Key Points
-
Altered quality and quantity of enamel can make the attaching and retaining of a fixed brace problematic.
-
An idealised orthodontic occlusion is not always the treatment goal at the end of the orthodontic phase, as the multidisciplinary nature implicit in the management of AI needs to be considered.
-
Attention needs to be paid to motivate the patient as compliance is key to attaining a successful outcome.
Abstract
Orthodontics in patients with amelogenesis imperfecta can be complicated by commonly occurring dental features in this group as well as patient factors. In this article we examine ways to avoid the common pitfalls of orthodontic management and the importance of adequate and timely liaison between the general dental practitioner and the multidisciplinary team.
Similar content being viewed by others
Introduction
Amelogenesis imperfecta (AI) is a rare developmental abnormality of tooth enamel, with variable occurrence of approximately 1:4,000 to 1:14,000 in Western populations.1,2,3,4,5 Amelogenesis imperfecta results in poor development or complete absence of tooth enamel of the teeth caused by improper differentiation of ameloblasts6 and affects the deposition, mineralisation and maturation of enamel in both the primary and the permanent dentitions. The presentation and effects of this condition have previously been described in part 1 of this series.boxed-text
The orthodontist's role usually begins in the late mixed dentition unless other concomitant orthodontic challenges such as failure of eruption of a central incisor arise in the early mixed dentition.
Early and vigorous monitoring of AI patients by the general dental practitioner and/or the paediatric team will allow timely and effective 'interceptive' means to be applied. It must be remembered that interceptive orthodontics should only be instigated when it will substantially decrease the severity and complexity of later treatment. This caveat is particularly important in the management of this group of patients who require maximum motivation for what is usually an extensive range of dental treatment, lasting several years. Ineffective interceptive measures could rapidly exhaust a patient's compliance.
The orthodontist plays a pivotal role in closely monitoring the developing dentition and placing the patient's teeth in the ideal position for definitive restorations and/or orthognathic surgery that may be needed.
There may be psychological concerns from the patient's point of view, particularly if the appearance of the dentition is a cause of bullying, and therefore treatment may be sought earlier to improve self confidence and esteem.7,8
Associated dental features of orthodontic relevance
The common dental features associated with AI and their effect on orthodontic management are described below.9,10,11
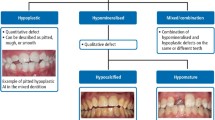
Quantitative and qualitative enamel deficiencies
This can be a challenging problem for the modern day orthodontist. The difficulty when using fixed appliances is for the orthodontist to manage the weak enamel and determine whether the enamel can withstand the forces both applied during treatment and when removing the appliances.
Conventionally bonded (acid-etched) fixed appliances can be used but problems exist with reliable bond strengths.12 Often the bond strengths are lower than ideal, leading to multiple bond failures in treatment and the need to step back to 'pick up' these teeth, thereby increasing treatment duration. This is compounded when glass ionomer and residual composite placed for aesthetics and sensitivity have not been thoroughly removed. Debonding of the appliance can cause factures to the fragile enamel and must therefore be performed with caution.
Glass ionomer cement-based adhesives are thought to improve appliance retention as they are less reliant on microtag formation, and also help in the reduction of further enamel demineralisation. The use of sodium hypochlorite to remove excess protein surrounding the enamel crystals and improve the quality of etch in amelogenesis imperfecta cases has been described.13 However, this study was conducted in primary teeth and the evidence for improved bracket retention with these methods remains weak, as does increasing etch times in this group of patients.14,15
Plastic brackets can be used instead of metal brackets because they can be removed with a hand piece at debond without damaging the enamel surface. Traditional banded appliances are old-fashioned, but may also be used to overcome some of these problems. If the clinical crown height is minimal and banding is not possible, the use of preformed stainless steel crowns with welded tubes or brackets is recommended. The use of these coverage crowns will help prevent further decrease in vertical height and will also enable stable bite raising to aid in placing restorations once the orthodontic treatment is complete.16 Both these techniques may help minimise the damage and further loss of enamel, but are not aesthetically pleasing and are time-consuming appliances to place.
The lack of uniformity of enamel coverage means that the second and third order bends (which are part of a pre–adjusted appliance prescription) are not uniformly expressed and more detailing bends at the end stage of treatment are needed to counteract this when final restorations using veneers and crowns are not indicated.
