Key Points
-
Provides insight to the location, organisation, case-mix and activity of paediatric dental general anaesthesia services in Yorkshire and Humber.
-
Identifies that no universal monitoring system existed and standards of best practice were often not met.
-
A universal monitoring system would help ensure quality services.
-
Suggests further training is required to meet standards of best practice.
Abstract
Background Following major change in UK policy regarding dental general anaesthesia (DGA) in 2001, there appears to be little information available about paediatric DGA services, their organisation, availability and utilisation.
Aims To establish the location, organisation and monitoring systems of paediatric DGA services in Yorkshire and the Humber Strategic Health Authority and to audit these services against existing standards of best practice.
Design A postal survey of all potential paediatric DGA providers in Yorkshire and the Humber.
Results Thirty-one possible DGA service providers were identified, 24 of which provided paediatric DGAs. Of 84 DGA lists identified, 75 regularly treated children, and nine were run on an ad hoc basis. The lists were held in 20 centres. The number of patients treated per list varied depending on treatment provided, ranging from 3.9 to 7.5 patients per list. Maximum waiting times varied from three to 84 weeks. Outcome data recording methods varied. Just over half of respondents used the Hospital Episode Statistics system; the remainder used other systems, or none.
Conclusions There was much variation in how DGA lists were organised. Most lists met some of the accepted standards, but very few met all. Waiting times were largely in accordance with national targets.
Similar content being viewed by others
Introduction
The provision of dental treatment under general anaesthesia (DGA) in the UK has changed considerably over the past few decades. Until the beginning of this century, DGA was routinely carried out in general dental practice, salaried dental services and hospitals. In the past, the safety of DGA has been a major concern, prompting the publication of recommendations by regulatory bodies.1,2 Following a number of DGA-related deaths, the Department of Health published A Conscious Decision in 2000.3 It highlighted that standards aimed at protecting patients from the potentially serious complications of DGA had not been met and recommended that from 2002, all DGA should take place in a hospital setting only.3
Before 2002 in the UK, the National Health Service (NHS) Dental Practice Board recorded all DGAs provided in general practice, but not in hospitals. Salaried dental service activity data were held by the Department of Health until 1999.3 Since 2002, there appears to have been no reliable recording of DGA activity at a national level.
Most studies of paediatric DGA over the past decade have reported on specific factors such as the need for DGA among those referred,4 trends in provision before and following guidance from the UK General Dental Council (GDC) in 1998,5,6,7,8 and reasons for referral for DGA.9 Today, over eight years since implementation of this major change in policy regarding DGA, there appears to be little information available about UK paediatric DGA services, especially their organisation, availability and utilisation.
Guidelines on the organisation and provision of paediatric DGA were published in 2008 (Table 1).10 Although all aspects of these guidelines were considered in the study, a selection is reported here. The guidelines provide best practice guidance on the DGA process including: explanation of risk and consent process; the need for pre-operative dental assessment and treatment planning; organisation of the clinical setting including the use of skill-mix; clinical record requirements and discharge processes (Table 1).10
The aims of this project were, firstly, to investigate the location, organisation and capacity of paediatric DGA services in Yorkshire and the Humber including outcome data capture and, secondly, to audit these services against existing best practice standards.8,10,11,12
Method
The region chosen for this evaluation was Yorkshire and the Humber Strategic Health Authority (SHA), one of ten strategic health authority areas in England. This SHA is comprised of 14 primary care trusts. Departments of paediatric dentistry are located within the two dental hospitals. There are 13 salaried dental services and 14 hospitals with departments of oral and maxillofacial surgery. The work was a collaborative exercise between the Leeds Dental Institute and School of Clinical Dentistry, Sheffield with support from Yorkshire and the Humber SHA. Current guidelines10 (Table 1) and other accepted standards8,11,12 were taken as 'best practice', against which the findings were audited.
