Abstract
Introduction:
A 42-year-old female with no significant comorbidities presented to our care with a penetrating glass injury to her mid-thoracic spine after falling backwards onto a table.
Case presentation:
A large fragment of glass was protruding from her spine, and multi-planar computed tomography imaging revealed protrusion through the thoracic spinal vertebrae with the glass shards located 2 mm from the aortic lumen. The management of this patient posed several challenges, including initial care of the patient, evaluation of potentially affected structures and the appropriate sequence of therapeutic interventions. After multidisciplinary discussion, our trauma, thoracic and neurosurgical teams formulated a diagnostic workup and two-step surgical approach to address her injuries.
Discussion:
Here we present the approach used by our team to successfully manage this type of injury. We hope this case report represents a platform for future discussion on best management approaches in patients presenting with the low-velocity penetrating thoracic, spinal and posterior mediastinal trauma.
Similar content being viewed by others
Introduction
In the United States, penetrating chest injuries are commonly encountered in civilian trauma centers and are reported to be up to 20% of the overall causes of major trauma.1 While high-velocity injuries frequently involves more than one organ system and may result in greater tissue destruction and morbidity, low-velocity injuries (such as stabbing, impalement and falling) often lead to variable injury patterns with unknown trajectory and depth. These factors create diagnostic and therapeutic challenges for trauma surgeons—so knowledge of local anatomy and awareness of potentially affected structures influences the patient’s ultimate outcome.
Here we present a case of a low-velocity glass impalement injury with simultaneous penetration of the posterior mediastinum and spinal column. Although past case reports have described isolated penetrating injuries to the spine and mediastinum, to our knowledge, there has never been a reported case of simultaneous mediastinal and spinal column glass injury.2–6 This case presentation poses several unique management challenges in patients presenting with low-velocity penetrating injuries. We successfully managed this patient in multidisciplinary manner with planned diagnostic workup and sequenced surgical procedures.
Case presentation
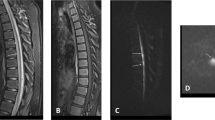
A 42-year-old woman tripped and fell backward onto a glass table in her home. She was found by emergency medical providers with a piece of glass protruding from her midline thoracic spinal region. She was placed on her side during transport and great care was taken to avoid moving the glass in her spine. Upon arrival to the emergency department, she was found to be hemodynamically stable and with no neurologic deficits. A glass shard was protruding 6 cm above the skin level. Multi-planar computed tomography of the thorax with contrast enhancement revealed multiple foreign bodies in the paraspinous muscles and through the left posterolateral spinal elements of the T6 vertebra with destruction of the left T6/T7 facet joint (Figure 1); the tip of a glass shard was located 2 mm from the thoracic aortic lumen in the posterior mediastinum without evidence of lung or major vascular injury. She was started on prophylactic antibiotics and admitted to the hospital. Given the close proximity of the esophagus, a water-soluble esophageal swallow study was obtained, which was negative for esophageal injury (Figure 2). Before proceeding with operative intervention, the trauma team pursued appropriate multidisciplinary discussion with the neurosurgical and thoracic surgery services. The neurosurgery service felt that the glass in subcutaneous tissues, paraspinous muscles and vertebrae could be extracted via laminectomy. The cardiothoracic surgery service was consulted and felt that the posterior mediastinal glass would be best removed via thoracotomy. All surgical teams decided that thoracotomy first approach would minimize chance of iatrogenic aortic injury.
Thus, the patient was taken to the operating room and placed in right lateral decubitus position, and a left posterolateral thoracotomy incision was made in the sixth rib interspace. The mediastinal pleura was visibly tented up by a glass shard immediately adjacent to the aorta, which had caused a small left-sided radicular artery injury. The radicular artery was controlled with clips, the posterior mediastinal pleura opened and the glass shard was removed. A 32-French thoracostomy tube was placed before closure. For the second surgery, the neurosurgery team positioned the patient in prone position and all externally visible glass was carefully removed (Figure 3). T6 laminectomy and removal of all remaining glass was approached through an incision, including the puncture wound. The T6/T7 facet joint was damaged, necessitating T6/T7 posterolateral arthrodesis and fusion. The patient had an uneventful postoperative course and was discharged on the fifth hospital day without neurologic deficits. She is now 1 year out from injury and continues to do well.
Discussion
Penetrating injuries to the thorax are common trauma encounters in the emergency setting and have various injury patterns. Given the various trajectories and depth of injury—as well as the risk of fragmentation as in our case—the trauma surgeon must be cognizant of potentially involved thoracic structures and plan appropriately before further intervention.
Impalement injuries to the mediastinum can have devastating consequences when involving the thoracic great vessels or viscera. The thoracic region accounts for 22–64% of penetrating spinal trauma though, among stabbing injuries, visceral injuries occur in 5–27% and thoracic great vessel injury in 2%.7–9 Pneumothorax and/or hemothorax are the most common injuries and most often only require tube thoracostomy, though 4% of patients require further surgical intervention.7,8 Penetrating low-velocity spinal wounds very rarely involve the aorta, and depending on level of injury, could be managed with thoracic, abdominal or even endovascular approaches.6
Care of impalement injury patients begins in the pre-hospital setting.2,3 Any foreign body should be left in place and great care should be taken to avoid manipulation of the object to limit further injury or exsanguination.2,3 When patients arrive in the emergency department, we believe the trauma surgery service should be the first to evaluate the patient in accordance with Advanced Trauma Life Support protocols and then engage all appropriate specialties. The reason for this is twofold: first, penetrating injuries may affect multiple organ systems for which the trauma surgeon is best-equipped to workup and prioritize therapies; second, the trauma team can then quickly involve consultants and initiate multidisciplinary discussion with regards to the appropriate surgical care of the injury.
