Key Points
-
Optimal intake of vitamin D and calcium slows bone resorption and ensures adequate calcium for bone mineralisation.
-
Optimal levels of vitamin D should have an immunosuppressive effect on periodontal disease.
-
Older adults, particularly those with dark skin colour and/or those who live in northern latitudes, should consider oral vitamin D supplementation.
Abstract
Objectives To determine the level of calcium and vitamin D oral supplementation in patients in periodontal disease maintenance programmes.
Design Convenience survey.
Setting St. Louis Metropolitan region.
Subjects and methods Patients (n = 228) in two university-based, periodontal disease maintenance programmes.
Main outcome measures Reported amounts of oral calcium and vitamin D supplementation were tested for differences based on gender and race.
Results The last published recommended daily intakes from the United States (US) Food and Nutrition Board (FNB) for adults >50 years of age are 1,200 mg calcium and 400 IU vitamin D (or 600 IU if over 70). The mean age of the 228 patients (125 females and 103 males) was 63.6 ± 11.0 years (standard deviation). Of the 228 patients surveyed: (1) 204 (89%) were >50 years of age and of these, only 15 (7%) met the US FNB's recommended intakes of calcium and vitamin D from supplementation; (2) 138 (66%) reported that they took no oral supplementation, with significantly more males (n = 82) than females (n = 56) not taking supplementation (p = 0.03); (3) 88 (39%) took calcium supplementation, with females (947 ± 511 mg/day) taking significantly (p <0.001) more than males (632 ± 907 mg/day); and (4) 66 (29%) took vitamin D supplementation, with females(420 ± 227 IU/day) taking approximately the same amount as males (443 ± 317 IU/day, p >0.05). The amounts of oral supplementation did not vary with race (p >0.05).
Conclusion The use of calcium and vitamin D supplementation has been promoted for years, yet the numbers of adults taking supplements remains low and the level of supplementation varies greatly. Knowledge of the benefits of supplementation needs to be better disseminated and research needs to be conducted to determine optimal levels of calcium and vitamin D supplementation.
Similar content being viewed by others
Introduction
Oral bone mass increases throughout infancy, childhood and adolescence to reach a genetically determined peak bone mass in early adulthood. Thereafter, the oral bone, just as total skeletal bone, loses bone mass. The rate of increase and loss is dependent upon heredity and the availability of calcium and vitamin D. If calcium intakes are inadequate, skeletal calcium is resorbed to maintain the body's calcium homeostasis, which is essential for life-sustaining processes such as blood clotting, muscle contraction and nerve excitability. The resorption of the body's calcium is mediated by parathyroid hormone (PTH), which increases osteoclastic activity in bone to release stored calcium to the circulation and increases the synthesis of 1,25-dihydroxyvitamin D [1,25(OH)2D] (the biologically active form of vitamin D), which in turn increases the absorption of calcium from the intestine. The best way to estimate vitamin D intake is to measure the serum levels of 25-hydroxyvitamin D [25(OH)D].1 When serum levels of 25(OH)D are low, there is decreased calcium absorption, increased PTH secretion and increased osteoclastic activity.
In a September 2002 review of 180 articles on bone status and calcium intake, it was reported that 68 of 70 (97%) randomised clinical trials found that individuals who received calcium supplementation had greater gains in bone during growth, less loss of bone with age and/or reduced fracture risk, relative to unsupplemented individuals, and that 85 of 110 (77%) observational studies found positive effects for calcium supplementation.2 It is also well established that vitamin D is essential for bone growth and that it has its greatest effect when combined with calcium supplementation.3,4,5
Dietary reference intakes [the last published recommendations of the US Institute of Medicine's Food and Nutrition Board (FNB)] suggests a total intake from diet and oral supplementation of 1,200 mg/day calcium and 400 IU (10.0 μg)/day vitamin D for ages 51-70 and for those >70 years of age, 1,200 mg calcium/day and 600 IU vitamin D (15.0 μg)/day.6 In the US, the median calcium intake for men 50 to 70 years of age is 708 mg/day and for women 571 mg/day, and 702 and 517 mg/day respectively for those >70 years of age.7 Therefore, on average, adult men and women need to consume an additional 500-600 mg/day of calcium through food or supplementation, just to meet health needs.
