogen peroxide, electrochemically activated water and antibiotic-based products) and supplemental disinfection methods (such as use of lasers, and electric currents) may be used in addition to sodium hypochlorite to improve disinfection and to combat a wider spectrum of intra-canal bacteria. In these cases, there is a greater need to remove the smear layer which may harbour bacteria with the potential to re-infect canals if sufficient nutritional support can be sustained, therefore the use of EDTA, citric acid or their products is encouraged.15
Irrigant activation
The efficacy of sodium hypochlorite can be enhanced by increasing its concentration, its temperature and by mechanical agitation16 (eg sonic and ultrasonic activation or manual dynamic irrigation using a close fitting gutta percha cone and a pumping action). While increasing its concentration may have adverse effects, should NaOCl be extruded through the apex, increasing its temperature has been shown to significantly improve both its tissue-dissolving ability and its antibacterial effect.16,17
Mechanical agitation results in an improved irrigant exchange, and hence tissue dissolving ability, better penetration within the dentinal tubules and enhanced debris flushing.16 Other simple means of improving the efficacy of NaOCl is to use a larger volume and to increase its time of application.18
In endodontic treatment of infected pulp spaces, it is more critical to use these methods of irrigant activation as the bacterial biofilm – and dentinal tubules – provide protection to the bacteria to escape the chemotherapeutic action of the irrigant. Longer irrigation times, larger volumes and higher temperatures of NaOCl and mechanical agitation can all improve the disinfection procedure. Care must be taken to ensure the irrigant remains within the confines of the root canal to avoid undue consequences of apical extrusion.
Single vs. multiple-visit treatments
In treatment of vital pulps, the emphasis is on removing the inflamed tissue and provision of a fluid-tight seal rather than disinfecting the root canal system. The need for inter-appointment medicaments in these cases is questionable. Furthermore, single visit treatment reduces the risk of coronal leakage and inter-appointment flare-ups.19 Therefore, single visit treatment is preferable for teeth with vital pulps providing that all aspects of the root canal system have been thoroughly debrided and all pulp remnants have been removed. In treatment of infected teeth, the need for meticulous disinfection cannot be over-emphasised. The irrigant must be allowed sufficient time to exert its anti-microbial effect. Single-visit treatments may not provide the clinician with the sufficient time to do so. This becomes more critical in retreatment cases as the majority of the initial appointment time is spent retrieving the old root filling materials, removing posts, crowns and fractured instruments, in order to regain full access to and biological control of the canal system. This reduces the time available for disinfection of the deeper aspects of the root canal system. Indeed the mere process of retreatment itself can fill inaccessible fins and anastomoses with previous filling debris.20 Furthermore, necrotic and infected pulp spaces are frequently associated with either acute or chronic apical abscesses. The clinician may prefer to observe signs of resolution of these peri-apical pathoses before completion of the root canal treatment. Multiple-visit treatment of these cases would therefore seem to be more appropriate.
Definitive restoration
Endodontically-treated posterior teeth are at higher risk of developing vertical root fracture (VRF) compared with their vital non-restored counterparts.21 Restoration of these teeth aims to restore their function and aesthetics, and to provide cuspal protection to reduce the risk of VRF. The timing of the definitive restoration of endodontically-treated teeth can be a matter of debate. On one hand, a definitive restoration is needed as soon as possible to protect the tooth from the wedging occlusal forces that can result in VRF. On the other hand, clinicians may prefer to delay the placement of the final restoration until the RCT is deemed 'successful'. Delaying the definitive restoration however may put the tooth at risk of VRF. Therefore, following RCT of vital pulps, the definitive restoration can be provided as soon as practical, as the resolution of symptoms occur almost immediately following the completion of the RCT. On the other hand, following RCT of infected teeth, it would be wise to delay the placement of the final restoration until there are definitive signs of healing of the peri-apical pathology. During this time, a temporary indirect cuspal protecting restoration should be provided. Protecting vulnerable teeth with a cemented orthodontic band before endodontic treatment will be a reasonable protective compromise in such circumstances.
Length of radiographic follow-up
Root canal treated teeth should be subjected to clinical and radiographic reviews in order that survival and success may be monitored. The absence of symptoms can be checked clinically shortly following the completion of the treatment. Radiographic follow-up should be carried out one year post-operatively.22 If no signs of apical pathology exist, no more review radiographs are required. This is more often the case when the pulp was vital pre-operatively.
