Key Points
-
Describes the micro-anatomy of the apical terminus for a root canal system and different methods of measuring root canal system length.
-
Describes basic physics, current electricity and how teeth can function as capacitors.
-
Describes how this capacitor model represents a starting point upon which all apex locators are based.
Abstract
To effectively carry out root canal therapy, the clinician must accurately determine the apical limit of the root canal system as well as the position of the canal terminus. Its position can be estimated using a variety of techniques, including radiographs, tactile feedback from endodontic instruments and electronic apex locators. This article describes the micro-anatomy of the apical terminus, different methods of measuring root canal system length and how a tooth can function as an electrical capacitor. This capacitor model represents a starting point upon which all apex locators are based. An understanding of this model can help the practitioner to optimise the use of apex locators, understand their limitations and avoid errors that can occur.
Similar content being viewed by others
Introduction
An inflammatory response in the pulp-dentinal complex can lead to complete pulpal necrosis, apical periodontitis and ultimately the formation of a dental abscess. If the tooth is to be asymptomatically retained, root canal therapy (RCT) must be implemented. The aims of RCT include:
-
1
Accessing the root canal system (RCS)
-
2
Chemo-mechanical debridement of the RCS1
-
3
Shaping the RCS to accept a root canal filling (RCF) material
-
4
Obturating the RCS
-
5
Providing cuspal coverage post endodontic treatment for posterior teeth2 (Fig. 1).
To effectively carry out the above stages, the clinician must accurately determine the apical limit of the RCS as well as the position of the canal terminus. The latter is especially true as the systematic review by Ng et al.3 strongly suggests that RCFs which extend beyond or are more than 2 mm short of the radiographic apex are associated with a higher chance of endodontic failure. It is therefore imperative that the clinician can identify the point at which the root canal system terminates.
Electronic Apex Locators (EALs) can be used to determine the length of a RCS and the position of the canal terminus. This two-part series of articles will update readers on our current understanding of apex locators. This first part will focus on (a) the anatomy of the apical terminus, (b) methods of determining the apical limit of the RCS and (c) basic physics of the instrument. The second part will discuss (a) how EALs work (b) how accurate they are in clinical practice and (c) practical points on how best to use them.
The Anatomy of the Apical Terminus
To appreciate the workings of an EAL, an understanding of the micro anatomical features of the apical terminus is essential.
Kuttler elegantly described the anatomy of the apical terminus.4 The foramen of the main root canal (the major apical foramen) is not always coincident with the radiographic or anatomical apex. It is situated at the tip of the root but is often located to one side of the anatomical apex (Fig. 1). Reported mean apex to foramen distances vary from 0.3 mm to 0.6 mm but distances of up to 3 mm have been reported.4,5 Deposition of cementum at the root apex over time also means that the discrepancy between the major apical foramen and the root tip increases with age.6 Furthermore, deviation of the major foramen can also occur as a result of pathological changes such as external root resorption.7
The major apical foramen is considered to lie entirely in cementum, from which the cementum narrows upwards into the minor apical foramen, also called the apical constriction (AC). The location of the AC can be highly variable between different RCSs8 and may not be present in all teeth. It is thought to be at (or close to) the point where the cementum fuses with radicular dentine (the cemento-dentinal junction, CDJ).9
The CDJ is considered to represent the point at which the RCS terminates and the periodontium begins.4,9,10 It represents the ideal apical limit for root treatment as there would be minimal contact between an endodontic instrument and the peri-radicular tissues at this point.10,11 This would minimise any mechanical trauma to the periodontal ligament during endodontic preparation. However, the CDJ cannot be detected clinically, only histologically after a tooth has been extracted and sectioned. Furthermore, it is a highly irregular reference point as in some cases, the CDJ can be up to 3 mm higher on one wall of the RCS compared with the opposite wall12 (Fig. 2). As such, it is not a practical landmark to use when terminating a root canal preparation/obturation.
