Key Points
-
Analyses the trends in high concentration fluoride toothpaste (HCFT) prescribing in Scotland.
-
Highlights there has been a significant increase in the prescription of 2,800 ppm and 5,000 ppm fluoride toothpaste.
-
Encourages prescription of HCFT as best practice care but also suggests it should be managed appropriately to ensure that its delivery is targeted at those who are most in need.
Abstract
Within Scotland there has been a significant increase in the prescription of 2,800 ppm and 5,000 ppm fluoride toothpaste. The objective of this paper was to analyse the trends in high concentration fluoride toothpaste (HCFT) in the five Scottish South East and Tayside (SEAT) health boards and consider the options for future national management of this prescribing. A retrospective analysis of routine prescribing data for the years 2006-2012 was carried out in primary care dental practices in Scotland. The cost of HCFT prescribing in the five Scottish health boards has increased from £15,243 (4,147 items) in 2006/07 to £206,529 (24,113 items), in 2011/12. Out of 2,430 dental list numbers, 100 list numbers (4.1%) accounted for 70% of the total prescribing costs (£144,367). The public dental service employs 153 (6%) of dentists working in Scotland, who in turn prescribe 11.6% HCFT. There is a need to ensure that the prescription of HCFT is both encouraged as best practice care but also managed appropriately to ensure that its delivery is targeted at those who are most in need.
Similar content being viewed by others
Introduction
The five East of Scotland health boards: NHS Borders, NHS Fife, NHS Forth Valley, NHS Lothian, and NHS Tayside; form part of a regional planning group known as SEAT (South East and Tayside). SEAT has a population of around two million people, 39% of the Scottish population.1
Within these health boards dental prescribers work on an independent contract or within the public dental service providing National Health Service (NHS) dentistry to their respective populations. Traditionally the independent service provides more general care while the public dental service has more of a focus on caring for children and priority groups. In addition a minority2 of dental care is provided privately to the Scottish public.
There have been a number of recent initiatives that have potentially influenced dental prescribing of high concentration fluoride toothpaste (HCFT). From 2006 dentists were allowed to prescribe, along with their medical colleagues, HCFT. In March 2008 the Scottish Dental Clinical Effectiveness Programme (SDCEP) released the first edition of the guidance Drug prescribing for dentistry.3 Other documents that could have influenced prescribing include the SDCEP guidance, Prevention and management of dental caries in children,4 SIGN 43 guidance5 and Delivering better oral health – an evidence-based toolkit.6 In April 2011 the Scottish Government introduced free prescribing for all patient groups. In 2012 the National oral health improvement strategy for priority groups7 was released as a guidance document for Health Boards to manage the oral healthcare in this population.
Since part of the role of dental public health is to ensure that appropriate dental care is provided to patients, an analysis of dental prescribing across all SEAT health boards was undertaken.
The analysis focused on the type, quantity and cost of dental prescribing. Within this analysis it was noted that although prescribing costs in general had not increased, there was a significant increase in both the amount and subsequent cost of HCFT. This paper describes the underlying patterns behind the increasing trend in the prescribing of HCFT, and discusses the authors' thoughts on how this indicator of best practice could inform public health strategies to support the provision of optimal preventive dental care for the Scottish population.
Materials and methods
Prescribing data for dentists from each SEAT health board was obtained for the period 2006-2012 from the PRISMS8 database, which contains information on all prescriptions dispensed in Scotland over the past 5 years. The PRISMS database is held centrally and is updated monthly. The data can be interrogated to provide reports at individual dentist level and can be aggregated up to practice, health board and Scotland levels.8
An initial analysis was undertaken of the prescribing patterns of all dentists who prescribe HCFT. Following this analysis additional information on the prescription of HCFT for every dentist by prescriber number was obtained. Prescribers were then categorised as either public dental service or independent dental service following communications with local clinical directors. This additional data was only obtained for the year 2011.
Specific objects of the prescribing analysis were to determine if in the SEAT health boards;
-
1
The prescription of HCFT had increased
-
2
There was a difference between the prescribing patterns of dentists who work within the public dental service compared with those in the independent dental service
-
3
The prescription of HCFT was evenly distributed across all dentists
-
4
The prescription of HCFT was targeted to specific population groups.
