Abstract
Introduction:
Coronary vasospasm is a transient sudden vasoconstriction of one of the coronary arteries that can lead to myocardial ischaemia, myocardial infarction, fatal arrhythmia and sudden death. Most patients with coronary spasm have underlying cardiac pathology.
Case Presentation:
This paper presents a rare case of intractable autonomic dysreflexia in a 36-year-old patient with chronic C5 paraplegia with silent myocardial ischaemia secondary to coronary vasospasm in the absence of underlying cardiac pathology. The MRI perfusion study revealed normal left ventricular contractility and no evidence of coronary artery occlusion.
Discussion:
This case highlights the cardiac complications associated with paroxysmal heightened sympathetic nervous system and proposes that autonomic dsyreflexia can predisposes to coronary vasospasm via uncontrolled sympathetic nervous system. The disruption of sensory input from the myocardium to the brain in patient with SCI predisposes them to asymptomatic myocardial ischaemia. The challenges in the diagnosis and management of coronary vasospasm associated with autonomic dysreflexia are described.
Similar content being viewed by others
Introduction
Autonomic dysreflexia (AD) is a potentially life-threatening symptom complex, which may occur in individuals with spinal cord injuries (SCI) at T6 or above. Noxious visceral or cutaneous stimuli causes a sudden, massive, uninhibited reflex sympathetic discharge, resulting in hypertensive crisis (that is, defined as more than 20 mm Hg sudden increase of blood pressure over baseline) and is associated with profound alterations in sudomotor, pilomotor and vasomotor activites. Patient can potentially succumb to life-threatening neurological, respiratory and cardiac complications.1–3 The higher the level of the SCI, the more severe the bouts of AD, as measured by the level of hypertension.4
Abnormal cardiovascular physiology after SCI has been well documented in human studies and animal models. It has been postulated that disruption of supraspinal control of the sympathetic nervous system resulted in the following pathophysiologic phenomena: 1) loss of supraspinal regulatory control, 2) reduced sympathetic activity, 3) morphologic changes in sympathetic preganglionic neurons and 4) peripheral alpha-adrenoceptor hyperresponsiveness in the blood vessels and the heart.4,5 Despite our understanding of the pathophysiology behind altered cardiac control in AD, there is a lack of emphasis of cardiac events in AD.
Various cardiac complications have been reported in association with AD, such as premature atrial-ventricular contraction, conduction block, sinus tachycardia and bradycardia, ventricular fibrillation, atrial fibrillation, myocardial infarction and cardiac arrest.1,3 However, the effect of AD on coronary artery has never been reported.
We report a unique case of intractable AD with coronary vasospasm in a young patient with complete SCI below C5. This case report illustrates the profound cardiac complication associated with repeated bouts of sympathetic overflow.
Case report
Mr LSZ, a 36-year-old Chinese gentleman with chronic cervical C5 AIS A (American Spinal Injury Association Impairment Scale), complete SCI presented with recurrent symptoms of AD to medical emergency unit. He had recurrent headache that was associated with sweating, palpitation and increasing lower limb spasms. AD started 2 days ago when he had a blocked suprapubic catheter and AD resolved after he had urine leaked through his penis. Though he has had suprapubic catheter changed, his symptoms recurred over the last 2 days. There was no urine discolouration or foul smelling, suggestive of urinary tract infection. On admission, he was afebrile with blood pressure (BP) and heart rate (HR) measuring 151/80 mm Hg and 150 beats per minute (b.p.m.), respectively. The established AD management protocol was instituted, which include positioning patient in a propped up position, loosening tight clothing and readjustment of suprapubic catheter. His symptoms subsided with BP and HR went down to 99/65 mm Hg and 74 b.p.m., respectively.
Initial evaluation revealed no obvious etiology (for example, obstructed urinary flow, impacted stool and pressure ulcers) of the AD. The full blood count, renal profile and the inflammatory markers were normal. The baseline ECG showed sinus tachycardia with no acute ischaemic changes and arrhythmias. Abdomen imaging (that is, ultrasound abdomen and plain abdominal radiograph) did not reveal abnormal abdominal causes. Urine analysis showed positive leucocytes with negative nitrite and protein.
