Key Points
-
An updated review of the literature relating to the ferrule effect with particular emphasis on the less explored elements of this accepted concept.
-
Presents a classification based on risk assessment for the various clinical presentations of broken down teeth.
-
Provides updated clinical guidelines on how to approach teeth with advanced structure loss that are to be restored.
Abstract
The 'ferrule effect' is a long standing, accepted concept in dentistry that is a foundation principle for the restoration of teeth that have suffered advanced structure loss. A review of the literature based on a search in PubMed was performed looking at the various components of the ferrule effect, with particular attention to some of the less explored dimensions that influence the effectiveness of the ferrule when restoring severely broken down teeth. These include the width of the ferrule, the effect of a partial ferrule, the influence of both, the type of the restored tooth and the lateral loads present as well as the well established 2 mm ferrule height rule. The literature was collaborated and a classification based on risk assessment was derived from the available evidence. The system categorises teeth according to the effectiveness of ferrule effect that can be achieved based on the remaining amount of sound tooth structure. Furthermore, risk assessment for failure can be performed so that the practitioner and patient can better understand the prognosis of restoring a particular tooth. Clinical recommendations were extrapolated and presented as guidelines so as to improve the predictability and outcome of treatment when restoring structurally compromised teeth. The evidence relating to restoring the endodontic treated tooth with extensive destruction is deficient. This article aims to rethink ferrule by looking at other aspects of this accepted concept, and proposes a paradigm shift in the way it is thought of and utilised.
Similar content being viewed by others
Introduction
When a tooth has suffered significant structure loss, the restorative options may include restoring the tooth with multiple involved procedures or extracting the tooth. When restoring these cases, the restoration's ability to brace solid sound tooth structure is the key for long-term success.1 However, often the practitioner is presented with a clinical dilemma, since a more predictable solution may be available and indicated, and saving such teeth may result in compromised periodontal support, aesthetic complications and sometimes damage to adjacent teeth.
Naturally, the literature discussing the restoration of severely damaged teeth often coincides with the literature discussing the restoration of endodontic treated teeth, however, the concepts presented in this paper are also applicable to severely broken down teeth that are vital.
The challenge of restoring pulpless teeth has been described to be directly associated with the extensive loss of natural tooth structure that is frequently seen in these teeth.2 Furthermore, it has been well established that the longevity of a root treated tooth is directly related to the amount of remaining sound tooth material.3,4,5
Routinely, endodontic treated teeth that have lost a substantial amount of natural tooth structure are treated with full coverage restorations.6 Often additional procedures including a post and a core and/or crown lengthening surgery may be indicated. Such treatments are recommended even though it is acknowledged that the incorporation of these procedures will further reduce the amount of sound tooth structure, thereby possibly further compromising the tooth.7 Some of the currently accepted clinical guidelines as to how to approach such teeth may be oversimplified, and for this reason some of the fundamental principles have been reviewed and rethought. Since it is difficult to quantitatively assess the amount of remaining tooth structure in a clinical setting, guidelines aimed at aiding the ability to accurately assess the condition of a given tooth are of prime importance.
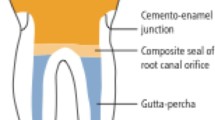
The incorporation of the concept of 'ferrule' or 'the ferrule effect' has been accepted as one of the foundations of the restoration of the endodontic treated tooth. The origin of the term is thought to come from the Latin terms 'ferrum' - iron, and 'viriola' - bracelet, such that the ferrule is an encircling band of cast metal around the coronal surface of the tooth. The rule established is that a 1.5-2 mm ferrule height directly above the margin improves long-term survival of endodontic treated teeth with a post and core.8,9,10,11,12,13,14,15,16,17,18,19 The cast restoration encircles the remaining parallel walled tooth structure with a metal band thereby 'bracing' the tooth, providing resistance to dislodgement and preventing fracture.
It should be clear that the term ferrule is often misinterpreted. It is often used as an expression of the amount of remaining sound dentine above the finish line. It is in fact not the remaining tooth structure that is the 'ferrule' but rather the actual bracing of the complete crown over the tooth structure that constitutes the ferrule effect, ie the protection of the remaining tooth structure against fracture.20 Various different ferrule designs have been suggested but currently there is little research supporting one design over another.10 Most publications discuss the required height of ferrule, however, other design characteristics like dentine thickness, location of the remaining dentine walls, and the loads the restoration has to withstand were not considered.
Posts are frequently used for the retention of a core material in teeth that have had extensive loss of coronal tooth structure.21 Their use, however, may increase root fracture due to excessive pressures during insertion or because of lateral movement of the post within the root, thus ironically increasing the risk of root fracture22,23 and treatment failure.24 Therefore, the use of a correct ferrule design is of particular importance in teeth restored with post and cores.4
Since placing crown margins significantly subgingivally is not advisable because of the violation of biologic width, the quest for the perfect ferrule may lead to the incorporation of treatments like crown lengthening and/or an orthodontic extrusion.25,26,27 Clearly, this presents a dilemma as crown lengthening surgery may result in a poorer crown to root ratio, compromised aesthetics, loss of the inter-dental papilla and a potential compromise of the support of the adjacent teeth. Orthodontic intervention may resolve some of these risks, however, the crown to root ratio may still be compromised and it adds significant time and an additional fee to the whole procedure, making it, in many cases, non-feasible. For this reason the authors found it necessary to explore the existing parameters of the ferrule effect as it stands in the literature.
The aim of this paper is threefold: 1) To review the literature relating to the ferrule effect; 2) To classify the different clinical presentations of broken down teeth; and 3) To suggest clinical guidelines to enable treatment planning of compromised teeth.
