Key Points
-
Highlights the importance of monitoring the development of the dentition: the patients were predominantly children and adolescents.
-
Clearly there is no 'one solution fits all'. Interceptive treatment was evident: to harness growth, improve aesthetics and provide the foundation for future dentistry.
-
There are cost implications in the management of this group of dentally compromised patients.
Abstract
Aim To gather information about planned treatment, outcomes and type of patient attending a multidisciplinary hypodontia clinic over a five year period at Glasgow Dental Hospital and School.
Study design There were three parts to the study: (i) to report demographics of the patients with hypodontia attending the multidisciplinary clinic from its outset in February 2002 until February 2007; (ii) to report on both the treatment planned on the clinic and whether this was completed as intended; and (iii) to show the number of patients for whom implants were considered.
Methods The existing hypodontia database was analysed, supplemented where required by data gathered retrospectively from patients' clinical records and radiographs.
Results In the demographic component there were 108 patients seen between February 2002 and February 2007, 57% female patients with a mean age of 13 years. Ninety-one percent (n = 107) of patients were missing two or more teeth, with the most common missing teeth being upper lateral incisors. Orthodontic therapy was most frequently considered in treatment planning. Nineteen patients (23%) may require dental implants.
Conclusions The majority of the patients were female, adolescent and had a positive or suspected family history of hypodontia. Orthodontic therapy was most frequently considered in treatment planning. Nineteen patients may undergo surgery for placement of dental implants.
Similar content being viewed by others
Introduction
Hypodontia is the congenital absence of teeth and is one of the most common dental anomalies in man.1 There are both genetic2,3 and environmental4,5 components to the aetiology of hypodontia.6 It can be associated with cleft lip/palate and other genetic syndromes.7,8,9 Various genes have been implicated, such as MSX, PAX9 and TGFA.10,11,12,13,14,15
Management of hypodontia can be challenging as not only is this often complex but also various treatment options exist. Thus treatment planning may involve multiple dental disciplines and treatment phases. Treatment options may range from no clinical intervention through to simple fixed and removable restorative procedures, and finally to combined orthodontic, restorative and sometimes surgical techniques. For many, osseointegrated dental implants are considered to be the gold standard in tooth replacement.
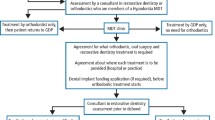
A multidisciplinary hypodontia clinic for patients with congenitally missing teeth has been held in the Paediatric Department of Glasgow Dental Hospital and School since February 2002. It incorporates consultants from paediatric, restorative, orthodontics and oral and maxillofacial surgery and aims to ensure appropriate timing and management at each stage of treatment.16
Similar combined, multidisciplinary clinics are held in other dental hospitals of the United Kingdom.1,17,18 Hobkirk et al.18 presented demographic data for those attenders, but there appears to be a dearth of contemporary information regarding treatment planning and outcomes. Furthermore, it would be useful for general dental practitioners to have information about treatment options and how it will affect their patients.
Since hypodontia treatment plans can continue over many years and include different dental specialties and locations, the management is very demanding of human, financial and material resources. All these factors may impact on long-term service provision and resource planning. In these regards, information about treatment and the outcomes could be of value.
Aims
-
A
To report the demographics of patients with congenital hypodontia attending the Glasgow Dental Hospital and School (GDH&S) multidisciplinary hypodontia clinic for the first time, from the date the clinic began in February 2002 until February 2007
-
B
(i) To report on both the treatment planned and whether this was completed in patients with hypodontia attending the multidisciplinary clinic at Glasgow Dental Hospital and School; (ii) to show the number of patients for whom implants were considered.
Method
For every patient attending the clinic, a data collection form is normally completed. The information obtained includes patient demographics, missing teeth, specialties involved and the treatment plans. This data are then entered into a database and updated periodically.