A postal questionnaire was sent to all potential paediatric DGA service providers within Yorkshire and the Humber SHA. The questionnaire was piloted with a selection of 16 service providers in Leeds and Sheffield. Modifications and additions were suggested and this led to the development of a two-part questionnaire. Part A contained three short sections on one page and collected background information regarding DGA provision. Part B comprised 22 multipart questions. It sought more detailed information relating to each DGA list that the service ran, such as the frequency of each list, the estimated waiting times, respondents' best estimate of average number of patients per list etc. Part B also inquired about data recording mechanisms. It was specified that answers should relate only to the treatment of children under the age of 16 years, even where lists provided treatment for children and adults. A DGA list was defined as 'a regularly occurring session, that is, no less frequent than once every two months, morning or afternoon, at which any type of dental treatment is provided for children under general anaesthesia'. The questionnaire can be made available on request.
Where feasible, methods identified as maximising response rates were employed.13,14 Following preliminary notification of the study by letter, questionnaires were posted during May and June 2008, with a reply-paid envelope, to all potential DGA service providers, including departments of paediatric dentistry, clinical directors of salaried dental services and oral and maxillofacial surgery hospital teams within Yorkshire and the Humber SHA. After two weeks a second questionnaire was sent to non-respondents. Telephone follow-up and a third mailing were employed if required. Two of the final wave questionnaires were emailed rather than posted to facilitate communication, and four questionnaires were completed over the phone. The two centres identified through analysis of Part A were contacted by telephone and asked to participate.
Where possible, any ambiguities or omissions were resolved by contacting respondents by telephone or email. Analysis was carried out using SPSS (version 16) and Microsoft Excel®. Differences between disciplines and types of lists were compared using Fisher's exact test. The significance level was set at 0.01.
Results
A completed questionnaire was obtained from all 29 previously known centres which had been initially contacted, giving a 100% response rate. Eleven service providers responded by post to the first wave, 12 to the second wave, and six to the final wave. In addition, two further centres were identified by analysing part A of the questionnaire, amounting to 31 possible DGA service providers. These were as follows: 14 maxillofacial surgery departments (OMFS), 13 salaried dental services (SDS), two departments of paediatric dentistry (DPD) and two general practitioner-led services (GDP). These different services are referred to as 'disciplines' in this report. Twenty-four respondents were involved in the provision of children's DGA; the remainder referred to DGA services nearby (Table 2).
Where data were provided for all-day sessions, these were treated as two lists. Data were also obtained for ad-hoc sessions, such as emergencies or those implemented periodically to manage long waiting times. The providers involved were contacted for clarification and they explained that these lists occurred at very infrequent intervals.
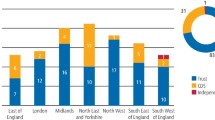
In total, 84 DGA lists on which children were treated were identified. Fifty-two lists ran weekly, one list ran three times per month, nine lists ran fortnightly, 11 lists were monthly lists and two lists ran once every two months. These lists, that is, those running at least once every two months, were considered to be 'regular' lists. The remaining nine lists were labelled 'ad-hoc'. Figure 1 shows a breakdown of 'child-only' lists and 'mixed child and adult' lists and Figure 2 illustrates the types of treatment provided according to discipline.
n = 75. OMFS: oral and maxillofacial surgery. SDS: salaried dental service. DPD: departments of paediatric dentistry. GDP: general dental practitioner. *Definition of regular: 'A regularly occurring session, ie no less frequent than once every two months, morning or afternoon, at which any type of dental treatment is provided for children under general anaesthesia'
Assuming a 40-week year (accounting for annual leave, illness and other reasons for list cancellation), approximately 2,410 regular paediatric DGA lists operated per year (with a mean of 60.3 lists per week) equating to about 13,500 patients receiving treatment annually. As the population of those under 16 years of age in the SHA is estimated to be 979,200 (ONS, 2009), this suggests that approximately 1.4% of the child population undergo a DGA each year. This estimation assumes that each DGA represents a different child, and that cross-border flows of referral are similar and it does not include 'ad-hoc' lists.
The Hospital Episode Statistics (HES) system was used to record DGA activity on 42 (56%) 'regular' lists, 16 (21.3%) did not know what method of data recording was used and the remainder (22.7%) listed ten 'other' methods of data recording.
Lists which were exodontia-only had a mean of 7.5 (SD 1.9) patients per list, 'extractions with minor oral surgery' had 3.5 (SD 1.2) patients and those where restorative care could be provided had a mean of 3.4 (SD 2.8) patients per list (Table 3). The difference in the mean number of patients according to type of treatment provided was found to be statistically significant (p <0.01).