In addition the prescribing analysis would allow the authors to consider the options and the cost implications of future national management of this prescribing.
Results
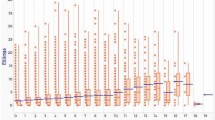
Over the last 5 years there were 73,874 prescriptions dispensed of HCFT. Figure 1 illustrates the rise in the prescribing of HCFT items in the SEAT health boards. The number of items prescribed rose from 4,147 items in 2006/07 to 24,113 items in 2011/12 – an almost six-fold increase.
There were 153 dentists employed by the public dental service, accounting for 6% of the dentist workforce in the SEAT health boards. The public dental service prescribed, by item, approximately 11.6% of the total HCFT within the SEAT region. The rest of the HCFT was prescribed by the independent dental sector.
There were considerable differences across dentists in the amount of HCFT prescribed. Out of 2,430 list numbers within SEAT just 100 list numbers (4.0%) were responsible for 70% of the total items prescribed. The abolition of prescription charges means that pharmacists are no longer required to record the exemption categories (for example, widows pension, job seekers allowance). In addition few dental prescribers currently use the Community Health Index (CHI). It was therefore not possible in this analysis to determine which population group was receiving a higher proportion of HCFT.
Discussion
Current guidance recommends the provision of HCFT to individuals who are at high risk of dental decay.3,4,5,6,7 The provision of HCFT to people at increased risk of dental decay is in keeping with NHS free at point of care service and may also be an effective low cost way of reducing dental disease in a patient at increased risk of dental caries. Scotland already has an innovative, preventive oral care programme for children, Childsmile (www.child-smile.org), which provides toothbrushes and toothpaste and toothbrushing programmes, plus additional targeted support where necessary. With the increase in HCFT prescribing it is important that the use of HCFT is equitable, appropriate, and cost effective.
Equitable provision
Equitable provision would mean that every person who needs higher fluoride toothpaste due to their risk of dental caries would be able to access the product. However, determining whether the current practice of prescribing HCFT is equitable is difficult due to lack of comprehensive data. In Scotland patients are provided with a unique ten-digit number, the CHI; this could be used to collect information from prescriptions.
The public dental services have a higher proportion of patients with special needs. In a recent needs assessment of the NHS Lothian Salaried dental service, 68% of the adult patients seen by the service had some form of special need.9 People with special needs are more likely to be at a high risk of dental disease.10 Consequently as anticipated there is higher prescribing of HCFT in the public dental services, consistent with the guidance that encourages the prescription of HCFT within these groups.
The finding that just 4% of list numbers across the public and independent dental sectors are responsible for 70% of HCFT prescribing does require further examination.
Appropriate care
While good evidence exists to support the use of fluoridated toothpaste twice daily to reduce caries in children,11 there are only a small number of trials to support the use of HCFT.12,13 There are a number of guidance documents that advise the provision of HCFT to high-risk children and adults.3,4,5,6,7 However, the number of trials on the efficacy of topical fluoride use in adults and special needs groups is limited. In addition there is need for research on longer term use of HCFT or alternative topical fluoride agents to determine the most effective and appropriate approaches.
Cost effectiveness
The current prescription spend (2012) on fluoride toothpaste within the SEAT health boards is £206,529, with a HCFT costing £3.26 for 2,800 ppm toothpaste and £6.50 per prescription for 5,000 ppm toothpaste.14
To consider the cost effectiveness of this product one needs to consider how for the same given outcome (reduction in dental caries) the cost of toothpaste compares with other similar products, whether the cost paid for the product is reasonable and whether there are other more cost effective ways of providing the product.