PART 1: Literature review
The literature explores many aspects relating to both the quality and quantity of remaining tooth structure to be restored, and the bracing by the crown of this tooth structure. Four direct factors (a-d) influencing the ferrule were examined, as well as two additional indirect factors (e-f) that may influence the functionality of the ferrule:
-
a
Ferrule height
-
b
Ferrule width
-
c
Number of walls and ferrule location
-
d
Type of tooth and the extent of lateral loads
-
e
Type of post
-
f
Type of core material.
a) Ferrule height
The overwhelming majority of the literature presents the importance of having enough height of dentine to be embraced by the crown. A ferrule of 1 mm of vertical height successfully doubled the resistance to fracture versus teeth without a ferrule, and appears to be the minimal acceptable amount of ferrule height.10 Other studies have shown the maximum benefit to be achieved out of having 1.5-2 mm vertical tooth structure.9,19,26,28 Some authors suggest that the crown must extend at least 2 mm beyond the tooth core junction to ensure a protective ferrule effect,13,29 or that even 3 mm of height provides even further fracture resistance.15 What seems clear is that the greater the height of remaining tooth structure above the margin of the preparation, the better fracture resistance provided.30
b) Ferrule width
Although there is relative consistency in the dental literature supporting the 2 mm height rule, some questions have been raised in the literature as to the significance of the remaining axial wall thickness of dentine and its role in preventing tooth fracture.10,29 Some papers have implicated the amount of residual axial tooth structure to be significant in resisting fracture,31,32,33 whereas other papers have excluded the width of shoulder preparation and crown margin as a significant factor.34 It does, however, appear to be a topic that needs further exploration, especially since aesthetic demands often require aggressive preparations at the margin, or previously existing buccal lesions may severely compromise the thickness of the buccal dentine wall.
Clinically it is generally accepted that walls are considered 'too thin' when they are less than 1 mm in thickness, such that the minimal ferrule height is only of value if the remaining dentine has a minimal thickness of 1 mm.35,36,37 No papers that looked at the effect of having a dentine thickness of less than 1 mm incorporated as part of the ferrule were located by the authors.
Tjan and Whang38 looked at four groups of varying thicknesses: 1 mm, 1 mm with a 60° bevel, 2 mm and 3 mm of remaining buccal dentine. No significant differences were noted between the different groups other than that the two groups of 1 mm thick dentine were more likely to fail due to fracture rather than cement failure. Similarly Sorenson and Engleman in 199010 seemed to negate the importance of dentine thickness. However, their paper looked at the thickness of dentine at the margin when using various contra-bevel ferrule designs, rather than at the thickness of the coronal extension of dentine. It is the thickness of the coronal extension above the crown margin that is thought to have significance in the fracture resistance of crowned teeth.
In 1990 Joseph and Ramachandran37 looked at the effectiveness of incorporating a cervical collar into the preparation with differing buccal thicknesses of dentine. The authors concluded that the thicker dentine of 2 mm increased the resistance to fracture, however, the presence of a cervical collar had no influence on the point of failure. In general there is no consensus regarding contra-bevel ferrule designs, or the incorporation of a cervical collar and therefore these designs are not widely accepted.
A laboratory study by Gegauff in 200039 investigated whether crown lengthening decoronated premolars so as to achieve an acceptable ferrule height improved the fracture resistance of these teeth. He concluded that it did not improve the fracture resistance of these teeth. The question was raised by Hinkfuss and Wilson,40 as to whether the reason the ferrule did not prove to be effective in this study was because the teeth used in Gegauff's study were mandibular premolars. These teeth have conical roots, therefore although by performing crown lengthening, an added dentine height results, a decrease in dentine width at the margin is inevitable after the tooth is further prepared for a new margin. This is possibly the cause for their poorer fracture resistance results. In their own study Hinkfuss and Wilson attributed the increased fracture resistance witnessed with the incorporation of a 2 mm ferrule to be attributed to the use of molar teeth with a thick amount of remaining dentine (2.4 mm). Perhaps the thickness of axial dentine after crown preparation has more of a role than previously thought? They concluded that further investigation needs to be done as to the effect of remaining dentine thickness on endodontic treated teeth prepared for crowns.
c) Number of walls and ferrule location
Another aspect that should be re-thought is the assumption that a full 'all around' ferrule is needed in every case. This has substantial clinical significance. Caries frequently affects some walls (primarily the proximal ones), but not others, and erosion and abrasion more commonly affect only the buccal walls. Similarly, tooth preparations aiming to achieve maximum aesthetics may result in remaining low and/or excessively thin buccal walls. In each of these examples it is common for only a partial ferrule to remain after crown preparation.
Various studies have demonstrated the superiority of a uniform all around ferrule over a ferrule that varies in different parts of the tooth.41,42,43 However, the concept of partial ferrule should not be ruled out. The literature suggests that a non-uniform ferrule is still superior to no ferrule at all. Al-Wahadni et al. in 200234 looked at the presence of a partial ferule on anterior teeth. They compared having no ferrule to having 3 mm or more height of ferrule on the buccal surface alone. They concluded that teeth with retained buccal dentine of 3 mm height, but no other dentine walls remaining, had significantly higher resistance to fracture compared to the control. Heights greater than 3 mm did not produce statistically significant improvements.
Ng et al.20 investigated the common clinical scenario of only a partial ferrule being present due to destruction by the caries process. They suggest that it is the location of sound tooth structure to resist occlusal forces that is more important than having 360° of circumferential axial wall dentine. They depicted an in vitro replication of the maxillary incisor scenario. Their results showed that having good palatal ferrule only is as effective as having a complete 'all around' ferrule, as this tooth structure will resist the forces applied in function to the palatal surface of the maxillary incisor. Similarly, a maxillary incisor that is only missing the palatal wall despite the presence of three other favourable walls shows poor fracture resistance and is at greater risk of failing than some conditions with fewer walls remaining, for example when both the mesial and distal walls are missing. This is because when the palatal wall is missing, the non-axial load from the palatal side in a maxillary anterior crown challenges the post/core/root junction. When a palatal wall is present, it is the remaining wall that resists the load.
Alternative results, however, by Arunpraditkal et al. in 2009,41 negated the relevance of the site of the missing wall, when only one wall was deficient in having adequate ferrule. Their study showed that although the lack of a buccal wall displayed the poorest mean failure load, their result was not statistically significant. It should be noted, however, that even though their study did not find significance in the location of a single missing wall on mandibular second premolars, this study was performed using a static load from the buccal direction which does not accurately reflect the clinical setting - neither the direction of the load nor the nature of the load. They acknowledge that the direction of the load may be the critical point and using a thermocycling/fatigue model may have more accurately depicted the clinical/functional setting. If this had been done, the missing buccal coronal wall may have had more significance than their results showed. Thus, there is evidence to suggest that a partial ferrule, although not as ideal as a full 360°, 2 mm ferrule, still has value in providing fracture resistance.
d) Type of tooth and the extent of lateral load
Two factors distinguish anterior from posterior teeth: their relative size and the direction of loads they need to withstand. An analysis of force distribution in different teeth shows that anterior teeth are loaded non-axially and posterior teeth in normal function have the majority of the load in an occluso-gingival direction. Lateral forces have a greater potential to damage the tooth-restoration interface when compared to vertical loads.41
Literature reviews by Torbjorner and Fransson44,45 concluded that favourable occlusal prosthesis design is probably more important for survival of structurally compromised endodontic treated teeth than is the type of post used, as non-desirable forces introduced by way of an interference on the restoration are a risk for fatigue fracture of teeth.