There is also growing concern that recent studies have identified high prevalences of vitamin D insufficiency in otherwise healthy adults and that current FNB recommendations of vitamin D intake are inadequate. A number of investigators convincingly argue that serum 25(OH)D levels <70-80 nmol/l are deficient.8 Another source for information, the National Osteoporosis Foundation (NOF), recommends 1,000 mg calcium and 400-800 IU vitamin D daily for adults <50 years of age, and for those >50 years of age, 1,200 mg calcium and 800-1,000 IU vitamin D daily.9 A periodontal disease vitamin D study of the Third National Health and Nutrition Examination Survey (NHANES III) data found that the majority of subjects had serum 25(OH)D levels far below 80 nmol/l.10 As pointed out in recent studies, the older recommendations of 400 or 600 IU vitamin D/day were intended to maintain health and are inadequate for correcting vitamin D insufficiencies.11
It is reasonable to think that calcium and vitamin D affect oral bone in the same way that they affect other bones of the body, and various studies, including analyses of data from NHANES III, have found associations between periodontal health and intakes of calcium and vitamin D.10,12 Researchers have found that (1) optimal intakes of calcium and vitamin D slow bone resorption and speed bone formation, thereby reducing bone loss,13 (2) vitamin D stimulates the expression of antimicrobial peptides (α- and β-defensins and cathelicidins),14,15 and (3) vitamin D has an immunosuppressive effect on periodontal disease.10 As the levels of calcium and vitamin D oral supplementation for patients with periodontal disease are unknown, the purpose of this study was to survey adult patients in two university-based periodontal disease maintenance programmes to determine their levels of calcium and vitamin D oral supplementation.
Methods
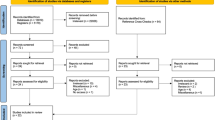
Study population
We conducted our survey at Southern Illinois University School of Dental Medicine (SIU-SDM) in Alton, Illinois and the Saint Louis University Center for Advanced Dental Education (SLU-CADE) in St. Louis, Missouri. Study subjects were recruited from periodontal disease recall programmes based at these two institutions, whose patient populations are from the Greater St. Louis region, an area comprising 12 counties in Eastern Missouri and Southern Illinois. According to the latest US census, this area has a population of approximately 2.3 million, which makes it the 18th largest market area in the United States. There are approximately 920 patients in the periodontal disease maintenance programme at Southern Illinois University and 200 at Saint Louis University.
Patient questionnaire
We obtained Institutional Review Board (IRB) approvals for our protocol and our use of a brief patient questionnaire at SIU-SDM, SLU-CADE and Washington University in St. Louis (principal investigator's home institution). Signs were posted in the periodontal maintenance programme dental operatories at SIU-SDM and SLU-CADE, with the signs informing patients of a potential research study involving calcium and vitamin D. Interested patients were invited to complete our brief questionnaire, which requested information on age, gender, number of years postmenopausal, use of vitamin D and/or calcium supplements (including multivitamins and antacids), and use of bone-active prescription drugs such as risedronate (Actonel, Procter & Gamble Pharmaceuticals, Inc.), alendronate (Fosamax, Merck Co., West Point, VA), raloxifene (Evista [raloxifene hydrochloride, a selective oestrogen receptor modulator (SERM)], Eli Lilly and Company, Indianapolis, IN), or oestrogen. Questionnaires were checked for completeness, and if additional information on amounts of calcium and vitamin D was needed after the patients had gone home, they were contacted by telephone.