Comparison with other products
Based on the SDCEP recommendations for HCFT use ('use three times daily') one tube of toothpaste (with an average dose of 12 mg per day) would provide a person with enough HCFT for 20 days. However, considering the traditional habit of brushing twice a day a tube of toothpaste would last about a month. A study by Ekstrand found 22,600 ppm fluoride varnish and the 5,000 ppm fluoride toothpastes were equally effective at reducing dental decay but, because of the cost of the hygienist, the cost analysis found that fluoride varnish was more than 30 times more expensive to provide.15
Cost of providing product is reasonable
The Pharmaceutical Price Regulation Scheme (PPRS) is the mechanism that the Department of Health (on behalf of the UK health departments) uses to ensure that the NHS has access to good quality branded medicines at reasonable prices. There are only two high strength toothpastes available in the UK; Duraphat 5,000 ppm fluoride and Duraphat 2,800 ppm fluoride16 on prescription. Currently the pharmacist receives £3.26 for 2,800 ppm toothpaste, and £6.50 for every 5,000 ppm product they supply to a patient. Within Childsmile the cost to the Scotland of providing toothpaste under national procurement is cheaper. National procurement of toothpaste may be a considerably cheaper way of providing HCFT to the relevant section of the population
There are insufficient studies demonstrating the increased benefits of the use of 5,000 ppm over 2,800 ppm. The Scottish Government should consider the benefits of providing 5,000 ppm toothpaste (in comparison with 2,800 ppm) on free prescription.
Future developments
Dentists have been allowed to prescribe HCFT since 2006. It is only recently that guidance has highlighted the importance of prescribing this product to high risk groups. The product diffusion model illustrates how a new product or intervention is taken up by a group; this usually involves a small number (for example, 2.5%) of innovators taking up a new process, followed by a slightly larger number (13.5%) who are known as early adopters.17 The fact that 100 list numbers (4.1%) account for 70% of the total prescribing costs (£144,367) gives support to the fact that the adoption of prescribing of HCFT is currently being prescribed by early adopters. As more dentists prescribe HCFT this may result in substantial increases in prescribing costs for the Scottish Government.
The Scottish Government needs either to manage the increasing costs of HCFT over the next few years, or consider alternative ways of funding. The authors of this paper suggest three options to control funding.
Cease provision under the Pharmaceutical Price Regulation Scheme
The cessation of prescribing of HCFT is probably not a good long term option for the Scottish Government. Provision of no cost fluoride toothpaste to at risk groups should, in the long term improve oral health resulting in a reduction in costs to the Scottish Government, in a similar mechanism to Scottish toothbrushing programmes.18 The Scottish government currently spends £400 million providing dental care to its population.
Consider a national tender to procure HCFT
The Scottish Government could provide HCFT to the general public using a similar procurement process to the current Childsmile model. There are other companies who produce HCFT including Sensodyne NUPRO 5,000 ppm,19 Clinpro 5,000ppm 1.1% Sodium Fluoride20 and Medical 5,000ppm.21 Providing a guaranteed minimum purchase of product may support the entry of additional suppliers into the market, which may encourage competition. This may enable the continued provision (and expansion) of HCFT to the public while reducing cost.
Consider the 'value' of the current toothpaste paste available on prescription
Value based pricing is shortly to be introduced by the UK government. Value based pricing looks not only at the profits of prescription supply companies, but the cost effectiveness of each product available under PPRS. Any reduction in the cost of HCFT may ultimately influence the cost of HCFT paid by the government under the PPRS system. Working with National Procurement (Scotland) it would be beneficial for any reduced tender price to influence the cost of a prescription and ensure best value for money.
Conclusion
In conclusion, there is a need to ensure that the prescription of HCFT is both encouraged as best evidence-based care but also managed appropriately to ensure that its delivery is targeted at those in the population who are most in need.
References
General Register Office for Scotland. Mid-year estimates. Online estimates available at http://www.gro-scotland.gov.uk/statistics/theme/population/estimates/mid-year/ (accessed March 2014).
Office of Fair Trading. The private dentistry market in the UK, 2003. London: OFT, 2013.
Scottish Dental Clinical Effectiveness Programme. Drug prescribing for dentistry. 2nd Ed. Dundee: SDCEP, 2011. Online guidelines available at http://www.sdcep.org.uk/?o=2334 (accessed March 2014).