Hence, a differential approach needs to be adopted when it comes to the restoration of anterior and posterior teeth. Deep bite situations, parafunction and dietary habits may further increase the risk for anterior teeth. In posterior teeth, occlusal scheme patterns and cuspal heights significantly influence the type and direction of load that is applied to each tooth. Group function situations, especially when the buccal cusps of the maxillary teeth are long, generate higher lateral forces, when compared to canine guidance situations.46,47 Similarly posterior teeth with high cusps translate higher lateral forces when compared to severely worn down teeth. Noteworthy wear faceting also implies the presence of high loads. Force vectors which have a significant lateral component, when cusps are present, may change into mainly vertical vectors once cusps are flattened.48
For this reason, conclusions drawn from literature relating to the restoration of anterior teeth should not automatically be assumed for the posterior teeth and vice versa. It is recommended that before restoring a tooth, a thorough review of the occlusal pattern as well as functional and parafunctional forces is performed, as these will influence the success of the final restoration of the particular tooth.5
e) Type of post
The dental literature relating to the different types of posts presents too many variables to enable a true comparison between all available post types. The profession lacks long-term clinical results with a high level of evidence pertaining to survival data for various post systems.45 No universal recommendations have been established, however, many studies demonstrate that the presence of a ferrule of 1.5-2 mm sound coronal tooth structure between the core and the finish line is more important in fracture resistance than the post design or type.18,19,30,49
Alternatively, new evidence is continually emerging favouring the reinforcement abilities of fibre reinforced composite posts. A study by Saupe in 199650 reported no difference in fracture resistance of teeth with bonded posts with or without a ferrule. However, this result should be interpreted with caution as although bonded posts are reported to strengthen the root initially,51 the strengthening effect may be lost over time.52,53,54 This is thought to possibly be due to fluid leakage through the apical foramina and lateral canals.45 Furthermore, bonding to radicular dentine has been shown to be less reliable than bonding to coronal dentine.55,56 This places further speculation on the ability of bonded posts to reinforce teeth enough to protect against fracture. Likewise, Oliveira in 2008 found that endodontic treated teeth restored with bonded fibre posts and composite cores did not show altered fracture resistance with varying amounts of ferrule height from 0-3 mm.57 Their study was conducted on maxillary canines - the largest and most sturdy tooth in the mouth - and therefore it seems reasonable to question the influence of the bulk or thickness of the remaining dentine in addition to the reinforcing effect of the bonded post/core restoration as playing a part in the fracture resistance of these endodontic teeth restored with bonded fibre posts and composite cores. Overall, fibre reinforced composite posts have shown positive results when compared to metal posts. Despite their significantly lower load bearing values, their performance is considered favourable because failure of this type of post seems to be protective of the remaining tooth structure by displaying a more favourable failure pattern, with virtually no root fracture.57,58,59,60 Fracture of the remaining tooth structure has been shown to occur more occlusally with fibre posts, making these failures restorable vs. a more apical positioned fracture occurring with metal posts, rendering such teeth non-restorable. It can therefore be concluded that although the profession embraces the needs for ferrule, in compromised cases where a good ferrule is not attainable, it might be desirable to restore a tooth with a bonded post rather than a metal post.
Nevertheless, cast posts or even bonded cast posts have been recommended over resin based fibre posts in many instances.61,62 However, clear guidelines for situations when one type of post is favourable over another post are not available and further laboratory and clinical studies are still necessary.22,36,63,64
f) Core materials
The core material may be a further influencing factor on the effect the differing thickness of remaining dentine has on the functionality of the ferrule. Composite resin with a dentine bonding agent has frequently been implicated as a material that can strengthen the tooth and reinforce cusps compared to amalgam.65,66,67,68 Teeth with wide MOD cavities restored with amalgam have repeatedly shown cusp failure due to the inability of this material to strengthen weakened cusps.69 This is true both because amalgam does not bond to tooth structure and it requires undercuts for retention, which weakens the remaining walls. Alternatively, multiple studies have shown improved fracture resistance in teeth with MOD cavity preparations restored with composite resin or fibre reinforced resin.70,71,72,73,74,75
It can be extrapolated that dentine bonding agents coupled with composite materials may reinforce residual tooth structure of prepared teeth, and may be beneficial when only thin dentine ferrule remains. The effect of bonded composite and how much it is able to reinforce the remaining dentine of varying thicknesses has not yet been thoroughly studied. The current literature is contradictory. Several studies demonstrate bonded restorations reinforcing tooth structure.3,76,77 Others show fracture strengths similar to unrestored cavity preparations.78,79
Another question to be addressed is what is the amount of dentine reinforcement that can be achieved in thin walled roots with a thin layer of resin cement with a metal post as opposed to resin based posts and resin based core materials.80 A thin layer of resin cement used to bond a post to the radicular dentine may be the key to the dentine reinforcement rather than the type of post/core material used per se.45
Some investigators81 have suggested based on in vitro studies that prefabricated posts bonded with resin cement and composite resin cores fail to demonstrate a difference between restored endodontic treated teeth with or without remaining coronal tooth structure between the core and the preparation margin. The ability of the bonded post to negate the need for the commonly accepted ferrule, as well as the effect of bonded materials in variable dentine thicknesses, needs further investigation. Since there is no consensus, currently it is not accepted that resin based bonded materials are able to improve the prognosis of a structurally compromised tooth, however there are instances where using such materials may aid the clinical situation.
PART 2: Ferrule Classification
Although current literature does not present a uniform description and design of the ideal ferrule, a classification that is based on the remaining tooth structure would be of value to the profession. Such a classification will enable the creation of standardised guidelines for treatment, and will enable researchers to evaluate published articles or plan future research utilising a uniform key for tooth evaluation.
A classification of single rooted pulpless teeth based on the amount of remaining supra-gingival tooth structure has been recommended by Kurer in 199182 to aid with treatment planning the endodontic treated tooth. This classification described five classes of pulpless teeth: 1 with sufficient coronal tissue for a crown, 2 requiring a core, 3 with no coronal tooth structure and 4 and 5 with deep fractures and periodontal complication respectively. As suggested by Stankiewicz and Wilson,9 the classification could be of more value if a subgroup were included that accounted for the presence of a minimal effective ferrule.