Information on 'average waiting times' and 'longest waiting times' was provided by 73 lists. Waiting times varied according to treatment provided, as illustrated in Table 3, however these differences were not statistically significant. Data on the estimated 'longest waiting time' a patient could expect to wait are not presented but ranged from three to 84 weeks. Twelve (16.4%) lists had estimated 'longest waiting times' of longer than 18 weeks, with six of these being lists on which restorative treatment could be provided for children with special needs. Respondents' best estimates of 'average waiting times' along with ranges are shown in Table 3.
Of the 75 'regular' lists, eight (10.6%) had no pre-operative assessment. Nine (12%) carried out pre-operative assessments on the same day as the DGA and 58 (77.3%) lists held pre-operative assessments on a separate day. The difference between the disciplines regarding when the pre-operative assessment was held was not statistically significant. Forty-nine (65.3%) 'regular' lists had a written referral protocol in place of which 15 (30.6%) were OMFS lists, 30 (61.2%) were SDS lists and four (8.2%) were GDP-led lists. Neither dental school had written referral protocols in place.
Sixty-five (86.7%) 'regular' lists provided information on who confirmed treatment plans. A consultant/specialist in paediatric dentistry confirmed the treatment plan on 21 (32.3%) of these lists, and a consultant/specialist in oral and maxillofacial surgery confirmed treatment plans on 11 (16.9%) lists. A community dental officer confirmed the treatment plan on 22 (33.8%) lists. Staff grade oral surgeons, registrars or house officers, clinical directors and 'other' confirmed treatment plans for the remaining 11 (16.9%) lists. Thirty-six (48%) 'regular' lists had a specialist as the most senior operator: 22 (29.3%) 'regular' lists had an OMFS surgeon and 14 (18.6%) lists had a paediatric dentist. Of the 39 lists which did not have a specialist as the most senior operator, 26 (66%) lists were SDS lists, nine (23%) were OMFS lists and four (10.2%) were GDP-led lists.
Restorative care was available on 28 (37.3%) 'regular' lists, of which 11 lists (39.2%) only offered restorative care under specific circumstances, for example for the medically compromised or those with special needs. Fifteen (53.5%) of the lists providing restorative treatment provided restorative care for all children, including healthy children still entirely in the primary dentition. The types of treatment provided on each 'regular' list are summarised in Table 3.
All carious teeth were not routinely dealt with on twenty-one (28%) of the 'regular' lists. Nineteen (90.4%) of these were OMFS lists and the remainder were GDP-led services. All 14 lists which had a specialist in paediatric dentistry as the most senior operator and 36 (92%) lists with a non-specialist as the most senior operator routinely dealt with all carious teeth at the DGA appointment. Eighteen (82%) lists with an oral and maxillofacial surgeon as the most senior operator did not routinely treat all teeth which had been diagnosed with caries. Over half (53.3%) of the 'regular' lists did not routinely request that the referring dentist provide ongoing preventive care following discharge, of which 25 (62.5%) were OMFS-led, 13 (32.5%) were SDS-led and two (5%) were GDP-led services. All DPD lists requested that the referring dentist provide follow-up preventive care and advice.
Following completion of the DGA, most provided some form of follow-up, with 57 (76%) 'regular' lists having a routine discharge letter, seven (9.3%) providing a routine postoperative review appointment before discharge and eight (10.6%) citing 'other' follow-up such as telephoning the patients.
Discussion
To our knowledge, this is the first evaluation of paediatric DGA services since the introduction of the change in UK policy in 2002.3 It found that there was significant variation in local provision of paediatric DGA in Yorkshire and the Humber with respect to many factors, including waiting times, number of patients per list, treatments provided and recording of data etc. Given the large geographic area and population (5.1 million) covered, these findings arguably represent service provision elsewhere in the UK.