Prophylactic antibiotics and tetanus should be given upon admission. Penetrating injuries can have unpredictable trajectories and multiple foreign bodies can be concealed or inadvertently retained.6,10 Thus, if the situation allows, surgeons need to have a low threshold for high-resolution imaging to rule out visceral injury and examine all potentially injured structures. In our case, the patient was hemodynamically stable and neurologically intact; hence, we were able to obtain contrast-enhanced computer tomography of the thorax, which demonstrated puncture of fragmented glass shards into the posterior mediastinum in immediate proximity to the aorta and esophagus. We were also able to obtain water-soluble swallow study to rule out esophageal injury. While others have reported on thoracotomy to remove glass shards10 or retained knife fragments,6 we are the first to discuss multiple surgical approaches for this type of penetrating glass injury with simultaneous posterior mediastinal and spinal column involvement.
Management of injuries involving multiple organ systems requires multidisciplinary discussion, specifically to discuss appropriately sequenced intervention. After meeting with neurosurgeons and thoracic surgeons, we concluded that spinal first approach may lead to iatrogenic aortic injury and that migration of the peri-aortic glass shard was probably the largest threat to life. Though the patient did not have any focal neurologic deficits, the retained glass was situated in the T6/7 facet joint and also represented an infection risk so the neurosurgery service felt it prudent to excise the remaining glass through laminectomy and stabilize the facet joint. We recognize that intact neurologic exam and hemodynamic stability were positive prognostic factors for our patient, implying lower injury severity and allowing time to coordinate appropriate therapeutic plans. Likewise, if glass shards had entered the left pleural space and caused a hemodynamically significant pneumothorax and/or hemothorax, emergent tube thoracostomy would have been indicated. A posterior and apically oriented chest tube may have dislodged the glass shards and potentially led to iatrogenic aortic injury. Finally, if glass shards had injured the esophagus at the T6–T7 location, this may have required bilateral thoracotomies to repair the esophagus and clear the peri-aortic glass with need for intraoperative repositioning. Overall, the multidisciplinary management of this patient could have been essential in preventing neurological and/or spinal cord injury in the operative setting. This highlights the benefit of pre-emptive multidisciplinary management even in patients presenting with intact neurological exam. This patient was fortunate to have spinal trauma without spinal cord injury or neurologic deficit. There are several instances of spinal cord injury from penetrating trauma with variable outcomes,6,7 and practitioners involved in the care of spinal cord injury patients—especially in the acute setting—need to be aware of possible injury to surrounding structures and the impact of related injuries on the care of spinal cord injury patients. Practitioners must be comfortable with multidisciplinary consultation potentially delaying intervention for devastating spinal cord injuries to ensure there are no more acute threats to life. Most important, spinal precautions must be exercised until fixation, and extra care given to maintaining strict spinal immobilization when transferring patients from the intensive care unit to the operating or radiology suites.
There are several factors to consider when faced with this type of penetrating injury, though we feel that addressing the highest-risk injuries in systematic manner and with involvement of surgical sub-specialists provides a good framework for tackling these injuries. Ultimately, we propose that future patients with similar injury patterns to our patient be managed with a comparable diagnostic and multidisciplinary treatment paradigm, emphasizing properly sequenced interventions.
Conclusion
This case demonstrates the first reported successful treatment of penetrating glass injury to the to the spine and posterior mediastinum. Careful preoperative planning with appropriate imaging and multidisciplinary consultation resulted in a plan of treatment that minimized potential iatrogenic injuries. Pre-hospital care, early multidisciplinary involvement and appropriate sequence of intervention led to uneventful surgeries and benign postoperative course.
Additional Information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW Jr et al. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma 1990; 30: 1356–1365.
Edwin F, Tettey M, Sereboe L, Aniteye E, Kotei D, Tamatey M et al. Impalement injuries of the chest. Ghana Med J 2009; 43: 86–89.
Wimalachandra W, Asmat A . Mediastinal impalement with a fibreglass sheet. Singapore Med J 2014; 55: e148–e149.
Begaz T, Bokhari F . Spinal impalement with a drill bit. J Emerg Med 2009; 36: 400–401.
Shahlaie K, Chang DJ, Anderson JT . Nonmissile penetrating spinal injury. Case report and review of the literature. J Neurosurg Spine 2006; 4: 400–408.
Simşek O, Kilincer C, Sunar H, Hamamcioğlu MK, Canbaz S, Cobanoğlu S et al. Surgical management of combined stab injury of the spinal cord and the aorta—case report. Neurol Med Chir (Tokyo) 2004; 44: 263–265.
Peacock WJ, Shrosbree RD, Key AG . A review of 450 stab wounds of the spinal cord. S Afr Med J 1977; 51: 961–964.
Simpson RK, Venger BH, Narayan RK . Treatment of acute penetrating injuries of the spine: a retrospective analysis. J Trauma 1989; 29: 42–46.
Demetriades D . Penetrating injuries to the thoracic great vessels. J Card Surg 1997; 12: 173–179, discussion 179–180.
Shoko T . Accidental chest penetration of glass foreign bodies in a 53 year old lady—the challenges with video assisted thoracoscopic extraction. Int J Surg Case Rep 2016; 23: 124–127.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Deramo, P., Agrawal, V. & Jefferson, H. Near miss for big red: a unique case of penetrating glass injury of the thoracic spine and posterior mediastinum. Spinal Cord Ser Cases 3, 17060 (2017). https://doi.org/10.1038/scsandc.2017.60
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2017.60