The proposed classification considers the amount of remaining tooth structure available to be incorporated into the ferrule effect in a given tooth, so that the risk of mechanical failure can be judged and appropriate treatment options selected. Ideally, a tooth should be classified before preparation, but with the desired preparation in mind, so that the practitioner can make adjustments to the plan in order to make sure that maximum thickness and height of the remaining tooth structure are preserved. Clinical guidelines are suggested based on conclusions drawn from the review of current literature.
Four aspects relating to the remaining natural tooth structure were considered important factors to be considered when analysing the potential ferrule present in a structurally compromised tooth. These aspects are:
-
a
The height of remaining dentine after tooth preparation. A wall is considered to contribute to the ferrule only if it is 2 mm of height and continues along more than half of the tooth surface
-
b
The thickness of remaining dentine after tooth preparation. A wall is considered to contribute to the ferrule only if it is 1 mm thick
-
c
The number of remaining dentine walls, and their location (location is represented by corresponding side)
-
d
The lateral vectors of load on the tooth. These are defined as light lateral loads or heavy lateral loads based on the type of tooth and occlusal scheme.
These factors enabled the authors to develop a classification based on risk assessment (Fig. 1).
Category A: No anticipated risk
Sound dentine walls remaining all around the tooth, with height greater than 2 mm and with a minimum thickness of 1 mm. Such teeth do not present an anticipated risk for structural or mechanical failure (Fig. 2).
Category B: Low risk
Compromised or no ferrule present on either proximal surface. (ie less than 2 mm height and/or 1 mm thickness) OR two compromised proximal walls on a tooth that undergoes light lateral loads. Such teeth present low risk for structural or mechanical failure.
Category C: Medium risk
Two compromised proximal walls on a tooth that undergoes heavy lateral loads OR a compromised buccal or lingual wall on a tooth that undergoes light lateral loads. Such teeth present medium risk for structural or mechanical failure.
Category D: High risk
A compromised buccal or lingual wall on a tooth that undergoes heavy lateral loads OR a compromised buccal, and lingual wall on any tooth OR a tooth that has only two adjacent walls or only a single wall remaining. Such teeth present high risk for structural or mechanical failure and alternate treatment modalities should be considered and may be more appropriate.
Category X
No ferrule can be established, such that the tooth is non-restorable.
Actual treatment rendered will be determined based on considering the entire dentition and attachment apparatus, as well as individual patient risk factors and expectations.
PART 3: Suggested clinical guidelines
A careful plan of the desired preparation, which maximises ferrule strength, will minimise the risks when restoring severely broken down teeth.
In addition to the traditionally accepted consideration of ensuring adequate ferrule height, the additional aspects that the literature supports to be incorporated when restoring teeth are: a) the width of remaining dentine, b) the number of walls remaining and their location and c) the type of tooth and the lateral load on that tooth.
a) Width considerations
Techniques aimed to restore aesthetics of anterior teeth require significant reduction of tooth structure. Beautiful ceramic restorations require thickness of at least 1.5 mm at the margins to allow for adequate aesthetics.83 This type of preparation reduces dramatically the thickness of the remaining dentine in the most critical area - the margin in the cervical area of the tooth. The cervical region of the tooth is the area subject to bearing the most stress in function and is where the majority of fractures occur18 and wide margin preparations therefore further weaken the tooth at its most critical area. Soew, Toh and Wilson84 looked at the amount of remaining dentine width after preparations for various types of restorations. Inlay/onlay preparations left more dentine thickness than did metal ceramic crowns, which in turn left more dentine thickness than did the all-ceramic crown preparation. They concluded that decisions as to the type of definitive restoration to restore the endodontic treated maxillary second premolar should be influenced by the amount of thickness of the remaining tooth tissue.
Similarly special care needs to be taken with axial reduction in young patients, where the teeth have relatively large pulps and a resultant decreased thickness of dentine. For these reasons, it is the recommendation of the authors that the preparation of such or small teeth will be differential, with minimal preparation on the palatal and non-aesthetic walls, and that metal or a thin all ceramic core coping are used, in order to ensure maximum thickness of the dentinal walls that do not influence the aesthetics of the final restoration.
Root canal treatment and post space preparation of teeth with thin root configuration often leaves less than the recommended 1 mm residual dentine thickness, even before the tooth has been prepared for a crown.85 For this reason, these teeth frequently display a poorer prognosis resulting from their root anatomy.86 In these situations it is often wise to try and avoid post preparation and/or crowning these teeth so as not to compromise them further.
b) Partial ferrule considerations
Although it is clear that a full 360° ferrule is desirable, there are clinical circumstances where adopting a partial ferrule is still better than the alternative treatment options. In general the more walls of ferrule present, the better the fracture resistance, but sometimes it is not the number of walls that are the focus of consideration, but rather the location of these walls.
Most of the forces in the posterior segment of the mouth are occluso-gingival and bucco-lingual in nature and therefore it is reasonable to assume that oral forces do not challenge a tooth that lacks a full 2 mm ferrule on the proximal side/s as much as when the buccal and/or lingual walls are missing. In anterior teeth, where the load is generally bucco-lingual and lacks the occluso-gingival force component, the location of the wall becomes crucial. Since maxillary anterior teeth are loaded from the palatal, adequate ferrule on the lingual aspect of maxillary anteriors is of prime importance so as to resist the load.20 Similarly mandibular anterior teeth are loaded from the buccal and here the presence of a buccal wall to resist the load is the one that has the most significance.
In both anterior and posterior teeth deep proximal boxes are a common outcome of interproximal caries, which commonly results in a compromised ferrule in these areas. Therefore, a clinical decision needs to weigh the benefits vs. the risks of achieving an 'all around' uniform ferrule. The clinical implications of a crown lengthening procedure with the risk of damaging adjacent teeth should be evaluated against the biomechanical risks of a crown that does not have a 360° ferrule. When extensive lateral forces are not anticipated, it appears that a non-complete ferrule may be a more appropriate alternative if it is the proximal wall/s missing. This idea should be adopted for the treatment of such teeth as an attempt to minimise damage to the neighbouring teeth, and to preserve as much bone as possible for a future implant should it become necessary. Further research should aim to look at this question.
c) Type of tooth and lateral load considerations
Not all teeth withstand the same type of loads. Even the same type of tooth may withstand different forces, depending on the patient's occlusal scheme and their position within the arch.