A complete list of all patients seen on the hypodontia clinic was obtained by searching the hospital's computerised patient appointment system. Data regarding patient demographics, ie gender, age and social status was collected from each patient's initial visit to the clinic during the period February 2002 to February 2007. Family history and related medical history information was also collected at this time, along with the number and type of congenitally missing teeth. The patients' social statuses were referenced from their post codes and matched to deprivation categories.19 Data pertaining to treatment planning, details of the specialties involved and outcome of treatment was collected for each visit attended during the period February 2002 to December 2005, allowing a minimum of 14 months follow-up time.
Outcome of treatment was categorised as:
-
Completed as planned
-
Completed with changes made
-
Abandoned
-
Ongoing as planned
-
Ongoing with changes made
-
No treatment required.
This data was collected from three sources:
-
1
The existing hypodontia database
-
2
Hypodontia clinic form within the patients' notes
-
3
Information directly from the patients' clinical records and radiographs.
The potential use of implants was also recorded. Finally, the distribution of missing permanent teeth was referenced against different patterns based on postulated gene expression.10,11,12,13
Results
There were 26 clinics, over which 178 patients had been booked. Of the 153 appointments kept, 128 of these were new patients and 25 were follow-up appointments.
A. Demographics
A total of 128 patients were seen for an initial appointment between February 2002 and February 2007. Of these, three had been booked to the clinic in error, one had acquired hypodontia, two had inadequate data in the notes and fourteen casenotes were unobtainable. Therefore, complete data was collected for 108 patients. One hundred and seven were cases of hypodontia in the permanent dentition and one was of hypodontia affecting the primary dentition.
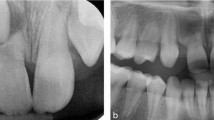
There were 57% female patients, ages ranged from 5 to 35 years with a mean of 13 years, and 27% (29) lived in areas of social deprivation (DEPCAT scores of 6 and 7). A positive or suspected family history of hypodontia was present in 56% (55) of patients, and 3.7% (4) had a hypodontia-related medical history. Ninety-one percent (n = 107) of patients were missing two or more teeth (Fig. 1). The most commonly missing teeth were upper lateral incisors and lower and upper second premolars (Fig. 2).
B. Treatment planning and outcomes
There were 83 patients eligible for inclusion in this part of the study.
Specialities involved in treatment included paediatric dentistry, orthodontics, oral and maxillofacial surgery and restorative dentistry. The treatment planned is shown in Table 1 and treatment outcomes are shown in Figure 3. There were 19 (21.3%) patients considered for implants. The patients that abandoned treatment numbered 13 (16%) and this included three who were satisfied with their outcome midway through their course of treatment. A further ten did not attend their appointments to complete the treatment.
On examination of the database information regarding the patterns of missing teeth, there is a suggestion that one patient may have had the gene marker PAX9m pattern. This person was found to be missing all second permanent molar teeth.
Discussion
It is evident from the data collected that maxillary lateral incisors are the most commonly absent tooth. This has also been reported by other groups of workers.20,21 The demographic data obtained was similar to that previously published by Hobkirk et al.18 with similar distribution patterns being found for the number and frequency of missing teeth. Minimum to maximum missing teeth ranged form one to 23. Therefore, there were comparable distribution patterns for the number and range of missing teeth.
Since our sample was mainly adolescent, the absence of third molars could not be fully ascertained by radiographic means. Historically, hypodontia studies have not included wisdom teeth and it is generally accepted that they are often not radiographically evident until a patient reaches early teenage years. However, previous studies suggested that the majority (85%) are only radiographically visible at 12 years,22 while in a small number of cases third molar genesis has been reported up to the age of 16 years.23,24 Finally, patients with hypodontia may also have delayed dental development.25,26
Third molars were not included in the present study, agreeing with the definition of severe hypodontia by Hobkirk et al.17 Additionally this data collection protocol has been used in previous studies.18
MSX-1 (a mutation of the homeobox gene) is a genetic marker associated with hypodontia, which relates to the absence of both second premolars and third molars.10 It could not be established whether MSX-1 was a factor in our sample population. Though only one patient may possibly have had PAX9m gene marker, this can only be confirmed by genetic investigation of this patient. Occasionally, hypodontia may be indicative of an underlying genetic disease and further referral for genetic testing may desirable.23
The level of social deprivation19 was less than the local population within this health board region, however closer to the national average. This may reflect that the Dental Hospital covers a large area of referral and includes patients from at least four out of Scotland's fourteen National Health Service health boards.