For almost a quarter of lists, respondents were unaware of the recording method used for collection of activity data. Those who did record activity used a wide range of recording methods. Analysis of hospital admissions for child dental care using HES data have been published previously.15,16 However, as approximately half of lists in Yorkshire and Humber did not use this system, their findings should be interpreted with care. Before 2002, DGAs were provided mainly by GDPs and SDS, and were monitored through data recorded by the then Dental Practice Board and Department of Health respectively. Since the change to hospital-only provision of DGA in 2002, the lack of a single activity recording system prevents accurate activity analysis and hinders the monitoring and planning of services. A universal data recording system for all DGA service providers would help inform future service planning and also aid further research in this area.
The respondents' best estimates of the usual waiting times were analysed, and are referred to here as 'average waiting times'. The term 'average' is not intended as a precise statistical expression. There was significant variation in waiting times, although the majority of 'average waiting times' were shorter than 18 weeks. Depending on the list in question, however, children could wait for up to 21 months for their treatment. As poor dental health can have deleterious effects on children's quality of life,17 waiting times of up to 21 months are inconsistent with quality dental care. In this study, however, the vast majority of lists had waiting times of shorter than 18 weeks. The NHS initiative of target waiting times of no more than 18 weeks was in place at the time of this study, however, this initiative has since ceased.18 The mean number of patients (3.5) on lists where restorative care could be provided was higher than anticipated. This may be due to some lists only very occasionally providing restorative care. Further, more detailed investigation of the case mix of lists would be useful to inform commissioning decisions.
Referral letters should include the reasons for prescribing DGA, the patient's medical history and a clear indication for the treatment requested.10 Existing data suggest that referrals are often inadequate.6,9,19,20,21 In this study, over one third of lists did not have a referral protocol. A well-designed and agreed referral protocol would ensure provision of adequate information, introducing an element of consistency and control into the process and ensuring that professional responsibilities are being met.
Current guidelines10 state that the pre-operative dental assessment should be held on a separate day to the DGA in order to allow time to investigate medical conditions; confirm or amend the referrer's treatment requests; take appropriate radiographs or gain an orthodontic opinion; and to ensure that the requirements for obtaining informed consent are met.20,22 The introduction of an assessment appointment has been found to reduce the prescription of DGA and need for repeat DGA.23 This study found that over one fifth (22.7%) of regular lists had no pre-operative dental assessment or conducted the pre-operative dental assessment on the same day as the DGA. This suggests that in spite of recommendations to the contrary,19 some DGA operators work to the referring dentist's prescription without performing their own assessment.
Treatment plans provided by referring dentists are often altered by DGA providers, with respect to choice of behaviour management technique as well as the number of teeth treated.20,24 Referring dentists may fail to detect all caries, especially if the child was difficult to examine, and additional caries may develop during their wait for DGA. Furthermore, where the child presents fasted and prepared for a DGA, it may prove difficult to offer alternative treatment modalities, and unnecessary DGAs may be performed.11 Same-day routine GA is inconsistent with the practice of other surgical specialties and should be questioned.24
Treatment of all carious teeth in one episode (comprehensive care) has been recommended to reduce the risk of repeat DGA.19 A significant proportion of 'regular' lists did not routinely treat all diagnosed caries under one DGA. Patients were significantly less likely to have had diagnosed caries treated on OMFS-led lists, although the small sample size should be considered when interpreting these results. It could be argued that OMFS procedures such as exposure or removal of supernumeraries or impacted teeth are often carried out in isolation from caries management. It is, however, considered good practice to treat all carious teeth in advance of DGA for minor oral surgery or, if that is not possible, to include all carious teeth in the DGA treatment plan.20 This again emphasises the importance of an appropriate pre-anaesthetic assessment.19,24
Studies have indicated that pre-operative assessment by a specialist in paediatric dentistry is associated with a reduction in repeat DGAs, possibly due to more comprehensive planning.23,24 A specialist in paediatric dentistry was the most senior operator on less than one fifth of lists in this study, but as there are currently only 20 specialist paediatric dentists registered in Yorkshire and the Humber SHA, it would be unrealistic for all the lists to include their involvement, either at the pre-assessment stage or during actual treatment. SDS officers were the most senior operators on over a third of lists. Although not specialists, such clinicians often have significant experience of working with children, especially those with special needs and all SDS lists in this study routinely dealt with all carious teeth at the DGA appointment, reducing the potential for repeat DGA. Involvement of the specialists in paediatric dentistry in paediatric DGA training could improve the quality of referrals as well as pre-operative assessment and comprehensive treatment planning.