Molars: In ideal occlusion, molars usually withstand forces that are mainly vertical in nature and the lateral load on these teeth is less influential. In group function situations, and when cusps are high, the lateral vector may be significant. In the common scenario of severe loss of interproximal tooth structure, but thick buccal and lingual walls are present, it is recommended that preparations aim to keep as much of the buccal and lingual walls as possible, and aim to minimally pass the core/tooth junction in the proximal areas without violating the biologic width. When the buccal and/or lingual walls are also compromised, or when extensive lateral forces are anticipated, additional ferrule on the proximal sides should be considered. In these cases, the pros and cons of crown lengthening must again be evaluated and may be chosen as the preferred treatment modality.
It is the recommendation of the authors that a partial coverage restoration should be considered if it is anticipated that after crown preparation the buccal and/or lingual walls will have less than 1 mm remaining dentine thickness. In these cases, the use of an onlay may enable the preservation of walls that may be eliminated if a full crown preparation is made.
Premolars: When it comes to lateral loads, premolars may function either as molars or as anterior teeth. Mandibular premolars present a unique problem. Since their lingual cusp is small, the remaining lingual wall may be lost in part while preparing the tooth for a crown. Since aesthetics are not a major concern in this area, a minimal preparation approach should be chosen on the lingual side. However, even if the lingual wall on these teeth is compromised, biomechanically this is not a hazardous situation since in most cases, forces are applied from the buccal area towards the lingual, making the buccal wall more significant for this specific tooth.
Maxillary premolars, on the other hand, withstand lateral forces from the lingual to the buccal direction. The buccal cusps are usually long, and even in canine protected occlusion some lateral forces may be present at the onset of the lateral movement. For this reason, a more favourable bucco-lingual ferrule is crucial. In contrast to molars, maxillary premolars are within the aesthetic zone, requiring significant buccal reduction, and often cannot undergo significant crown lengthening without compromising aesthetics, and often have a less desirable root configuration. A detailed plan of the preparation is necessary in order to preserve as much tooth structure as possible, so the longevity of the tooth and the restoration is ensured.
Anterior teeth: In ideal occlusion, these teeth are always exposed to relatively high lateral vectors of force. This becomes even more significant in deep bite situations. Furthermore, maxillary anterior teeth (including the canines) require careful attention to aesthetics, and therefore demand an aggressive buccal reduction. As with mandibular premolars, it may be wise to preserve the lingual aspects of anterior teeth by using a metal lingual surface, that is not visible, to ensure maximum structural durability. This approach is recommended especially when the natural tooth structure is significantly deficient or when the occlusal scheme indicates eg deep bite situations.
d) To crown or not to crown?
It should be emphasised that there is no consensus regarding the preferred type of final restoration for endodontic treated teeth.87 Although the overwhelming majority of the literature supports the need for full coverage restorations of most endodontic treated teeth, and a strong association between the success of endodontic treated teeth and crowned teeth has been shown,88,89,90 alternatives have been suggested too. These include using complex amalgam restorations,91,92 overlays65 or composite restorations.67,93 More recently partial restorations like indirect onlays have been suggested as a restoration that preserves more sound tooth structure than does a full coverage crown while at the same time provides cuspal coverage to protect weakened cusps.7 By implementing the proposed risk assessment classification of the remaining dentine in severely broken down teeth, practitioners will consider alternative methods of restoring these teeth.
The need for crowning a tooth is directly related to its mechanical weakening due to previous restorations, decay and/or endodontic access cavity preparation. Previous beliefs that the mechanical weakening of endodontic treated teeth was due to the difference in moisture content when compared to vital teeth has been disproven.94 On the contrary, no significant biochemical change, indicating that endodontic treated teeth are more brittle, has been demonstrated.95 It is now accepted that cuspal deflection and thickness of the residual walls and cusps are the key factors. As cavity size increases, especially after endodontic access,96 and the marginal ridges are lost, structural stability decreases.97,98 For this reason, the use of alternative restorations should be considered for certain clinical presentations, due to their ability to preserve thick residual walls better than do crowns. Alternatives include gold crowns and more recently, minimal preparation composite crowns with a 0.5 mm chamfer finish line, bonded with resin cements.99 Similarly, cuspal coverage direct or indirect composite restorations have been advocated for use in molar teeth so as to eliminate the need for axial wall destruction.100,101 With the improved wear characteristics the newer composites are showing this type of restoration may be an option, particularly in teeth of poorer prognosis, as currently there is sparse long-term information on the longevity of cusp-replacing composite restorations.102 These non-conventional solutions for the restoration of endodontic treated teeth still need in vivo testing.
e) Proposed protocol for restoring teeth with full coverage crowns
Since crown preparations which produce highly aesthetic crowns are often aggressive and may compromise the structural durability of the tooth, careful planning of the preparation, as well as assessing the potential weakening of the tooth if aesthetics is the ultimate goal, must be practised as the first step. A minimum of 2 mm ferrule height all the way around is the accepted dimension used, and is usually visible after crown preparation. However, teeth that have already been restored with posts and/or cores have an unknown thickness of remaining sound dentine. In these situations it is advisable to assume that only a minimal amount of dentine is available. For this reason preparing a tooth with no core in it is beneficial, since when looking at a prepped tooth without the presence of a core, a correct analysis of the height, thickness and location of available dentine walls is possible. Root anatomy must also be taken into consideration as conical roots or bifurcated upper first premolars may result in thin remaining dentine. Based on the literature review and the discussion, the authors propose the following protocol for treatment planned for a full coverage crown (Fig. 3).
A. Determine if a crown is feasible:
-
Select desired type of full coverage crown after consideration of aesthetics vs. structural durability
-
Plan the most minimal preparation type that will achieve your goal, and acknowledge the most ideal preparation for the selected restoration
-
Remove all restorative materials and evaluate the remaining dentine height, thickness and location/s:
-
In situations where minimal tooth remains the patient is informed of the risk assessment accompanying the tooth. An alternative and less expensive option (such as a composite restoration or a core and post) should be considered as an interim solution.
-
B. If a crown has been determined feasible:
-
Perform a minimal preparation, based on your initial plan
-
Further risk assess the remaining tooth structure, and alter your plan accordingly. If the remaining thickness of dentine enables a thicker preparation to be safely performed, do so. Otherwise discuss refining your plan with the patient to a crown that requires less preparation
-
Post and/or core – evaluate the need of a post, based on the remaining tooth structure's ability to retain the core. Restore core material as appropriate
-
Finalise preparation – ensuring an optimum balance between aesthetic needs and structural durability.