A single patient could have any number of combinations of the planned treatments as outlined in Table 1. This reflects the numerous permutations of treatment available for managing hypodontia. It is unsurprising that orthodontic therapy was the most frequently planned treatment component, included in the treatment plans of just under half the patients in the study. Patients with hypodontia may often have spaced dentitions, requiring space localisation prior to placement of fixed prostheses.
The second most common treatment planned was composite/veneer restoration, utilised at different stages of the patients' treatment. In earlier stages of treatment, composite may be used to disguise spaces that are aesthetically displeasing to the patient, having an immediate impact on their self-esteem. Therefore, interim aesthetics can be dealt with while awaiting further growth development by reviewing/monitoring. This monitoring process was the third most common planned treatment at the hypodontia clinic. In the latter stages, after the conclusion of orthodontic therapy, the composite/veneers constructed would be the final definitive restoration.
Hypodontia patients are a priority group for implant treatment under the National Health Service.27 Of the 19 patients for whom implant surgery has been planned, given their age, it is not known whether this ultimate goal will be achieved. Patients planned for implants may subsequently not undergo the required surgery. This may be due to unfavourable bone quality, morphology or volume in the proposed fixture sites.28 There was a small cohort of patients that were planned for significant oral/maxillofacial surgical procedures, eg osteotomies, ridge augmentation and sinus lifts, as a prerequisite to their implant treatment.
Absence of teeth is usually identified by the general dental practitioner, who has an important role for hypodontia patients in their identification, appropriate referral, preventative care and maintenance of existing dentition before and especially after treatment.
Practitioners can advise their patient on the nature of a multidisciplinary clinic, the extensive time and commitment required by the patient for treatment and the differing maintenance regimes required at completion of treatment. Orthodontic maintenance can involve long-term retention, including permanent retention. Osseointegrated implants will require the practitioner to be aware of their collective apparatus, maintenance of the health of the surrounding periodontal tissues and replacement of failing components.
Finally, not only is there a commitment by the patient, but also by their accompanying parent/guardian, as the majority of cases involve children. This could include cost and time to travel to the dental hospital, time off work and child care. This may be an area for future study to understand patient and family obligations over these long treatment plans.
Conclusions
The majority of the patients were female, adolescent and had a positive or suspected family history of hypodontia. The most commonly missing teeth were upper lateral incisors and lower and upper second premolars. Over a quarter of patients were socially deprived. Orthodontic therapy was the treatment most frequently considered in treatment planning. Nineteen patients (23%) may undergo surgery for placement of dental implants.
References
Nunn J H, Carter N E, Gillgrass T J et al. The interdisciplinary management of hypodontia: background and role of paediatric dentistry. Br Dent J 2003; 194: 245–251.
Grahnen H . Hypodontia in the permanent dentition. A clinical and genetical investigation. Odont Revy 1956; 7(3): 1–100.
Burzynski N J, Escobar V H . Classification and genetics of numeric anomalies of dentition. Birth Defects Orig Artic Ser 1983; 19: 95–106.
Gravely J F, Johnson D B . Variation in the expression of hypodontia in monozygotic twins. Dent Pract Dent Rec 1971; 21: 212–220.
Boruchov M J, Green L J . Hypodontia in human twins and families. Am J Orthod 1971; 60: 165–174.