It appears from this study that restoration of primary teeth under GA is only available to a small minority, with extraction-only the sole option available to most. On 11 'regular' lists, restorative care was only available where the child had special needs, a significant medical condition or where permanent teeth were present. The terms 'special needs' and 'medically compromised' were used in the questionnaire; however, these terms are open to various interpretations, for example a child with an extreme dental anxiety or phobia may not be defined as having a 'special need' in some centres, but may in others. This issue did not arise in the piloting process but in retrospect it would have been helpful to provide a definition of these terms to avoid ambiguity. The question of provision of dental care under general anaesthesia for children with additional needs was not the focus of this study, but is certainly an area for future research and indeed, oral health inequalities for those with disabilities have been highlighted again recently.28
The majority of DGA lists provided follow up in the form of a discharge letter. Discharge letters may be useful in raising the issue of the need for future prevention. Over half did not request that the referring dentist provide preventive care and advice following discharge. As children who have undergone DGA are at high risk of further dental disease and repeat GA,9,25 it is of concern that over half of lists did not include post-operative preventive strategies and that three lists did not provide any post-DGA follow up. It would be beneficial to emphasise the importance of prevention for these children, as outlined in Delivering Better Oral Health.26
Conclusions
There was no universal data recording mechanism for paediatric DGA with many respondents not using the HES coding system. There was much variation in how DGA lists were organized and although there was no consistent pattern of deficiency, many lists did not meet all current guideline standards and other accepted principles. Absence of agreed referral protocols and lack of, or unstructured approach to, pre-operative treatment planning consultation and assessment were among the issues identified. Although most complied with the NHS 18-week waiting time initiative, there were inequities in waiting times for, and access to different services. In addition, the maximum times patients could wait were considerable in several areas. The availability of restorative care varied considerably suggesting that some children in the region may be disadvantaged in this respect. These findings are specific to Yorkshire and Humber, and although they could be generalised to other regions in the UK, further investigation of paediatric DGA services here and in other regions would contribute to a country-wide situational analysis.
References
Poswillo D. General anaesthesia, sedation and resuscitation in dentistry: report of an expert working party prepared for the Standing Dental Advisory Committee. London: Department of Health, 1990.
The Royal College of Anaesthetists. Standards and guidelines for general anaesthesia for dentistry. London: Royal College of Anaesthetists, 1999.
Department of Health. A conscious decision: a review of the use of general anaesthesia and conscious sedation in primary dental care. Department of Health, London 2000. Gateway reference 21967.
Tyrer G L. Referrals for dental general anaesthetics – how many really need GA? Br Dent J 1999; 183: 440–443.
Jones C, Taylor G, Morrant A, Cook G . Paediatric dental general anaesthesia rates and dental caries regionally and in districts in the former north western region. Community Dent Health 1998; 15: 162–167.
Clewett J A, Treasure E T . A retrospective study of dental general anaesthesia carried out in children living in North Wales 1995-1998. Community Dent Health 2004; 21: 212–216.
Whittle J G. The provision of primary care dental general anaesthesia and sedation in the northwest region of England, 1996-1999. Br Dent J 2000; 189: 500–502.
General Dental Council. Amendments to Maintaining standards: guidance to dentists on professional and personal conduct. London: General Dental Council, 1997. Amendments approved 2001. Available from http://www.gdc-uk.org/NR/rdonlyres/F7730541-EC84-4001-9F57-5A0ABD246CFD/15200/MaintainingStandards.pdf. Accessed 23 November 2010.
Albadri S S, Lee S, Lee G T, Llewelyn R, Blinkhorn A S, Mackie I C . The use of general anaesthesia for the extraction of children's teeth. Results from two UK dental hospitals. Eur Arch Paediatr Dent 2006; 7: 110–115.
Davies C, Harrison M, Roberts G . UK national clinical guidelines in paediatric dentistry: guideline for the use of general anaesthesia (GA) in paediatric dentistry 2008. London: Royal College of Surgeons of England, 2008. Available from http://www.rcseng.ac.uk/fds/publications-clinical-guidelines/ clinical_guidelines/documents/Guideline%20for%20the%20 use%20of%20GA%20in%20Paediatric%20Dentistry%20May%202008%20Final.pdf. Accessed 26 October 2010.