For all compromised situations a risk-benefit analysis must be done to determine if procedures aimed at improving ferrule (crown lengthening surgery or orthodontic extrusion) will successfully provide more ferrule (both height and width) without unduly compromising the tooth's support or any surrounding structures. This analysis should be done before preparation begins so as to determine feasibility of restoring with a crown and again after the initial preparation so as to adapt preparation design as necessary.
Conclusion
This paper has drawn together the various elements relating to one of the most important aspects when restoring the structurally compromised tooth – the ferrule effect. The evidence base available relating to the ferrule effect was pooled, and a classification was derived, based on this evidence. The aspects considered of prime importance were the height of the ferrule, its width, the number of walls remaining and their location, and the degree of lateral load placed on the tooth. A classification system has been recommended so that teeth can be allotted into groups and alternate treatment decisions can be made based on the risk status of the particular tooth. It is of utmost importance to remember that other, less invasive restoration types have been suggested so as to be able to preserve as much sound tooth structure as possible when restoring severely broken down teeth. This is of particular value when the remaining axial wall dentine thickness is compromised.
Many aspects of the traditionally accepted 'ferrule effect' have not been extensively studied and these include the influence of the width of the ferrule, the effect of having a partial ferrule and the influence that resin based materials (posts, cores and cements) have on reinforcing the tooth structure. A standard classification of clinical conditions should be adopted, so that a uniform approach and accepted clinical guidelines can be adapted for the restoration of broken down teeth.
References
Cheung GS, Chan T K . Long-term survival of primary root canal treatment carried out in a dental teaching hospital. Int Endod J 2003; 36: 117–128.
Robbins J W . Restoration of the endodontically treated tooth. Dent Clin North Am 2002; 46: 367–384.
Dietschi D, Duc O, Krejci I, Sadan A . Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature - Part 1. Composition and micro-and macrostructure alterations. Quintessence Int 2007; 38: 733–743.
Schwartz R S, Robbins J W . Post placement and restoration of endodontically treated teeth: a literature review. J Endod 2004; 30: 289–301.
Fernandes A S, Dessai G S . Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont 2001; 14: 355–363.
Hobo S, Whitsett L D, Jacobi R, Brackett S E, Shillingburg H T . Fundamentals of fixed prosthodontics. Quintessence Publishing, 1997.
Murphy F, McDonald A, Petrie A, Palmer G, Setchell D . Coronal tooth structure in root-treated teeth prepared for complete and partial coverage restorations. J Oral Rehabil 2009; 36: 451–461.
Cheung G S . Endodontic failures - changing the approach. Int Dent J 1996; 46: 131–138.
Stankiewicz N R, Wilson P R . The ferrule effect: a literature review. Int Endod J 2002; 35: 575–581.
Sorensen J A, Engelman M J . Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent 1990; 63: 529–536.
Cathro P R, Chandler N P, Hood J A . Impact resistance of crowned endodontically treated central incisors with internal composite cores. Endod Dent Traumatol 1996; 12: 124–128.
Hoag E P, Dwyer T G . A comparative evaluation of three post and core techniques. J Prosthet Dent 1982; 47: 177–181.
Assif D, Bitenski A, Pilo R, Oren E . Effect of post design on resistance to fracture of endodontically treated teeth with complete crowns. J Prosthet Dent 1993; 69: 36–40.
Barkhordar R A, Radke R, Abbasi J . Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent 1989; 61: 676–678.
Pereira J R, de Ornelas F, Conti P C, do Valle A L . Effect of a crown ferrule on the fracture resistance of endodontically treated teeth restored with prefabricated posts. J Prosthet Dent 2006; 95: 50–54.
Haemmings K W, King P A, Setchell D J . Resistance to torsional forces of various post and core designs. J Prosthet Dent 1991; 66: 325–329.
Pierrisnard L, Bohin F, Renault P, Barquins M . Corono-radicular reconstruction of pulpless teeth: a mechanical study using finite element analysis. J Prosthet Dent 2002; 88: 442–448.
Milot P, Stein R S . Root fracture in endodontically treated teeth related to post selection and crown design. J Prosthet Dent 1992; 68: 428–435.
Isidor F, Brondum K, Ravnholt G . The influence of post length and crown ferrule length on the resistance to cyclic loading of bovine teeth with prefabricated titanium posts. Int J Prosthodont 1999; 12: 78–82.
Ng C C, Dumbrigue H B, Al-Bayat M I, Griggs J A, Wakefield C W . Influence of remaining coronal tooth structure location on the fracture resistance of restored endodontically treated anterior teeth. J Prosthet Dent 2006; 95: 290–296.
Christensen G J . When to use fillers, build-ups or posts and cores. J Am Dent Assoc 1996; 127: 1397–1398.
Heydecke G, Peters M C . The restoration of endodontically treated, single-rooted teeth with cast or direct posts and cores: a systematic review. J Prosthet Dent 2002; 87: 380–386.
Trope M, Maltz D O, Tronstad L . Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol 1985; 1: 108–111.
Sorensen J A, Martinoff J T . Endodontically treated teeth as abutments. J Prosthet Dent 1985; 53: 631–636.
Smukler H, Chaibi M . Periodontal and dental considerations in clinical crown extension: a rational basis for treatment. Int J Periodontics Restorative Dent 1997; 17: 464–477.
Libman W J, Nicholls J I . Load fatigue of teeth restored with cast posts and cores and complete crowns. Int J Prosthodont 1995; 8: 155–161.
Kocadereli I, Tasman F, Guner S B . Combined endodontic-orthodontic and prosthodontic treatment of fractured teeth. Case report. Aust Dent J 1998; 43: 28–31.
Zhi-Yue L, Yu-Xing Z . Effects of post-core design and ferrule on fracture resistance of endodontically treated maxillary central incisors. J Prosthet Dent 2003; 89: 368–373.
Trabert K C, Cooney J P . The endodontically treated tooth. Restorative concepts and techniques. Dent Clin North Am 1984; 28: 923–951.
Akkayan B . An in vitro study evaluating the effect of ferrule length on fracture resistance of endodontically treated teeth restored with fiber-reinforced and zirconia dowel systems. J Prosthet Dent 2004; 92: 155–162.
Mattison G D . Photoelastic stress analysis of cast-gold endodontic posts. J Prosthet Dent 1982; 48: 407–411.
Hock D A . Impact resistance of post and cores (Masters thesis). Ann Arbor, 1978.