Brook A H . A unifying aetiological explanation for anomalies of human tooth number and size. Arch Oral Biol 1984; 29: 373–378.
Bohn A . Dental anomalies in harelip and cleft palate. Acta Odontol Scand 1963; 21: 1–109.
Ranta R . The development of the permanent teeth in children with complete cleft lip and palate. Proc Finn Dent Soc 1972; 68: 1–27.
Shapira Y, Lubit E, Kuftinec M M . Congenitally missing second premolars in cleft lip and cleft palate children. Am J Orthod Dentofacial Orthop 1999; 115: 396–400.
Vastardis H, Karimbux N, Guthua S W et al. A human MSX1 homeodomain missense mutation causes selective tooth agenesis. Nat Genet 1996; 13: 417–421.
van den Boogaard M J, Dorland M, Beemer F A et al. MSX1 mutation is associated with orofacial clefting and tooth agenesis in humans. Nat Genet 2000; 24: 342–343.
Stockton D W, Das P, Goldenberg M et al. Mutation of PAX9 is associated with oligodontia. Nat Genet 2000; 24: 18–19.
Lidral A C, Reising B C . The role of MSX1 in human tooth agenesis. J Dent Res 2002; 81: 274–278.
Vieira A R, Meira R, Modesto A et al. MSX1, PAX9, and TGFA contribute to tooth agenesis in humans. J Dent Res 2004; 83: 723–727.
Cobourne M T . Familial human hypodontia – is it all in the genes? Br Dent J 2007; 203: 203–208.
Hobson R S, Carter N E, Gillgrass T J et al. The interdisciplinary management of hypodontia: the relationship between an interdisciplinary team and the general dental practitioner. Br Dent J 2003; 194: 479–482.
Hobkirk J A, Brook A H . The management of patients with severe hypodontia. J Oral Rehabil 1980; 7: 289–298.
Hobkirk J A, Goodman J R, Jones S P . Presenting complaints and findings in a group of patients attending a hypodontia clinic. Br Dent J 1994; 177: 337–339.
McLoone P . Carstairs scores for Scottish postcode sectors from the 2001 Census Report. Glasgow: MRC Social & Public Health Sciences Unit, 2004.
Muller T P, Hill I N, Peterson A C et al. A survey of congenitally missing teeth. J Am Dent Assoc 1970; 81: 101–107.
Brekhus P J, Oliver C P, Montelius G . A study of the pattern and combinations of congenitally missing teeth in man. J Dent Res 1944; 23: 117–131.
Clow I M . A radiographic survey of third molar development: a comparison. Br J Orthod 1984; 11: 9–15.
Richardson M . Late third molar genesis: its significance in orthodontic treatment. Angle Orthod 1980; 50: 121–128.
Van der Weide Y S, Prahl-Andersen B, Bosman F . Tooth formation in patients with oligodontia. Angle Orthod 1993; 63: 31–37.
Garn S M, Lewis A B . The gradient and the pattern of crown size and reduction in simple hypodontia. Angle Orthod 1970; 40: 51–57.
Rune B, Sarnas K . Tooth size and tooth formation in children with advanced hypodontia. Angle Orthod 1974; 44: 316–321.
Faculty of Dental Surgery of the Royal College of Surgeons of England. Guidelines for selecting appropriate patients to receive treatment with dental implants: priorities for the NHS. London: RCSE, 1997.
Jepson N J, Nohl F S, Carter N E et al. The interdisciplinary management of hypodontia: restorative dentistry. Br Dent J 2003; 194: 299–304.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Shafi, I., Phillips, J., Dawson, M. et al. A study of patients attending a multidisciplinary hypodontia clinic over a five year period. Br Dent J 205, 649–652 (2008). https://doi.org/10.1038/sj.bdj.2008.1080
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.1080
This article is cited by
-
The interdisciplinary management of hypodontia patients in the UK: a national service evaluation
British Dental Journal (2017)