Data analysis
Data are reported as means ± standard deviation. For categorical variables, frequencies were calculated for patients who were or were not taking calcium/vitamin D and/or bone-active prescription drugs. Distributions of age, mg of calcium taken per day and international units (IUs – 40 IU = 1 μg) of vitamin D taken per day were tested for normality with the Shapiro-Wilk W test, and equality of variances were tested with O'Brien, Brown-Forsythe, Levene, and Bartlett tests. Differences in responses based on gender, menopausal status and race were tested for statistical significance with the chi-square test, Fisher's exact test, analysis of variance (ANOVA) and Student's t test. If data were non-normally distributed and/or variances were not equal, the Welch ANOVA and/or Wilcoxon tests were used. For those who took neither calcium nor vitamin D oral supplementation, the binomial test was used to determine if there were more males than females. This test is used when there are only two possible outcomes, with fixed rates of occurrence – in this case 0.5 for males and 0.5 for females.16 The chi-square goodness-of-fit test was used to test for differences in racial proportions between respondents and the St. Louis region. If for the chi-square test, 20% of the cells had expected counts of less than 5, exact p values were calculated by means of data permutation. If default time limits were exceeded for calculations of exact p values, Monte Carlo estimates were used. Monte Carlo estimates and exact calculations of p values were performed with StatXact Statistical Software for Exact Nonparametric Inference (Version 6 with Cytel Studio™, Cytel Software Corporation, Cambridge, MA). All other statistical testing was performed with JMP Statistical Software (SAS Institute, Inc., Cary, NC).
Results
From May 2003 through September 2004, 228 questionnaires were completed and returned. The racial make-up of the pooled sample was not significantly different (p = 0.15) from that for the St. Louis region. The mean age of the 228 patients surveyed was 63.6 ± 11.0 years, with 204 (89%) being over the age of 50 years. Males were significantly older (64.2 ± 9.5 years) than females (58.8 ± 11.9 years, Table 1). Postmenopausal women were significantly older than pre-menopausal women (p <0.0001), and African Americans were significantly younger than Whites (p <0.05).
Eighty-eight patients reported taking oral calcium supplementation. Females took significantly more calcium than did men (p <0.001). The percentage of African Americans, who we surveyed who took calcium (13.6%, n = 12, Table 1) was higher than the percentage of African Americans living in the St. Louis region (9.6%). Conversely, the percentage of Whites who we surveyed who took calcium (84.1%, n = 74, Table 1) was lower than the percentage of Whites living in the St. Louis region (87.9%).
Sixty-six patients reported taking oral vitamin D supplementation. Unlike what was observed with calcium, there was no significant difference between men and women in the amounts of vitamin D supplementation taken. There was also no variation in vitamin D oral supplementation by race when compared to the makeup of the St. Louis region (p >0.05, Table 1).
Among all subjects studied, 64 of the 228 (28%) took both oral calcium and vitamin D supplementation and 138 of the 228 (61%) took no oral supplementation. Insufficient calcium and vitamin D intake, as assessed by supplementation amounts, was seen in 93% of the study population (Table 2).
Thirty-three patients reported use of bone-active prescription drugs used for osteoporosis, specifically risedronate (n = 5), alendronate (n = 13), oestrogen (n = 4), raloxifene (n = 10) and 1 unknown drug (unable to follow up with patient). Ninety-one percent of these patients were females, 97% were postmenopausal; and 91% were White (Table 1). Fifteen (45%) of these 33 patients indicated use of calcium supplements (1,252 ± 456 mg/day) and 11 (33%) of the 33 indicated use of vitamin D supplements (473 ± 185 IU/day).