Delayed tooth eruption
The developmental age of the patient should be used when assessing AI patients for tooth eruption. Occasionally, space maintainers may be indicated to prevent tipping of adjacent teeth into the space.
Impacted teeth
Preventative approaches such as removal of the deciduous canines and space creation should be employed even in the absence of clear supportive evidence of their efficacy.17 Where a tooth remains impacted despite these measures, a decision as to whether to radiographically monitor, surgically remove, orthodontically align, or autotransplant the tooth needs to be made. The patient's motivation and in particular the general health of the remaining dentition must be considered as orthodontic extrusion can inadvertently place large anchorage demands and possible intrusive forces on the remaining dentition.
When orthodontic alignment is the treatment of choice, the orthodontist is best to request an open exposure (as opposed to a closed exposure) from the surgeon due to the lower bond strengths of the affected enamel.18 This can lead to a higher probability of loss of the attachment, that is (the gold chain debonding when a closed exposure is used), necessitating further surgical intervention.
If a permanent impacted tooth is surgically removed, the orthodontist can work in collaboration with the restorative team to decide whether to close, maintain or redistribute the space.
Congenitally missing teeth
The treatment options are the same as for a hypodontia case and can largely be categorised into total space closure obviating the need for prosthetic replacement, space opening and redistribution of space with subsequent restorations.
Root malformations
Alterations in normal root form need to be detected before commencement of treatment so that the direction in which the root is moved and the magnitude of force to be applied can be adjusted accordingly. Root malformations have been considered a risk factor for orthodontic apical root resorption. Teeth with blunt or pipette-shaped roots were resorbed more than teeth with a normal root form.19 This is of great importance in a group of patients who are known to also exhibit generalised root resorption.
Progressive root and crown resorption
More rigorous monitoring of root resorption during orthodontic treatment is recommended. Occasionally forced extrusion of a tooth is required when there has been such marked crown resorption that there is insufficient tooth material to retain the restorative elements.
Taurodontism
This feature of AI can increase the susceptibility to root resorption during orthodontic treatment.20 In addition to this, extractions may be more difficult as the furcation is located more apically and the root apices may be shorter and thinner. The root morphology exhibited is thought to decrease the anchorage value of teeth, although this is more a theoretical than clinical finding.21
Pulpal calcification
Pulpal calcifications22 are often seen in patients with AI. This is further compounded by orthodontic treatment, which can cause pulpal calcifications in general patients as well as those with AI.23 The need for meticulous oral hygiene around the orthodontic appliance is paramount as the lack of a protective enamel covering increases the ingress of bacteria into the pulp chamber. Once this occurs, the pulpal calcifications make endodontic treatment challenging. Additionally, the orthodontic appliance must often be removed around the tooth in question for ease of access, causing further delays in treatment progression.
Anterior and posterior open bite occlusions
Persson et al. found the open bite occlusion frequently found in AI cases to be skeletal in origin.24,25,26 It has been suggested that the frequent finding is caused by a genetically determined anomaly of craniofacial development, rather than by local factors influencing alveolar growth; although the causal relationship between the enamel defect and the skeletal deformity remains to be explored. This will need correcting either with orthodontics alone or a combination of orthodontics and surgery,27 unless the open bites are to be accepted or thought to have been caused by severe tissue loss in which case a restorative approach is the treatment of choice.
Treatment rationale
The general principles for AI management are based upon a comprehensive and timely approach, addressing the clinical elements as well as the patient's demands and motivation.
There needs to be close liaison between the multidisciplinary team for planning in the immediate, transitory and long-term phases of treatment.
The most challenging aspects of orthodontic treatment in a patient with amelogenesis imperfecta is maintaining a high level of motivation for what could be a prolonged cause of treatment spanning many years. Treatment must be divided into achievable sectors with clearly defined goals that the patient can relate to.
To facilitate this, one must always start with the end in mind. The orthodontist must wean themselves from the usual goals of establishing and achieving Andrews' six keys,28 a perfect occlusion, as the overlying principle is often to place the teeth in a position that maximises the placement of restorations for function, aesthetics and stability. An example of this is that many mildly rotated teeth can be left in their original positions when the definitive plan is for either tooth build up or crown placements and full space closure is not obligatory.
Treatment for patients with AI occurs during three broad phases: infancy, childhood and adolescence, and adulthood.