Micro-anatomical features of the apical terminus (modified from Kuttler5)
The minor apical foramen/apical constriction (AC) is the narrowest point of the root canal system. It is on average 0.5 to 1.0 mm short of the radiographic apex but there can be considerable discrepancy in terms of location between the two landmarks.11,13 Although the AC can demonstrate considerable morphological variation between teeth,14 it is a consistent anatomical reference point. It is a more practical landmark to use when terminating a root canal preparation, compared to the CDJ.
Methods for determining the length of the RCS
In addition to EALS, there are several techniques that can be used to determine the length of the RCS and the position of the canal terminus.
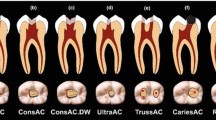
1. Tactile feedback from endodontic instruments
The tactile sensation afforded by hand instruments during endodontic instrumentation can be useful at determining the position of the AC. However, even experienced endodontists could only detect the landmark in 60% of cases using tactile sensation alone.15 Although pre-flaring the orifice of the RCS can increase the clinicians ability to 'feel' the AC by up to 75%16 this method clearly has limitations in cases where the canal is sclerosed or the landmark itself has been obliterated by inflammatory resorption.6,17 Furthermore the topography of the AC can vary considerably from tooth to tooth14 (Fig. 3). This coupled with the fact that there will be considerable variation between the clinician's ability to accurately 'feel' the AC18 makes this technique of length determination unreliable.
The varying topographies of the apical terminus (from Dummer et al.14)
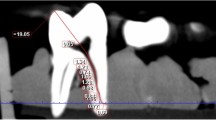
2. Radiographic determination of the working length (WL)
The use of a periapical radiograph (taken with a paralleling device) with an endodontic file in the RCS is a popular way to determine the WL. Coupled with the clinician's knowledge of dental anatomy and the average lengths of root canal systems, this can be a useful method. Although the image provides valuable information regarding the shape and curvature of the root apex, it is only a two-dimensional representation of a three-dimensional structure. It is based on the premise that (on average) the AC lies 0.5 to 1.0 mm short of the radiographic apex.13 This assumption has probably led to the common teaching practice of terminating a RCF 1.0 mm short of the radiographic apex.6 However, this technique is inherently flawed in that the position of the AC from the radiographic apex can vary considerably from tooth to tooth. In some case, it can be up to 3.8 mm short of the radiographic apex12 leaving potential for the RCS to be over-instrumented. Furthermore the apical foramen is not always co-incident with the radiographic apex. It is often to one side of the apex in a buccal or palatal direction making it difficult to visualise radiographically.11,19 It is therefore not surprising that numerous studies have revealed considerable variation between the radiographic working length and the actual working length of a tooth.14,20,21
Radiographs are technique sensitive in terms of interpretation22 and involve exposing the patient to ionising radiation. In addition, superimposition of other structures (such as dense bone, the zygomatic buttress, metal plates) over the root apex can make visualisation difficult. It is thus logical to always supplement a radiographically determined WL with some other WL reading (such as a length determined from an EAL).
3. The paper point technique
This has been well described by Rosenberg23,24 and is dependent on having achieved apical patency. This technique is based on the premise that the RCS of an uninfected tooth is dry while the external periodontium is wet, hydrated tissue. It has been suggested that the dry/wet interface should be the apical limit of a RCF material. This seems logical as any point beyond the interface would be exposed to the body's defence mechanisms (and therefore amenable to apical healing). The RCS is relatively well protected by the dentinal layer and is therefore more inaccessible to the host's defence mechanisms.25
The technique itself involves preparing the RCS to a point 0.5 mm short of the apical constriction (as determined by an EAL). The RCS is then dried. A paper point is selected which has a taper less than that to which the RCS was prepared. It is then advanced to the point where moisture is detected on its tip. A second point is then advance to a point 1-2 mm shy of the 'wet' length and checked for moisture. If the point is dry, it should be advanced 0.5 mm at a time until moisture is detected. Using this technique, it will be possible to detect the dry/wet interface and therefore the apical limit of the proposed RCF. Although this technique is useful when managing teeth with open apices or abnormal apical anatomy, it cannot be used in cases where it is impossible to dry the canal (due to inflammatory exudate) or achieve apical patency. Furthermore there have been no prospective, controlled and blinded trials which have been carried out to verify the effectiveness of this technique.