Trabert K C, Caput A A, Abou-Rass M . Tooth fracture - a comparison of endodontic and restorative treatments. J Endod 1978; 4: 341–345.
Al-Wahadni A, Gutteridge D L . An in vitro investigation into the effects of retained coronal dentine on the strength of a tooth restored with a cemented post and partial core restoration. Int Endod J 2002; 35: 913–918.
Pilo R, Tamse A . Residual dentin thickness in mandibular premolars prepared with gates glidden and ParaPost drills. J Prosthet Dent 2000; 83: 617–623.
Peroz I, Blankenstein F, Lange K P, Naumann M . Restoring endodontically treated teeth with posts and cores-a review. Quintessence Int 2005; 36: 737–746.
Joseph J, Ramachandran G . Fracture resistance of dowel channel preparations with various dentin thickness. Fed Oper Dent 1990; 1: 32–35.
Tjan A H, Whang S B . Resistance to root fracture of dowel channels with various thicknesses of buccal dentin walls. J Prosthet Dent 1985; 53: 496–500.
Gegauff A G . Effect of crown lengthening and ferrule placement on static load failure of cemented cast post-cores and crowns. J Prosthet Dent 2000; 84: 169–179.
Hinckfuss S, Wilson P R . Effect of core material and restoration design on strength of endodontically treated bovine teeth: a laboratory study. J Prosthodont 2008; 17: 456–461.
Arunpraditkul S, Saengsanon S, Pakviwat W . Fracture resistance of endodontically treated teeth: three walls versus four walls of remaining coronal tooth structure. J Prosthodont 2009; 18: 49–53.
Morgano S M, Brackett S E . Foundation restorations in fixed prosthodontics: current knowledge and future needs. J Prosthet Dent 1999; 82: 643–657.
Tan P L, Aquilino S A, Gratton D G et al. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent 2005; 93: 331–336.
Torbjorner A, Fransson B . Biomechanical aspects of prosthetic treatment of structurally compromised teeth. Int J Prosthodont 2004; 17: 135–141.
Torbjorner A, Fransson B . A literature review on the prosthetic treatment of structurally compromised teeth. Int J Prosthodont 2004; 17: 369–376.
Okeson J P . Management of temporomandibular disorders and occlusion. St. Louis: Mosby, Inc, 2003.
Neff P A . Temporomandibular joint, occlusion and function. Washington DC: Georgetown University School of Dentistry, 1987.
Dawson P E . Functional occlusion: from TMJ to smile design. Mosby, 2006.
Ng C C, al-Bayat M I, Dumbrigue H B, Griggs J A, Wakefield C W . Effect of no ferrule on failure of teeth restored with bonded posts and cores. Gen Dent 2004; 52: 143–146.
Saupe W A, Gluskin A H, Radke R A J . A comparative study of fracture resistance between morphologic dowel and cores and a resin-reinforced dowel system in the intraradicular restoration of structurally compromised roots. Quintessence Int 1996; 27: 483–491.
Mannocci F, Ferrari M, Watson T F . Microleakage of endodontically treated teeth restored with fiber posts and composite cores after cyclic loading: a confocal microscopic study. J Prosthet Dent 2001; 85: 284–291.
Fissore B, Nicholls J I, Yuodelis R A . Load fatigue of teeth restored by a dentin bonding agent and a posterior composite resin. J Prosthet Dent 1991; 65: 80–85.
Hashimoto M, Ohno H, Sano H, Kaga M, Oguchi H . In vitro degradation of resin-dentin bonds analysed by microtensile bond test, scanning and transmission electron microscopy. Biomaterials 2003; 24: 3795–3803.
Hashimoto M, Ohno H, Kaga M, Endo K et al. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J Dent Res 2000; 79: 1385–1391.
Mannocci F, Bertelli E, Watson T F, Ford T P . Resin-dentin interfaces of endodontically-treated restored teeth. Am J Dent 2003; 16: 28–32.
Ferrari M, Vichi A, Grandini S, Goracci C . Efficacy of a self-curing adhesive-resin cement system on luting glass-fiber posts into root canals: an SEM investigation. Int J Prosthodont 2001; 14: 543–549.
de Oliveira J A, Pereira J R, Lins do Valle A, Zogheib L V . Fracture resistance of endodontically treated teeth with different heights of crown ferrule restored with prefabricated carbon fiber post and composite resin core by intermittent loading. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: e527.
Newman M P, Yaman P, Dennison J, Rafter M, Billy E . Fracture resistance of endodontically treated teeth restored with composite posts. J Prosthet Dent 2003; 89: 360–367.
Fokkinga W A, Kreulen C M, Vallittu P K, Creugers N H . A structured analysis of in vitro failure loads and failure modes of fiber, metal, and ceramic post-and-core systems. Int J Prosthodont 2004; 17: 476–482.
Hayashi M, Takahashi Y, Imazato S, Ebisu S . Fracture resistance of pulpless teeth restored with post-cores and crowns. Dent Mater 2006; 22: 477–485. .
Maccari P C, Cosme D C, Oshima H M, Burnett L H J, Shinkai R S . Fracture strength of endodontically treated teeth with flared root canals and restored with different post systems. J Esthet Restor Dent 2007; 19: 30–36, discussion 37.
Dorriz H, Alikhasi M, Mirfazaelian A, Hooshmand T . Effect of ferrule and bonding on the compressive fracture resistance of post and core restorations. J Contemp Dent Pract 2009; 10: 1–8.
Tait C M, Ricketts D N, Higgins A J . Weakened anterior roots-intraradicular rehabilitation. Br Dent J 2005; 198: 609–617.
Bolla M, Muller-Bolla M, Borg C, Lupi-Pegurier L et al. Root canal posts for the restoration of root filled teeth. Cochrane Database Syst Rev 2007; CD004623.
Reeh E S, Douglas W H, Messer H H . Stiffness of endodontically-treated teeth related to restoration technique. J Dent Res 1989; 68: 1540–1544.
Jagadish S, Yogesh B G . Fracture resistance of teeth with Class 2 silver amalgam, posterior composite, and glass cermet restorations. Oper Dent 1990; 15: 42–47.
Hurmuzlu F, Kiremitci A, Serper A, Altundasar E, Siso S H . Fracture resistance of endodontically treated premolars restored with ormocer and packable composite. J Endod 2003; 29: 838–840.
Ausiello P, De Gee A J, Rengo S, Davidson C L . Fracture resistance of endodontically-treated premolars adhesively restored. Am J Dent 1997; 10: 237–241.