Infancy (birth to around 5 years of age)
The orthodontist's input at this stage is minimal and treatment remains the mainstay of the general dental practitioner and paediatric team.
Childhood and adolescence (6 years of age to mid/late teens)
The orthodontist is likely to see the patient during this period to advise on appropriate interceptive measures on receiving an appropriate referral. This is often for first molars of poor long term prognosis, where appropriate timing and care can lead to excellent outcomes (Figs 1a-b).
The use of removable appliances in the correction of malocclusion
This circumvents many of the issues with fixed appliances. Careful consideration needs to be paid to the retentive element due to the decrease in crown height and lack of undercuts. Where possible, aesthetics should be considered and improved upon to act as an aid in patient compliance. In this case a midline screw was used to correct the crossbite (Fig. 2a). However, the patient was reluctant to wear the removable appliance until the appliance was redesigned (Figs 2b-c) to incorporate aesthetic elements that were clearly beneficial psychosocially.
The role of functional appliances
Growth modification may play a role in treating AI patients with Class III or Class II malocclusions. In contemporary British orthodontics, the use of functional appliances is largely for Class II malocclusions. The vertical element needs to be carefully considered and managed, as often vertical clearance and an open bite are required for subsequent restorations.
The role of fixed appliances
The potential difficulties with bond strengths have already been discussed. Consideration should be given to appointment scheduling especially when the appliance is placed to allow the patient to return to the surgery were the appliance to debond.
In addition to this a staged bond up is often required due to the sensitivity experienced by the patient. Figures 3a and b illustrate a case where molar bands have been used in preference to molar tubes. Placement of separators is seldom needed due to the crown morphology and absence of enamel contacts. A two stage acid etch technique was used for bracket placement.
Adulthood (17 years of age onwards)
Liaison with oral and maxillofacial surgeons
In cases where there is a discrepancy in the maxilla or mandible, an osteotomy may be required to correct this. With open bite problems, a Le Fort 1 osteotomy with posterior impaction of the maxilla will allow for closure, possibly with mandibular movement depending on the antero-posterior problem. This is carried out in combination with fixed appliances to align and decompensate the arches. Temporary anchorage devices could also play a role in mild anterior open bites.
In this instance, while the patient (Figs 4a-c) had moderate to severe bimaxillary retrusion, with excessive show of gingiva on smiling, her main concern was the aesthetics of the teeth. A decision was therefore made to accept the skeletal components and correct the crossbite (Figs 4d-h) before entering the restorative phase of treatment.
Liaison with restorative dentists
The definitive restorative phase of treatment is the final phase in the management of these patients and this revolves around crowns, veneers or resin restorations. This phase of treatment for this cohort of patients will be described in the next paper in this series. Where pre-restorative orthodontics has been undertaken, it is important that orthodontic retention to prevent relapse is incorporated into this phase of treatment either by the nature of the restorations provided or by ensuring that new retainers are provided for the patients.
Conclusion
The orthodontic management of patients with amelogenesis imperfecta has been described. Of note is the need for a multidisciplinary approach and the need to continually motivate this group of patients while using techniques and appliances that aim to preserve the fragile tooth structure.
References
Witkop C J Jr . Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: problems in classification. J Oral Pathol 1988; 17: 547–553.
Yip H K, Smales R J . Oral rehabilitation of young adults with amelogenesis imperfecta. Int J Prosthodont 2003; 16: 345–349.
Kida M, Ariga T, Shirakawa T, Oquchi H, Sakiyama Y . Autosomal-dominant hypoplastic form of amelogenesis imperfecta caused by an enamelin gene mutation at the exon-intron boundary. J Dent Res 2002; 81: 738–742.
Dong J, Gu T T, Simmons D, MacDougall M . Enamelin maps to human chromosome 4q21 within the autosomal dominant amelogenesis imperfecta locus. Eur J Oral Sci 2000; 108: 353–358.
MacDougall M, Simmons D, Gu T T et al. Cloning, characterization and immunolocalization of human ameloblastin. Eur J Oral Sci 2000; 108: 303–310.
Seymen F, Kiziltan B . Amelogenesis imperfecta: a scanning electron microscopic and histopathologic study. J Clin Pediatr Dent 2002; 26: 327–335.
de Oliveira C M, Sheiham A . Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod 2004; 31: 20–27; discussion 15.