Discussion
With regard to periodontal disease, the many benefits of calcium and/or vitamin D include strengthening the bone,13 stimulating an antimicrobial effect14,15 and providing an immunosuppressive effect.10
The self-reported calcium and vitamin D intake levels would be insufficient by themselves to prevent deficiencies in our older adult population. Periodontal maintenance patients receive no advice concerning calcium and vitamin D intake at either institution. Accurate estimates of total intakes of calcium and vitamin D for our study subjects would have required performing dietary analyses, assessing sunlight exposures, or (in the case for vitamin D) assessing serum levels of 25(OH)D – none of which were done for our study. Nevertheless, of the patients we surveyed, 204 (89%) of 228 were over the age of 50 and based on the recommendations given in U.S. dietary reference intakes,6 of these, only 15 (7%) obtained adequate intakes of calcium and vitamin D from oral supplementation and only six (0.03%) met the higher recommendations of the National Osteoporosis Foundation.9 Other studies of St. Louis women also indicate inadequate intakes (food and oral supplementation) of calcium and vitamin D.17,18
The median calcium intakes (food plus oral supplementation) in the US for men 50 to 70 years of age is 708 mg/day and for women 571 mg/day. Over the age of 70, the respective median intakes are 702 and 517 mg/day.7 U. S. dietary reference intakes contains no table for vitamin D intakes such as it does for calcium; however, there is growing concern among researchers that recent studies have identified an alarming prevalence of vitamin D insufficiency in otherwise healthy adults and a re-emergence of vitamin D deficiency-induced rickets.19 Many researchers now believe that for adults, daily supplementation with vitamin D at levels of at least 800 to1,000 IU (20 and 25 μg)/day would be safe and beneficial to health, and that the US Food and Nutrition Board (FNB) of the Institute of Medicine needs to raise the recommended levels of intake for vitamin D.8
Dental studies of the effects of calcium and vitamin D on alveolar bone, periodontal health and tooth retention
It has been found that increased periodontal attachment loss is related to decreased intakes of both calcium and vitamin D.10,12 The investigators suggested that inadequate calcium intake increased risk of periodontal disease and could be related to decreased alveolar bone density. Inadequate intake of vitamin D could increase levels of periodontal disease either through an effect on bone mineral density or a suppression of vitamin D's immunomodulatory effects.12 The anti-inflammatory effects of vitamin D (particularly the suppression of cytokine production) and vitamin D's inducing of the production of antimicrobial cathelicidin have been noted by various investigators.15,20,21,22,23,24 There have been a number of studies that indicate that calcium/vitamin D intakes affect alveolar bone, periodontal health and tooth retention, and even though there were limitations associated with these studies, there is strong evidence that calcium and vitamin D intake are positively associated with periodontal/alveolar bone health.25
Anti-resorptive agents
Fourteen percent (33/228) of the patients took bone-active prescription drugs, with the majority being female. Some patients in our study took risedronate or alendronate, which are bisphosphonates, which may improve periodontal health but also may cause osteonecrosis and painful refractory bone exposures of the jaws.26,27,28,29,30,31 The incidence of osteonecrosis of the jaw in patients taking oral bisphosphonate therapy for osteoporosis is low, with a reported risk of less than 1 in 100,000 patients.32 Some of the patients in our study took oestrogen, which may benefit periodontal health.33,34,35,36 Other patients in our study took raloxifene [a selective oestrogen receptor modulator, SERM]. No study has been published on the effect of this anti-resorptive agent on periodontal health.
Study limitations
The results of our study were drawn from self-reported questionnaires. Although the data were unconfirmed (except by telephone in a few cases), we gained knowledge about the use of oral calcium and vitamin D supplementation in a group of adults with known periodontal disease.
Conclusion
Calcium and vitamin D supplements are reasonably priced and widely available, yet many older adults in the US take neither calcium nor vitamin D supplementation, and of those who do, intake levels are often inadequate.
Randomised clinical trials and observational studies have consistently demonstrated positive effects of calcium and/or vitamin D oral supplementation on postcranial (below the head) and alveolar bone.25 There are few health concerns associated with calcium and vitamin D use, but perhaps more important, there is considerable potential for health benefits,37 including periodontal health. Dentists and dental health professionals should advise all of their adult patients to follow the National Osteoporosis Foundation's daily intake recommendations of 1,000 mg calcium and 400–800 IU vitamin D for adults <50 years of age, and 1,200 mg calcium and 800–1,000 IU vitamin D for adults >50 years of age. Controlled studies should be conducted to establish the extent to which adequate intakes of calcium and vitamin D can stabilise/improve periodontal health.