Scottish Dental Clinical Effectiveness Programme. Prevention and management of dental caries in children. Dundee: SDCEP, 2010. Online guidelines available at http://www.sdcep.org.uk/index.aspx?o=2332 (accessed March 2014).
Scottish Intercollegiate Guidelines Network. Preventing dental caries in children at high caries risk. Targeted prevention of dental caries in the permanent teeth of 6–16 year olds presenting for dental care. SIGN, 2000. Online guidelines available at http://www.sign.ac.uk/pdf/sign47.pdf (accessed March 2014).
Department of Health, British Association for the Study of Community Dentistry. Delivering better oral health: an evidence-based toolkit for prevention. London: DH, 2009.
National oral health improvement strategy for priority groups: frail older people, people with special care needs and those who are homeless. Scottish Government, 2012. Online article available at http://www.scotland.gov.uk/Publications/2012/05/7031 (accessed March 2014).
Information Systems Scotland. PRISMS: prescribing and medicines. Online information available at http://www.isdscotland.org/Health-Topics/Prescribing-and-Medicines/PRISMS/ (accessed March 2014).
NHS Lothian special care dentistry service review 2013. Available on request.
Gallagher J E, Fiske J . Special care dentistry: a professional challenge. Br Dent J 2007; 202: 619–629.
Marinho V C C, Higgins J P T, Logan S, Sheiham A . Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Summaries, 2009. Online article available at http://summaries.cochrane.org/CD002278/fluoride-toothpastes-for-preventing-dental-caries-in-children-and-adolescents#sthash.XXTmX9L2.dpuf (accessed March 2014).
Nordström A, Birkhed D . Preventive effect of high-fluoride dentifrice (5,000 ppm) in caries-active adolescents: a 2-year clinical trial. Caries Res 2010; 44: 323–331.
Dreizen S, Brown L R, Daly T E et al. Prevention of xerostomia-related dental caries in irradiated cancer patients. J Dent Res 1977; 56: 99–104.
National Institute for Health and Care Excellence. Duraphat. Online information available at http://www.evidence.nhs.uk/formulary/bnfc/current/9-nutrition-and-blood/95-minerals/953-fluoride/fluorides/toothpastes/duraphat (accessed March 2014).
Ekstrand K, Martignon S, Holm-Pedersen P. Development and evaluation of two root caries controlling programmes for home-based frail people older than 75 years. Gerodontology 2008; 25: 67–75.
Colgate. Dentistry products: Colgate Duraphat 2,800 ppm fluoride toothpaste. Online information available at http://www.colgateprofessional.co.uk/products/Colgate-Duraphat-2800ppm-Fluoride-Toothpaste/details (accessed March 2014).
Quick MBA. Product diffusion curve. Online information available at http://www.quickmba.com/marketing/product/diffusion/ (Accessed March 2014).
Anopa Y, Macpherson L M, Ball G E, McMahon A D, Conway D I, McIntosh E . Economic burden of childhood caries: cost analysis of national nursery toothbrushing programme. EADPH September 2013, Poster No. 2317.
DENTSPLY. Sensodyne® NUPRO® 5,000 ppm professional fluoride ion toothpaste with NovaMin™. DENTSPLY, 2011. Online information available at http://www.nupro-sensodyne.com/lib/pdf/toothpaste-product-list.pdf (accessed March 2014).
3M ESPE. Clinpro™ 5000 1.1% sodium fluoride anti-cavity toothpaste. Online information available at http://solutions.3m.com/wps/portal/3M/en_US/3M-ESPE-NA/dental-professionals/products/espe-catalog/∼/Clinpro-5000-1-1-Sodium-Fluoride-Anti-Cavity-Toothpaste?N=5144762+3294768934&rt=rud (accessed March 2014).
Remineralizing Oral Care Systems. R O.C S. Medical 5,000 ppm high fluoride toothpaste. Online information available at http://www.rocs.ru/toothpaste_medical_5000_ppm_eng.html (accessed March 2014).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Duane, B., Richards, D., Young, L. et al. Trends and costs of high concentration fluoride toothpaste prescribing in Scotland. Br Dent J 216, 589–591 (2014). https://doi.org/10.1038/sj.bdj.2014.397
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.397