Clayton M, Mackie I C . The development of referral guidelines for dentists referring children for extractions under general anaesthesia. Br Dent J 2003; 194: 561–565.
Fayle S A, Welbury R R, Roberts J F . British Society of Paediatric Dentistry: a policy document on management of caries in the primary dentition. Int J Paediatr Dent 2001; 2: 153–157.
Edwards P, Roberts I, Clarke M et al. Methods to increase response rates to postal questionnaires. Cochrane Database Syst Rev 2009; 3: MR000008. DOI: 10.1002/14651858.MR000008.pub4.
Dillman D. Mail and internet surveys: the tailored design method. 2nd ed. New York: Wiley, 2000.
Thomas S J, Atkinson C, Hughes C, Revington P, Ness A R . Is there an epidemic of admissions for surgical treatment of dental abscesses in the UK? Brit Med J 2008; 336: 1219–1220.
Moles D R, Ashley P . Hospital admissions for dental care in children: England 1997-2006. Br Dent J 2009; 206: E14.
Sheiham A. Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J 2006; 201: 625–626.
Department of Health 2010: Revision to the Operating Framework for the NHS in England 2010/11. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_110107. Accessed 23 November 2010.
Harrison M, Nutting L . Repeat general anaesthesia for paediatric dentistry. Br Dent J 2000; 189: 37–39.
Landes D P, Clayton-Smith A J . The role of pre-general anaesthetic assessment for patients referred by general dental practitioners to the Community Dental Service. Community Dent Health 1996; 13: 169–171.
Macpherson L M, Pine C M, Tochel C, Burnside G, Hosey M T, Adair P . Factors influencing referral of children for dental extractions under general and local anaesthesia. Community Dent Health 2005; 22: 282–288.
Nunn J, Foster M, Master S, Greening S . British Society of Paediatric Dentistry: a policy document on consent and the use of physical intervention in the dental care of children. Int J Paediatr Dent. 2008; 18 Suppl 1: 39–46.
Grant S M, Davidson L E, Livesey S . Trends in exodontia under general anaesthesia at a dental teaching hospital. Br Dent J 1998; 185: 347–352.
Tochel C, Hosey M T, Macpherson L M, Pine C M . Assessment of children prior to dental extractions under general anaesthesia in Scotland. Br Dent J 2004; 196: 629–633.
Almeida A G, Roseman M M, Sheff M, Huntington N, Hughes C V . Future caries susceptibility in children with early childhood caries following treatment under general anaesthesia. Pediatr Dent 2000; 22: 302–306.
Department of Health and British Association for the Study of Community Dentistry. Delivering better oral health. An evidence based toolkit for prevention. 2nd edition. London: Department of Health, 2009. Gateway reference 12231. Available from http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_102331. Accessed 26 October 2010.
The Children Act 2004. London: Her Majesty's Stationery Office, 2004. Available from http://www.legislation.gov.uk/ukpga/2004/31/contents. Accessed 26 October 2010.
Owens J, Dyer T A, Mistry K . People with learning disabilities and specialist services. Br Dent J 2010; 208: 203–205.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Ní Chaollaí, A., Robertson, S., Dyer, T. et al. An evaluation of paediatric dental general anaesthesia in Yorkshire and the Humber. Br Dent J 209, E20 (2010). https://doi.org/10.1038/sj.bdj.2010.1081
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2010.1081
This article is cited by
-
Variations in provision of dental general anaesthetic for children in England
British Dental Journal (2022)
-
A rapid review of variation in the use of dental general anaesthetics in children
British Dental Journal (2020)
-
Frequency, variation and cost of dental extractions for adults in secondary care in Great Britain
British Dental Journal (2019)
-
Prevention in the context of caries-related extractions under general anaesthesia: an evaluation of the use of sealants and other preventive care by referring dentists
British Dental Journal (2019)
-
Neighbourhood incidence rate of paediatric dental extractions under general anaesthetic in South West England
British Dental Journal (2018)