References
Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. pp 253. Washington, DC: National Academy Press, 1997.
Heaney R P. The importance of calcium intake for lifelong skeletal health. Calcif Tissue Int 2002; 70: 70–73.
Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 2001; 22: 477–501.
Papadimitropoulos E, Wells G, Shea B et al. Meta-analyses of therapies for postmenopausal osteoporosis. VIII. Meta-analysis of the efficacy of vitamin D treatment in preventing osteoporosis in postmenopausal women. Endocr Rev 2002; 23: 560–569.
Shea B, Wells G, Cranney A et al. Meta-analyses of therapies for postmenopausal osteoporosis. VII. Meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis. Endocr Rev 2002; 23: 552–559.
Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. pp 115–117, 273–275. Washington, DC: National Academy Press, 1997.
Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. pp 388–389. Washington, DC: National Academy Press, 1997.
Dawson-Hughes B, Heaney R P, Holick M F et al. Estimates of optimal vitamin D status. Osteoporos Int 2005; 16: 713–716.
National Osteoporosis Foundation. National Osteoporosis Foundation's updated recommendations for calcium and vitamin D intake. [NOF Scientific Statement]. National Osteoporosis Foundation, 2008. http://www.nof.org/prevention/calcium_and_VitaminD.htm.
Dietrich T, Joshipura K J, Dawson-Hughes B, Bischoff-Ferrari H A. Association between serum concentrations of 25-hydroxyvitamin D3 and periodontal disease in the US population. Am J Clin Nutr 2004; 80: 108–113.
Heaney R P. Barriers to optimizing vitamin D3 intake for the elderly. J Nutr 2006; 136: 1123–1125.
Nishida M, Grossi S G, Dunford R G et al. Calcium and the risk for periodontal disease. J Periodontol 2000; 71: 1057–1066.
Frost H M. Remodeling as a determinant of envelope physiology. In Bone remodeling and its relationship to metabolic bone diseases. pp 28–53. Springfield, IL: Charles C. Thomas, 1973.
Cannell J J, Zasloff M, Garland C F, Scragg R, Giovannucci E . On the epidemiology of influenza. Virol J 2008; 5: 29.
Gombart A F, Borregaard N, Koeffler H P . Human cathelicidin antimicrobial peptide (CAMP) gene is a direct target of the vitamin D receptor and is strongly upregulated in myeloid cells by 1,25-dihydroxyvitamin D3. FASEB J 2005; 19: 1067–1077.
Levin R I, Rubin D S . Applied elementary statistics. Englewood Cliffs, NJ: Prentice-Hall, 1980.
Hildebolt C F, Pilgram T K, Dotson M et al. Attachment loss with postmenopausal age and smoking. J Periodontal Res 1997; 32: 619–625.
Villareal D T, Civitelli R, Chines A, Avioli L V . Subclinical vitamin D deficiency in postmenopausal women with low vertebral bone mass. J Clin Endocrinol Metab 1991; 72: 628–634.
Holick M F. Resurrection of vitamin D deficiency and rickets. J Clin Invest 2006; 116: 2062–2072.
Murakami M, Ohtake T, Dorschner R A, Gallo R L . Cathelicidin antimicrobial peptides are expressed in salivary glands and saliva. J Dent Res 2002; 81: 845–850.
Wang T T, Nestel F P, Bourdeau V et al. Cutting edge: 1,25-dihydroxyvitamin D3 is a direct inducer of antimicrobial peptide gene expression. J Immunol 2004; 173: 2909–2912.
Cannell J J, Vieth R, Umhau J C et al. Epidemic influenza and vitamin D. Epidemiol Infect 2006; 134: 1129–1140.