Basic Physics and Current Electricity
An understanding of physics and current electricity is essential to appreciate the operating principles of an EAL. A number of terms and concepts in this field will be briefly discussed. For a full summary, the reader is advised to consult the works of Nekoofar et al.:11
Voltage (V): Also known as potential difference and measured in volts. It provides the driving force/energy to allow charged particles to move through an electrical circuit. It is therefore the driving force in any electric circuit.
Current (I): Refers to the movement of charged particles (electrons or ions) throughout a circuit and is measured in amperes. Direct current (DC) refers to a fixed amount of current per unit time while alternating current (AC) refers to a phenomenon where the amount of current under investigation alternates over time.11
Resistance (R): Refers to a material's ability to resist the movement of charged particles within it. It varies with the type of material under investigation and is measured in Ohms. The resistance of an object depends on three factors: its resistivity ρ (a constant value at a given temperature), length (l) and cross sectional area (A). The relationship between these three factors is expressed by the formula:
Equation 1: R = (ρ × l)/A
Clearly an increase in length or resistivity will lead to an increase in resistance while an increase in cross-sectional area decreases resistance. An insulator is a material that has a high resistivity and thus offers high resistance to the movement of electrons or ions.11 The term 'resistance' strictly applies to DC while the term 'impedance' is reserved for AC. The latter is comprised of the resistance and capacitance of the circuit under investigation.
Ohm's Law: describes the mathematical relationship between all three components required for an electrical circuit to function:
Equation 2: V = I × R
By this equation, keeping the V constant would increase the flow of I if the R is decreased.
Capacitor: this refers to any structure consisting of two conductive materials sandwiching an insulator (or a dielectric). It is able to store charge. The amount of charge it stores is called its capacitance (C) and is dependent on the nature of the insulating material between the plates (the dielectric constant or ε), the distance between the conductors (D) and their surface areas (A). These features can be compared to an endodontic instrument in the RCS of a tooth, surrounded by the periodontium. Therefore a tooth also has the ability to act as a capacitor, a feature exploited by modern EALs. The relationship between C and its variables is shown by the equation:

The tooth as a capacitor
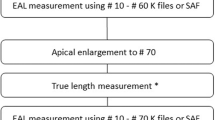
A tooth can be compared to a capacitor. Dentine and cementum are insulators of current. The periodontal ligament (PDL), the AC and a file in the RCS are all conductors of electricity. Therefore an advancing file in the RCS and the PDL surrounding the radicular dentine will act as the conductors in a capacitor. The dentine, cementum and any associated fluid or tissue within the RCS will act as the insulator of the system and will have its own dielectric constant (ε)11 (Fig. 4).
This model (Fig. 4) represents a starting point upon which all EALs are based. An electrical circuit is formed that starts from the EAL, runs through a clip on an endodontic file, through the root canal, through the AC, out the PDL and finally through the mucosa and onto a clip on the patient's lip. The circuit is complete when the current returns to the device. EALs extrapolate the position of the file in the canal by measuring the resistance, impedance, capacitance (or some variant or combination of these) in the electrical circuit formed. An understanding of this can help the practitioner to optimise their use, understand their limitations and avoid errors that can occur.
Discussion
This first paper has introduced the reader to the micro-anatomical features of the apical terminus and discussed how a tooth can function as a capacitor. This is a gross over-simplification of a highly complex electrical network, as discussed by Meredith and Gulabivala.26 It does, however, serve as a useful model when understanding the mechanics of an EAL. These principles will be developed in the next paper where readers will be introduced to different EALs, their relative accuracies and methods to optimise their success in clinical practice.
References
Chugal N . Clive J, Spangberg L . Endodontic infection: some biologic and treatment factors associated with outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 81–90.