Coffield K D, Phillips C, Brady M, Roberts M W, Strauss R P, Wright J T . The psychosocial impact of developmental dental defects in people with hereditary amelogenesis imperfecta. J Am Dent Assoc 2005; 136: 620–630.
Winter G B . Amelogenesis imperfecta with enamel opacities and taurodontism: an alternative diagnosis for 'idiopathic dental fluorosis'. Br Dent J 1996; 181: 167–172.
Dellow E L, Harley K E, Unwin R J, Wrong O, Winter G B, Parkins B J . Amelogenesis imperfecta, nephrocalcinosis, and hypocalciuria syndrome in two siblings from a large family with consanguineous parents. Nephrol Dial Transplant 1998; 13: 3193–3196.
Poulsen S, Gjørup H, Haubek D et al. Amelogenesis imperfecta – a systematic literature review of associated dental and oro-facial abnormalities and their impact on patients. Acta Odontol Scand 2008; 66: 193–199.
Seow W, Amaratunge A . The effects of acid-etching on enamel from different clinical variants of amelogenesis imperfecta: an SEM study. Pediatr Dent 1998; 20: 37–42.
Saroğlu I, Aras S, Oztaş D . Effect of deproteinization on composite bond strength in hypocalcified amelogenesis imperfecta. Oral Dis 2006; 12: 305–308.
Venezie R D, Vadiakas G, Christensen J R, Wright J T . Enamel pretreatment with sodium hypochlorite to enhance bonding in hypocalcified amelogenesis imperfecta: case report and SEM analysis. Pediatr Dent 1994; 16: 433–436.
Hiraishi N, Yiu C K, King N M . Effect of acid etching time on bond strength of an etch-and-rinse adhesive to primary tooth dentine affected by amelogenesis imperfecta. Int J Paediatr Dent 2008; 18: 224–230.
Bachmann J . Amelogenesis imperfecta – orthodontic problems and their solution using multiband appliances and temporary steel crowns. Fortschr Kieferorthop 1985; 46: 66–71.
Parkin N, Benson P E, Shah A et al. Extraction of primary (baby) teeth for unerupted palatally displaced permanent canine teeth in children. Cochrane Database Syst Rev 2009; CD004621.
Parkin N, Benson P E, Thind B, Shah A . Open versus closed surgical exposure of canine teeth that are displaced in the roof of the mouth. Cochrane Database Syst Rev 2008; CD006966.
Levander E, Malmgren O . Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors. Eur J Orthod 1988; 10: 30–38.
Seow W . Taurodontism of the mandibular first permanent molar distinguishes between the tricho-dento-osseous (TDO) syndrome and amelogenesis imperfecta. Clin Genet 1993; 43: 240–246.
Haskova J E, Gill D S, Figueiredo J A, Tredwin C J, Naini F B . Taurodontism – a review. Dent Update 2009; 36: 235–236, 239–240, 243.
Gertzman G B, Gaston G, Quinn I . Amelogenesis imperfecta: local hypoplastic type with pulpal calcification. J Am Dent Assoc 1979; 99: 637–639.
Delivanis H P, Sauer G J . Incidence of canal calcification in the orthodontic patient. Am J Orthod 1982; 82: 58–61.
Persson M, Sundell S . Facial morphology and open bite deformity in amelogenesis imperfecta. A roentgenocephalometric study. Acta Odontol Scand 1982; 40: 135–144.
Rowley R, Hill F J, Winter G B . An investigation of the association between anterior open-bite and amelogenesis imperfecta. Am J Orthod 1982; 81: 229–235.
Hoppenreijs T J, Voorsmit R A, Freihofer H P . Open bite deformity in amelogenesis imperfecta. Part 1: An analysis of contributory factors and implications for treatment. J Craniomaxillofac Surg 1998; 26: 260–266.
Hoppenreijs T J, Voorsmit R A, Freihofer H P, Van't Hoff M A . Open bite deformity in amelogenesis imperfecta. Part 2: Le Fort I osteotomies and treatment results. J Craniomaxillofac Surg 1998; 26: 286–293.
Andrews L . The six keys to normal occlusion. Am J Orthod 1972; 62: 296–309.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Arkutu, N., Gadhia, K., McDonald, S. et al. Amelogenesis imperfecta: the orthodontic perspective. Br Dent J 212, 485–489 (2012). https://doi.org/10.1038/sj.bdj.2012.415
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.415