Liu P T, Stenger S, Li H et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science 2006; 311 (5768): 1770–1773.
Zittermann A. Vitamin D in preventive medicine: are we ignoring the evidence? Br J Nutr 2003; 89: 552–572.
Hildebolt C. Effect of vitamin D, calcium on periodontitis. J Periodontol 2005; 76: 1576–1587.
Takaishi Y, Miki T, Nishizawa Y, Morii H . Clinical effect of etidronate on alveolar pyorrhoea associated with chronic marginal periodontitis: report of four cases. J Int Med Res 2001; 29: 355–365.
Jeffcoat M K, Reddy M S . Alveolar bone loss and osteoporosis: evidence for a common mode of therapy using the bisphoshonate alendronate. In Davidovitch Z, Norton L (eds) The biologic mechanism of tooth resorption and replacement by implants. pp 365–373. Boston: Harvard Society for the Advancement of Orthodontics, 1996.
Rocha M, Nava L E, Vazquez de la Torre C et al. Clinical and radiological improvement of periodontal disease in patients with type 2 diabetes mellitus treated with alendronate: a randomized, placebo-controlled trial. J Periodontol 2001; 72: 204–209.
Lane N, Armitage G C, Loomer P et al. Bisphosphonate therapy improves the outcome of conventional periodontal treatment: results of a 12-month, randomized, placebo-controlled study. J Periodontol 2005; 76: 1113–1122.
Marx R E, Sawatari Y, Fortin M, Broumand V . Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg 2005; 63: 1567–1575.
Migliorati C A, Schubert M M, Peterson D E, Seneda L M . Bisphosphonate-associated osteonecrosis of mandibular and maxillary bone: an emerging oral complication of supportive cancer therapy. Cancer 2005; 104: 83–93.
Grbic J T, Landesberg R, Lin S Q et al. Incidence of osteonecrosis of the jaw in women with postmenopausal osteoporosis in the health outcomes and reduced incidence with zoledronic acid once yearly pivotal fracture trial. J Am Dent Assoc 2008; 139: 32–40.
Payne J B, Zachs N R, Reinhardt R A, Nummikoski P V, Patil K . The association between estrogen status and alveolar bone density changes in postmenopausal women with a history of periodontitis. J Periodontol 1997; 68: 24–31.
Krall E A, Dawson-Hughes B, Hannan M T, Wilson P W, Kiel D P . Postmenopausal estrogen replacement and tooth retention. Am J Med 1997; 102: 536–542.
Paganini-Hill A. The benefits of estrogen replacement therapy on oral health. The Leisure World cohort. Arch Intern Med 1995; 155: 2325–2329.
Civitelli R, Pilgram T K, Dotson M et al. Alveolar and postcranial bone density in postmenopausal women receiving hormone/estrogen replacement therapy: a randomized, double-blind, placebo-controlled trial. Arch Intern Med 2002; 162: 1409–1415.
Food and Nutrition Board, Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. Washington, DC: National Academy Press, 1997.
Acknowledgements
This publication was made possible by Grant Number R21 DE016918-01A2 from the National Institute of Dental and Craniofacial Research (NIDCR) and Grant Number UL1 RR024992 from the National Center for Research Resources (NCRR), components of the US National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIDCR, NCRR, or NIH.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Dixon, D., Hildebolt, C., Miley, D. et al. Calcium and vitamin D use among adults in periodontal disease maintenance programmes. Br Dent J 206, 627–631 (2009). https://doi.org/10.1038/sj.bdj.2009.519
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2009.519
This article is cited by
-
Serum levels of 25-hydroxyvitamin D are associated with periodontal disease
Clinical Oral Investigations (2017)
-
Osteoporosis and Periodontitis
Current Osteoporosis Reports (2016)
-
Intakes of calcium, vitamin D, and dairy servings and dental plaque in older Danish adults
Nutrition Journal (2013)