He was started on empirical ciprofloxacin to treat possible urinary tract infection (UTI), triggering the AD symptoms. However, within 24 h of admission, the AD symptoms recurred and wide variability in blood pressure was recorded with systolic and diastolic pressures measuring 120–210 mm Hg and 100–160 mm Hg, respectively. He continued to experience repeated AD attacks in the ward without any obvious precipitants based on serial workup. Gentle water irrigation of the bladder failed to abort the bouts of AD attack. In addition to the non-pharmacological measures, sublingual glyceryl trinitrate was given to control his BP.
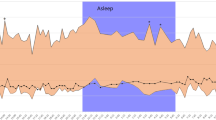
A ECG done during an AD attack with systolic BP rose up to 180–210 mm Hg, showed ST elevation at leads II, III, aVF, V4–6 and T-wave inversion on V1, V2 with no reciprocal changes on right-sided ECG leads (Figure 1). He was asymptomatic without symptoms of myocardial ischaemia. Medical history reviewed no cardiac history of coronary artery disease or cardiovascular risk factors and serial cardiac enzymes level were normal. The ECG changes were transient and preceded by AD attack, and the ECG changes were normalised when AD was aborted. He was transferred to high dependency unit for haemodynamic and telemetry monitoring. During observation over the next 2 days, he had five similar transient ST-segment changes in the ECG leads. The impression was coronary vasospasm, which coincides with AD attack and spontaneously resolved without the use of nitrolycerin.
The intractable AD aborted spontaneously during the fifth day of admission and serial repeated ECG remained normal (Figure 2). He had MRI cardiac perfusion study done, which showed normal left ventricular ejection fraction of 63%, no regional wall abnormality and normal stress perfusion. He had no further episodes of AD at 1 year follow-up visit.
Discussion
We report a case of myocardial ischaemia secondary to coronary vasospasm following an uncontrolled AD in an individual with chronic cervical SCI and no evidence of coronary artery disease.
To our knowledge, only 2 cases of silent myocardial ischaemia have been previously reported in individuals with cervical SCI. Walker et al.6 described a case of asymptomatic cardiac ischaemia that was not associated with AD attack in a 65-year-old patient with C7 incomplete SCI and multiple cardiac risk factors for coronary atherosclerosis. On the other hand, Ho et al.7 reported a 45-year-old male with chronic C5 complete SCI and a normal coronary artery on angiography presented with silent myocardial ischaemia that was associated with elevated troponin and ST-segment depression in V5 and V6 leads. Although significant, coronary artery disease has been ruled out, the troponin elevation and the ECG changes can be explained by oxygen supply-demand mismatch of the myocardium observed during the episode of AD, instead of secondary to coronary artery constriction. However, our case has numerous distinct and unique aspects. Firstly, the myocardial ischaemia was postulated to be due to coronary vasospasm developed as a consequence of uncontrolled AD. Our patient (that is, 36-year-old) was much younger than the individuals described by Walker et al.6 and Ho et al.7 Furthermore, beside his SCI, our patient had no previous medical history or any predisposing risk factors for coronary atherosclerosis. A normal MRI cardiac perfusion study further reinforced the fact that the coronary vasospasm was caused by the sympathetic overflow in persistent AD.
This is the only reported case of recurrent coronary vasospasm precipitated by AD attacks. Patients with coronary vasospasm typically described resting angina with circadian rhythm characteristic. However, in our case, diagnosis of coronary vasospasm was not straightforward as such classic presentation was absent, since the sensation below the level of C5 was impaired. Strictly speaking, the diagnosis of coronary spasm must be made on the basis of coronary angiographic findings.2 However, it is not possible to perform coronary angiography during the period of haemodynamic instability observed in recurrent AD attacks. Our diagnosis of coronary artery vasospasm was based on the indirect evidence of transient appearance of the classical ECG findings (that is, transient ST segment elevation in the anterolateral lead with reciprocal ST segment depression) and ruling out other important causes of chest pain.