Heling B, Gorfil C, Slutzky H et al. Endodontic failure caused by inadequate restorative procedures: review and treatment recommendations. J Prosthet Dent 2002; 87: 674–678.
Ng Y-L, Mann V, Rahbaran S, Lewsey J, Gulabivala K . Outcome of primary root canal treatment: systematic review of the literature - Part 2. Influence of clinical factors. Int Endod J 2008; 41: 6–31.
Kuttler Y . Microscopic investigation of root apexes. J Am Dent Assoc 1955; 50: 544–552.
Green D . Stereomicroscopic study of 700 root apices of maxillofacial and mandibular posterior teeth. Oral Surg Oral Med Oral Path 1960; 13: 728–733.
Gordon M P J, Chandler N P . Electronic apex locators. Int Endod J 2004; 37: 425–437.
Malueg L, Wilcox L, Johnson W . Examination of external apical root resorption with scanning electron microscopy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82: 89–93.
Ponce E H, Fernandez J A V . The cemento-dentinal-canal junction, the apical foramen, and the apical constriction: evaluation by optical microscopy. J Endod 2003; 29: 214–219.
Kuttler Y . A precision and biologic root canal filling technique. J Am Dent Assoc 1958; 56: 38–50.
Ricucci D Apical limit of root canal instrumentation and obturation, part 1. Literature review. Int Endod J 1998; 31: 384–393.
Nekoofar M H, Ghandi M M, Hayes S J, Dummer P M H . The fundamental operating principles of electronic root canal length measuring devices. Int Endod J 2006; 39: 595–609.
Gutierrez J H, Aguayo P . Apical foraminal openings in human teeth. Number and location. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995; 79: 769–777.
Katz A, Tamse A, Kaufman A Y . Tooth length determination: a review. Oral Surg Oral Med Oral Pathol 1991; 72: 328–342.
Dummer P M, McGinn J H, Rees D G . The position and topography of the apical canal constriction and apical foramen. Int Endod J 1984; 17: 192–198.
Seidberg B H, Alibrandi B V, Fine H, Logue B . Clinical investigation of measuring working lengths of root canals with an electronic device and with digital-tactile sense. J Am Dent Assoc 1975; 90: 379–387.
Stabholtz A, Rostein I, Torabinejad M . Effect of preflaring on tactile detection of the apical constriction. J Endod 1995; 21: 92–94.
Stock C . Endodontics – position of the apical seal. Br Dent J 1994; 176: 329.
Chandler N P, Bloxham G P . Effect of gloves on tactile discrimination using an endodontic model. Int Endod J 1990; 23: 97–99.
Sheaffer J, Eleazer P, Scheetz J, Clark S, Farman A . Endodontic measurement accuracy and perceived radiographic quality: effects of film speed and density. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96: 441–448.
Martinez-Lozano M, Forner-Navarro L, Sanchez-Cortes J, Llena-Puy C . Methodological considerations in the determination of working length. Int Endod J 2001; 34: 371–376.
Green D . A stereomicroscopic study of the root apices of 400 maxillary and mandibular anterior teeth. Oral Surg Oral Med Oral Pathol 1956; 9: 1224–1232.
Cox V S, Brown CE Jr, Bricker S L, Newton C W . Radiographic interpretation of endodontic file length. Oral Surg Oral Med Oral Pathol 1991; 72: 340–344.
Rosenberg D B . The paper point technique, Part 1. Dent Today 2003; 22: 62–67.
Rosenberg D B . The paper point technique, Part 2. Dent Today 2003; 22: 80–86.
Robinson S, Brunton P . Endodontic length determination: what lengths should we go to? Dent Update 2008; 35: 678–683.
Meredith N, Gulabivala K . Electrical impedance measurement of root canal length. Endod Dent Traumatol 1997; 13: 126–131.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Ali, R., Okechukwu, N., Brunton, P. et al. An overview of electronic apex locators: part 1. Br Dent J 214, 155–158 (2013). https://doi.org/10.1038/sj.bdj.2013.161
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2013.161