In teeth with established intra-radicular infection and large peri-radicular lesions, longer follow-up may be required (up to four years) until the treatment is deemed either successful (complete absence of per-radicular pathology), surviving (incomplete resolution of the peri-radicular pathology with the absence of clinical symptoms) or failing (persistence or deterioration of the apical pathology ± clinical symptoms).22
Treatment outcomes
The fundamental difference in pathology between an infected and non-infected but irreversibly inflamed tooth is reflected in the outcomes of treatment. Success rates of up to 96% have been reported in teeth without pulpal necrosis yet positive outcomes can drop to 62% in infected retreatment cases.23 The presence of periapical pathology can decrease positive outcome rates by up to 49%.24 This difference is not surprising considering the differences in the biology of endodontic disease and the challenges that present to the operator when performing endodontic treatment. It is for this reason that clinicians must diagnose and definitively manage the dying pulp before bacterial ingress occurs. Reassuringly, if root canal treatment protocols are robust with thorough consideration to instrumentation and irrigation regimes, high success rates can be achieved despite the underlying pathology.24
Summary
To summarise, there are significant differences in the objectives and technicalities of root canal treatment of teeth with non-infected vital pulps and those with necrotic and infected pulps with peri-radicular pathology. These differences need to be made clear to the busy general dental practitioner who plays a fundamentally important role to the patient in the management of these scenarios (Fig. 4). This starts with resisting the inappropriate decision to prescribe antibiotics (unless there is systemic involvement) but by offering positive advice regarding prescribable analgesics, but even better still, early intervention with profound analgesia and emergency endodontic management to eliminate acute endodontic pain. This is then followed by more timely provision of the correct root canal treatment appropriate as the case demands and finally a definitive restoration preserving as much natural tooth tissue as possible to optimise the long-term outcome for the tooth.
References
Langeland K . Tissue response to dental caries. Endodon Dent Traumatol 1987; 3: 149–171.
Nair P N R . Pathobiology of primary apical periodontitis. In Cohen S, Hargreaves KM Pathways of the pulp. 9th ed. pp 541–579. Missouri: Mosby, 2006.
Fowler S, Reader A . Is a volume of 3.6 mL better than 1.8 mL for inferior alveolar nerve blocks in patients with symptomatic irreversible pulpitis? J Endod 2013; 39: 970–972.
Hargreaves K M, Keiser K . Local anesthetic failure in endodontics: mechanisms and management. Endod Topics 2002; 1: 26–39.
Jungermann G B, Burns K, Nandakumar R, Tolba M, Venezia R A, Fouad A F . Antibiotic resistance in primary and persistent endodontic infections. J Endod 2011; 37: 1337–1344.
Abbott P V, Hume W R, Pearman J W . Antibiotics and endodontics. Aust Dent J 1990; 35: 50–60.
Weine F S, Kelly R F, Lio P J . The effect of preparation procedures on original canal shape and on apical foramen shape. J Endod 1975; 1: 255–262.
Shovelton D S . The presence and distribution of microorganisms within non-vital teeth. Br Dent J 1964; 117: 101–107.
Baugh D, Wallace J . The role of apical instrumentation in root canal treatment: a review of the literature. J Endod 2005; 31: 333–340.
Ram Z . Effectiveness of root canal irrigation. Oral Surg Oral Med Oral Pathol 1977; 44: 306–312.
Ricucci D, Langelaand K . Apical limit of root canal instrumentation and obturation II. A histological study. Int Endodon J 1998; 31: 394–409.
Wu M K, Wesselink P R, Walton R E . Apical terminus location of root canal treatment procedures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 99–103.
Zehnder M . Root canal irrigants. J Endod 2006; 32: 389–398.
Jungbluth H, Peters C, Peters O, Sener B, Zehnder M . Physicochemical and pulp tissue dissolution properties of some household bleach brands compared with a dental sodium hypochlorite solution. J Endod 2012; 38: 372–375.
Mancini M, Cerroni L, Iorio L, Armellin E, Conte G, Cianconi L . Smear layer removal and canal cleanliness using different irrigation systems (endoactivator, endovac, and passive ultrasonic irrigation): field emission scanning electron microscopic evaluation in an in vitro study. J Endod 2003; 39: 1456–1460.
Stojicic S, Zivkovic S, Qian W, Zhang H, Haapasalo M . Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod 2010; 36: 1558–1562.
Sirtes G, Waltimo T, Schaetzle M, Zehnder M . The effects of temperature on sodium hypochlorite short-term stability, pulp dissolution capacity, and antimicrobial efficacy. J Endod 2005; 31: 669–671.
Zou L, Shen Y, Li W, Haapasalo M . Penetration of sodium hypochlorite into dentin. J Endod 2010; 36: 793–796.
Siqueira Jr J F . Microbial causes of endodontic flare-ups. Int Endod J 2003; 36: 453–463.
Zehnder M, Paque F . Disinfection of the root canal system during root canal re-treatment. Endod Topics 2011; 19: 58–73.
Fuss Z, Lustig J, Tamse A . Prevalence of vertical root fractures in extracted endodontically treated teeth. Int Endodon J 1999; 32: 283–286.
European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J 2006; 39: 921–930.
Sjögren U, Hägglund B, Sundqvist G, Wing K . Factors affecting the long-term results of endodontic treatment. J Endod 1990; 16: 498–504.
Ng Y L, Mann V, Gulabivala K . A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J 2011; 44: 583–609.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
El-Ma'aita, A., Qualtrough, A., Darcey, J. et al. Rethinking root canal treatment: understanding the difference between preventing and treating endodontic infection. Br Dent J 219, 13–16 (2015). https://doi.org/10.1038/sj.bdj.2015.527
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.527