Boyer D B, Roth L . Fracture resistance of teeth with bonded amalgams. Am J Dent 1994; 7: 91–94.
Eakle W S . Increased fracture resistance of teeth: comparison of five bonded composite resin systems. Quintessence Int 1986; 17: 17–20.
Gelb M N, Barouch E, Simonsen R J . Resistance to cusp fracture in class II prepared and restored premolars. J Prosthet Dent 1986; 55: 184–185.
McCullock A J, Smith B G . In vitro studies of cusp reinforcement with adhesive restorative material. Br Dent J 1986; 161: 450–452.
Soares P V, Santos-Filho P C, Martins L R, Soares C J . Influence of restorative technique on the biomechanical behaviour of endodontically treated maxillary premolars. Part I: fracture resistance and fracture mode. J Prosthet Dent 2008; 99: 30–37.
Soares P V, Santos-Filho P C, Gomide H A, Araujo C A et al. Influence of restorative technique on the biomechanical behaviour of endodontically treated maxillary premolars. Part II: strain measurement and stress distribution. J Prosthet Dent 2008; 99: 114–122.
Mondelli R F, Ishikiriama S K, de Oliveira Filho O, Mondelli J . Fracture resistance of weakened teeth restored with condensable resin with and without cusp coverage. J Appl Oral Sci 2009; 17: 161–165.
Dietschi D, Duc O, Krejci I, Sadan A . Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behaviour, interfaces, and in vivo studies). Quintessence Int 2008; 39: 117–129.
Cotert H S, Sen B H, Balkan M . In vitro comparison of cuspal fracture resistances of posterior teeth restored with various adhesive restorations. Int J Prosthodont 2001; 14: 374–378.
St-Georges A J, Sturdevant J R, Swift E J J, Thompson J Y . Fracture resistance of prepared teeth restored with bonded inlay restorations. J Prosthet Dent 2003; 89: 551–557.
Allara FW J, Diefenderfer K E, Molinaro J D . Effect of three direct restorative materials on molar cuspal fracture resistance. Am J Dent 2004; 17: 228–232.
Mendoza D B, Eakle W S, Kahl E A, Ho R . Root reinforcement with a resin-bonded preformed post. J Prosthet Dent 1997; 78: 10–14.
al-Hazaimeh N, Gutteridge D L . An in vitro study into the effect of the ferrule preparation on the fracture resistance of crowned teeth incorporating prefabricated post and composite core restorations. Int Endod J 2001; 34: 40–46.
Kurer H G . The classification of single-rooted, pulpless teeth. Quintessence Int 1991; 22: 939–943.
Lawn B R, Pajares A, Zhang Y et al. Materials design in the performance of all-ceramic crowns. Biomaterials 2004; 25: 2885–2892.
Seow L L, Toh C G, Wilson N H . Remaining tooth structure associated with various preparation designs for the endodontically treated maxillary second premolar. Eur J Prosthodont Restor Dent 2005; 13: 57–64.
Pilo R, Shapenco E, Lewinstein I . Residual dentin thickness in bifurcated maxillary first premolars after root canal and post space preparation with parallel-sided drills. J Prosthet Dent 2008; 99: 267–273.
Samet N, Jotkowitz A . Classification and prognosis evaluation of individual teeth-a comprehensive approach. Quintessence Int 2009; 40: 377–387.
Cobankara F K, Unlu N, Cetin A R, Ozkan H B . The effect of different restoration techniques on the fracture resistance of endodontically-treated molars. Oper Dent 2008; 33: 526–533.
Goerig A C, Mueninghoff L A . Management of the endodontically treated tooth. Part II: Technique. J Prosthet Dent 1983; 49: 491–497.
Aquilino S A, Caplan D J . Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 2002; 87: 256–263.
Sorensen J A, Martinoff J T . Clinically significant factors in dowel design. J Prosthet Dent 1984; 52: 28–35.
Liberman R, Judes H, Cohen E, Eli I . Restoration of posterior pulpless teeth: amalgam overlay versus cast gold onlay restoration. J Prosthet Dent 1987; 57: 540–543.
Smales R J, Hawthorne W S . Long-term survival of extensive amalgams and posterior crowns. J Dent 1997; 25: 225–227.
Hernandez R, Bader S, Boston D, Trope M . Resistance to fracture of endodontically treated premolars restored with new generation dentine bonding systems. Int Endod J 1994; 27: 281–284.
Papa J, Cain C, Messer H H . Moisture content of vital vs endodontically treated teeth. Endod Dent Traumatol 1994; 10: 91–93.
Sedgley C M, Messer H H . Are endodontically treated teeth more brittle? J Endod 1992; 18: 332–335.
Panitvisai P, Messer H H . Cuspal deflection in molars in relation to endodontic and restorative procedures. J Endod 1995; 21: 57–61.
Shahrbaf S, Mirzakouchaki B, Oskoui S S, Kahnamoui M A . The effect of marginal ridge thickness on the fracture resistance of endodontically-treated, composite restored maxillary premolars. Oper Dent 2007; 32: 285–290.
Strand G V, Tveit A B, Gjerdet N R, Eide G E . Marginal ridge strength of teeth with tunnel preparations. Int Dent J 1995; 45: 117–123.
Ohlmann B, Gruber R, Eickemeyer G, Rammelsberg P . Optimizing preparation design for metal-free composite resin crowns. J Prosthet Dent 2008; 100: 211–219.
Krejci I, Duc O, Dietschi D, de Campos E . Marginal adaptation, retention and fracture resistance of adhesive composite restorations on devital teeth with and without posts. Oper Dent 2003; 28: 127–135.
Plotino G, Buono L, Grande N M, Lamorgese V, Somma F . Fracture resistance of endodontically treated molars restored with extensive composite resin restorations. J Prosthet Dent 2008; 99: 225–232.
Van Nieuwenhuysen J P, D'Hoore W, Carvalho J, Qvist V . Long-term evaluation of extensive restorations in permanent teeth. J Dent 2003; 31: 395–405.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Jotkowitz, A., Samet, N. Rethinking ferrule – a new approach to an old dilemma. Br Dent J 209, 25–33 (2010). https://doi.org/10.1038/sj.bdj.2010.580
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2010.580
This article is cited by
-
Considerations for restorative dentistry secondary care referrals - part 2: predictability of treatment
British Dental Journal (2022)
-
Does an intracanal composite anchorage replace posts?
Clinical Oral Investigations (2014)