The various stimuli for coronary vasospasm suggest that a variety of pathophysiological mechanisms are likely to be operating in different patients.2 In this case report, uncontrolled AD preceded ECG changes of coronary vasospasm. We postulated that the widespread activation of the sympathetic nervous system and the increase in norepinephrine level during the event of AD probably had induced severe vasoconstriction in the coronary vasculature in our patient. There are evidences in the cardiology literature using animal and human models to support that increased sympathetic outflow to the heart and stimulation of alpha-adrenoreceptor can trigger coronary spasm.8,9 Although this remains an attractive, yet unproven, pathophysiological hypothesis, we cannot exclude the possibility that this patient could have spontaneous coronary spasm precipitating an AD attack. The latter hypothesis is less likely as the coronary spasm resolved itself with the abortion of AD and the patient did not require the administration of nitroglycerine to abort the coronary spasm.
Management of coronary vasospasm in patient with AD poses a unique challenge. Due to overflow of sympathetic discharge triggering coronary vasoconstriction, identifying the causes of AD and the management of its hypertensive crisis are crucial to relieve the coronary vasospasm. All factors that could stimulate the gastrointestinal or genitourinary system can trigger AD. Bladder distension or irritation, followed by bowel distention represent the most common causes of AD.1 The etiology of the intractable AD in our case was not clear despite thorough evaluation, which posed a greater challenge in the management. The cause of AD was presumably due to UTI, though there was lack of convincing evidence.
Conclusion
Coronary vasospasm can arise in patient with recurrent refractory AD even in the absence of underlying coronary pathology as illustrated in this case. In view of the possibility of silent myocardial ischemia in individuals with SCI, patients with intractable AD should be admitted for closer BP control, and cardiac enzymes and ECG should be routinely ordered. Future prospective study using Holter monitor can be conducted to determine cardiac effects of heightened sympathetic adrenergic activity occurring during episodes of AD.
References
Krassioukov AV, Karlsson AK, Wecht JM, Wuermser LA, Mathias CJ, Marino RJ et al. Assessment of autonomic dysfunction following spinal cord injury: rationale for additions to International Standards for Neurological Assessment. J Rehabil Res Dev 2007; 44: 103–112.
Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y . Coronary artery spasm–clinical features, diagnosis, pathogenesis, and treatment. J Cardiol 2008; 51: 2–17.
Wan D, Krassioukov AV . Life-threatening outcomes associated with autonomic dysreflexia: a clinical review. J Spinal Cord Med 2014; 37: 2–10.
Krassioukov A . Autonomic function following cervical spinal cord injury. Respir Physiol Neurobiol 2009; 169: 157–164.
Teasell RW, Arnold JM, Krassioukov A, Delaney GA . Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch Phys Med Rehabil 2000; 81: 506–516.
Walker WC, Khokhar MS . Silent cardiac ischemia in cervical spinal cord injury: case study. Arch Phys Med Rehabil 1992; 73: 91–94.
Ho CP, Krassioukov AV . Autonomic dysreflexia and myocardial ischemia. Spinal Cord 2010; 48: 714–715.
Kakihana M, Noda H, Ohtsuka S, Sugishita Y, Ito I . Significant role of alpha 2-adrenoceptors in coronary artery spasm. Jpn Circ J 1985; 49: 108–118.
Chierchia S . The role of alpha-adrenergic receptors in the pathogenesis of coronary spasm. Clin Cardiol 1983; 6: 496–500.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Tan, S., Rahman, Z., Fauzi, A. et al. Coronary vasospasm in intractable autonomic dysreflexia. Spinal Cord Ser Cases 2, 16030 (2016). https://doi.org/10.1038/scsandc.2016.30
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/scsandc.2016.30